ABSTRACT
Low vaccine acceptance remains a public health threat, which is still common among healthcare workers. Therefore, the purpose of this review is to determine the level of COVID-19 vaccine acceptance among healthcare professionals in Ethiopia. This review was reported using the PRISMA checklist. Eleven articles were retrieved, then extracted on Excel, and exported to STATA version 11 software for meta-analysis. The pooled prevalence of vaccine acceptance and it is 95% CI were presented using forest plots. Tests to check heterogeneity and publication bias were done. The estimated pooled prevalence of COVID-19 vaccine acceptance among healthcare professionals in Ethiopia with a random-effects model was 54.59% (95% CI: 42.49, 66.69) through a heterogeneity index (I2) of 99.1% (p < .001), which is relatively low. Therefore, it is important to identify and remove any myths or obstacles preventing healthcare professionals from accepting the COVID-19 vaccination.
Introduction
Coronavirus disease 2019 (COVID-19) is a lethal contagious disease caused by infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which is mainly transmitted from human to human through respiratory dropletsCitation1. It is the global pandemic which was first identified in Wuhan, China, at the end of December 2019.Citation2 COVID-19 remains a worldwide challenge and it has been stated to be a global community health emergency.Citation3 Besides substantial morbidity and mortality, it also causes an extensive economic crisis around the globe.Citation4,Citation5
Now a time, several vaccines have received approval from the regulatory authorities and are being given in most countries, including Ethiopia, to end the global pandemic.Citation6 However, experts concur that mass vaccination campaigns are the best way to build up enough “herd immunity” to control the epidemic. Convincing citizens that vaccines are safe, effective, and necessary is a critical component of an effective vaccination program. Evidence suggests that front-line healthcare professionals (HCPs) COVID-19 test results have an 11-fold higher positive rate than those of the general public.Citation7 Because of this risk, the World Health Organization (WHO) advisory committee recommended that HCPs receive priority vaccination.Citation8
Vaccine acceptance is defined as “the degree to which individuals accept, question, or refuse vaccination.” It is a determinant of vaccine uptake rate, and consequently vaccine distribution success.Citation9 There is considerable evidence between vaccine acceptance among HCPs and the general public, as health professionals are trusted sources of information on public health concerns. Higher vaccination rates are attained by clients under the care of HCPs who have favorable views and acceptance of vaccinations.Citation10–13 The WHO designated vaccine hesitancy as one of the 10 threats to global health in 2019.Citation14 Surprisingly, in the era of COVID-19, the problem is significant even among healthcare workers.Citation15 A rapid systematic review of global vaccine acceptance among HCPs ranged from 28% to 73%.Citation16 If health professionals continue to be dubious of COVID-19 vaccines, they will be unable to recommend vaccines to the general public and ensure mass vaccinations with the available COVID-19 vaccines.Citation17 Lastly, they do not have a role in instilling confidence in the general population about vaccine safety and efficacy.Citation11,Citation18
In Ethiopia, low vaccine acceptance forms a major challenge to the uptake of COVID-19 vaccines.Citation19,Citation20 Reports from observational studies have shown the problem is significant even among HCPs.Citation21–24 However, no comprehensive reviews or meta-analyses of HCPs have been conducted to date. As a result, we sought to assess the HCP acceptance level of the COVID-19 vaccine in Ethiopia. The finding will allow stakeholders to create effective awareness to increase COVID-19 vaccine uptake in the country.
Methods
Search strategies
This systematic review and meta-analysis were reported using the preferred reporting items for systematic reviews and meta-analyses protocols (PRISMA) checklist guidelinesCitation18 (see S1_file). We registered the protocol into PROSPERO (ID: CRD42022332702) and searched for related papers in African journals online, PubMed, Cochrane review, HINARI, Google Scholar, and Web of Science. During this, the search was done by using the keywords such as; “COVID-19,” coronavirus disease 2019,” SARS-CoV-2,” “COVID,” “Covid-19,” “vaccine acceptance,” “vaccine hesitancy,” “vaccine refusal,” “vaccination,” “vaccine willingness,” “vaccine uptake” health care workers,” “professionals in health care,” “health-care professionals,” “healthcare workers,” “clinicians,” “health care professionals,” “health care worker,” “care providers,” “health professionals,” “health worker,” “primary care providers,” and “health care providers.” To integrate these keywords, Boolean operators “AND” and “OR” were used.
Eligibility criteria
All observational studies on COVID-19 vaccine acceptance among Ethiopian healthcare workers and papers published in English up to August 20,2022 were utilized as inclusion criteria. Publications in which the outcome variable was not clearly defined and assessed, as well as low-quality articles (see S2_file), were eliminated from this systematic review and meta-analysis.
Data extraction and quality appraisal
To organize search results and remove duplicated papers, all research collected from all databases were exported to EndNote citation manager software version X7. All studies were then exported to a Microsoft Excel spreadsheet. The search approach was used to retrieve study titles and abstracts. The studies that met the inclusion criteria through title or abstract screening were then subjected to a comprehensive full-text evaluation for eligibility and data extraction. The data were extracted by five independent authors (TM, TL, MS, AS, and TG) using a data extraction format prepared in a Microsoft Excel 2019 spreadsheet. The extracted data were as follows: the first author’s name, study year, study area, region, study design, sample size, data collection methods, response rate, and prevalence of vaccine acceptance (see S3_ file). The quality of all included articles was determined independently by five authors (TM, MS, TL, MS, and BT) by using Newcastle–Ottawa Scale (NOS) quality assessment criteria for cross-sectional studies (see S2_file). The modified NOS for cross-sectional studies was used to include articles with ≥5 out of 8 considered as a high-quality scoreCitation25 and any disagreements were resolved by discussion and consensus.
Outcome of interest
The primary outcome of this systematic review and meta-analysis was to estimate the level of COVID-19 vaccine acceptance among healthcare professionals in Ethiopia. COVID-19 vaccine acceptance among HCPs is the percentage of healthcare professionals who had intention to take the vaccine.
Statistical analysis
The extracted data on Microsoft Excel 2019 were exported to STATA version 11 software for meta-analysis. COVID-19 vaccine acceptance among HCPs in Ethiopia was pooled using a random effects model. The pooled prevalence of vaccine acceptance and it is 95% CI were presented using forest plots. For heterogeneity, inverse variance, subgroup analysis, and meta-regression were done. Inverse variance (I2) (for quantification) was used, and low, moderate, and high heterogeneity was defined as I2 test statistics of <50, 50–75%, and >75%, respectively.Citation26 Subgroup analysis was also conducted using data collection methods and region. In addition, sensitivity analysis was done to see the effect of a single study on the overall result. Lastly, a funnel plot and the Egger's regression test at P-value <.05 were used to assess publication bias.
Ethics approval and consent to participate
Not applicable. This is because the study is a systematic review and meta-analysis. None of the data was collected from the people for this study. The study was performed by reviewing the recently published articles.
Result
Study screening
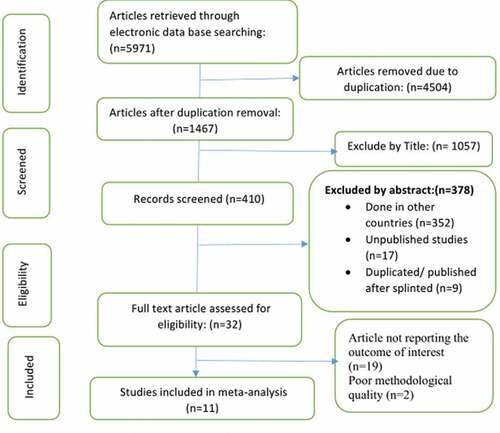
The initial literature search yielded a total of 5,971 articles through database searches such as African journals online, PubMed, Cochrane review, HINARI, Google Scholar, and Web of science. Of these, 1467 articles remained after removing duplication. After screenings of their titles and abstracts, there were 32 articles remaining whose full texts were assessed for eligibility. Finally, 11 studies were potentially eligible to undertake a systematic review (see ).
Study characteristics
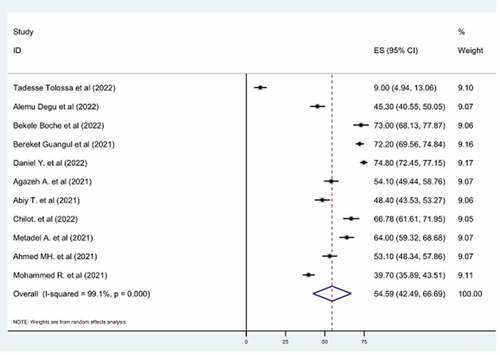
A total of 11 articles with 5,981 study participants were included in this systematic review and meta-analysis. All of the studies used are cross-sectional surveys. Six out of 11 studies were conducted in 2021 and the rest by 2022. The sample size of the included studies ranged from 191 to 1,314, with an average sample size of 544 participants. In most of the samples, the age of respondents lies between 25 and 40 years (See ). Among the included studies, COVID-19 vaccine acceptance ranged from 9% up to 74.8%.Citation21,Citation23,Citation24,Citation27–33
Table 1. Study characteristics in the studies conducted on COVID-19 vaccine acceptance among healthcare professionals in Ethiopia, 2022.
COVID-19 vaccine acceptance among healthcare professionals
From those 11 included studies, the estimated pooled prevalence of COVID-19 vaccine acceptance among healthcare professionals in Ethiopia with a random-effects model was 54.59% (95% CI: 42.49, 66.69) through a heterogeneity index (I2) of 99.1% (p < .001) ().
Heterogeneity
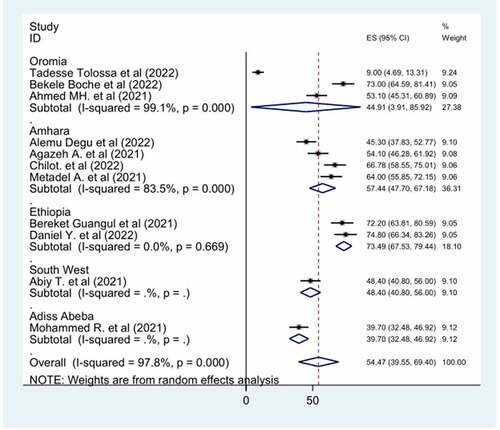
Because of the high heterogeneity observed among selected studies (I-squared = 99.1, p < .001), subgroup analysis, meta-regression, and sensitivity analysis was implemented to clarify the source of heterogeneity. Subgroup analyses were performed using the data collection method and region. It revealed a slight variation due to data collection methods. As the result showed, the highest ((66.88%; 95% CI: 57.64,76.11), I2 = 80.2%, p = .002) observed among studies that were collected by web-based self-administered questionnaire (). The subgroup analysis result by region showed that there is no significant difference across the region. Despite this, there is generally no considerable difference between subgroup heterogeneity and overall heterogeneity exhibited in subgroup analysis, indicating that the heterogeneity was not associated with study region and data collection methods ().
Figure 3. Sub-group analysis by data collection method of the pooled prevalence of COVID-19 vaccine acceptance among Ethiopian healthcare professionals, 2022.
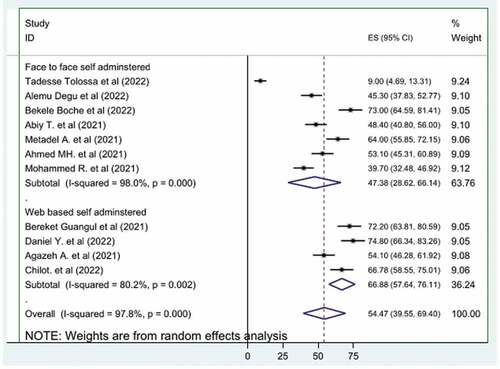
Figure 4. Sub-group analysis by region of the pooled prevalence of COVID-19 vaccine acceptance among Ethiopian healthcare professionals, 2022.
Meta-regression was conducted to identify the source of heterogeneity using sample size and study year as a covariate. The P-value of both sample size and study year is non-significant. It means there is no effect of sample size difference and study year on heterogeneity between studies. In this systematic review and meta-analysis, sensitivity analysis was done using the random-effects model for the estimates of COVID-19 vaccine acceptance. The results of the sensitivity analysis suggested that there is no influential study as none of the points are estimated outside of the overall 95% confidence interval.
Publication bias
The presence of publication bias was checked by using Egger’s test, and a graphical funnel plot. The result of Egger’s test was not significant (p = .386) (). Also, a visual inspection of the funnel plot indicated a symmetrical distribution (), suggesting the absence of publication bias for COVID-19 vaccine acceptance among healthcare professionals.
Figure 5. Funnel plot assessed for publication bias in the studies conducted on of COVID-19 vaccine acceptance among healthcare professionals in Ethiopia, 2022.
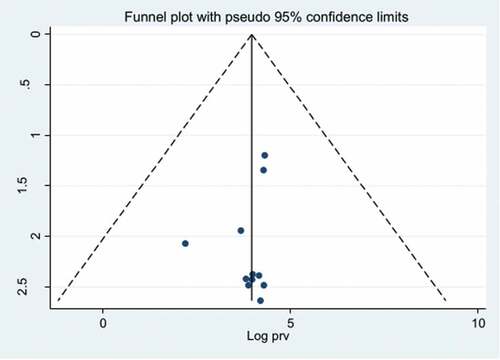
Table 2. Egger's test assessed for publication bias in the studies conducted on COVID-19 vaccine acceptance among healthcare professionals in Ethiopia, 2022.
Discussion
Although WHO and its partners are tirelessly working to distribute the COVID-19 vaccine, some countries are experiencing difficulties administering it.Citation34 The acceptance of COVID-19 vaccination by health professionals is crucial for successful virus control. Since HCPs are role models for the population and believe that they know a lot about health-related conditions. Compared to the general population, we expect a high acceptance of COVID-19 vaccine among HCPs. Therefore, they play a crucial role in instilling confidence in the general population regarding the vaccine.Citation11,Citation18 Even though people’s willingness to receive vaccinations varies greatly within and between populations, the global willingness to receive a vaccine against COVID-19 is estimated at 66.01% (95% CI 60.76–70.89% I2 = 99.40%).Citation35 The global rate of coronavirus vaccine acceptance is quite low, especially in the Middle East, Russia, Africa, and several European countries. This represents a significant opposition to global efforts to contain the current COVID-19 pandemic.Citation36 In this review, we have critically reviewed the published papers that showed the acceptance of HCPs toward the COVID-19 vaccine in Ethiopia, which is among the major challenges the world is currently facing.
The estimated pooled prevalence of COVID-19 vaccine acceptance among healthcare professionals in Ethiopia with a random-effects model is 54.59% (95% CI: 42.49, 66.69) through a heterogeneity index (I2) of 99.1% (p < .00). The finding is in line with China’s healthcare providers’ acceptance rate at early invention of the vaccineCitation37 and COVID-19 vaccine acceptance of Central African, West African, and East African healthcare professionals.Citation38 This may be due to certain common barriers to the acceptance of the vaccine that seemed to be shared by HCPs in early invention of vaccine in China, middle- and low-income countries. These included fear of side effects of vaccines; short duration of the clinical trials; issues of vaccine safety, efficacy, and effectiveness; limited information on vaccines; and lack of social trust.Citation38 But it is much lower than among healthcare professionals in Israel (78.1%), in China after the invention of their own vaccine (86.2%), and among nurses in Italy (91.5%).Citation36,Citation39,Citation40 The finding was also lower than the vaccine acceptance rate of healthcare professionals in Southern Africa which was 90% (CI: 85%–96%).Citation38 The reason for this difference may be that in China the vaccine is developed by their own professionals. This may make them develop more trust and decide to take the vaccine, whereas in Italy, Israel, and South Africa, the morbidity and mortality as a result of COVID-19 is much higher.Citation41–43 This may have its own contribution to this significant difference. However, the finding is higher than the pooled estimated COVID-19 vaccine acceptance rate of health professionals in the Democratic Republic of Congo (27.70%).Citation39
In comparison with the general population, the result is in line with a rapid systematic review and meta-analysis of COVID-19 vaccine acceptance of the general population among low- and lower-middle-income countries result, which was 58.5% (95% CI: 46.9, 69.7, I2 = 100%),Citation40 and among adults in Africa.Citation44 The result also has no difference with the vaccine acceptance level of populations of East Africa (60.2%, 95% CI: 52.8–67.3),Citation45 and with a pooled prevalence of COVID-19 vaccine acceptance among the general population of Ethiopia which was 56.02% (95% CI: 47.84, 64.20).Citation46 But the estimated value is lower than other studies of COVID-19 vaccine acceptance, most notably, among adults in Ecuador (97.0%), Malaysia (94.3%), Indonesia (93.3%), China (91.3%), and India (76.7%). This difference may be explained by low illness risk and low mortality in the country during the first two waves of the COVID-19 epidemic.Citation47 The hesitancy is mostly induced by the dissemination of misleading information through social media in Africa, specifically in Ethiopia.Citation48 Notably, low confidence in the vaccine, insufficient trust in the vaccine’s source and from the government, different conspiracy theories, religious beliefs, and possibly past vaccine hesitancy in the county are factors which are contributing to the low COVID-19 vaccination acceptance rate.Citation49–51 Lastly, it may be due to political instability in the country, Ethiopia, resulting in lower governmental concern for COVID-19 vaccination awareness creation. Even though this, the result of this study is higher than the vaccine acceptance rate among adults in Kuwait (23.6%), Jordan (28.4%),Citation36 and North Africa (37%).Citation38
Conclusion
The review shows generally low acceptance of the COVID-19 vaccine among healthcare professionals in Ethiopia. COVID-19 vaccine acceptance of HCPs acts as a valuable role model for the general public and, hence, it is very important to identify and address barriers to COVID-19 vaccine acceptance among them.
Limitation of the study
The presence of high heterogeneity between studies was the primary limitation of our meta-analysis. Even if subgroup analysis and meta-regression were used to deal with the heterogeneity, the exact source could not be determined. As a result, the interpretation of the result took these difficulties into account. Another limitation of this review was its geographic restriction to Ethiopia.
Abbreviations
| Cl | = | Confidence interval |
| COVID-19 | = | Coronavirus disease 2019 |
| HCPs | = | Healthcare professionals |
| WHO | = | World Health Organization |
Author contributions
Data curation: Tebabere Moltot, Tesfanesh Lemma. Formal analysis: Tebabere Moltot, Tesfanesh Lemma, Mulualem Silesh, Birhan Tsegaw. Investigation: Tebabere Moltot, Tesfanesh Lemma. Methodology: Tebabere Moltot, Tesfanesh Lemma, Mulualem Silesh, Birhan Tsegaw, Moges Sisay, Abayneh Shewangzaw. Software: Tebabere Moltot, Tesfanesh Lemma, Mulualem Silesh, Birhan Tsegaw, Moges Sisay, Temesgen Getaneh, Abayneh Shewangizaw. Supervision: Tebabere Moltot, Tesfanesh Lemma, Birhan Tsegaw, Temesgen Getaneh. Validation: Tebabere Moltot, Tesfanesh Lemma, Mulualem Silesh, Birhan Tsegaw, Moges Sisay, Temesgen Getaneh, Abayneh Shewangizaw. Visualization: Tebabere Moltot, Tesfanesh Lemma, Mulualem Silesh, Birhan Tsegaw, Temesgen Getaneh. Writing – original draft: Tebabere Moltot. Writing – review & editing: Tebabere Moltot and Tesfanesh Lemma
Acknowledgments
We would like to express our gratitude to all of the authors of the original articles included in this systematic review and meta-analysis.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
All relevant data are within the manuscript and its supporting information files.
Additional information
Funding
References
- Gelderblom HR. Chapter 60: Structure and classification of viruses. In: Med Microbiology. Vol. 3. 4th ed; 1996. p. 1221.
- Ayobami F, Nnorom S, Godwin O. Covid-19: the role of welfare and safety of health workers. Afr J Biol Med Res. 2020;3:60–8.
- Lotfi M, Hamblin MR, Rezaei N. COVID-19: transmission, prevention, and potential therapeutic opportunities. Clin Chim Acta. 2020;508:254–66. doi:10.1016/j.cca.2020.05.044.
- Dariya B, Nagaraju GP. Understanding novel COVID-19: its impact on organ failure and risk assessment for diabetic and cancer patients. Cytokine Growth Factor Rev. 2020;53:43–52. doi:10.1016/j.cytogfr.2020.05.001.
- Ataguba JE. COVID-19 pandemic, a war to be won: understanding its economic implications for Africa. Vol. 18. Switzerland: Springer Nature Switzerland AG; 2020. p. 325–8.
- Loembé MM, Nkengasong JN. COVID-19 vaccine access in Africa: global distribution, vaccine platforms, and challenges ahead. Immunity. 2021;54(7):1353–62. doi:10.1016/j.immuni.2021.06.017.
- Nguyen LH, Drew DA, Graham MS, Joshi AD, Guo C-G, Ma W, Mehta RS, Warner ET, Sikavi DR, Lo C-H. Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Public Health. 2020;5(9):e475–83. doi:10.1016/S2468-2667(20)30164-X.
- Shrivastava SR, Shrivastava PS. 2019-nCov outbreak declared as public health emergency of international concern: what next? Int J Prev Med. 2020;11(1):65. doi:10.4103/ijpvm.IJPVM_63_20.
- Thomson A, Robinson K, Vallée-Tourangeau G. The 5as: a practical taxonomy for the determinants of vaccine uptake. Vaccine. 2016;34(8):1018–24. doi:10.1016/j.vaccine.2015.11.065.
- Paterson P, Meurice F, Stanberry LR, Glismann S, Rosenthal SL, Larson HJ. Vaccine hesitancy and healthcare providers. Vaccine. 2016;34(52):6700–6. doi:10.1016/j.vaccine.2016.10.042.
- MacDonald NE. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161–4. doi:10.1016/j.vaccine.2015.04.036.
- Fotiadis K, Dadouli K, Avakian I, Bogogiannidou Z, Mouchtouri VA, Gogosis K, Speletas M, Koureas M, Lagoudaki E, Kokkini S. Factors associated with healthcare workers’ (HCWs) acceptance of COVID-19 vaccinations and indications of a role model towards population vaccinations from a cross-sectional survey in Greece, May 2021. Int J Environ Res Public Health. 2021;18(19):10558. doi:10.3390/ijerph181910558.
- Ulbrichtova R, Svihrova V, Tatarkova M, Hudeckova H, Svihra J. Acceptance of COVID-19 vaccination among healthcare and non-healthcare workers of hospitals and outpatient clinics in the northern region of Slovakia. Int J Environ Res Public Health. 2021;18(23):12695. doi:10.3390/ijerph182312695.
- World Health Organization. World Health Organization ten threats to global health in 2019.
- Paris C, Bénézit F, Geslin M, Polard E, Baldeyrou M, Turmel V, Tadié É, Garlantezec R, Tattevin P. COVID-19 vaccine hesitancy among healthcare workers. Infect Dis Now. 2021;51(5):484–7. doi:10.1016/j.idnow.2021.04.001.
- Ilesanmi O, Afolabi A, Uchendu O. The prospective COVID-19 vaccine: willingness to pay and perception of community members in Ibadan, Nigeria. PeerJ. 2021;9:e11153. doi:10.7717/peerj.11153.
- Biswas N, Mustapha T, Khubchandani J, Price JH. The nature and extent of COVID-19 vaccination hesitancy in healthcare workers. J Community Health. 2021;46(6):1244–51. doi:10.1007/s10900-021-00984-3.
- Wiley K, Massey P, Cooper S, Wood N, Quinn H, Leask J. Pregnant women’s intention to take up a post-partum pertussis vaccine, and their willingness to take up the vaccine while pregnant: a cross sectional survey. Vaccine. 2013;31(37):3972–8. doi:10.1016/j.vaccine.2013.06.015.
- Yehualashet DE, Seboka BT, Tesfa GA, Mamo TT, Yawo MN, Hailegebreal S. Prevalence and determinants of COVID-19 vaccine hesitancy among the Ethiopian population: a systematic review. Risk Manag Healthc Policy. 2022;15:1433. doi:10.2147/RMHP.S368057.
- Mose A, Wasie A, Shitu S, Haile K, Timerga A, Melis T, Sahle T, Zewdie A. Determinants of COVID-19 vaccine acceptance in Ethiopia: a systematic review and meta-analysis. PloS One. 2022;17(6):e0269273. doi:10.1371/journal.pone.0269273.
- Tolossa T, Fetensa G, Ayala D, Wakuma B. Health professionals’ COVID-19 vaccine acceptance and associated factors in Wollega University Referral Hospital, Western Ethiopia: a cross-sectional study. Hum Vaccines Immunother. 2022;2022(5):2069960. doi:10.1080/21645515.2022.2069960.
- Ayele AD, Ayenew NT, Tenaw LA, Kassa BG, Yehuala ED, Aychew EW, Mihretie GN, Belay HG. Acceptance of COVID-19 vaccine and associated factors among health professionals working in hospitals of South Gondar Zone, Northwest Ethiopia. Hum Vaccines Immunother. 2021;17(12):4925–33. doi:10.1080/21645515.2021.2013082.
- Boche B, Kebede O, Damessa M, Gudeta T, Wakjira D. Health professionals’ COVID-19 vaccine acceptance and associated factors in tertiary hospitals of South-West Ethiopia: a multi-center cross-sectional study. INQUIRY: J Health Care Organ Provision Financ. 2022;59:00469580221083181. doi:10.1177/00469580221083181.
- Yilma D, Mohammed R, Abdela SG, Enbiale W, Seifu F, Pareyn M, Liesenborghs L, van Griensven J, van Henten S. COVID-19 vaccine acceptability among healthcare workers in Ethiopia: do we practice what we preach? Trop Med Int Health. 2022;27(4):418–25. doi:10.1111/tmi.13742.
- Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa: Ottawa Hosp Res Inst. 2011;2:1–12.
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60. doi:10.1136/bmj.327.7414.557.
- Adane M, Ademas A, Kloos H. Knowledge, attitudes, and perceptions of COVID-19 vaccine and refusal to receive COVID-19 vaccine among healthcare workers in northeastern Ethiopia. BMC Public Health. 2022;22(1):1–14. doi:10.1186/s12889-021-12362-8.
- Aemro A, Amare NS, Shetie B, Chekol B, Wassie M. Determinants of COVID-19 vaccine hesitancy among health care workers in Amhara region referral hospitals, Northwest Ethiopia: a cross-sectional study. Epidemiol Infect. 2021;149:E225. doi:10.1017/S0950268821002259.
- Angelo AT, Alemayehu DS, Dachew AM. Health care workers intention to accept COVID-19 vaccine and associated factors in southwestern Ethiopia, 2021. PloS One. 2021;16(9):e0257109. doi:10.1371/journal.pone.0257109.
- Demeke CA, Kifle ZD, Atsbeha BW, Wondmsigegn D, Yimenu DK, Woldeyohanins AE, Kasahun AE. COVID-19 vaccine hesitancy among health professionals in a tertiary care center at the University of Gondar Specialized Hospital, Ethiopia: a cross-sectional study. SAGE Open Med. 2022;10:20503121221076991. doi:10.1177/20503121221076991.
- Guangul BA, Georgescu G, Osman M, Reece R, Derso Z, Bahiru A, Azeze ZB. Healthcare workers attitude towards SARS-COVID-2 vaccine, Ethiopia. Glob J Infect Dis Clin Res. 2021;7(1):043–048. doi:10.17352/2455-5363.000045.
- Ahmed MH, Kanfe SG, Jarso MH, Gopichandran V. Intention to receive vaccine against COVID-19 and associated factors among health professionals working at public hospitals in resource limited settings. PloS One. 2021;16(7):e0254391. doi:10.1371/journal.pone.0254391.
- Mohammed R, Nguse TM, Habte BM, Fentie AM, Gebretekle GB, Doering S. COVID-19 vaccine hesitancy among Ethiopian healthcare workers. PloS One. 2021;16(12):e0261125. doi:10.1371/journal.pone.0261125.
- Ayenigbara IO, Adegboro JS, Ayenigbara GO, Adeleke OR, Olofintuyi OO. The challenges to a successful COVID-19 vaccination programme in Africa. Germs. 2021;11(3):427. doi:10.18683/germs.2021.1280.
- Nehal KR, Steendam LM, Campos Ponce M, van der Hoeven M, Smit GSA. Worldwide vaccination willingness for COVID-19: a systematic review and meta-analysis. Vaccines. 2021;9(10):1071. doi:10.3390/vaccines9101071.
- Sallam M. COVID-19 vaccine hesitancy worldwide: a concise systematic review of vaccine acceptance rates. Vaccines. 2021;9(2):160. doi:10.3390/vaccines9020160.
- Luo C, Yang Y, Liu Y, Zheng D, Shao L, Jin J, He Q. Intention to COVID-19 vaccination and associated factors among health care workers: a systematic review and meta-analysis of cross-sectional studies. Am J Infect Control. 2021;49(10):1295–304. doi:10.1016/j.ajic.2021.06.020.
- Ackah M, Ameyaw L, Gazali Salifu M, Afi Asubonteng DP, Osei Yeboah C, Narkotey Annor E, Abena Kwartemaa Ankapong E, Boakye H, Aslam MS. COVID-19 vaccine acceptance among health care workers in Africa: a systematic review and meta-analysis. PloS One. 2022;17(5):e0268711. doi:10.1371/journal.pone.0268711.
- Shakeel CS, Mujeeb AA, Mirza MS, Chaudhry B, Khan SJ. Global COVID-19 vaccine acceptance: a systematic review of associated social and behavioral factors. Vaccines. 2022;10(1):110. doi:10.3390/vaccines10010110.
- Patwary MM, Alam MA, Bardhan M, Disha AS, Haque MZ, Billah SM, Kabir MP, Browning MH, Rahman MM, Parsa AD, et al. COVID-19 vaccine acceptance among low-and lower-middle-income countries: a rapid systematic review and meta-analysis. Vaccines. 2022;10(3):427. doi:10.3390/vaccines10030427.
- Burdorf A, Porru F, Rugulies R. The COVID-19 (coronavirus) pandemic. Scand J Work Environ Health. 2020;46(3):229–30. doi:10.5271/sjweh.3893.
- Stein-Zamir C, Abramson N, Shoob H, Libal E, Bitan M, Cardash T, Cayam R, Miskin I. A large COVID-19 outbreak in a high school 10 days after schools’ reopening, Israel, May 2020. Eurosurveillance. 2020;25(29):2001352. doi:10.2807/1560-7917.ES.2020.25.29.2001352.
- Naidu T. The COVID-19 pandemic in South Africa. Psychol Trauma: Theory Res Pract Policy. 2020;12(5):559. doi:10.1037/tra0000812.
- Wake AD. The acceptance rate toward COVID-19 vaccine in Africa: a systematic review and meta-analysis. Glob Pediatr Health. 2021;8:2333794X211048738. doi:10.1177/2333794X211048738.
- Alemayehu A, Demissie A, Yusuf M, Gemechu Lencha A, Oljira L. Covid-19 vaccine acceptance and determinant factors among general public in East Africa: a systematic review and meta-analysis. Health Serv Res Manag Epidemiol. 2022;9:23333928221106269. doi:10.1177/23333928221106269.
- Mekonnen BD, Mengistu BA. COVID-19 vaccine acceptance and its associated factors in Ethiopia: a systematic review and meta-analysis. Clin Epidemiol Glob Health. 2022;14:101001. doi:10.1016/j.cegh.2022.101001.
- Salyer SJ, Maeda J, Sembuche S, Kebede Y, Tshangela A, Moussif M, Ihekweazu C, Mayet N, Abate E, Ouma AO, et al. The first and second waves of the COVID-19 pandemic in Africa: a cross-sectional study. Lancet. 2021;397(10281):1265–75. doi:10.1016/S0140-6736(21)00632-2.
- Szmyd B, Karuga FF, Bartoszek A, Staniecka K, Siwecka N, Bartoszek A, Błaszczyk M, Radek M. Attitude and behaviors towards SARS-CoV-2 vaccination among healthcare workers: a cross-sectional study from Poland. Vaccines. 2021;9(3):218. doi:10.3390/vaccines9030218.
- Jegede AS. What led to the Nigerian boycott of the polio vaccination campaign? PLoS Med. 2007;4(3):e73. doi:10.1371/journal.pmed.0040073.
- Wonodi C, Obi-Jeff C, Adewumi F, Keluo-Udeke SC, Gur-Arie R, Krubiner C, Jaffe EF, Bamiduro T, Karron R, Faden R. Conspiracy theories and misinformation about COVID-19 in Nigeria: implications for vaccine demand generation communications. Vaccine. 2022;40(13):2114–21. doi:10.1016/j.vaccine.2022.02.005.
- Neel AH, Closser S, Villanueva C, Majumdar P, Gupta S, Krugman D, Akinyemi OO, Deressa W, Kalbarczyk A, Alonge O. 30 years of polio campaigns in Ethiopia, India and Nigeria: the impacts of campaign design on vaccine hesitancy and health worker motivation. BMJ Glob Health. 2021;6(8):e006002. doi:10.1136/bmjgh-2021-006002.