ABSTRACT
Ganglion cysts are relatively common, but intraneural ganglion cysts (INGCs) within peripheral nerves are rare and poorly understood. We present the case of a 58-year-old woman who presented with acute right-foot drop. She experienced acute knee pain radiating from the lateral leg to the dorsal foot two days after the first coronavirus disease-19 (COVID-19) vaccination (BNT162b2, Pfizer-BioNTech). She had no history of trauma or medication use. Two weeks after the onset of symptoms, she developed a dorsiflexor weakness of the right foot (Medical Research Council grade, poor). The weakness worsened to a “trace” grade despite providing conservative management for one month. Ultrasonography revealed a fusiform echolucent structure within the course of the right common peroneal nerve around the fibular head. Magnetic resonance imaging revealed multiple intraneural cysts within the right common peroneal nerve. Nerve conduction and electromyographic studies revealed multiphasic motor unit action potentials accompanied by abnormal spontaneous activities in the innervated muscles, along with axonal degeneration of the deep peroneal nerves. Surgical removal of the cyst was performed, and the patient’s symptoms gradually improved. Pathological examination revealed a cystic structure containing mucinous or gelatinous fluid and lined with flattened or cuboidal cells. The clinical course and sequential electromyographic findings relevant to this symptomatic cyst were temporally related to the vaccination date. The present case suggests that INGC-induced peroneal palsy is a possible complication after COVID-19 vaccination.
Introduction
Coronavirus disease-19 (COVID-19) vaccines have been developed and administered globally to help control the spread of the virus and protect individuals from severe illnesses. Although most people experience mild-to-no side effects, like with any medical intervention, COVID-19 vaccination can be associated with potential complications. Notably, these complications are generally rare, and the benefits of vaccination in preventing COVID-19 far outweigh the risks.
The known adverse events (AEs) associated with COVID-19 vaccination are injection site reaction, general fatigue and myalgia, allergic reactions, blood clotting, myocarditis, and pericarditis, and local neuromusculoskeletal AEs have been reported relatively rarely.Citation1 A few isolated cases of myositis, osteonecrosis, and exacerbated rheumatological conditions have been reported following COVID-19 vaccination.Citation2
Intraneural ganglion cysts (INGCs) are rare cystic lesions that occur within peripheral nerves, typically at the level of the nerve root or within nerve branches. The exact pathophysiological mechanism of INGCs is not fully understood, but several theories have been proposed, including infiltration of joint fluid into the nerve sheath through the adjacent joint capsule, herniation of outpouching articular cysts into the nerve sheath, formation of cysts directly from the epineurium or perineurium, and degenerative changes within the nerve itself (probably from the extracellular matrix).Citation3 The purpose of this article was to present a case of INGC-induced peroneal palsy that occurred after COVID-19 vaccination and to analyze the possibility of an association.
Patient presentation
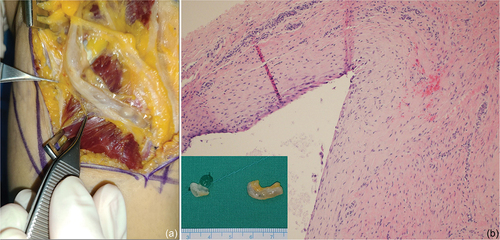
A 58-year-old previously healthy woman presented with acute right knee pain and progressively worsening right ankle dorsiflexor weakness approximately two days after receiving the first dose of COVID-19 vaccine (BNT162b2, Pfizer-BioNTech). Three weeks after the onset of symptoms, at the first visit to the outpatient clinic of our hospital, the tingling on the dorsal first web space was severe, and the foot drop was of “trace” grade on Medical Research Council grading system. She reported no signs of infection (fever, chills, myalgia, or diarrhea) before the vaccination and no history of trauma, drug allergy, or familial disease. Laboratory test results revealed elevated levels of inflammatory markers, including C-reactive protein (5.6 mg/L; (reference: <5 mg/L), and the erythrocyte sedimentation rate was 17.1 mm/h (reference: <10 mm/h). Complete blood count and blood chemistry results were normal. Tests for hepatitis, syphilis, human immunodeficiency virus, antistreptolysin O, mycoplasma, antinuclear antibody, rheumatoid factor, anti-Cyclic Citrullinated Peptide antibody, and HLA-B27 were negative. Arthrocentesis of the knee joint performed for the differential diagnosis revealed exudate (leukocyte count, 20–25/HP with 90% neutrophils, 5% lymphocytes, and 5% monocytes), negative bacterial cultures, and no visible crystals. Musculoskeletal ultrasonography revealed a moderate knee effusion and multiple lobulated cystic masses along the course of the peroneal nerve around the fibular head. The cystic mass enlarged slightly in size two weeks later. Magnetic resonance imaging revealed multiple lobulated INGCs in the common and deep peroneal nerves (). Nerve conduction and electromyographic findings revealed multiphasic motor unit action potentials accompanied by abnormal spontaneous activities in the innervated muscles along with axonal degeneration of the deep peroneal nerve. Although conservative management was performed for four weeks, the surgical method was selected because the improvement in motor function was insignificant. Intraoperatively, visually identifiable lobulated cysts that could be exposed without removing the bony structures were observed inside the neural sheath of the deep peroneal nerve. The cysts were removed. Pathological examination confirmed a ganglion cyst (). After surgical removal, the symptoms gradually improved (ankle dorsiflexor motor function: “fair” grade at three months postoperatively; “good” grade at six months postoperatively). After one year, exudation into the knee joint subsided, and normal muscle strength and gait patterns were confirmed; however, mild hypoesthesia on the dorsal first web space persisted.
Figure 1. Musculoskeletal ultrasonographic scans (a and b) and MRIs (c and d) of knee after noting a significant foot drop. (a) longitudinal scan view, lobulated feature of deep peroneal nerve (white arrows), (b) two-week follow-up scan view, slightly enlarged in size for two weeks. (HOF: head of fibula) (c) axial T2-weighted image shows about 11 cm extent of longitudinal cystic lesion (asterisk) along common peroneal nerve and articular branch with high signal intensity. T2 high signal intensity changes probably due to denervation are shown on tibialis anterior and extensor hallucis longus muscles (arrow head). (d) sagittal T2-weighted image shows cyst (asterisk) along the track of the common peroneal nerve (white arrows) around the fibular head.
Figure 2. Intraoperative findings and histological confirmation. (a) the common peroneal nerve runs around the fibular head, and a longitudinal and lobulated mass (arrowhead) is observed inside the nerve sheath. (b) Pathological examination reveals a cystic structure containing mucinous or gelatinous fluid and lined by flattened or cuboidal cells, confirming the diagnosis as a ganglion cyst. (hematoxylin and eosin stain, ×100).
Discussion
INGCs are rare, benign cysts that occur within the peripheral nerves. These cysts typically originate from nearby joint capsules or tendon sheaths and gradually expand into nerve fascicles. The exact cause of INGCs is not fully understood; however, theories suggest that they may result from a combination of joint or tendon trauma and joint instability. The cysts are filled with thick, gelatinous fluid, similar to the synovial fluid found in joints.Citation4 As they grow, they exert pressure on nerve fibers, leading to pain, weakness, tingling, and sensory changes in the affected area. The symptoms may worsen over time if left untreated.
Reports of arthritis following COVID-19 vaccination are rare. However, arthralgia is one of the most common adverse events after the vaccination. In addition, a recently published survey of 1,377 participants diagnosed with rheumatoid disease revealed that 11% of those surveyed experienced flare-ups requiring treatment after receiving the vaccines.Citation5 In another survey about the potential role of vaccines in initiating inflammatory musculoskeletal manifestations, while a definitive cause-effect relationship remained elusive, their conclusions indicated that there was a possibility of inflammatory musculoskeletal symptoms emerging in proximity to the administration of the vaccines.Citation6 It is possible that the immune response triggered by the vaccine results in temporary joint inflammation.Citation7 Few reports of arthritis following other viral vaccinations exist.Citation8–11 Additionally, case reports of reactive arthritis occurring either during or following COVID-19 infection exist.Citation12,Citation13
Among the existing literature related to this case, the concept of autoimmune/inflammatory syndrome induced by adjuvants (ASIA syndrome) has implications to consider.Citation14 ASIA syndrome refers to a group of signs and symptoms hypothesized to be triggered by exposure to various environmental factors, including certain vaccine adjuvants, silicone implants, and other substances. The proposed mechanism suggests that adjuvants, which are added to vaccines to enhance immune responses, may lead to excessive or inappropriate immune reactions in susceptible individuals. Immune dysregulation can manifest as a range of symptoms, including fatigue, myalgia (muscle pain), joint pain, cognitive difficulties, fever, and other systemic symptoms.
Although the precise relationship between acute arthritis and ganglion cyst formation is not fully understood, acute aggravated arthritis can trigger the formation or enlargement of ganglion cysts. When arthritis flares up, increased inflammation and fluid accumulation in the joint occurs. This excess fluid can seep into adjacent structures, such as tendon sheaths or joint capsules, leading to the development of ganglion cysts. The cysts appear as fluid-filled sacs and are often located near the affected joint.Citation15
Peripheral neuropathy following COVID-19 vaccination has rarely been reported. A systemic review of neurologic immune-related AEs reported a total of 32 patients who experienced facial nerve palsy, seven cases of reactivation of herpes zoster virus, four cases of Guillian-Barre syndrome, four cases of other demyelinating diseases (including multiple sclerosis, acute disseminated encephalomyelitis, and transverse myelitis), and seven cases of neuropathic conditions (including neuritis and neuralgia).Citation16 One report described clinical and electromyographic features of six patients presenting with a clinical picture of Parsonage-Turner syndrome following COVID-19 vaccination.Citation17 One patient developed bilateral retrobulbar optic neuritis after exposure to the first dose of the vaccine.Citation18 One case of an immunocompetent young male patient who suffered from ipsilateral wrist drop with multiple lymphadenopathies in the cervical and axillary regions after vaccination has been reported.Citation19
In the present case, the timing and mechanism of capsular invagination into the neural sheath have not been investigated. The symptoms and signs of acute arthritis and progressive peroneal palsy with the sequential progression of axonal degeneration are likely pathological cascades following the vaccination. This AE concerning the peripheral nerve has an etiology different from the direct immune reaction to axons/myelin or the physical effect of enlarged lymph nodes.
In summary, INGCs occurring after COVID-19 vaccination are rare and may be associated with reactive arthritis or ASIA syndrome. Critical analysis of neurological complications is crucial for treatment decisions and prognosis. Potential AEs following vaccination should be investigated to ensure the safety of COVID-19 vaccines. Continuous monitoring, research, and reporting are essential for a comprehensive understanding of the relationship between COVID-19 vaccination and peripheral neuropathy.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data supporting the findings of this study are available upon request from the corresponding author.
Additional information
Funding
References
- Beatty AL, Peyser ND, Butcher XE, Cocohoba JM, Lin F, Olgin JE, Pletcher MJ, Marcus GM. Analysis of COVID-19 vaccine type and adverse effects following vaccination. JAMA Netw Open. 2021;4:e2140364. doi:10.1001/jamanetworkopen.2021.40364. PMID: 34935921.
- Ramani SL, Samet J, Franz CK, Hsieh C, Nguyen CV, Horbinski C, Deshmukh S. Musculoskeletal involvement of COVID-19: review of imaging. Skeletal Radiol. 2021;50:1763–4. doi:10.1007/s00256-021-03734-7. PMID: 33598718.
- Desy NM, Wang H, Elshiekh MA, Tanaka S, Choi TW, Howe BM, Spinner RJ. Intraneural ganglion cysts: a systematic review and reinterpretation of the world’s literature. J Neurosurg. 2016;125(3):615–30. doi:10.3171/2015.9.JNS141368. PMID: 26799306.
- Spinner RJ, Wang H. The first described joint-associated intraneural ganglion cyst. Neurosurgery. 2011;69:1291–8. doi:10.1227/NEU.0b013e3182237299. PMID: 21566539.
- Connolly CM, Ruddy JA, Boyarsky BJ, Barbur I, Werbel WA, Geetha D, Garonzik‐Wang JM, Segev DL, Christopher‐Stine L, Paik JJ. Disease flare and reactogenicity in patients with rheumatic and musculoskeletal diseases following two‐dose SARS–CoV‐2 messenger RNA vaccination. Arthritis Rheumatol. 2022;74:28–32. doi:10.1002/art.41924. PMID: 34346185.
- Ursini F, Ruscitti P, Raimondo V, Angelis RD, Cacciapaglia F, Pigatto E, Olivo D, Di Cola I, Galluccio F, Francioso F, et al. Spectrum of short-term inflammatory musculoskeletal manifestations after COVID-19 vaccine administration: a report of 66 cases. Ann Rheum Dis. 2022;81(3):440–1. doi:10.1136/annrheumdis-2021-221587. PMID: 34836886.
- Unal Enginar A. Arthritis following COVID-19 vaccination: report of two cases. Int Immunopharmacol. 2021;101:108256. doi:10.1016/j.intimp.2021.108256. PMID: 34673298.
- Maillefert JF, Tonolli-Serabian I, Cherasse A, Demoux AL, Tavernier C, Piroth L. Arthritis following combined vaccine against diphtheria, polyomyelitis, and tetanus toxoid. Clin Exp Rheumatol. 2000;18(2):255–6. PMID: 10812502.
- Sahin N, Salli A, Enginar AU, Ugurlu H. Reactive arthritis following tetanus vaccination: a case report. Mod Rheumatol. 2009;19(2):209–11. doi:10.1007/s10165-008-0140-2. PMID: 19083078.
- Geier DA, Geier MR. A one year followup of chronic arthritis following rubella and hepatitis B vaccination based upon analysis of the vaccine adverse events reporting system (VAERS) database. Clin Exp Rheumatol. 2002;20(6):767–71. PMID: 12508767.
- Asakawa J, Kobayashi S, Kaneda K, Ogasawara H, Sugawara M, Yasuda M, Hashimoto H. Reactive arthritis after influenza vaccination: report of a case. Mod Rheumatol. 2005;15(4):283–5. doi:10.1007/s10165-005-0399-5. PMID: 17029078.
- Ono K, Kishimoto M, Shimasaki T, Uchida H, Kurai D, Deshpande GA, Komagata Y, Kaname S. Reactive arthritis after COVID-19 infection. RMD Open. 2020;6:e001350. doi:10.1136/rmdopen-2020-001350. PMID: 32763956.
- López-González MD, Peral-Garrido ML, Calabuig I, Tovar-Sugrañes E, Jovani V, Bernabeu P, García-Sevila R, León-Ramírez JM, Moreno-Perez O, Boix V, et al. Case series of acute arthritis during COVID-19 admission. Ann Rheum Dis. 2021;80:e58. doi:10.1136/annrheumdis-2020-217914. PMID: 32471899.
- Watad A, Sharif K, Shoenfeld Y. The ASIA syndrome: basic concepts. Mediterr J Rheumatol. 2017;28(2):64–9. doi:10.31138/mjr.28.2.64. PMID: 32185259.
- Khan G, Kazmi Z, Khan B, Khan N, Datta S. Ganglion cyst at the proximal tibiofibular joint - a rare cause of compression neuropathy of the peroneal nerve. Radiol Case Rep. 2021;17(1):99–102. doi:10.1016/j.radcr.2021.10.004. PMID: 34765070.
- Shafiq A, Salameh MA, Laswi I, Mohammed I, Mhaimeed O, Mhaimeed N, Mhaimeed N, Paul P, Mushannen M, Elshafeey A, et al. Neurological immune‐related adverse events after COVID‐19 vaccination: a systematic review. J Clin Pharmacol. 2022;62:291–303. doi:10.1002/jcph.2017. PMID: 34921562.
- Shields LBE, Iyer VG, Zhang YP, Burger JT, Shields CB. Parsonage-turner syndrome following COVID-19 vaccination: clinical and electromyographic findings in 6 patients. Case Rep Neurol. 2022;14:58–67. doi:10.1159/000521462. PMID: 35350287.
- Arnao V, Maimone MB, Perini V, Giudice GL, Cottone S. Bilateral optic neuritis after COVID vaccination. Neurol Sci. 2022;43:2965–6. doi:10.1007/s10072-021-05832-9. PMID: 35098359.
- Lee SM, Hong JY, Kim SY, Na SJ. Ipsilateral radial neuropathy after COVID-19 mRNA vaccination in an immunocompetent young man. Yonsei Med J. 2022;63:966–70. doi:10.3349/ymj.2022.0038. PMID: 36168250.
