ABSTRACT
Conspiracies regarding vaccines are widely prevalent, with negative consequences on health-seeking behaviors. The current study aimed to investigate the possible association between the embrace of vaccine conspiracies and the attitude to booster COVID-19, seasonal influenza, and monkeypox (mpox) vaccinations as well as the perceived side effects following COVID-19 vaccination. The target population involved academic staff and university students in health colleges in the Kingdom of Saudi Arabia. A self-administered questionnaire was distributed in January 2023 to collect data on participants’ demographics, self-reported side effects following each dose, willingness to get booster COVID-19, seasonal influenza, and mpox vaccinations, as well as an evaluation of vaccine conspiracies and attitude to mandatory vaccination. Among the 273 participants, the willingness to receive yearly booster COVID-19 vaccination was observed among 26.0% of the participants, while it was 46.9% and 34.1% for seasonal influenza and mpox vaccinations, respectively. Multinomial logistic regression analyses demonstrated a significant correlation between endorsing vaccine conspiracies and higher frequency of self-reported side effects following uptake of the second and third doses of COVID-19 vaccines. Vaccine conspiracies were also correlated with attitude toward booster COVID-19, influenza, mpox, and mandatory vaccination. The findings of this pilot study highlighted the potential adverse impact of the preexisting notions and negative attitudes toward vaccines, which could have contributed to heightened perceived side effects following COVID-19 vaccination. The study also highlighted the ongoing divisions concerning mandatory vaccination policies, emphasizing the need for cautious implementation of this strategy as a last resort for public health benefit.
Introduction
Recently, a growing interest raised to explore possible correlation between the adoption of specific medical conspiracy theories and health-seeking behaviors.Citation1–3 The research interest in medical-related conspiracies gained substantial momentum during the coronavirus disease 2019 (COVID-19) pandemic.Citation4–7 Evidence accumulated showing the association between pandemic-specific conspiracies, skepticism of the health initiatives, and negative attitudes toward recommended health practices, including the adherence to non-pharmaceutical intervention (NPI) measures.Citation8–12 Notably, vaccine hesitancy or resistance, closely linked to pandemic-related conspiracies, exemplified the detrimental impact of medical conspiracy theories on public health.Citation13–15
Exploring the correlations between endorsing conspiracy theories and negative health-seeking behaviors necessitates a comprehensive understanding of the psychological aspects of this threatening issue.Citation13,Citation16–19 Conspiracies could prevail at times of heightened anxiety, with subsequent predisposition to seek meaningful patterns and causality.Citation20,Citation21 As a result, conspiracy theories may appeal to certain individuals by offering straightforward explanations for complex health concepts.Citation1,Citation20 Consequently, embracing medical-related conspiracies could manifest in negative health behaviors, such as vaccine hesitancy or resistance and avoidance to seek professional medical advice.Citation18,Citation22,Citation23
Vaccine uptake is a type of health behavior that is primarily driven by attitude.Citation24–26 Therefore, understanding attitudes toward vaccination is a critical step to promote vaccination for the benefit of public health through effective communication.Citation27–30 Although COVID-19 cases are declining, booster vaccination appears a key strategy to prevent future waves of infection, pending further evidence to support this approach.Citation31–35 The declining immunity to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) coupled with emergence of novel virus variants with immune escape properties may require continuous vaccination with booster doses.Citation36
Vaccine hesitancy can be defined as the reluctance to get vaccinated despite the availability of vaccination services.Citation37,Citation38 During the COVID-19 pandemic, vaccine hesitancy was prominent in the Middle East countries including the Kingdom of Saudi Arabia (KSA), North Africa, Eastern Europe, and some African countries.Citation14,Citation15,Citation39–42 The correlated factors included fear of vaccine side effects, medical mistrust, complacency toward the disease risks, constraints limiting access of vaccines, and vaccine-related conspiracy beliefs.Citation43 Globally, COVID-19 conspiracies were widely reported and recently, medical-related conspiracies extended to involve other emerging infections like monkeypox (mpox).Citation3,Citation5,Citation44,Citation45
Despite the credible evidence showing the high safety and efficacy (at least over the short term) profiles of the currently approved COVID-19 vaccines, lack of vaccine confidence due to fear of adverse events remains a major factor driving COVID-19 vaccine hesitancy.Citation46–52 The commonly reported side effects following COVID-19 vaccination include pain at injection site, fever, fatigue, headache, nausea, myalgia, arthralgia, dyspnea, and diarrhea, among others.Citation53–68 The frequency and intensity of self-reported side effects following COVID-19 vaccination were variable in different studies; nevertheless, the occurrence of vaccine-related serious adverse events was reported at an extremely low rate.Citation53–71
The perception of side effects post-COVID-19 vaccination could be exaggerated among individuals embracing conspiracy theories.Citation72 The adoption of conspiracy theories may induce elevated fear and anxiety, potentially altering the subjective perception of side effects following vaccination.Citation72,Citation73 The heightened perception of COVID-19 vaccination side effects can raise individual belief in conspiracy theories, triggering a vicious cycle of negative health behavior.Citation13 Therefore, to counteract the adverse impacts of medical conspiracies, intervention measures should involve careful consideration of diverse information sources and reliance on scientific evidence for accurate dissemination of COVID-19 vaccine safety information.Citation30 Another strategy used for vaccine promotion is the implementation of vaccine mandates; however, the mandatory (compulsory) vaccination strategy remains highly controversial with ethical concerns.Citation74,Citation75 Thus, careful investigation of the attitude toward mandatory vaccination is needed for its successful implementation. It is important to emphasize that mandatory vaccination entails the requirement of vaccination for certain activities but allows exemptions (e.g., a history certain medical conditions).Citation76 Hence, while mandatory, the mandate consequences influence choice, but it does not constitute a fully compulsory policy.Citation77
Therefore, the current pilot study aimed to evaluate the attitude toward vaccination, and its association to perceived side effects following COVID-19 vaccination among a knowledgeable group comprising university students and academic staff in Saudi universities. Additionally, the study objectives included the assessment of the correlation between the attitude toward vaccination and the embrace of vaccine conspiracies and views toward mandatory vaccination.
The implication of this pilot study is elucidation of the negative impact of vaccine conspiracies manifested in heightened perceived side effects following COVID-19 vaccine uptake. Comprehensive understanding of this subject can guide targeted communication strategies to encourage informed attitudes and address concerns regarding COVID-19 vaccination side effects.Citation78–80 This aim is of particular relevance in the Arab countries of the Middle East, where COVID-19 misinformation and conspiracy theories have been widely reported.Citation81–84 Additionally, exploring attitudes toward mandatory vaccination could provide valuable insights into the sentiment toward mandates in the context of public health, helping policymakers achieve the right balance between collective benefit and individual freedom.Citation85,Citation86
Methods
Study design and ethics statement
This pilot cross-sectional survey-based study was based on a self-administered questionnaire distributed between 4 January 2023 to 25 January 2023. This study adhered to the Declaration of Helsinki guidelines and received approval from the Standing Committee for Scientific Research Ethics at King Saud University (reference No. KSU-HE-22-715, 20 December 2022). Informed consent was obtained through a mandatory agreement question in the survey: “Do you agree to participate in the current survey?”
The electronic survey (e-survey) was distributed in Arabic language without incentives for participation. The first author (S.A.) contacted the possible participants through e-mails, social media platforms, and instant messaging channels (Facebook, WhatsApp, LinkedIn, and Twitter). Pilot testing was conducted on a sample of university students (n = 6) to evaluate the survey content. Minor modifications were made based on the feedback to improve the language clarity.
The sampling approach employed was convenience-based, utilizing a snowball sampling technique. Initially, contacts of the first author (S.A.) were approached, and they were requested to distribute the survey link within their network, thus expanding the participant pool.
Since the current study aimed to investigate the possible correlation between vaccine attitude, vaccine conspiracy beliefs, and the self-reported side effects post-COVID-19 vaccination, we opted to conduct the study among academic staff and university students studying at health colleges/schools in KSA. The selection of this particular demographic stratum was based on a higher likelihood of being vaccinated against COVID-19 among these groups due to study and work mandates that urged students and academic staff to get vaccinated against COVID-19 in the country.Citation87,Citation88
Inclusion criteria included (1) age 18 years or older; (2) enrollment as a student or member of academic staff in a university in KSA; and (3) proficient reading and understanding of Arabic language. The exclusion criteria included (1) not enrolled as a student or member of academic staff in a university in KSA at the time of survey distribution; and (2) lack of proficient reading and understanding of Arabic language.
Following an introductory section that explained the study objectives and ensured full privacy and confidentiality of the participants, an informed consent was ensured from every single participant before proceeding through the e-survey by the presence of a mandatory item needed to complete the survey and clearly stating the agreement to participate.
Sample size calculation
We calculated the minimum required sample size for this pilot study based on the latest estimates of the Ministry of Education in KSA as follows: 1,383,882 students were enrolled in public and private universities and related institutions, while the number of faculty members in universities and private colleges was 75,807.Citation89 Assuming 50% as the prevalence of endorsing conspiracy beliefs regarding COVID-19 vaccination, a desired precision of ± 0.05, and confidence level of 0.90, the minimum sample size was estimated at 271 participants.Citation90
Assessment of the socio-demographic characteristics and COVID-19 variables
The next section of the e-survey assessed the following sociodemographic variables: age (as a scale variable), sex (male vs. female), occupational category (student vs. academic staff), nationality (Saudi vs. non-Saudi), educational level (undergraduate vs. postgraduate), seniority level for students (students in the first 3 years of their studies vs. students at the fourth-year level of higher), seniority level for staff (staff with less than three-year experience vs. 3–10-year experience vs. more than 10-year experience), and university sector (public vs. private).
Next, assessment of COVID-19 parameters was done as follows: history of documented COVID-19 (yes vs. no), frequency of documented COVID-19, COVID-19 vaccine uptake (yes vs. no), number of COVID-19 vaccine doses received, and the type of COVID-19 vaccine received for each dose (Pfizer-BioNTech COVID-19 vaccine vs. Oxford – AstraZeneca COVID-19 vaccine vs. others). For the participants who did not receive COVID-19 vaccination, an open question was asked to inquire regarding the reasons for vaccine non-uptake.
Attitude to booster COVID-19, seasonal influenza, mpox, and mandatory vaccinations
The assessment of the willingness to receive booster COVID-19, seasonal influenza and mpox vaccines was conducted using the following items: (1) I am willing to get a yearly booster dose of COVID-19 vaccination, (2) I am willing to get a yearly seasonal influenza vaccination, and (3) I am willing to get mpox vaccination upon its availability. The responses were based on a 5-point Likert scale as follows: agree, somewhat agree, neutral/no opinion, somewhat disagree, and disagree. Participants were then categorized into three groups: the “vaccine acceptance” group, comprising individuals who agreed or somewhat agreed to receive the vaccine; the “vaccine hesitant” group, consisting of those who answered neutrally or had no opinion; and finally, the “vaccine resistance” group, which included individuals who disagreed or somewhat disagreed with the idea of receiving the vaccine.
The assessment of mandatory COVID-19 and seasonal influenza vaccination was done using three items that comprised the Score for Mandatory Vaccination (SMV) as follows: (1) in KSA, COVID-19 and influenza vaccination should be compulsory, (2) in KSA, a financial penalty should be imposed on persons who reject vaccination such as COVID-19 and influenza vaccines, and (3) in KSA, an occupational penalty (such as denying promotions) should be imposed on persons who reject vaccination such as COVID-19 and influenza vaccines. Possible responses were based on a 5-point Likert scale that was scored as follows: agree = 1, somewhat agree = 2, neutral = 3, somewhat disagree = 4, and disagree = 5. The sum of the scores comprised the SMV, which showed an acceptable internal consistency with a Cronbach alpha value of 0.916. The SMV scores were then grouped into three categories: the “agreement” category for SMV scores below 9 denoting favorable attitude to mandatory vaccination, the “neutral attitude” category for an SMV score of 9, and the “disagreement” category for SMV scores above 9 denoting unfavorable attitude to mandatory vaccination.
Assessment of the self-reported COVID-19 vaccination side effects
For the measurement of self-reported side effects following COVID-19 vaccination, the Self-Reported Vaccination Side Effects Score (SERVASE) was conceived and employed. Each administered dose was evaluated independently using this scale. The scoring methodology was structured as follows: If an individual did not report any side effect within 7 days of receiving the dose, or if it was deemed not applicable, a score of zero was attributed to each distinct side effect. Mild side effects, defined as those lasting for a duration of one day or less, were assigned a score of 1. For more sustained side effects, persisting for a period exceeding one day, a score of 2 was assigned. The SERVASE encompassed a total of 14 listed side effects, and the sum of the scores for these side effects yielded the final SERVASE score for each participant.
The 14 side effects that were listed following comprehensive literature review includedCitation53–71 (1) pain at injection site, (2) fatigue, (3) fever, (4) headache, (5) myalgia, (6) arthralgia, (7) gastrointestinal (GI) symptoms (i.e., vomiting, diarrhea), (8) dizziness, (9) allergy, (10) respiratory symptoms, (11) diagnosed cardiovascular system (CVS) complications, (12) work absenteeism, (13) menstrual irregularities among females, and (14) hair loss.
The SERVASE score was assessed for each COVID-19 vaccine dose separately as follows: SERVASE-1 following the first dose (n = 268); SERVASE-2 following the second dose (n = 263); SERVASE-3 following the third dose (n = 213); and SERVASE-4 following the fourth dose (n = 10).
Assessment of the embrace of vaccine conspiracies
The assessment of the embrace of vaccine conspiracy beliefs was conducted using a miniaturized version of the vaccine conspiracy beliefs scale (VCBS) by Shapiro et al.Citation91 The use of this scale aimed to assess general vaccine conspiracies, rather than targeting the assessment of specific vaccine conspiracies. Three items were used as follows: (1) pharmaceutical companies cover up the dangers of vaccines, (2) people are deceived about vaccine efficacy, and (3) the international organizations try to cover up the link between vaccines and serious side effects. The possible responses were scored based on a 5-point Likert scale as follows: agree = 5, somewhat agree = 4, neutral = 3, somewhat disagree = 2, and disagree = 1. The sum formed the mini-VCBS score, which showed an acceptable internal consistency by a Cronbach alpha value of 0.891.
The mini-VCBS was then divided into three categories: the “disagreement” category for scores less than 9 denoting lower embrace of vaccine conspiracies, the “neutral attitude” category for a score of 9 on the mini-VCBS, and the “agreement” category for scores greater than 9 denoting higher embrace of vaccine conspiracies.
Statistical analysis
The statistical analysis was performed using IBM SPSS Statistics for Windows, Version 26.0. Categorical variables were analyzed using the chi-squared test, while the Mann – Whitney U test (M-W) or Kruskal – Wallis test (K-W) were employed for dichotomous or trichotomous variables compared to scale variables. The normality of scale variables was assessed using the Kolmogorov – Smirnov test (K-S). After conducting the univariate analysis, variables with a p-value less than .200 were included in multinomial logistic regression analyses. The statistical significance level was set at p < .050, indicating that results with p values below this threshold were considered statistically significant.
Results
Description of the study sample
The total number of retrieved responses was 281, of which eight respondents did not consent to participate. Thus, the final sample size comprised a total of 273 respondents divided as follows: 184 university students with a mean age of 23 ± 4.6 years (median = 22 years, interquartile range (IQR): 20–23), and 89 participants who were academic staff with a mean age of 41 ± 8.6 years (median = 40 years, IQR: 35–47). The characteristics of the study sample based on occupation are illustrated in .
Table 1. Summary description of the study sample divided by occupation (N = 273).
The vast majority of students (n = 182, 98.9%) and academic staff (n = 86, 96.6%) who participated in the study reported COVID-19 vaccine uptake of at least a single dose of COVID-19 vaccination. The majority of respondents (about three-fourths) indicated the uptake of three COVID-19 vaccine doses (). For the five participants who did not receive COVID-19 vaccination, four cited safety concerns as the reason for declining to get the vaccine, while the fifth female participants cited pregnancy/nursing as the reason for non-uptake of the vaccine.
For the different doses of COVID-19 vaccination, the majority of respondents reported the uptake of Pfizer-BioNTech COVID-19 vaccine ().
Attitude towards vaccination in the study sample
The summary of attitude toward booster COVID-19, influenza, mpox, and mandatory vaccinations is shown in .
Figure 1. Attitude of the participants towards booster COVID-19, seasonal influenza and monkeypox (mpox) vaccination and their attitude towards compulsory vaccination.
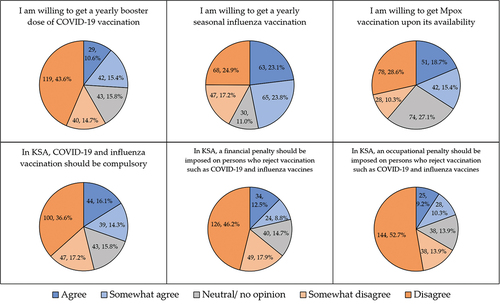
The summary of attitude toward booster COVID-19, influenza, mpox, and mandatory vaccinations is shown in .
Based on the mini-VCBS, the overall conspiratorial attitude toward vaccination in the study sample was slightly in favor of endorsing conspiracy theories (mean: 10.2 ± 3.5, 95% CI: 9.7–10.6), (median: 10.0, IQR: 8.0–13.0).
Higher resistance to seasonal influenza and mpox vaccinations was observed among older participants and among postgraduates. Additionally, higher resistance to mpox vaccination was noted among participants with a history of COVID-19. Furthermore, unfavorable attitude to mandatory vaccination was found among academic staff, postgraduates, and participants with a history of COVID-19 ().
Table 2. Attitude toward vaccination stratified by participants’ demographics.
Self-reported side effects following COVID-19 vaccination in the study sample
The summary of side effects that were self-reported per dose following COVID-19 vaccination is provided in .
Figure 2. Self-reported side effects of COVID-19 vaccines per dose.
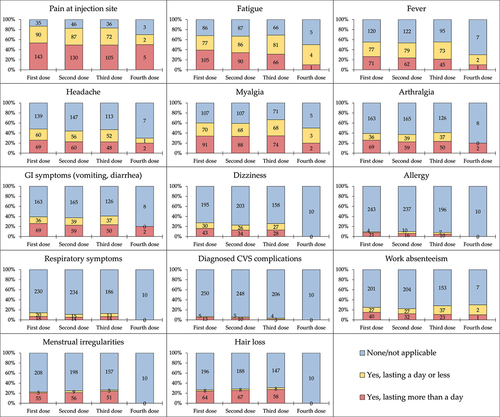
The highest mean SERVASE score was reported for the first dose (8.1, 95% confidence interval (CI): 7.3–8.9) followed by the third dose (7.8, 95% CI: 7.0–8.7), the second dose (7.6, 95% CI: 6.8–8.4) and finally the fourth dose (4.2, 95% CI: 1.5–6.9). Despite higher SERVASE scores observed among participants who received Oxford – AstraZeneca COVID-19 vaccine, this difference lacked statistical significance ().
Table 3. Summary of the self-reported COVID-19 vaccination side effects (SERVASE) scores per dose comparing different study variables.
Variables associated with lower scores of self-reported side effects following COVID-19 vaccination
In multinomial logistic regression analyses, following the first COVID-19 vaccine dose, lower scores for side effects were associated with male sex compared to females (adjusted odds ratio (OR) = 2.90, 95% CI: 1.70–4.93, p < .001) and the uptake of Pfizer-BioNTech COVID-19 vaccine compared to Oxford – AstraZeneca COVID-19 vaccine (aOR = 2.35, 95% CI: 1.20–4.61, p = .012), while higher scores were associated with being students compared to academic staff (aOR = 0.45, 95% CI: 0.25–0.81, p = .007, ).
Table 4. Variables associated with higher self-reported vaccination side effects scores (SERVASE) following COVID-19 vaccination in multinomial logistic regression analyses.
For the second COVID-19 vaccine dose, lower scores for side effects were associated with male sex compared to females (aOR = 2.91, 95% CI: 1.68–5.04, p < .001), the lower embrace of vaccine conspiracies, and the neutral attitude to vaccine conspiracies compared to higher embrace of vaccine conspiracies (aOR = 2.14, 95% CI: 1.14–4.04, and aOR = 2.64, 95% CI: 1.26–5.55, p = .019 and p = .010, respectively), and the favorable attitude to mandatory vaccination compared to unfavorable attitude to mandatory vaccination (aOR = 1.94, 95% CI: 1.02–3.68, p = .042, ).
For the third COVID-19 vaccine dose, lower scores for side effects were associated with male sex compared to females (aOR = 4.07, 95% CI: 2.12–7.79, p < .001), the neutral attitude to vaccine conspiracies compared to higher embrace of vaccine conspiracies (aOR = 4.60, 95% CI: 1.88–11.28, p = .001), and the favorable attitude to mandatory vaccination compared to unfavorable attitude to mandatory vaccination (aOR = 2.87, 95% CI: 1.31–6.27, p = .008, ).
Variables associated with acceptance of booster COVID-19, influenza, mpox, vaccination and favorable attitude to mandatory vaccination
In multinomial logistic regression analyses, and for booster COVID-19 vaccination, higher acceptance vs. vaccine resistance was associated with lower embrace of vaccine conspiracies compared to higher embrace of vaccine conspiracies (aOR = 3.78, 95% CI: 1.96–7.26, p < .001). Hesitancy to booster COVID-19 vaccination vs. vaccine resistance was associated with the lower embrace of vaccine conspiracies, and the neutral attitude to vaccine conspiracies compared to higher embrace of vaccine conspiracies (aOR = 2.85, 95% CI: 1.11–7.33, and aOR = 7.10, 95% CI: 3.05–16.55, p = .030 and p < .001, respectively, ).
Table 5. Factors associated with acceptance of yearly booster COVID-19, seasonal influenza, and mpox vaccination in multinomial logistic regression analyses.
For seasonal influenza vaccination, higher acceptance vs. vaccine resistance was associated with lower and embrace of vaccine conspiracies and the neutral attitude to vaccine conspiracies compared to higher embrace of vaccine conspiracies (aOR = 2.75, 95% CI: 1.46–5.19, and aOR = 3.28, 95% CI: 1.55–6.91, p = .002, for both comparisons). Conversely, lower seasonal influenza vaccine acceptance vs. vaccine resistance was associated with Saudi nationality compared to non-Saudi nationality ().
Hesitancy to seasonal influenza vaccine vs. vaccine resistance was associated with the neutral attitude to vaccine conspiracies compared to higher embrace of vaccine conspiracies (aOR = 6.35, 95% CI: 2.25–17.88, p < .001). Additionally, hesitancy to seasonal influenza vaccine vs. vaccine resistance was associated with the undergraduate educational level compared to postgraduate level ().
For mpox vaccination, lower acceptance was associated with a higher likelihood of having a previous history of COVID-19 compared to lack of infection history (). Hesitancy to mpox vaccination vs. vaccine resistance was associated with the lower embrace of vaccine conspiracies, and the neutral attitude to vaccine conspiracies compared to higher embrace of vaccine conspiracies (aOR = 3.18, 95% CI: 1.47–6.88, and aOR = 5.63, 95% CI: 2.52–12.57, p = .003 and p < .001, respectively, ).
Finally, respondents with a favorable attitude toward mandatory vaccination were less likely to have a history of COVID-19, while having a neutral attitude toward mandatory vaccination, as opposed to having an unfavorable attitude, was associated with having a neutral attitude to vaccine conspiracies rather than endorsing these conspiracies ().
Discussion
Previous evidence showed the harmful effects of misinformation spread and medical-related conspiracy beliefs by means of its association with negative health behaviors such as vaccination hesitancy and non-adherence to preventive measures.Citation5,Citation23,Citation44,Citation92 In this study, we demonstrated another potential harmful effect of medical-related conspiracy beliefs. Specifically, a significant correlation was observed between the self-reported post-COVID-19 side effects following the second and third COVID-19 vaccine doses and the endorsement of vaccine conspiracies. This noteworthy observation, albeit in a small sample might point to the heightened perceived risks if the vaccine uptake was achieved via coercive measures rather than promoting vaccine uptake voluntarily. Unraveling this connection was reported recently for the first time by Khouri et al. in a large sample of the French population.Citation72
In KSA, COVID-19 vaccine mandates were implemented in August 2021 requiring students and academic staff from different universities to get vaccinated against SARS-CoV-2, and these mandates were lifted in June 2022.Citation87,Citation88,Citation93 The implementation of vaccine mandates may explain the discrepancy between the rates of COVID-19 vaccine uptake which are higher than vaccine acceptance rates reported in the country.Citation14,Citation15,Citation39–42 The finding of a higher prevalence of self-reported side effects following vaccination might be linked to a greater perceived sense of side effects among the individuals who were reluctant to get vaccinated. This reluctance has been shown to be more common among individuals who hold vaccine conspiracy beliefs.Citation5,Citation43,Citation94
Regarding the frequency of side effects, our results were consistent with findings in literature as followsCitation53–72,Citation95: the most common side effect was pain at injection site which was reported among 87% of the respondents following the first dose and 83% following the second and third doses. This was followed by fatigue, myalgia, and fever which were reported among more than 50% of the participants for the first three doses. Headache and arthralgia were reported by more than a third of the participants in this study.
For the post-COVID-19 perceived side effects in a collective manner, female sex emerged as a conspicuous variable associated with higher reporting of side effects across the first three doses; a finding that is in line with results of previous studies.Citation72,Citation96 Higher prevalence of side effects following COVID-19 vaccination among females can point to genuine differences due to genetic and hormonal variations that are sex-based which could influence immune responses following vaccination.Citation97,Citation98 On the other hand, this difference could be attributed to reporting bias where females could be more likely to report side effects than males following vaccination. This pattern may appear due to psychological and societal factors, such as differences in health-seeking behavior and cultural norms regarding reporting of symptoms, which could generate a notion that females experience more side effects.Citation99,Citation100 Additionally, for the first vaccine dose, the students displayed significantly higher frequency of side effects compared to the academic staff. This can be explained by the previous evidence showing the more robust immune response among younger individuals upon vaccination, leading to a greater likelihood of experiencing side effects.Citation101–103
In addition to the assessment of COVID-19 side effects, the current study evaluated the attitude toward three different vaccines: booster COVID-19, seasonal influenza, and mpox vaccinations. The willingness to receive a yearly booster COVID-19 vaccination was expressed only by 26% of the participants who either agreed or somewhat agreed to receive such vaccination. This very low rate may be attributed to the previous uptake of the primary COVID-19 vaccination series or having a history of previous infection, which can confer complacency toward the disease risks.Citation104 On the other hand, the willingness to get influenza vaccination was higher at a rate of 47%, close to the rates observed in the recently in the Middle East in general and in KSA in particular.Citation105–108 Regarding mpox vaccination, and by taking into consideration the time of survey distribution in early 2023 for this study when mpox cases were rising globally, the willingness to take the mpox vaccine if available was expressed by 34% of the respondents. This low rate could be linked to the extremely low number of cases recorded in KSA with subsequent low level of awareness regarding this emerging infection.Citation109–111
In line with previous studies that were conducted in the Arab countries of the Middle East and North Africa, the prevalence of conspiracy beliefs regarding COVID-19 specifically and emerging virus infections in general was commonplace.Citation5,Citation43,Citation45,Citation105 In this study, the general attitude of the participants was leaning toward endorsing vaccine conspiracy beliefs despite being a knowledgeable group. Specifically, 55% of the participants either agreed or somewhat agreed with the false notion stating that pharmaceutical companies cover up the dangers of vaccines. In addition, 50% of the participants agreed with the false idea that the international organizations try to cover up the link between vaccines and serious side effects. Moreover, 26% of the participants agreed that people are deceived about vaccine efficacy. This false notion comes despite the strict regulations and guidelines for development and approval of vaccines, and it highlights the continuous need for education to fight harmful misinformation regarding vaccination.Citation112
In this study and using the multinomial logistic regression, the embrace of vaccine conspiracy beliefs was a major factor associated with attitude to vaccination and perceived side effects following COVID-19 vaccination. A possible explanation of the correlation between endorsing vaccine conspiracies and the higher frequency of perceived side effects following vaccination is as follows. It is plausible that individuals who endorse the vaccine conspiracy theories may be more likely to attribute unrelated events to the vaccine and report them as side effects in relation to heightened perception of risk.Citation113 This phenomenon can be influenced by confirmation bias, where the preexisting beliefs can play a prominent role in shaping the experience to COVID-19 vaccination.Citation114,Citation115 Thus, the endorsement of vaccine conspiracies could be an influencing factor on how individuals would interpret and report side effects following vaccination.Citation72 Consequently, the confirmation bias has the potential to influence the interpretation of normal sensations or mild side effects as indications of vaccine harm.Citation114 Furthermore, conspiracy beliefs could be associated with fear and anxiety, leading to heightened perception of side effects, while anxiety itself can be associated with physical symptoms, mistakenly attributed to the vaccine.Citation83,Citation116,Citation117 Reporting side effects could also serve as a way to justify the preexisting notions that vaccine can cause harm among individuals mandated to take the vaccine, resulting in higher reporting rates for the side effects.Citation118
Regarding the attitude to mandatory vaccination, the overall attitude of the participants was unfavorable for such a strategy. Specifically, 54% of the participants disagreed at least to some extent that COVID-19 and influenza vaccines need to be mandatory in KSA. Additionally, 64% disagreed with the idea that a financial penalty should be imposed to those who reject COVID-19 and influenza vaccination and 67% disagreed with the idea of occupational penalty. This result highlights the controversial nature of mandatory vaccination as a strategy to enforce vaccination for public health benefits which can backfire if not considered cautiously.Citation118–120
In this study, the only variables associated with attitude to mandatory vaccination were the lack of previous history of COVID-19 and the embrace of vaccine conspiracies. The observation that the absence of a previous history of COVID-19 infection was correlated with a more favorable attitude toward compulsory vaccination can be related to the following possible factors. Not experiencing COVID-19 could be the result of stricter adherence to preventive measures and reliance on information from trusted sources. Additionally, the lack of personal experience with COVID-19 could contribute to less complacency toward the disease due to lack of natural immunity from infection.Citation121 Regarding the correlation between the embrace of conspiracy beliefs and unfavorable attitude to compulsory vaccination, it is conceivable that those individuals may have higher levels of mistrust toward health authorities, medical professionals, and toward the vaccines.Citation122 Subsequently, this can result in a negative perception toward vaccination mandates.Citation123
Finally, the findings of the current study should be interpreted in light of the following limitations: (1) Participants may have inaccurately recalled their experiences, including side effects due to memory limitations, social desirability bias, or personal interpretations resulting in the self-reporting and recall biases. (2) The study sample was limited and may not be representative of the general population of university students and academic staff in KSA, resulting in sampling bias besides the possible selection bias due to the convenience approach used for sampling. The limited sample size can be related to the survey fatigue considering the timing of the study in 2023, with numerous survey studies that were conducted during COVID-19 pandemic.Citation124 Additionally, respondent fatigue could have resulted in limited sample size due to the prolonged questionnaire considering the pilot nature of the study.Citation125 (3) As a result of the cross-sectional design, the establishment of the cause-and-effect relationship between vaccine conspiracy beliefs, self-reported side effects, and attitudes towards vaccination was not possible. (4) The self-reported side effects were not clinically confirmed, which limits the ability to reach definitive conclusions regarding the correlation between vaccine conspiracy beliefs and post-COVID-19 vaccine side effects. (5) Possible measurement bias should be considered as well, based on the survey instrument used despite showing acceptable internal consistencies of the scales utilized. (6) It is important to consider the contextual differences in the policies implemented for COVID-19, influenza and mpox vaccinations, especially with regard to the vaccine mandates and rapid development of COVID-19 vaccines. This could have influenced the perception of side effects and should be considered in the interpretation of varying vaccine attitudes among the participants for the three difference vaccines. (7) In this study, each self-reported post-vaccination side effect was given an equal weight in the SERVASE score; however, it is crucial to emphasize that certain severe side effects (e.g., CVS complications, work absenteeism), may disproportionately influence vaccination attitude. (8) Finally, the target population, namely university students and academic staff in KSA further restricts the generalizability of the study findings to a broader population. Therefore, future research is recommended with refined sampling approaches and larger sample sizes to reach more robust conclusions similar to the study by Khouri et al.Citation72
To conclude, the current study demonstrated the correlation between endorsing vaccine conspiracies and the extent of self-reported side effects following COVID-19 vaccination. This finding suggests a potential harmful effect of vaccine conspiracies manifested in intensified perception of vaccination side effects in association with vaccine misconceptions. Nevertheless, this observation remains tentative pending further evidence from future studies with larger sample sizes and broader demographic representations. The current study also showed the tendency to disagree with mandatory vaccination resonating the previous divided opinion regarding this strategy which should be applied cautiously as a public health control measure aiming to reduce the burden of infectious diseases.
Author contributions
Conceptualization: Malik Sallam
Methodology: Samiyah Alshehri and Malik Sallam
Software: Malik Sallam
Validation: Samiyah Alshehri and Malik Sallam
Formal analysis: Malik Sallam
Investigation: Samiyah Alshehri and Malik Sallam
Resources: Samiyah Alshehri and Malik Sallam
Data Curation: Samiyah Alshehri and Malik Sallam
Writing – Original Draft: Malik Sallam
Writing – Review & Editing: Samiyah Alshehri and Malik Sallam
Visualization: Malik Sallam
Supervision: Malik Sallam
Project administration: Samiyah Alshehri and Malik Sallam
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data presented in this study are available on request from the corresponding author (Malik Sallam).
Additional information
Funding
References
- Leonard MJ, Philippe FL. Conspiracy theories: a Public health concern and how to address it. Front Psychol. 2021;12:682931. doi:10.3389/fpsyg.2021.682931.
- Oliver JE, Wood T. Medical conspiracy theories and health behaviors in the United States. JAMA Intern Med. 2014;174:817–15. doi:10.1001/jamainternmed.2014.190.
- Salazar-Fernández C, Baeza-Rivera MJ, Manríquez-Robles D, Salinas-Oñate N, Sallam M. From conspiracy to hesitancy: the longitudinal impact of COVID-19 vaccine conspiracy theories on perceived vaccine effectiveness. Vaccines. 2023;11(7):1150. doi:10.3390/vaccines11071150.
- van Prooijen JW, Etienne TW, Kutiyski Y, Krouwel APM. Conspiracy beliefs prospectively predict health behavior and well-being during a pandemic. Psychol Med. 2023;53:2514–21. doi:10.1017/s0033291721004438.
- Sallam M, Dababseh D, Eid H, Al-Mahzoum K, Al-Haidar A, Taim D, Yaseen A, Ababneh NA, Bakri FG, Mahafzah A, et al. High rates of COVID-19 vaccine hesitancy and its association with conspiracy beliefs: a study in Jordan and Kuwait among other Arab countries. Vaccines. 2021;9:42. doi:10.3390/vaccines9010042.
- Islam MS, Sarkar T, Khan SH, Mostofa Kamal AH, Hasan SMM, Kabir A, Yeasmin D, Islam MA, Amin Chowdhury KI, Anwar KS, et al. COVID-19–related infodemic and its impact on public health: A global social media analysis. Am J Trop Med Hyg. 2020;103:1621–9. doi:10.4269/ajtmh.20-0812.
- Bavel JJV, Baicker K, Boggio PS, Capraro V, Cichocka A, Cikara M, Crockett MJ, Crum AJ, Douglas KM, Druckman JN, et al. Using social and behavioural science to support COVID-19 pandemic response. Nat Hum Behav. 2020;4:460–71. doi:10.1038/s41562-020-0884-z.
- Earnshaw VA, Eaton LA, Kalichman SC, Brousseau NM, Hill EC, Fox AB. COVID-19 conspiracy beliefs, health behaviors, and policy support. Transl Behav Med. 2020;10:850–6. doi:10.1093/tbm/ibaa090.
- Juanchich M, Sirota M, Jolles D, Whiley LA. Are COVID-19 conspiracies a threat to public health? Psychological characteristics and health protective behaviours of believers. Eur J Soc Psychol. 2021;51:969–89. doi:10.1002/ejsp.2796.
- Pertwee E, Simas C, Larson HJ. An epidemic of uncertainty: rumors, conspiracy theories and vaccine hesitancy. Nat Med. 2022;28:456–9. doi:10.1038/s41591-022-01728-z.
- Bierwiaczonek K, Kunst JR, Pich O. Belief in COVID-19 conspiracy theories reduces social distancing over time. Appl Psychol Health Well Being. 2020;12:1270–85. doi:10.1111/aphw.12223.
- Mahmood S, Hussain T, Mahmood F, Ahmad M, Majeed A, Beg BM, Areej S. Attitude, perception, and Knowledge of COVID-19 among general Public in Pakistan. Front Public Health. 2020;8:602434. doi:10.3389/fpubh.2020.602434.
- van Mulukom V, Pummerer LJ, Alper S, Bai H, Čavojová V, Farias J, van Mulukom V, Kay CS, Lazarevic LB, Lobato EJC, et al. Antecedents and consequences of COVID-19 conspiracy beliefs: a systematic review. Social Sci Med. 2022;301:114912. doi:10.1016/j.socscimed.2022.114912.
- Sallam M, Al-Sanafi M, Sallam M. A global map of COVID-19 vaccine acceptance rates per country: an updated concise narrative review. J Multidiscip Healthc. 2022;15:21–45. doi:10.2147/jmdh.S347669.
- Sallam M. COVID-19 vaccine hesitancy worldwide: a concise systematic review of vaccine acceptance rates. Vaccines. 2021;9:160. doi:10.3390/vaccines9020160.
- Ecker UKH, Lewandowsky S, Cook J, Schmid P, Fazio LK, Brashier N, Kendeou P, Vraga EK, Amazeen MA. The psychological drivers of misinformation belief and its resistance to correction. Nat Rev Psychol. 2022;1:13–29. doi:10.1038/s44159-021-00006-y.
- Prooijen JV. Psychological benefits of believing conspiracy theories. Curr Opin Psychol. 2022;47:101352. doi:10.1016/j.copsyc.2022.101352.
- Jolley D, Douglas KM. The effects of anti-vaccine conspiracy theories on vaccination intentions. PLoS One. 2014;9:e89177. doi:10.1371/journal.pone.0089177.
- Douglas KM, Sutton RM, Cichocka A. The psychology of conspiracy theories. Curr Dir Psychol Sci. 2017;26:538–42. doi:10.1177/0963721417718261.
- van Prooijen JW, Douglas KM. Belief in conspiracy theories: basic principles of an emerging research domain. Eur J Soc Psychol. 2018;48:897–908. doi:10.1002/ejsp.2530.
- De Coninck D, Frissen T, Matthijs K, d’Haenens L, Lits G, Champagne-Poirier O, d’Haenens L, Carignan M-E, David MD, Pignard-Cheynel N, et al. Beliefs in conspiracy theories and misinformation about COVID-19: comparative perspectives on the role of anxiety, depression and exposure to and trust in information sources. Front Psychol. 2021;12:646394. doi:10.3389/fpsyg.2021.646394.
- Pavela Banai I, Banai B, Mikloušić I. Beliefs in COVID-19 conspiracy theories, compliance with the preventive measures, and trust in government medical officials. Curr Psychol. 2022;41:7448–58. doi:10.1007/s12144-021-01898-y.
- Bertin P, Nera K, Delouvée S. Conspiracy beliefs, rejection of vaccination, and support for hydroxychloroquine: a conceptual replication-extension in the COVID-19 pandemic context. Front Psychol. 2020;11:565128. doi:10.3389/fpsyg.2020.565128.
- Larson HJ, Broniatowski DA. Volatility of vaccine confidence. Science. 2021;371:1289. doi:10.1126/science.abi6488.
- Larson HJ, Gakidou E, Murray CJL. The vaccine-hesitant moment. N Engl J Med. 2022;387:58–65. doi:10.1056/NEJMra2106441.
- Enea V, Eisenbeck N, Carreno DF, Douglas KM, Sutton RM, Agostini M, Bélanger JJ, Gützkow B, Kreienkamp J, Abakoumkin G, et al. Intentions to be vaccinated against COVID-19: the role of prosociality and conspiracy beliefs across 20 countries. Health Commun. 2023;38:1530–9. doi:10.1080/10410236.2021.2018179.
- World Health Organization. Regional Office for Europe. Communicating with patients about COVID-19 vaccination: evidence-based guidance for effective conversations to promote COVID-19 vaccine uptake. [accessed 2023 Jul 1]. https://apps.who.int/iris/handle/10665/340751.
- Larson HJ, Jarrett C, Eckersberger E, Smith DM, Paterson P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007-2012. Vaccine. 2014;32:2150–9. doi:10.1016/j.vaccine.2014.01.081.
- Dubé E, Gagnon D, Vivion M. Optimizing communication material to address vaccine hesitancy. Can Commun Dis Rep. 2020;46:48–52. doi:10.14745/ccdr.v46i23a05.
- Lewandowsky S, Cook J, Schmid P, Holford DL, Finn A, Leask J, Thomson A, Lombardi D, Al-Rawi AK, Amazeen MA, et al. The COVID-19 vaccine communication handbook. A practical guide for improving vaccine communication and fighting misinformation. 2021.
- Wise J. Covid-19: WHO declares end of global health emergency. BMJ. 2023;381:1041. doi:10.1136/bmj.p1041.
- Mahase E. Covid-19: JCVI recommends autumn vaccine booster for the most vulnerable. BMJ. 2023;380:204. doi:10.1136/bmj.p204.
- Mahase E. Covid-19: annual flu-like booster approach may not be appropriate, says expert on infectious disease. BMJ. 2023;380:196. doi:10.1136/bmj.p196.
- Betsch C, Schmid P, Verger P, Lewandowsky S, Soveri A, Hertwig R, Fasce A, Holford D, De Raeve P, Gagneur A, et al. A call for immediate action to increase COVID-19 vaccination uptake to prepare for the third pandemic winter. Nat Commun. 2022;13:7511. doi:10.1038/s41467-022-34995-y.
- Silk BJ, Scobie HM, Duck WM, Palmer T, Ahmad FB, Binder AM, Cisewski JA, Kroop S, Soetebier K, Park M, et al. COVID-19 surveillance after expiration of the public health emergency declaration ― United States, May 11, 2023. Morb Mortal Wkly Rep. 2023;72:523–8. doi:10.15585/mmwr.mm7219e1.
- Chi W-Y, Li Y-D, Huang H-C, Chan TEH, Chow S-Y, Su J-H, Ferrall L, Hung C-F, Wu T-C. COVID-19 vaccine update: vaccine effectiveness, SARS-CoV-2 variants, boosters, adverse effects, and immune correlates of protection. J Biomed Sci. 2022;29:82. doi:10.1186/s12929-022-00853-8.
- Peretti-Watel P, Larson HJ, Ward JK, Schulz WS, Verger P. Vaccine hesitancy: clarifying a theoretical framework for an ambiguous notion. PLoS Curr. 2015;7. doi:10.1371/currents.outbreaks.6844c80ff9f5b273f34c91f71b7fc289.
- MacDonald NE. Vaccine hesitancy: Definition, scope and determinants. Vaccine. 2015;33:4161–4. doi:10.1016/j.vaccine.2015.04.036.
- Almeshari M, Abanomy A, Alzamil Y, Alyahyawi A, Al-Thomali AW, Alshihri AA, Althomali OW. Public acceptance of COVID-19 vaccination among residents of Saudi Arabia: a cross-sectional online study. BMJ Open. 2022;12:e058180. doi:10.1136/bmjopen-2021-058180.
- El Hassan ELW, Abu Alhommos AK, Aliadhy D, Alsalman S, Alnafaa O, Public Knowledge MA. Beliefs and attitudes toward the COVID-19 vaccine in Saudi Arabia: a cross-sectional study. Healthcare (Basel). 2022;10(5):853. doi:10.3390/healthcare10050853.
- Al Naam YA, Elsafi SH, Alkharraz ZS, Almaqati TN, Alomar AM, Al Balawi IA, Jebakumar AZ, Ghazwani AA, Almusabi SS, Albusaili S, et al. Factors related to COVID-19 vaccine hesitancy in Saudi Arabia. Public Health Pract (Oxf). 2022;3:100258. doi:10.1016/j.puhip.2022.100258.
- Alfageeh EI, Alshareef N, Angawi K, Alhazmi F, Chirwa GC. Acceptability of a COVID-19 Vaccine among the Saudi Population. Vaccines (Basel). 2021;9:226. doi:10.3390/vaccines9030226.
- Al-Sanafi M, Sallam M. Psychological determinants of COVID-19 vaccine acceptance among healthcare workers in Kuwait: a cross-sectional study using the 5C and vaccine conspiracy beliefs scales. Vaccines. 2021;9:701. doi:10.3390/vaccines9070701.
- Freeman D, Waite F, Rosebrock L, Petit A, Causier C, East A, Jenner L, Teale A-L, Carr L, Mulhall S, et al. Coronavirus conspiracy beliefs, mistrust, and compliance with government guidelines in England. Psychol Med. 2022;52:251–63. doi:10.1017/s0033291720001890.
- Sallam M, Eid H, Awamleh N, Al-Tammemi AB, Barakat M, Athamneh RY, Hallit S, Harapan H, Mahafzah A. Conspiratorial attitude of the general Public in Jordan towards emerging virus infections: a cross-sectional study amid the 2022 monkeypox outbreak. Trop Med Infect Dis. 2022;7:411. doi:10.3390/tropicalmed7120411.
- Lazarus JV, Wyka K, White TM, Picchio CA, Rabin K, Ratzan SC, Parsons Leigh J, Hu J, El-Mohandes A. Revisiting COVID-19 vaccine hesitancy around the world using data from 23 countries in 2021. Nat Commun. 2022;13:3801. doi:10.1038/s41467-022-31441-x.
- Chutiyami M, Salihu D, Bello UM, Winser SJ, Gambo AA, Sabo H, Kolo AM, Jalo HA, Muhammad AS, Mahmud FA, et al. Are fear of COVID-19 and vaccine hesitancy associated with COVID-19 vaccine uptake? A population-based online survey in Nigeria. Vaccines. 2022;10:1271. doi:10.3390/vaccines10081271.
- Wu N, Joyal-Desmarais K, Ribeiro PAB, Vieira AM, Stojanovic J, Sanuade C, Yip D, Bacon SL. Long-term effectiveness of COVID-19 vaccines against infections, hospitalisations, and mortality in adults: findings from a rapid living systematic evidence synthesis and meta-analysis up to December, 2022. Lancet Respir Med. 2023;11:439–52. doi:10.1016/s2213-2600(23)00015-2.
- Zheng C, Shao W, Chen X, Zhang B, Wang G, Zhang W. Real-world effectiveness of COVID-19 vaccines: a literature review and meta-analysis. Int J Infect Dis. 2022;114:252–60. doi:10.1016/j.ijid.2021.11.009.
- Liu Q, Qin C, Liu M, Liu J. Effectiveness and safety of SARS-CoV-2 vaccine in real-world studies: a systematic review and meta-analysis. Infect Dis Poverty. 2021;10:132. doi:10.1186/s40249-021-00915-3.
- Polack FP, Thomas SJ, Kitchin N, Absalon J, Gurtman A, Lockhart S, Perez JL, Pérez Marc G, Moreira ED, Zerbini C, et al. Safety and efficacy of the BNT162b2 mRNA COVID-19 vaccine. N Engl J Med. 2020;383:2603–15. doi:10.1056/NEJMoa2034577.
- Tregoning JS, Flight KE, Higham SL, Wang Z, Pierce BF. Progress of the COVID-19 vaccine effort: viruses, vaccines and variants versus efficacy, effectiveness and escape. Nat Rev Immunol. 2021;21:626–36. doi:10.1038/s41577-021-00592-1.
- Dhamanti I, Suwantika AA, Adlia A, Yamani LN, Yakub F. Adverse reactions of COVID-19 vaccines: a scoping review of observational studies. Int J Gen Med. 2023;16:609–18. doi:10.2147/ijgm.S400458.
- Pormohammad A, Zarei M, Ghorbani S, Mohammadi M, Razizadeh MH, Turner DL, Turner RJ. Efficacy and safety of COVID-19 vaccines: a systematic review and meta-analysis of randomized clinical trials. Vaccines. 2021;9:467. doi:10.3390/vaccines9050467.
- Beatty AL, Peyser ND, Butcher XE, Cocohoba JM, Lin F, Olgin JE, Pletcher MJ, Marcus GM. Analysis of COVID-19 vaccine type and adverse effects following vaccination. JAMA Netw Open. 2021;4:e2140364. doi:10.1001/jamanetworkopen.2021.40364.
- Kouhpayeh H, Ansari H. Adverse events following COVID-19 vaccination: a systematic review and meta-analysis. Int Immunopharmacol. 2022;109:108906. doi:10.1016/j.intimp.2022.108906.
- Majumder MAA, Singh K, Johnson WMS, Rajasundaram A, Gupta S, Gaur U, Kumar S, Chatterjee M, Fazle Rabbi AM, Sangishetti VP, et al. Evaluation of short-term side effects following the first dose of COVID-19 vaccines among physicians and dentists: a cross-sectional study from India. J Multidiscip Healthc. 2023;16:161–74. doi:10.2147/jmdh.S390364.
- Krause PR, Gruber MF. Emergency use authorization of Covid vaccines - safety and efficacy follow-up considerations. N Engl J Med. 2020;383:e107. doi:10.1056/NEJMp2031373.
- Santi Laurini G, Montanaro N, Broccoli M, Bonaldo G, Motola D. Real-life safety profile of mRNA vaccines for COVID-19: an analysis of VAERS database. Vaccine. 2023;41:2879–86. doi:10.1016/j.vaccine.2023.03.054.
- Xu K, Wang Z, Qin M, Gao Y, Luo N, Xie W, Zou Y, Wang J, Ma X. A systematic review and meta-analysis of the effectiveness and safety of COVID-19 vaccination in older adults. Front Immunol. 2023;14:1113156. doi:10.3389/fimmu.2023.1113156.
- Dagan N, Barda N, Kepten E, Miron O, Perchik S, Katz MA, Hernán MA, Lipsitch M, Reis B, Balicer RD, et al. BNT162b2 mRNA COVID-19 vaccine in a nationwide mass vaccination setting. N Engl J Med. 2021;384:1412–23. doi:10.1056/NEJMoa2101765.
- Baden LR, El Sahly HM, Essink B, Kotloff K, Frey S, Novak R, Diemert D, Spector SA, Rouphael N, Creech CB, et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N Engl J Med. 2021;384:403–16. doi:10.1056/NEJMoa2035389.
- Al Kaabi N, Zhang Y, Xia S, Yang Y, Al Qahtani MM, Abdulrazzaq N, Al Nusair M, Hassany M, Jawad JS, Abdalla J, et al. Effect of 2 inactivated SARS-CoV-2 vaccines on symptomatic COVID-19 infection in adults: a randomized clinical trial. Jama. 2021;326:35–45. doi:10.1001/jama.2021.8565.
- Francis AI, Ghany S, Gilkes T, Umakanthan S. Review of COVID-19 vaccine subtypes, efficacy and geographical distributions. Postgrad Med J. 2022;98:389–94. doi:10.1136/postgradmedj-2021-140654.
- Ripabelli G, Sammarco ML, D’Amico A, De Dona R, Iafigliola M, Parente A, Samprati N, Santagata A, Adesso C, Natale A, et al. Safety of mRNA BNT162b2 COVID-19 (Pfizer-BioNtech) vaccine in children aged 5–11 years: results from an active pharmacovigilance study in central Italy. Hum Vaccin Immunother. 2022;18:2126668. doi:10.1080/21645515.2022.2126668.
- Gee J, Marquez P, Su J, Calvert GM, Liu R, Myers T, Nair N, Martin S, Clark T, Markowitz L, et al. First Month of COVID-19 vaccine safety monitoring — United States, December 14, 2020–January 13, 2021. MMWR Morb Mortal Wkly Rep. 2021;70:283–8. doi:10.15585/mmwr.mm7008e3.
- Woo EJ, Gee J, Marquez P, Baggs J, Abara WE, McNeil MM, Dimova RB, Su JR. Post-authorization safety surveillance of Ad.26.COV2.S vaccine: reports to the vaccine adverse Event reporting System and v-safe, February 2021–February 2022. Vaccine. 2023;41:4422–30. doi:10.1016/j.vaccine.2023.06.023.
- Bürzle O, Menges D, Maier JD, Schams D, Puhan MA, Fehr J, Ballouz T, Frei A. Adverse effects, perceptions and attitudes related to BNT162b2, mRNA-1273 or JNJ-78436735 SARS-CoV-2 vaccines: population-based cohort. NPJ Vaccines. 2023;8:61. doi:10.1038/s41541-023-00657-3.
- Torp Hansen K, Kusk Povlsen F, Hammer Bech B, Nygaard Hansen S, Ulrikka Rask C, Fink P, Jørgensen T, Nielsen H, Meinertz Dantoft T, Marie Thysen S, et al. Immediate adverse reactions following COVID-19 vaccination among 16–65-year-old Danish citizens. Vaccine. 2023;41:4879–87. doi:10.1016/j.vaccine.2023.06.069.
- Dziedzic A, Riad A, Attia S, Klugar M, Tanasiewicz M. Self-reported adverse events of COVID-19 vaccines in polish healthcare workers and medical students. Cross-sectional study and pooled analysis of CoVaST project results in central Europe. J Clin Med. 2021;10:5338. doi:10.3390/jcm10225338.
- Wu Q, Dudley MZ, Chen X, Bai X, Dong K, Zhuang T, Salmon D, Yu H. Evaluation of the safety profile of COVID-19 vaccines: a rapid review. BMC Med. 2021;19:173. doi:10.1186/s12916-021-02059-5.
- Khouri C, Larabi A, Verger P, Gauna F, Cracowski JL, Ward J. Impact of vaccine hesitancy on onset, severity and type of self-reported adverse events: a French cross-sectional survey. Drug Saf. 2022;45:1049–56. doi:10.1007/s40264-022-01220-0.
- van Prooijen J-W. An existential threat Model of conspiracy theories. Eur Psychol. 2019;25:16–25. doi:10.1027/1016-9040/a000381.
- Julian S. Good reasons to vaccinate: mandatory or payment for risk? J Med Ethics. 2021;47:78. doi:10.1136/medethics-2020-106821.
- Giubilini A, Vaccination SJ. Risks, and freedom: the seat belt analogy. Public Health Ethics. 2019;12:237–49. doi:10.1093/phe/phz014.
- Saunders B. How mandatory can we make vaccination? Public Health Ethics. 2022;15:220–32. doi:10.1093/phe/phac026.
- World Health Organization. COVID-19 and mandatory vaccination: ethical considerations. [accessed 2023 Oct 2]. https://www.who.int/publications/i/item/WHO-2019-nCoV-Policy-brief-Mandatory-vaccination-2022.1.
- Alderotti G, Corvo MF, Buscemi P, Stacchini L, Giorgetti D, Lorini C, Bonaccorsi G, Pinilla MJC, Lastrucci V. Communicating with patients about COVID-19 vaccination: a qualitative study on vaccinators in Tuscany Region, Italy. Vaccines. 2023;11:223. doi:10.3390/vaccines11020223.
- Hong S-A. COVID-19 vaccine communication and advocacy strategy: a social marketing campaign for increasing COVID-19 vaccine uptake in South Korea. Humanit Soc Sci Commun. 2023;10:109. doi:10.1057/s41599-023-01593-2.
- Motta M, Sylvester S, Callaghan T, Lunz-Trujillo K. Encouraging COVID-19 vaccine uptake through effective health communication. Front Polit Sci. 2021;3:630133. doi:10.3389/fpos.2021.630133.
- Al-Rawi A, Fakida A, Grounds K. Investigation of COVID-19 misinformation in Arabic on Twitter: content analysis. JMIR Infodemiol. 2022;2:e37007. doi:10.2196/37007.
- Sauerland J. Covid-19, Conspiracy narratives, and the Arab State. In: Butter M, Knight P, editors. Covid conspiracy theories in global perspective. London: Routledge; 2023. p. 15.
- Sallam M, Dababseh D, Yaseen A, Al-Haidar A, Ababneh NA, Bakri FG, Mahafzah A. Conspiracy beliefs are associated with lower Knowledge and higher anxiety levels regarding COVID-19 among students at the university of Jordan. Int J Environ Res Public Health. 2020;17:4915. doi:10.3390/ijerph17144915.
- Alasmari A, Addawood A, Nouh M, Rayes W, Al-Wabil A. A retrospective analysis of the COVID-19 infodemic in Saudi Arabia. Future Internet. 2021;13:254. doi:10.3390/fi13100254.
- Paul KT, Eberl JM, Partheymüller J. Policy-relevant attitudes toward COVID-19 vaccination: associations with demography, health risk, and social and political factors. Front Public Health. 2021;9:671896. doi:10.3389/fpubh.2021.671896.
- Bardosh K, de Figueiredo A, Gur-Arie R, Jamrozik E, Doidge J, Lemmens T, Keshavjee S, Graham JE, Baral S. The unintended consequences of COVID-19 vaccine policy: why mandates, passports and restrictions may cause more harm than good. BMJ Glob Health. 2022;7:e008684. doi:10.1136/bmjgh-2022-008684.
- The Saudi Ministry of Education. The Ministry of education urges all its employees and intermediate and secondary school students to get two doses of the COVID-19 vaccine. [accessed 2023 Jul 3]. https://www.moe.gov.sa/en/mediacenter/MOEnews/Pages/s-2021-274.aspx.
- Alammari D, Al-Kadri H, Al-Qurashi M, Alshamrani M, Farahat F, Altamimi A, Najjar A. Lessons learned from an academic institution for improving COVID-19 vaccine uptake in Saudi Arabia. East Mediterr Health J. 2023;29:580–6. doi:10.26719/emhj.23.034.
- The Saudi Ministry of Education. Higher Education. [accessed 2023 Jul 3]. https://icee.sa/about-the-ministry/ministry-of-education/index.html.
- Alammari D, Al-Kadri H, Al-Qurashi M, Alshamrani M, Farahat F, Altamimi A. Sample size to estimate a proportion or apparent prevalence with specified precision. [accessed 2023 Jul 3]. https://epitools.ausvet.com.au/oneproportion.
- Shapiro GK, Holding A, Perez S, Amsel R, Rosberger Z. Validation of the vaccine conspiracy beliefs scale. Papillomavirus Res. 2016;2:167–72. doi:10.1016/j.pvr.2016.09.001.
- Caceres MMF, Sosa JP, Lawrence JA, Sestacovschi C, Tidd-Johnson A, Rasool MHU, Gadamidi VK, Ozair S, Pandav K, Cuevas-Lou C, et al. The impact of misinformation on the COVID-19 pandemic. AIMS Public Health. 2022;9:262–77. doi:10.3934/publichealth.2022018.
- The Saudi Ministry of Health. Saudi Arabia Lifts COVID-19 Precautionary Measures. [accessed 2023 Oct 3]. https://www.moh.gov.sa/en/Ministry/MediaCenter/News/Pages/News-2022-06-16-001.aspx.
- Yıldırım DF, Serçekuş P, Özkan S. Reasons for individuals’ COVID-19 vaccine hesitations and changing decisions over time: a longitudinal qualitative study. Vacunas. 2022;23:S1–s7. doi:10.1016/j.vacun.2022.06.006.
- Alhossan A, Alsaran AK, Almahmudi AH, Aljohani ZS, Albishi MR, Almutairi AK. Adverse events of COVID-19 vaccination among the Saudi population: a systematic review and meta-analysis. Vaccines. 2022;10:2089. doi:10.3390/vaccines10122089.
- Ahlam A, Alnada I, Rhagda A, Mercy J, Ghaida A, Aljohara A. A cross-sectional survey of side effects after COVID-19 vaccination in Saudi Arabia: male versus female outcomes . J Adv Pharm Educ Res. 2021;11:51–6. doi:10.51847/bCwca2qGfP.
- Klein SL, Flanagan KL. Sex differences in immune responses. Nat Rev Immunol. 2016;16:626–38. doi:10.1038/nri.2016.90.
- Xiong X, Yuan J, Li M, Jiang B, Lu ZK. Age and gender disparities in adverse events following COVID-19 vaccination: real-world evidence based on big data for risk management. Front Med. 2021;8:700014. doi:10.3389/fmed.2021.700014.
- Al-Qazaz HK, Al-Obaidy LM, Attash HM. COVID-19 vaccination, do women suffer from more side effects than men? A retrospective cross-sectional study. Pharm Pract (Granada). 2022;20:2678. doi:10.18549/PharmPract.2022.2.2678.
- Green MS, Peer V, Magid A, Hagani N, Anis E, Nitzan D. Gender differences in adverse events following the Pfizer-BioNTech COVID-19 vaccine. Vaccines. 2022;10:233. doi:10.3390/vaccines10020233.
- Di Resta C, Ferrari D, Viganò M, Moro M, Sabetta E, Minerva M, Ambrosio A, Locatelli M, Tomaiuolo R. The gender impact assessment among healthcare workers in the SARS-CoV-2 vaccination—an analysis of serological response and side effects. Vaccines. 2021;9:522. doi:10.3390/vaccines9050522.
- Izumo T, Kuse N, Awano N, Tone M, Sakamoto K, Takada K, Muto Y, Fujimoto K, Saiki A, Ito Y, et al. Side effects and antibody titer transition of the BNT162b2 messenger ribonucleic acid coronavirus disease 2019 vaccine in Japan. Respir Investig. 2021;59:635–42. doi:10.1016/j.resinv.2021.06.003.
- Derhovanessian E, Pawelec G. Vaccination in the elderly. Microb Biotechnol. 2012;5:226–32. doi:10.1111/j.1751-7915.2011.00283.x.
- Kwok KO, Li KK, Tang A, Tsoi MTF, Chan EYY, Tang JWT, Wong A, Wei WI, Wong SYS. Psychobehavioral responses and likelihood of receiving COVID-19 vaccines during the pandemic, Hong Kong. Emerg Infect Dis. 2021;27:1802–10. doi:10.3201/eid2707.210054.
- Sallam M, Ghazy RM, Al-Salahat K, Al-Mahzoum K, AlHadidi NM, Eid H, Kareem N, Al-Ajlouni E, Batarseh R, Ababneh NA, et al. The role of psychological factors and vaccine conspiracy beliefs in influenza vaccine hesitancy and uptake among Jordanian healthcare workers during the COVID-19 pandemic. Vaccines. 2022;10:1355. doi:10.3390/vaccines10081355.
- Aljamili AA. Knowledge and practice toward seasonal influenza vaccine and its barriers at the community level in Riyadh, Saudi Arabia. J Family Med Prim Care. 2020;9:1331–9. doi:10.4103/jfmpc.jfmpc_1011_19.
- Sales IA, Syed W, Almutairi MF, Al Ruthia Y. Public knowledge, attitudes, and practices toward seasonal influenza vaccine in Saudi Arabia: a cross-sectional study. Int J Environ Res Public Health. 2021;18:479. doi:10.3390/ijerph18020479.
- Alshahrani SM, Zahrani Y. Prevalence and predictors of seasonal influenza vaccine uptake in Saudi Arabia post COVID-19: a web-based online cross-sectional study. Vaccines (Basel). 2023;11:353. doi:10.3390/vaccines11020353.
- Mahameed H, Al-Mahzoum K, AlRaie LA, Aburumman R, Al-Naimat H, Alhiary S, Barakat M, Al-Tammemi AB, Salim NA, Sallam M, et al. Previous vaccination history and psychological factors as significant predictors of willingness to receive mpox vaccination and a favorable attitude towards compulsory vaccination. Vaccines. 2023;11:897. doi:10.3390/vaccines11050897.
- Meo SA, Al-Khlaiwi T, Aljofan ZF, Alanazi AI, Meo AS. Public perceptions of the emerging Human monkeypox disease and vaccination in Riyadh, Saudi Arabia: a cross-sectional study. Vaccines (Basel). 2022;10:1534. doi:10.3390/vaccines10091534.
- Alshahrani NZ, Alzahrani F, Alarifi AM, Algethami MR, Alhumam MN, Ayied HAM, Awan AZ, Almutairi AF, Bamakhrama SA, Almushari BS, et al. Assessment of Knowledge of monkeypox Viral infection among the general population in Saudi Arabia. Pathogens. 2022;11:904. doi:10.3390/pathogens11080904.
- Marco-Franco JE, Pita-Barros P, Vivas-Orts D, González-de-Julián S, Vivas-Consuelo D. COVID-19, fake news, and vaccines: should regulation be implemented? Int J Environ Res Public Health. 2021;18(2):744. doi:10.3390/ijerph18020744.
- Colautti L, Cancer A, Magenes S, Antonietti A, Iannello P. Risk-perception change associated with COVID-19 vaccine’s side effects: the role of individual differences. Int J Environ Res Public Health. 2022;19(3):1189. doi:10.3390/ijerph19031189.
- Malthouse E. Confirmation bias and vaccine-related beliefs in the time of COVID-19. J Public Health (Oxf). 2023;45:523–8. doi:10.1093/pubmed/fdac128.
- Acar K, Horntvedt O, Cabrera A, Olsson A, Ingvar M, Lebedev AV, Petrovic P. COVID-19 conspiracy ideation is associated with the delusion proneness trait and resistance to update of beliefs. Sci Rep. 2022;12:10352. doi:10.1038/s41598-022-14071-7.
- Hause AM, Gee J, Johnson T, Jazwa A, Marquez P, Miller E, Su J, Shimabukuro TT, Shay DK. Anxiety-related adverse event clusters after Janssen COVID-19 vaccination — five U.S. Mass vaccination sites, April 2021. MMWR Morb Mortal Wkly Rep. 2021;70:685–8. doi:10.15585/mmwr.mm7018e3.
- Šrol J, Ballová Mikušková E, Čavojová V. When we are worried, what are we thinking? Anxiety, lack of control, and conspiracy beliefs amidst the COVID-19 pandemic. Appl Cogn Psychol. 2021;35:720–9. doi:10.1002/acp.3798.
- Kevin B, Alex de F, Rachel G-A, Euzebiusz J, James D, Trudo L, Keshavjee S, Graham JE, Baral S. The unintended consequences of COVID-19 vaccine policy: why mandates, passports and restrictions may cause more harm than good. BMJ Glob Health. 2022;7:e008684. doi:10.1136/bmjgh-2022-008684.
- Mello MM, Opel DJ, Benjamin RM, Callaghan T, DiResta R, Elharake JA, Flowers LC, Galvani AP, Salmon DA, Schwartz JL, et al. Effectiveness of vaccination mandates in improving uptake of COVID-19 vaccines in the USA. Lancet. 2022;400:535–8. doi:10.1016/s0140-6736(22)00875-3.
- Olick RS, Shaw J, Yang YT. Ethical issues in mandating COVID-19 vaccination for health care personnel. Mayo Clin Proc. 2021;96:2958–62. doi:10.1016/j.mayocp.2021.10.020.
- Horton R. Offline: complacency threatens progress against COVID-19. Lancet. 2022;399:615. doi:10.1016/S0140-6736(22)00266-5.
- Van Oost P, Yzerbyt V, Schmitz M, Vansteenkiste M, Luminet O, Morbée S, Van den Bergh O, Waterschoot J, Klein O. The relation between conspiracism, government trust, and COVID-19 vaccination intentions: the key role of motivation. Social Sci Med. 2022;301:114926. doi:10.1016/j.socscimed.2022.114926.
- Lewandowsky S, Holford D, Schmid P. Public policy and conspiracies: the case of mandates. Curr Opin Psychol. 2022;47:101427. doi:10.1016/j.copsyc.2022.101427.
- de Koning R, Egiz A, Kotecha J, Ciuculete AC, Ooi SZY, Bankole NDA, de Koning R, Erhabor J, Higginbotham G, Khan M, et al. Survey fatigue during the COVID-19 pandemic: an analysis of neurosurgery survey response rates. Front Surg. 2021;8:690680. doi:10.3389/fsurg.2021.690680.
- Jeong D, Aggarwal S, Robinson J, Kumar N, Spearot A, Park DS. Exhaustive or exhausting? Evidence on respondent fatigue in long surveys. J Dev Econ. 2023;161:102992. doi:10.1016/j.jdeveco.2022.102992.
