ABSTRACT
In 2023, the process of gradually introducing universal, free HPV vaccination into the vaccination program for children in Poland began. For this reason, the attitudes of parents of adolescents toward these vaccinations were examined in this study. The survey was conducted among 360 parents of children (girls and boys) aged 9–15. To achieve the best possible representativeness of the sample, parents were selected for the survey using a random-quota method. The survey was carried out using the CATI. The surveyed parents declared a high level of knowledge about HPV and awareness of HPV vaccination (74.2% of parents had heard of HPV, and 61.4% had heard of the HPV vaccine). The study showed a statistically significant relationship between parents’ education and knowledge of HPV infection – the higher the parent’s (mother or father) education, the higher the declared knowledge. Education was also a statistically significant factor influencing the declaration of vaccinating a child against HPV. In addition to parental education, the gender of the child was also a significant factor influencing willingness to vaccinate against HPV. Parents of boys were significantly more likely – than parents of girls – to declare that they would not vaccinate their sons against HPV. A significant factor influencing declarations to vaccinate against HPV was the child’s vaccination against COVID-19. The study results indicate a strong correlation between parental education and parental knowledge and attitudes about HPV and the HPV vaccine.
The most indicated disease caused by HPV infection is cervical cancer. According to WHO data, cervical cancer is the fourth most common cancer among the world’s female population; more than 324,000 women worldwide died because of it in 2020.Citation1 In Poland, the incidence and mortality rates for cervical cancer are 12.2/100,000 and 5.4/100,000, respectively, and the incidence of head and neck cancer is 1.27/100,000 (2018 data).Citation2 While HPV infection of types 16 and 18 is associated with about 70% of cervical cancers, HPV infection is etiologically linked to the development of other diseases as well.Citation3 It is assumed that globally nine out of ten cases of anal cancer, seven out of ten cases of vaginal cancer, one in two cases of penile cancer, and four out of ten cases of vulvar cancer are caused by HPV infection.Citation4,Citation5
One of the most effective ways to prevent HPV infection is vaccination. The first vaccine was approved in 2006.Citation6 By 2020, 107 countries had introduced HPV vaccination into the vaccination calendar.Citation7 Countries with high levels of HPV vaccination have seen significant decreases in HPV infections, precancerous cervical lesions, cervical cancer, and genital warts.Citation5,Citation8 The best example of the effectiveness of universal HPV vaccination for adolescents is the vaccination program, introduced in 2007 in Australia and consistently implemented to this day. Thanks to HPV vaccination and concurrent cytological screening among women, it is assumed that Australia will be the first country to eradicate cervical cancer as a public health problem. This goal is assumed to be achieved in 2028.Citation9–11 In the UK, on the other hand, a universal HPV vaccination program has led to nearly eliminating cervical cancer in women born after September 1, 1995, who were vaccinated at age 12–13.Citation12
As indicated by the results of a meta-analysis by Drolet et al., after several years of universal, routine vaccination in developed countries among girls aged 13–19, the incidence of HPV 16 and 18 decreased by 83%, and HPV 31, 33, and 45 by 54%. Among boys aged 15–19, the diagnosis of anogenital warts decreased by 48%.Citation13 For this reason, in most countries where vaccination is widespread, girls and boys are vaccinated, which has an evident scientific rationale.Citation14,Citation15
In 2020, the WHO adopted the “Global strategy to accelerate the elimination of cervical cancer as a public health problem.”Citation16 With this, the world is committed to the eradication of cervical cancer. Following this, the 53 member states of the WHO European Region developed the “Roadmap to accelerate the elimination of cervical cancer as a public health problem in the WHO European Region 2022–2030.”Citation17 The plan assumes that 90% of girls’ residence in the region who are less than 15 years old will be vaccinated against HPV, 70% of women will be screened with a high-performance test by 35 years of age and again by 45 years, and 90% of women identified with the cervical disease receive treatment.Citation17 The Polish government has decided to join the program and implement the WHO’s goals to eliminate HPV infections through population-based vaccination of adolescents.
In Poland, the HPV vaccine is included in the Immunization Program; however, as a recommended vaccination and thus not reimbursed, the patient or the patient’s parents must pay the full price of the vaccine. Over the past decade, even though there has been a lot of moral controversy surrounding HPV vaccination,Citation18 free HPV vaccination has been implemented in more than 100 cities and municipalities as part of local governments programs. In some cities, e.g., Wrocław, a high vaccination status of>80% of vaccinated adolescents was achieved.Citation19 As of November 2021, one formulation (a 2-valent vaccine targeting HPV16 and HPV18) has achieved a 50% reimbursement level for all registered indications. However, regardless of grassroots and local efforts, there was a need for a widespread, national HPV vaccination program for adolescents because the lack of a universal vaccination program is the reason for the HPV vaccination status of adolescents in the general Polish population at only 10% (data from 2020).Citation20 The National Oncology Strategy, created in 2022, assumes the introduction of free universal HPV vaccination for girls in 2023 and for adolescent boys in 2026. The goal of such that strategy is to vaccinate at least 60% of adolescent girls and boys against HPV in Poland by 2028.Citation21
The COVID-19 pandemic and the global use of COVID-19 vaccination have made vaccination, in general, one of the significant topics not only at the level of health policy and prevention but also individual decisions and attitudes toward vaccination. The odium of misinformation that afflicted COVID-19 vaccination may have translated into other vaccinations, including HPV vaccination, which may have implications for population-based vaccination and public health management in the near and long term.Citation22–24
Predictors of health behavior for HPV vaccination of children and adolescents who have not reached adulthood are socially “borrowed” since the parent’s decision to vaccinate is made, and the vaccination is performed on the child. Nevertheless, one of the best theoretical fields for considering HPV vaccination is the Health Belief Model by Becker.Citation25 The premise of this theory is based on two variables drawn from theoretical considerations of individual and social actions. First, on the value attributed by the individual to a given action to lead to a particular goal. Second, the individual’s estimate of the probability that a given action will bring about a specific goal.Citation26 In this case, the action is to vaccinate a child against HPV to protect against HPV infection while considering the risk of the child being infected with HPV. The Health Belief Model highlights four dimensions based on which a decision is made for a specific action, in this case, vaccinating a child against HPV. Perceived susceptibility is an assessment of the risk of HPV infection; perceived severity is an assessment of the health consequences that HPV infection will bring; perceived benefits refer to the effectiveness of preventing HPV infection, in this case by vaccinating against HPV; perceived barriers by assessing costs and benefits against the risks of vaccination.Citation27
Given these procedural changes, which are an opportunity for higher vaccination rates among adolescents against HPV in Poland, as well as the recommendations of medical institutions that specifically recommend vaccinating younger adolescents who have not yet begun their sexual lives,Citation28,Citation29 we decided to carry out a study whose principle aim of the study was to find out the level of knowledge and attitudes of parents about HPV and the HPV vaccine. The parental examination is critical because – due to current laws – teenagers cannot be vaccinated against HPV without the consent of a parent/legal guardian.
During the study, we wanted to find answers to the following research questions:
Do parents know of the existence and effects of the HPV vaccine?
What percentage of parents have vaccinated their children against HPV?
What factors influence a parent’s decision to vaccinate their child against HPV?
To what extent does parents’ trust in the doctor who recommends HPV vaccination influence the decision to vaccinate?
Do parents of children vaccinating their child against COVID-19 show a higher level of a declaration of vaccinating their child against HPV?
Materials and methods
Design of the study and study sample
The study’s main objective was to learn about the attitudes of parents (mothers and fathers) of children toward HPV vaccination. We narrowed the group to parents of children between 9 and 15 years old, i.e., from the recommended optimal age for HPV vaccine administration until the child finished primary education. In situations where the surveyed parent had more children – including more children between the ages of 9 and 15 – we asked them to answer the questions with their youngest child between 9 and 15 in mind. A stratified random sampling of respondents was used to make the survey representative.
The survey was representative of parents of children aged 9–15 in Poland. Random-quota method was used to select the survey sample. Respondents to the survey were qualified by the child’s place of residence, gender, and relevant age bracket based on the Central Statistical Office’s data on the population by single age and gender of children for 2021. One quota was the distinction between urban (percentage share 55.9%, number of surveys 201) and rural (share and the other one was the distinction between 16 provinces (). Sample size was calculated by statisticians based on a sample of parents of children aged 9–15 in Poland. The survey was conducted in September 2022, 360 parents of children aged 9–15 participated in the survey.
Table 1. Distribution of the sample by gender and place of residence (province) of the child (N = 360).
The survey was carried out through computer-assisted questionnaire interviews by telephone – CATI (Computer Assisted Telephone Interviewing) by interviewers explicitly trained for the study. The interviewers, using the telephone, asked questions from the interview questionnaire and then entered the responses received using specialized computer software. Respondents’ answers were added to the database in real time. Therefore, there is no risk of losing responses. The computer program automatically checks answers coherence and set control questions.
The questionnaire
The questionnaire was created specifically for the study, based on the authors’ knowledge and expertise – sociological, methodological, medical, and clinical. The questionnaire was validated ad hoc by interdisciplinary experts. The survey questionnaire consisted of 9 metric questions and 9 factual questions. The metric questions included questions about the respondent’s gender, the sex of the child, place of residence, education, and assessment of their financial situation. In the factual part, respondents were asked about their attitude toward vaccination, their level of trust in the doctor who cares for the child and manages the child’s vaccination calendar, their awareness of HPV, the diseases that HPV causes, and their willingness to vaccinate their child against HPV. All questions were single-choice questions, with some questions being dichotomous. Before the implementation of the actual survey, the tool was evaluated on a group of 12 parents of children aged 9–15 so that the validity of the concepts used in the tool was checked, and the methodological and structural correctness of the questionnaire was verified. The results from the pilot study were excluded from the main study.
Statistical analysis
Descriptive statistics was conducted for presenting the demographic variables. Outcome variable in our study is HPV vaccine. The relationship between variables was evaluated by using the Chi-squared test. Statistical analyzes were performed in IBM SPSS Statistics 27.0.1.0. For all analyzes, a p-level of < .05 was considered statistically significant. The statistical significance threshold was set at p < .050
Ethical considerations
The survey was conducted by the Biostat Research and Development Center, which is among the research units with CBR status in the register maintained by the Minister of Entrepreneurship and Technology, which provides a guarantee that the survey was conducted ethically, under international requirements for ethical action in conducting quantitative research. All survey participants were informed about the survey and its purpose and assured anonymity and confidentiality.
Results
Sociodemographic characteristics of respondents
Most respondents were women, and one in two were in their 40s ().
Table 2. Sociodemographic characteristics of respondents (N = 360).
Parents’ attitudes toward vaccinating their child according to the vaccination calendar
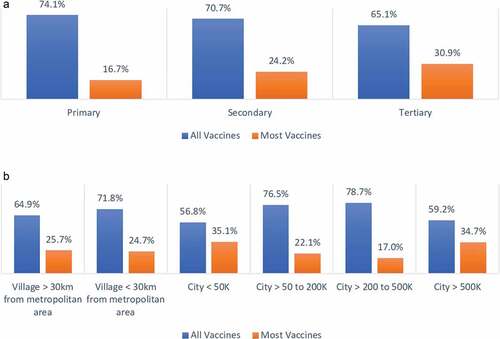
Two-thirds of respondents (68.9%, N = 248) vaccinated their children with all possible vaccinations. One in four respondents (25.8%, N = 93) vaccinated their child with most vaccines, with a few exceptions. In a few cases (N = 12), the child was only vaccinated with selected vaccines, a minority on the vaccination calendar. In five cases, the parent did not remember whether the child had been vaccinated. In two cases, the child was not vaccinated at all.
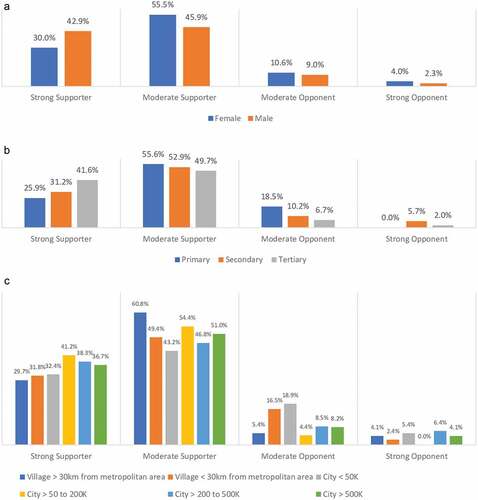
The higher the education level, the percentage of vaccinating their child with all vaccines decreased (). The lowest percentage of those vaccinated their child with all vaccines was in the largest cities ().
Figure 1. (a) Percentage of parents vaccinated their child with all or most indicated vaccines (by education) (N = 341). (b) Percentage of parents vaccinated their child with all or most indicated vaccines (by place of residence) (N = 341).
Parents’ attitudes toward vaccinating their child against COVID-19
Nearly half of the respondents (N = 163, 45.3%) had vaccinated their children against COVID-19. As parents’ education increased, the percentage of vaccinated children increased (). The lowest percentage of children vaccinated against COVID-19 was in rural areas and small towns, and the highest was in cities with more than 500,000 residents (p < .006) ().
Parents’ general attitude toward vaccination
One in three respondents (N = 125, 34.7%) strongly supported vaccination. Half of the respondents (N = 187, 51.9%) described themselves as moderate supporters of vaccination. One in ten parents (N = 36, 10.0%) declared themselves moderate opponents of vaccination, and twelve parents (3.3%) described themselves as strong opponents of vaccination.
Men were significantly more likely to declare themselves as strong supporters of vaccination than women (), those with a college education (p = .021) (), and those from medium and large cities ().
Parents’ trust in the doctor/pediatrician caring for the child regarding vaccinations
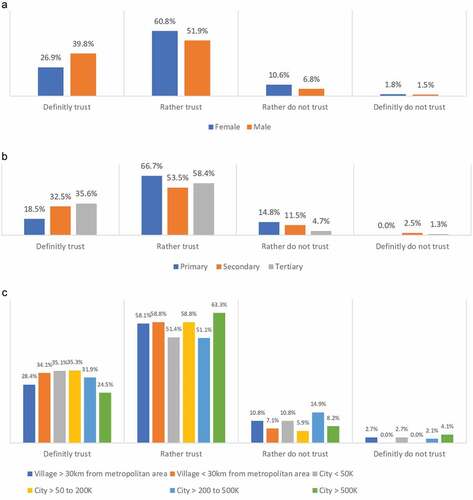
Most parents surveyed said they trust the doctor/pediatrician caring for their child regarding the doctor’s recommended vaccinations. One in three respondents (N = 114, 31.7%) trust the doctor regarding vaccinations, and more than half (n = 207, 57.5%) trust the doctor regarding vaccinations. One in eleven parents (N = 33, 9.2%) tend not to trust the doctor caring for their child on the issue of vaccinations, and six parents (1.7%) do not trust the doctor.
Fathers are more likely to strongly trust the doctor on the issue of vaccination for their child than mothers (), people with secondary and higher education (p = .048) (), and residents of small and medium-sized towns and villages close to urban areas ().
Figure 4. (a) Parents’ trust in the doctor caring for the child regarding vaccinations for the child (by gender) (N = 360). (b) Parents’ trust in the doctor caring for the child regarding vaccinations for the child (by education) (N = 360). (c) Parents’ trust in the doctor caring for the child regarding vaccinations for the child (by place of residence) (N = 360).
Parents’ knowledge of the dangers of HPV infection
Most parents (N = 267, 74.2%) have heard of HPV. One in four parents (N = 93, 25.8%) had not heard of the virus. Women were significantly more likely to have heard of HPV than men, parents of girls than boys (), those with higher education, and residents of cities and villages close to urban areas ().
Table 3. Do you know what diseases are caused by HPV infection? (by sex of parent and sex of child) (N = 360).
Table 4. Do you know what diseases are caused by HPV infection? (by parent’s education and place of residence) (N = 360).
Among those who had heard of the virus, one in three in this group (N = 100, 37.5%) knew what diseases it causes. The remaining, nearly two-thirds of parents (N = 167, 62.5%), despite having heard of the virus, did not know what diseases it causes. The disease that respondents most often indicated as being caused by HPV was cervical cancer and other cancers.
Parents’ knowledge and attitudes about HPV vaccination
Six in ten respondents (N = 221, 61.4%) had heard of the HPV vaccine, while 38.6% of respondents (N = 139) had not heard of the HPV vaccine. Women and girls’ parents were significantly more likely to have heard of the HPV vaccine (), those with higher education, from the largest cities, and those residence in rural areas ().
Table 5. Have you heard of the HPV vaccine? (by gender of parent and gender of child) (N = 360).
Table 6. Have you heard of the HPV vaccine (by education and place of residence) (N = 360).
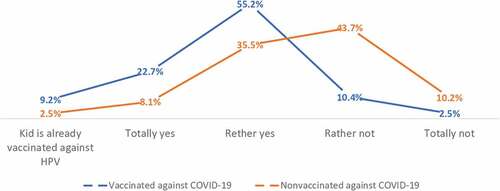
Twenty parents (5.6%) declared their child was already vaccinated against HPV. Six in ten respondents (N = 213, 59.1%) would like to vaccinate their child against HPV, with one in seven (N = 53, 14.7%) definitely wanting to vaccinate their child, and four in ten (N = 160, 44.4%) rather wanting to do so. Nearly three in ten parents (N = 103, 28.6%) would rather not want to vaccinate their child against HPV, and twenty-four parents (6.7%) definitely would not want to vaccinate their child.
Fathers were more likely to want to vaccinate their child than mothers, and those with higher education residence in the largest cities (). Parents of daughters were more likely than parents of sons to declare their willingness to vaccinate their child against HPV (p = .003) ().
Table 7. Declaration of child HPV vaccination by demographic category (N = 360).
Table 8. Declaration of child HPV vaccination by demographic category (N = 360).
Parents who declared that they did not want to vaccinate their child against HPV (N = 127) were presented with a list of diseases that HPV can cause and were then asked if they knew the dangers of the virus, they would vaccinate their child. One in four (25.2% – the total number of people who would definitely vaccinate or rather vaccinate their child) changed their minds, and one in three respondents in this group (63.0%) answered that they would rather not vaccinate. One in nine (11.8%) declared that they would definitely not vaccinate their child against HPV. The declaration of non-vaccination after learning about the diseases that women often sustained HPV causes, parents of boys, people with the lowest education, and residents of small towns and villages far from urban areas ().
Table 9. Declaration of vaccinating a child against HPV after learning about the list of diseases that can be caused by HPV by demographic category (n = 360).
Respondents who had vaccinated their child against COVID-19 were more likely to have their child vaccinated against HPV (p < .001) ().
Discussion
The main aim of the survey was to learn about the level of knowledge and attitudes of parents of Polish teenagers toward HPV vaccination. Learning about the attitudes and knowledge of parents of Polish adolescents is important because the Minister of Health announced that HPV vaccination will be a vaccination available free of charge in Poland in 2023 as a recommended vaccination for the population of girls 11–13 years old and – in subsequent years – boys.
The epidemiology of HPV infection and the risk of diseases that may develop as a result of HPV infection, as described in the Introduction, means that when considered within the framework of the Health Belief Model and its four dimensions (threat, efficacy, barriers, and benefits), HPV vaccination may be seen as beneficial to health care. The barriers associated with vaccination may seem insignificant from the perspective of HPV-caused diseases.
Our study showed a significant statistical relationship between parents’ education and their attitudes toward vaccination (p = .021). Strong supporters of vaccination were almost twice as many among parents with higher education than parents with primary education (41.6% vs. 25.9%). A study of a representative population of Americans found that less-educated parents showed less confidence in vaccinations in general and in doctors’ recommendations for their child’s vaccinations than parents with higher education.Citation22,Citation23,Citation30,Citation31 Researchers analyzing hesitation toward vaccination among mothers in Albania,Citation24,Citation32 Greece,Citation25,Citation33 and SpainCitation26,Citation34 have reached similar conclusions. The studies above provide evidence of a strong correlation between parental education and child immunization. They are part of the narrative of Gakidou’s meta-analysis, based on the results of nearly a thousand studies from many countries around the world, indicating the role of parental education, especially of mothers, on child health.Citation27,Citation35 Moreover, parents’ education also translates into the future attitudes of their children toward vaccination.Citation28,Citation36
We also showed a statistically significant relationship between parents’ education and trust in their child’s doctor on vaccinations (p = .048). In this case – as in the case of general attitudes toward vaccination – almost twice as many parents with higher education than parents with primary education strongly trusted their child’s doctor on vaccination (35.6% vs. 18.5%). Trust in a doctor regarding vaccinations is crucial in the decision to vaccinate a child,Citation29–31,Citation37–39 also when it comes to HPV vaccination.Citation32,Citation40 Furthermore, the higher a parent’s education level, the greater the chance the child will be vaccinated, according to the vaccination schedule.Citation26,Citation33,Citation34,Citation41 In an Israeli study, based on the results, a profile was drawn of a parent who trusts the doctor regarding vaccinations for the child and follows the rules outlined by the doctor. It is a parent who is highly educated, young, lives in the city, with no food preferences, and trusts medicine.Citation34,Citation42 Trusting your doctor about recommended vaccinations for your child, including HPV vaccination, is very important. In Spanish studies examining the influence of information sources on parents’ decision to vaccinate, the advice of the nurse and doctor is crucial.Citation35,Citation43
The declaration of vaccinating a child against HPV was statistically significantly correlated with the parent’s education and the child’s gender in our study (p = .003; p = .007). The higher the parent’s education, the significantly higher the percentage of respondents who declared that they would definitely vaccinate their child against HPV. This result is consistent with other studies that indicate that the lower the education, the lower the acceptance of vaccinating a child against HPV.Citation36–38,Citation44–46 On the other hand, it should be noted that although better-educated parents showed a higher degree of acceptance of vaccination in general and HPV vaccination, the highest percentage of already vaccinated children was declared by parents with the lowest education (p = .003). Similar indications were obtained in a U.S. study of adolescent girlsCitation39,Citation47 and studies focusing on the effect of race, income, and ethnicity on HPV vaccination.Citation40,Citation48 There are many indications that the higher rate of HPV vaccination among less-educated children (often associated with lower income and lower social standing) results from personal experience with cervical cancer and limited access to highly specialized health care, prompting preventive.Citation40,Citation41,Citation48,Citation49
Parents of boys were more likely to declare that they would rather not vaccinate or definitely not vaccinate their child against HPV (25.6% – a sum of negative responses for parents of girls vs. 44.8% – a sum of negative responses for parents of boys). These differences may be due to many myths about the potential effects of HPV vaccination in boys.Citation42,Citation50 A narrative review of publications completed by Grandahl and Neveus based on more than one hundred articles on HPV vaccination in boys and men provided insight into barriers to public awareness of the vaccine. In addition to a lack of knowledge and recommendations about vaccination, respondents identified promiscuity as an adverse event following vaccination.Citation43,Citation44,Citation51,Citation52 As Cooper points out, the WHO’s recommendations that the primary target population for HPV vaccination is adolescent girls who have not yet begun their sexual lives has led to a “feminization” of HPV vaccination, which may project its acceptance among boys or parents of boys,Citation45,Citation53 as indicated by a systematic analysis by Radisic et al.Citation46,Citation54 In addition, we indicated in our study that the parents of the children studied statistically significantly perceived the HPV vaccine more as a vaccine for girls than for boys (p = .003). That the feminization of the HPV vaccine may have a negative impact on health prevention related to HPV infections was pointed out by Daley et al. As the authors of this article point out, politics, economics, social norms, and scientific policy have influenced the fact that the HPV vaccine is still mainly associated with girls and women. Therefore, it is crucial to “normalize” HPV vaccines as important in maintaining the health of all people regardless of gender.Citation47,Citation55
A Chinese study observed that attitudes toward vaccination were strongly correlated with attitudes toward the COVID-19 vaccination. Those who were confident in the safety of the COVID-19 vaccination showed a belief in the safety of vaccination in general, and those who perceived vaccination as safe also perceived the COVID-19 vaccination as safe [Jing]. For this reason, in our study, we decided to contrast parents’ attitudes and actions toward COVID-19 and the HPV vaccine.Citation56 A statistically significant factor influencing the declaration of vaccinating a child against HPV was the child’s vaccination against COVID-19 (p < .001). Parents who declared that they had vaccinated their child against COVID-19 were significantly more likely to declare that they would also vaccinate their child against HPV. The researchers analyzed the relationships and similarities of recommendations for COVID-19 and HPV vaccination using quantitative and qualitative methods. What both vaccinations have in common is that they are administered to adolescents, and in most countries, they are not mandatory, and parents/guardians do not pay the cost of the vaccination. There was also concern that the COVID-19 pandemic would significantly disrupt population-based HPV vaccination. According to U.S. reports, only a dozen percent of physicians reported a decrease in HPV vaccination, one in eleven reported an increase in HPV vaccination during the pandemic, and the remainder, more than three-quarters of physicians, reported no change.Citation48,Citation57 Meanwhile, a qualitative study by Footman et al. examining parents’ attitudes about COVID-19 and HPV vaccines indicated that while concern about post-vaccination reactions for both vaccines was at similar levels, media coverage that explicitly promoted COVID-19 vaccination made attitudes toward the vaccines more favorable, and declarations of COVID-19 vaccination more frequent than declarations of HPV vaccination.Citation49,Citation58
Finally, it is worth noting that many studies that examine parental attitudes toward HPV vaccination mainly ask mothers of children. In our study, we asked mothers and fathers. Moreover, although the gender of the parent did not prove to be a statistically significant factor in many aspects of the survey, it is worth noting that in our study, fathers declared a higher degree of confidence in vaccination in general (p = .021) and declared a significantly higher degree of confidence in the doctor regarding recommended vaccinations for the child (p = .048). At the same time, the declaration of knowledge about HPV vaccination was similar in mothers and fathers, with mothers more likely to have heard about vaccination than fathers. Chen et al., in their meta-analysis, pointed out that in most of the studies analyzed, it is fathers who are more likely to accept vaccination in children than mothers,Citation59 as exemplified by Italian,Citation60 American,Citation61 or ArabCitation62 studies.
Study limitations
Our study had two main limitations. The first concerns the choice of technique. When conducting surveys using the CATI technique, there can be a halo effect that causes respondents, more often than with the CAWI technique, for example, to answer as one would expect them to rather than as they think and what they know. Such a sensitive topic as child vaccination can make a big difference. The second limitation was that we did not test parents’ factual knowledge of the effects of HPV infection but only relied on declarations of knowledge, which may differ from actual knowledge. An additional limitation of the survey is the quantitative method, which, while it allows for mapping respondents’ attitudes and range of knowledge, cannot examine their motivations.
Conclusions
Our study indicates that parental education has a very significant impact on several factors related to vaccination. The higher the parents’ education, the greater the group of supporters of vaccination, the greater the trust in the doctor regarding the vaccination he/she offers to the child, and the greater the declaration of knowledge about the risks of HPV infection and the declarative willingness to vaccinate the child against HPV. Our study showed that the implementation of HPV vaccination for girls and women, promoted in comprehensive media coverage, may have led to the “feminization” of vaccination. A pervasive educational work should be done to make boys and their parents (especially fathers) aware of the risks and pathways of HPV infection to strengthen the belief in this group that HPV vaccination affects them to the same extent as vaccination among girls.
Authors’ contributions
TS – study conceptualization, methodology, validation, investigation, statistical analysis, formal analysis, writing original draft, editing; IM – study conceptualization, review, editing; EA – study conceptualization, review, editing.
Acknowledgments
TS would like to thank Renata and Jan Sobierajski for guardianship and intellectual support and Prof. Waleria Hryniewicz for scientific and intellectual opportunities.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors upon request.
Additional information
Funding
References
- World Health Organisation. Cervical cancer. 2022 [accessed 2022 Oct 12]. https://www.who.int/news-room/fact-sheets/detail/cervical-cancer.
- Krajowy Rejestr Nowotworów. 2022 [accessed 2022 Oct 12]. http://onkologia.org.pl/raporty/#mapa_polski.
- McCormack PL. Quadrivalent human papillomavirus (types 6, 11, 16, 18) recombinant vaccine (gardasil(®)): a review of its use in the prevention of premalignant anogenital lesions, cervical and anal cancers, and genital warts. Drugs. 2014;74(11):1253–12. doi:10.1007/s40265-014-0255-z.
- Forman D, de Martel C, Lacey CJ, Soerjomataram I, Lortet-Tieulent J, Bruni L, Vignat J, Ferlay J, Bray F, Plummer M, et al. Global burden of human papillomavirus and related diseases. Vaccine. 2012;30:12–23. doi:10.1016/j.vaccine.2012.07.055.
- Martín-Hernán F, Sánchez-Hernández JG, Cano J, Campo J, Del Romero J. Oral cancer, HPV infection and evidence of sexual transmission. Med Oral Patol Oral Cir Bucal. 2013;18(3):e439–44. doi:10.4317/medoral.18419.
- Ljubojevic S, Skerlev M. HPV-associated diseases. Clin Dermatol. 2014;32(2):227–34. doi:10.1016/j.clindermatol.2013.08.007.
- Bruni L, Saura-Lázaro A, Montoliu A, Brotons M, Alemany L, Diallo MS, Afsar OZ, LaMontagne DS, Mosina L, Contreras M, et al. HPV vaccination introduction worldwide and WHO and UNICEF estimates of national HPV immunization coverage 2010–2019. Prev Med. 2021; 144:106399. doi:10.1016/j.ypmed.2020.106399.
- Herrero R, González P, Markowitz LE. Present status of human papillomavirus vaccine development and implementation. Lancet Oncol. 2015;16(5):e206–16. doi:10.1016/S1470-2045(14)70481-4.
- Schiffman M, Saraiya M. Control of HPV-associated cancers with HPV vaccination. Lancet Infect Dis. 2017;17(1):6–8. doi:10.1016/S1473-3099(16)30146-3.
- Patel C, Brotherton JM, Pillsbury A, Jayasinghe S, Donovan B, Macartney K, Marshall H. The impact of 10 years of human papillomavirus (HPV) vaccination in Australia: what additional disease burden will a nonavalent vaccine prevent? Euro Surveill. 2018;23(41):1700737. doi:10.2807/1560-7917.ES.2018.23.41.1700737.
- NHMRC Centre of Research Excellence in Cervical Cancer Control. 2021 Cervical Cancer Elimination Progress Report: Australia’s progress towards the elimination of cervical cancer as a public health problem. Melbourne, Australia; 2022 [accessed 2022 Oct 7]. https://www.cervicalcancercontrol.org.au/wp-content/uploads/2021/03/2021-C4-CRE-Elim-Report.pdf.
- Falcaro M, Castañon A, Ndlela B, Checchi M, Soldan K, Lopez-Bernal J, Elliss-Brookes L, Sasieni P. The effects of the national HPV vaccination programme in England, UK, on cervical cancer and grade 3 cervical intraepithelial neoplasia incidence: a register-based observational study. Lancet. 2021;398(10316):2084–92. doi:10.1016/S0140-6736(21)02178-4.
- Drolet M, Bénard É, Pérez N, Brisson M, HPV Vaccination Impact Study Group. Population-level impact and herd effects following the introduction of human papillomavirus vaccination programmes: updated systematic review and meta-analysis. Lancet. (2019);10(394):497–509. doi:10.1016/S0140-6736(19)30298-3.
- Crosignani P, De Stefani A, Fara GM, Isidori AM, Lenzi A, Liverani CA, Lombardi A, Mennini FS, Palu’ G, Pecorelli S, et al. Towards the eradication of HPV infection through universal specific vaccination. BMC Public Health. 2013;13(1):642. doi:10.1186/1471-2458-13-642.
- Temkin SM, Seibel NL. Are we missing an opportunity for cancer prevention? Human papillomavirus vaccination for survivors of pediatric and young adult cancers. Cancer. 2015;121(19):3395–402. doi:10.1002/cncr.29515.
- World Health Organisation. Global strategy to accelerate the elimination of cervical cancer as a public health problem. 2020 [accessed 2022 Oct 8]. https://www.who.int/publications/i/item/9789240014107.
- World Health Organisation. Roadmap to accelerate the elimination of cervical cancer as a public health problem in the WHO European Region 2022–2030. 2022 [accessed 2022 Oct 8]. https://apps.who.int/iris/bitstream/handle/10665/361293/72wd11e-Roadmap-Elim-CC-220591.pdf?sequence=1&isAllowed=y.
- Drejza M, Rylewicz K, Lewandowska M, Gross-Tyrkin K, Łopiński G, Barwińska J, Majcherek E, Szymuś K, Klein P, Plagens-Rotman K, et al. HPV vaccination among Polish adolescents-results from POLKA 18 study. Healthcare (Basel). 2022;10(12):2385. doi:10.3390/healthcare10122385.
- Ludwikowska KM, Biela M, Szenborn L. HPV vaccine acceptance and hesitancy - lessons learned during 8 years of regional HPV prophylaxis program in Wroclaw, Poland. Eur J Cancer Prev. 2020;29(4):346–49. doi:10.1097/CEJ.0000000000000556.
- NIZP-PZH, GIS. Szczepienia ochronne w Polsce w 2020 roku. 2022 [accessed 2022 Oct 14]. http://wwwold.pzh.gov.pl/oldpage/epimeld/2020/Sz_2020.pdf.
- Ministerstwo Zdrowia. Narodowa Strategia Onkologiczna. 2020 [accessed 2022 Oct 8]. https://www.gov.pl/web/zdrowie/narodowa-strategia-onkologiczna-nso.
- Mohamad E, Tham JS, Mohd Ajis SZ, Hamzah MR, Ayub SH, Tri Sakti AM, Azlan AA. Exposure to misinformation, risk perception, and confidence towards the government as factors influencing negative attitudes towards COVID-19 vaccination in Malaysia. Int J Environ Res Public Health. 2022 Nov 8;19(22):14623. doi:10.3390/ijerph192214623.
- Loomba S, de Figueiredo A, Piatek SJ, de Graaf K, Larson HJ. Measuring the impact of COVID-19 vaccine misinformation on vaccination intent in the UK and USA. Nat Hum Behav. 2021 Mar;5(3):337–48. doi:10.1038/s41562-021-01056-1.
- Lockyer B, Islam S, Rahman A, Dickerson J, Pickett K, Sheldon T, Wright J, McEachan R, Sheard L, Bradford Institute for Health Research COVID-19 Scientific Advisory Group. Understanding COVID-19 misinformation and vaccine hesitancy in context: findings from a qualitative study involving citizens in Bradford, UK. Health Expect. 2021 Aug;24(4):1158–67. doi:10.1111/hex.13240.
- Becker MH. The Health Belief Model and sick role behavior. Health Educ Behav. 1974;2(4):409–19. doi:10.1177/109019817400200407.
- Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the Health Belief Model. Health Educ Q. 1988 Summer;15(2):175–83. doi:10.1177/109019818801500203.
- Janz NK, Becker MH. The Health Belief Model: a decade later. Health Educ Q. 1984 Spring;11(1):1–47. doi:10.1177/109019818401100101.
- World Health Organization. WHO updated recommendations on HPV vaccination schedule. 2022 [accessed 2023 Feb 2]. https://www.who.int/news/item/20-12-2022-WHO-updates-recommendations-on-HPV-vaccination-schedule.
- Petrosky EY, Liu G, Hariri S, Markowitz LE. Human papillomavirus vaccination and age at first sexual activity, national health and nutrition examination survey. Clin Pediatr (Phila). 2017 Apr;56(4):363–70. doi:10.1177/0009922816660541.
- Nowak GJ, Cacciatore MA. Parents’ confidence in recommended childhood vaccinations: extending the assessment, expanding the context. Hum Vaccin Immunother. 2017;13(3):687–700. doi:10.1080/21645515.2016.1236881.
- Szilagyi PG, Shah MD, Delgado JR, Thomas K, Vizueta N, Cui Y, Vangala S, Shetgiri R, Kapteyn AP. Intentions and perceptions about COVID-19 vaccination for their children: results from a national survey. Pediatrics. 2021;148(4). doi:10.1542/peds.2021-052335.
- Mayerová D, Abbas K. Childhood immunisation timeliness and vaccine confidence by health information source, maternal, socioeconomic, and geographic characteristics in Albania. BMC Public Health. 2021;21(1):1724. doi:10.1186/s12889-021-11724-6.
- Giannakou K, Kyprianidou M, Hadjikou A, Fakonti G, Photiou G, Tzira E, Heraclides A. Knowledge of mothers regarding children’s vaccinations in Greece: an online cross-sectional study. BMC Public Health. 2021;21(1):2119. doi:10.1186/s12889-021-12179-5.
- Mora T, Trapero-Bertran M. The influence of education on the access to childhood immunization: the case of Spain. BMC Public Health. 2018;18(1):893. doi:10.1186/s12889-018-5810-1.
- Gakidou E, Cowling K, Lozano R, Murray CJ. Increased educational attainment and its effect on child mortality in 175 countries between 1970 and 2009: a systematic analysis. Lancet. 2010;376(9745):959–74. doi:10.1016/S0140-6736(10)61257-3.
- Zychlinsky Scharff A, Paulsen M, Schaefer P, Tanisik F, Sugianto RI, Stanislawski N, Blume H, Schmidt BMW, Heiden S, Stiesch M, et al. Students’ age and parental level of education influence COVID-19 vaccination hesitancy. Eur J Pediatr. 2022;181(4):1757–62. doi:10.1007/s00431-021-04343-1.
- Benin AL, Wisler-Scher DJ, Colson E, Shapiro ED, Holmboe ES. Qualitative analysis of mothers’ decision-making about vaccines for infants: the importance of trust. Pediatrics. 2006;117(5):1532–41. doi:10.1542/peds.2005-1728.
- Brunson EK. How parents make decisions about their children’s vaccinations. Vaccine. 2013;31(46):5466–70. doi:10.1016/j.vaccine.2013.08.104.
- Kennedy A, Lavail K, Nowak G, Basket M, Landry S. Confidence about vaccines in the United States: understanding parents’ perceptions. Health Aff. 2011;30(6):1151–59. doi:10.1377/hlthaff.2011.0396.
- Ylitalo KR, Lee H, Mehta NK. Health care provider recommendation, human papillomavirus vaccination, and race/ethnicity in the US National Immunization Survey. Am J Public Health. 2013;103(1):164–69. doi:10.2105/AJPH.2011.300600.
- Falagas ME, Zarkadoulia E. Factors associated with suboptimal compliance to vaccinations in children in developed countries: a systematic review. Curr Med Res Opin. 2008;24(6):1719–41. doi:10.1185/03007990802085692.
- Tal O, Ne’eman Y, Sadia R, Shmuel R, Schejter E, Bitan M. Parents’ attitudes toward children’s vaccination as a marker of trust in health systems. Hum Vaccin Immunother. 2021 2;17(11):4518–28. doi:10.1080/21645515.2021.1971472.
- Navarro-Illana P, Navarro-Illana E, Vila-Candel R, Díez-Domingo J. Drivers for human papillomavirus vaccination in Valencia (Spain). Gac Sanit. 2018;32(5):454–58. doi:10.1016/j.gaceta.2017.05.008.
- Smolarczyk K, Duszewska A, Drozd S, Majewski SP. Knowledge and attitude towards HPV and HPV vaccination in Poland. Vaccines. 2022 2;10(2):228. doi:10.3390/vaccines10020228.
- Kolek CO, Opanga SA, Okalebo F, Birichi A, Kurdi A, Godman B, Meyer JC. Impact of parental knowledge and beliefs on HPV vaccine hesitancy in Kenya-findings and implications. Vaccines. 2022 26;10(8):1185. doi:10.3390/vaccines10081185.
- Alarcão V, Zdravkova B. Attitudes and practices towards HPV vaccination and its social processes in Europe: an equity-focused scoping review. Societies. 2022;12(5):131. doi:https://doi.org/10.3390/soc12050131.
- Mohammed KA, Vivian E, Loux TM, Arnold LD. Factors associated with parents’ intent to vaccinate adolescents for human papillomavirus: findings from the 2014 national immunization survey-teen. Prev Chronic Dis. 2017;14:E45. doi:10.5888/pcd14.160314.
- Jeudin P, Liveright E, Del Carmen MG, Perkins RB. Race, ethnicity, and income factors impacting human papillomavirus vaccination rates. Clin Ther. 2014;36(1):24–37. doi:10.1016/j.clinthera.2013.11.001.
- Salz T, Gottlieb SL, Smith JS, Brewer NT. The association between cervical abnormalities and attitudes toward cervical cancer prevention. J Womens Health (Larchmt). 2010;19(11):2011–16. doi:10.1089/jwh.2009.1790.
- López N, Garcés-Sánchez M, Panizo MB, de la Cueva IS, Artés MT, Ramos B, Cotarelo M. HPV knowledge and vaccine acceptance among European adolescents and their parents: a systematic literature review. Public Health Rev. 2020 14;41(1):10. doi:10.1186/s40985-020-00126-5.
- Grandahl M, Nevéus T, Dalianis T, Larsson M, Tydén T, Stenhammar C. ‘I also want to be vaccinated!’ - adolescent boys’ awareness and thoughts, perceived benefits, information sources, and intention to be vaccinated against Human papillomavirus (HPV). Hum Vaccin Immunother. 2019;15(7–8):1794–802. doi:10.1080/21645515.2018.1551670.
- Grandahl M, Nevéus T. Barriers towards HPV vaccinations for boys and young men: a narrative review. Viruses. 2021 19;13(8):1644. doi:10.3390/v13081644.
- Cooper S, Schmidt BM, Ryan J, Leon N, Mavundza E, Burnett R, Tanywe AC, Wiysonge CS. Factors that influence acceptance of human papillomavirus (HPV) vaccination for adolescents: a qualitative evidence synthesis. Cochrane Database Syst Rev. 2019;9. doi:10.1002/14651858.CD013430.
- Radisic G, Chapman J, Flight I, Wilson C. Factors associated with parents’ attitudes to the HPV vaccination of their adolescent sons: a systematic review. Prev Med. 2017; 95:26–37. doi:10.1016/j.ypmed.2016.11.019.
- Daley EM, Vamos CA, Thompson EL, Zimet GD, Rosberger Z, Merrell L, Kline NS. The feminization of HPV: how science, politics, economics and gender norms shaped U.S. HPV vaccine implementation. Papillomavirus Res. 2017; 3:142–48. doi:10.1016/j.pvr.2017.04.004.
- Jing R, Fang H, Wang H, Wang J. The role of general attitudes and perceptions towards vaccination on the newly-developed vaccine: results from a survey on COVID-19 vaccine acceptance in China. Front Psychol. 2022 May 31;13:841189. doi:10.3389/fpsyg.2022.841189.
- Osaghae I, Chido-Amajuoyi OG, Shete S. Healthcare provider recommendations and observed changes in HPV vaccination acceptance during the COVID-19 pandemic. Vaccines. 2022 12;10(9):1515. doi:10.3390/vaccines10091515.
- Footman A, Kanney N, Niccolai LM, Zimet GD, Overton ET, Davies SL, Van Der Pol B. Parents' acceptance of COVID-19 compared to human papillomavirus vaccines. J Adolesc Health. 2022;5:673–8. doi:10.1016/j.jadohealth.2022.07.015.
- Chen F, He Y, Shi Y. Parents’ and guardians’ willingness to vaccinate their children against COVID-19: a systematic review and meta-analysis. Vaccines (Basel). 2022 Jan 24;10(2):179. doi:10.3390/vaccines10020179.
- Montalti M, Rallo F, Guaraldi F, Bartoli L, Po G, Stillo M, Perrone P, Squillace L, Dallolio L, Pandolfi P, et al. Would parents get their children vaccinated against SARS-CoV-2? Rate and predictors of vaccine hesitancy according to a survey over 5000 families from Bologna, Italy. Vaccines (Basel). 2021 Apr 10;9(4):366. doi:10.3390/vaccines9040366.
- Teasdale CA, Borrell LN, Kimball S, Rinke ML, Rane M, Fleary SA, Nash D. Plans to vaccinate children for coronavirus disease 2019: a survey of United States parents. J Pediatr. 2021 Oct;237:292–97. doi:10.1016/j.jpeds.2021.07.021.
- Almusbah Z, Alhajji Z, Alshayeb Z, Alhabdan R, Alghafli S, Almusabah M, Almuqarrab F, Aljazeeri I, Almuhawas F. Caregivers’ willingness to vaccinate their children against COVID-19 in Saudi Arabia: a cross-sectional survey. Cureus. 2021 Aug 17;13(8):e17243. doi:10.7759/cureus.17243.