ABSTRACT
Leptomeningeal metastasis (LM) of nasopharyngeal carcinoma (NPC) is rare and associated with a poor prognosis. Immune checkpoint inhibitors (ICIs) have been the standard first-line treatment for metastatic NPC, but their effect on meningeal metastasis of NPC needs further investigation. A 38-year-old man complained of bilateral neck masses and sought medical care. He was diagnosed with nasopharyngeal undifferentiated non-keratinizing carcinoma with bilateral cervical lymph node metastasis and multiple bone metastasis, stage cT4N2M1 IVb. Then, the patient received first-line anti-PD-1 antibody tislelizumab combined with gemcitabine and cisplatin and achieved partial response. After seven cycles of first-line chemoimmunotherapy, the patient subsequently developed neurological symptoms, including unsteady walking, slurred speech, coughing on drinking, and unconsciousness. MRI showed leptomeningeal linear enhancement, and cerebrospinal fluid (CSF) analysis indicated Epstein–Barr virus (EBV) infection and squamous cell carcinoma cytology, suggesting the diagnosis of leptomeningeal metastasis. After the definite diagnosis of LM, the patient’s condition deteriorated rapidly, leading to his death from brain herniation. We reported the first case of advanced NPC with pathologically confirmed leptomeningeal metastasis after receiving first-line chemoimmunotherapy. Considering the poor prognosis of LM, it is suggested to perform MRI and CSF examination when patients have neurological symptoms. Although immunotherapy significantly improved survival outcomes of advanced NPC patients, it seemed not effective in the setting of LM. The effect of other treatment options, such as radiation therapy and intrathecal therapy, requires further verification.
Introduction
Nasopharyngeal carcinoma (NPC) is an endemic malignancy in Southeast Asia, particularly in southern China.Citation1 Common metastatic sites of NPC are bone, lung, and liver, but leptomeningeal metastasis (LM) is extremely rare.Citation1 Classical non-keratinized cell types are associated with Epstein–Barr virus (EBV) infection. Immune checkpoint inhibitor (ICIs), in combination with chemotherapy, have been proved effective as first-line treatment for advanced or recurrent NPC, but their effect on LM remains unclear.Citation2,Citation3
Here, we present the first reported case of advanced NPC who developed pathologically confirmed leptomeningeal metastasis after first-line chemoimmunotherapy. The target lesion was still in partial response, but LM progressed suddenly, which might be misdiagnosed due to a variety of confounding factors such as immune-related encephalitis.
Case presentation
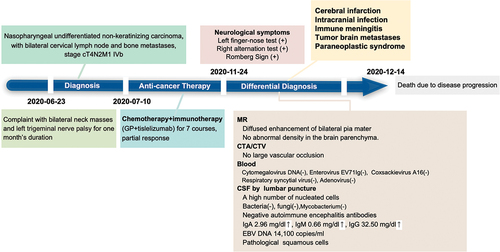
In June 2020, a 38-year-old male from China presented with bilateral neck masses and left trigeminal nerve palsy for one month’s duration. Nasopharyngoscopy revealed a nasopharyngeal mass, and the biopsy confirmed undifferentiated nonkeratinizing carcinoma. The plasma level of EBV DNA of this patient was 203,000 copies/mL. Magnetic resonance imaging (MRI) showed the nasopharyngeal mass occupies the right pharyngeal recess, bilateral pterygopalatine fossa, posterior nostrils, left posterior nasal cavity, ethmoid sinus, sphenoid sinus, bilateral cavernous sinus, and involves the left Merkle cavity and Gasser ganglion, without signs of meningeal metastasis (). After refining the PET-CT scan and pathological examination, he was diagnosed as nasopharyngeal undifferentiated non-keratinizing carcinoma with bilateral cervical lymph node metastasis and multiple bone metastasis, stage cT4N2M1 IVb. Then, he received six courses of treatment with tislelizumab (anti PD-1 monoclonal antibody), gemcitabine and cisplatin and one course of tislelizumab maintenance treatment from July 2020 to Nov 09, 2020. The treatment response was durable partial response (PR) with no serious adverse events (), and the plasma level of EBV DNA decreased to undetectable level after the first course of treatment.
Figure 1. (a). Magnetic resonance imaging (MRI) showed the nasopharyngeal mass occupies the right pharyngeal recess, bilateral pterygopalatine fossa, posterior nostrils, left posterior nasal cavity, ethmoid sinus, sphenoid sinus, bilateral cavernous sinus, and involves the left Merkle cavity and Gasser ganglion. (b). Baseline cranial MRI of this patient showed no signs of meningeal metastasis.
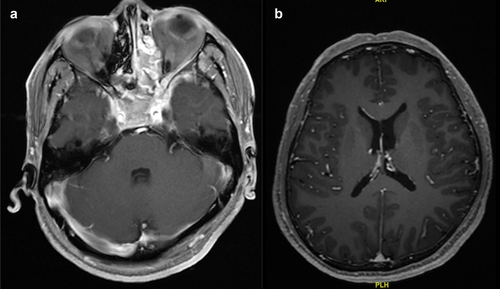
Figure 2. (a) Changes in target lesions by nasopharyngeal MRI every 2 cycles during first line chemoimmunotherapy; (b) Leptomeninges strengthening on T1WI enhancement; (c) Blurred sulcus on T2FLAIR. (d) Linear reinforcement in the sulci on CTA. (e) Cerebrospinal fluid cytology: cerebrospinal fluid smear and sediment paraffin-embedded sections showed large nuclei, deep staining, and a high nucleoplasm ratio, considering the possibility of cancer cells. Immunohistochemical results: heteromorphic cells CK (+), P63(+), Ki-67 (about 40%), CD20(-), CD3(-), consistent with squamous cell carcinoma.
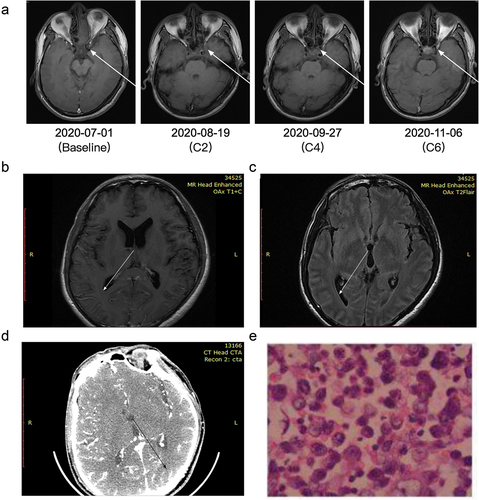
On Nov 24, 2020, the patient began to walk unsteadily without obvious causes, accompanied by slurred speech and coughing while drinking. He had no dizziness, headache, chest tightness, shortness of breath, nausea or vomiting. Physical examination revealed a slightly shallow negative lip fold on the right side, right tongue extension, left finger-nose test and right alternation test (+), Romberg Sign (+). On 26 Nov, the patient developed complete mixed aphasia and hemiplegia. Diffused enhancement of bilateral pia mater was observed in MRI examination, but no abnormal enhancement of facial nerve and hypoglossal nerve was seen. No large vascular occlusion was observed on head CTA/CTV (). Dehydration and diuretic hormones were used to reduce cerebral edema. The first lumbar puncture indicated that the pressure of cerebrospinal fluid (CSF) was 220mmH2O and the color was pale yellow, with a higher number of nucleated cells, higher level of protein, lower level of sugar, and negative bacteria, fungi, mycobacterium cultures. Intracranial infection and immune meningitis were suspected because of the increases of IgA, IgG, and IgM in CSF. After active anti-infective and anti-epileptic treatment, the patient remained in a coma with recurrent seizures. So, the second lumbar puncture was performed. The paraneoplastic and autoimmune antibodies were negative in CSF. The gene sequencing of CSF revealed EB virus infection. Plasma levels of EBV DNA were markedly elevated at 14,100 copies/ml. Pathological examination on Dec 7, 2020 found squamous cell carcinoma in CSF (). Finally, this patient was diagnosed with meningeal metastasis from nasopharyngeal carcinoma, and the disease progressed. Then, his condition deteriorated rapidly within several days. He needed to breathe with the assistance of a ventilator and had bilateral unequal pupils. The Glasgow Coma Scale (GCS) was three, tingled without eye opening, no verbal or motor response. After communicating with his family members, it was decided to postpone anti-tumor therapy. The symptomatic supportive treatments included dehydration and intracranial pressure reduction, sedation, and anti-epilepsy. On Dec 14, 2020, the patient suddenly had bilateral mydriasis, loss of light reflex, and a drop in blood pressure. Brain herniation was considered and led to death. The whole process of diagnosis and treatment is summarized in .
Discussion
Leptomeningeal metastasis is the infiltration of the leptomeninges by malignant cells, and the most common cases are caused by breast and lung cancer.Citation4 Direct intracranial invasion is commonly seen in NPC patients at a locally advanced stage, but leptomeningeal metastasis from NPC is extremely rare.Citation5 No leptomeningeal or brain metastasis cases were found in a study of 225 patients with NPC despite the high incidence of skull base invasion.Citation6 Less than 10 cases of NPC with meningeal involvement have been reported in the literature.Citation6–9 Of these, only four were undifferentiated nasopharyngeal carcinomas.Citation6,Citation10–12 Given the reported poor prognosis of LM with an average survival of 2–4 months,Citation13 the patient’s condition deteriorated rapidly, and died approximately 20 days after the disease progression.
The diagnosis of leptomeningeal metastasis has been challenging due to limitations of neuroimaging and cytology. LM is a comprehensive diagnosis based on clinical presentation, neuroimaging, and cytology. Common symptoms and signs of leptomeningeal metastasis include headache, confusion, nausea, vomiting, cranial nerve palsies, ataxia and cognitive impairment.Citation14 Brain MRI may reveal leptomeningeal enhancement with linear, irregular or nodular morphology. Recently, a case demonstrated the utility of PET/CT in the diagnosis of LM.Citation12 Cytological demonstration of malignant cells in the CSF is the gold standard for the diagnosis of LM. CSF cytology is positive in 50% to 60% of patients while the rate can be improved to 85% with repeat cytologic examinations.Citation15,Citation16 Meanwhile, due to the association between EBV and NPC, CSF EBV DNA also refers to a definitive diagnosis of NPC.Citation17 In clinical practice, considering the low incidence and poor prognosis of LM, it is suggested to perform MRI and CSF examination when patients have neurological symptoms, such as unsteady walking, slurred speech, coughing on drinking, and unconsciousness.
The pathological characteristics of NPCs are mainly manifested as a high invasion of immune cells around tumor lesions and in tumors, and EBV-induced nasopharyngeal non-keratinizing carcinoma of the nasopharyngeal is overexpressed with PD-L1 compared with EBV-negative NPCs, indicating that the tumor microenvironment of EBV-induced NPCs is in an immunosuppressive state, making immunotherapy is an effective treatment option.Citation18 Carrelizumab in combination with cisplatin and gemcitabine significantly prolongs progression-free survival for locally recurrent or distant metastatic nasopharyngeal carcinoma compared to cisplatin plus gemcitabine in first-line treatment.Citation19 About 38% of patients with meningeal metastasis from solid tumors responded to pembrolizumab.Citation11 Patients with leptomeningeal metastasis of NSCLC also benefited from immunotherapy monotherapy or combination therapy.Citation20 As for NPC, there is only one case reported that LM happened after initial ICIs regimen and radiotherapy, but it lacks the evidence of CSF cytology.Citation21 Therefore, data on leptomeningeal metastasis of NPC are still limited. In this patient, although immunotherapy was effective in controlling the primary lesion, meningeal metastasis still occurred. Therefore, anti-PD1 antibody combined with systemic chemotherapy seemed not effective in the setting of LM. Above all, the effect of immunotherapy on LM of nasopharyngeal carcinoma requires further research.
Treatment options for leptomeningeal metastasis include radiation therapy, systemic drug therapy, or intrathecal therapy. Recent studies have suggested that proton craniospinal cord irradiation (CSI) may be superior to traditional involved field radiation therapy (IFRT). Moreover, multiple trials have shown potential efficacy of targeted therapies (i.e., HER2, EGFR, ALK, BRAF, etc.).Citation22 As for nasopharyngeal carcinoma, it is reported that whole brain radiotherapy combined with oral capecitabine is effective in a case of LM of NPC.Citation21 A combination of local therapy and systemic chemotherapy might have therapeutic potential in these patients with LM. More investigation is required to identify optimal clinical choice among different treatments.
Due to the use of immune checkpoint inhibitors in first-line therapy in this patient, the possibility of ICI-associated aseptic meningitis should also be considered, of which the CSF cytology shows lymphocytic inflammation. Most patients with immune mediated meningitis respond well to glucocorticoid therapy. In this case, the normal levels of monocytes and adenylate deaminase in CSF, as well as a low T lymphocyte count, and the absence of other endocrine abnormalities do not support the diagnosis. As ICI-associated aseptic meningitis is an exclusive diagnosis, empiric application of corticosteroids should be cautious when infection and metastasis cannot be completely ruled out.
Conclusion
Leptomeningeal metastasis from NPC is rare but with a poor prognosis. Therefore, it is recommended to perform neuroimaging and cytology examination for LM if the patient has associated neurological symptoms. Comprehensive identification of leptomeningeal metastasis is important to optimize clinical decisions. The effect of immunotherapy and other treatment options, such as radiation therapy and intrathecal therapy, requires further verification in the setting of LM.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–5. doi:10.3322/caac.21660.
- Hsu C, Lee SH, Ejadi S, Even C, Cohen RB, Le Tourneau C, Mehnert JM, Algazi A, van Brummelen EMJ, Saraf S, et al. Safety and antitumor activity of pembrolizumab in patients with programmed death-ligand 1–positive nasopharyngeal carcinoma: results of the KEYNOTE-028 study. J Clin Oncol. 2017;35(36):4050–6. doi:10.1200/JCO.2017.73.3675.
- Ma BBY, Lim WT, Goh BC, Hui EP, Lo KW, Pettinger A, Foster NR, Riess JW, Agulnik M, Chang AYC, et al. Antitumor activity of nivolumab in recurrent and metastatic nasopharyngeal carcinoma: an international, multicenter study of the mayo clinic phase 2 consortium (NCI-9742). JCO. 2018;36(14):1412–8. doi:10.1200/JCO.2017.77.0388.
- DeAngelis LM, Boutros D. Leptomeningeal metastasis. Cancer Invest. 2005;23(2):145–54. doi:10.1081/CNV-50458.
- Ho JH. An epidemiologic and clinical study of nasopharyngeal carcinoma. Int J Radiat Oncol Biol Phys. 1978;4(3–4):182–98. doi:10.1016/0360-3016(78)90137-2.
- Cvitkovic E, Bachouchi M, Boussen H, Busson P, Rousselet G, Mahjoubi R, Flores P, Tursz T, Armand JP, Azli N, et al. Leukemoid reaction, bone marrow invasion, fever of unknown origin, and metastatic pattern in the natural history of advanced undifferentiated carcinoma of nasopharyngeal type: a review of 255 consecutive cases. J Clin Oncol. 1993;11(12):2434–42. doi:10.1200/JCO.1993.11.12.2434.
- Wang CJ, Wang CY. Nasopharyngeal carcinoma with leptomeningeal dissemination: case report. Chang Gung Med J. 2000;23:118–22.
- Redman BG, Tapazoglou E, Al-Sarraf M. Meningeal carcinomatosis in head and neck cancer. Report of six cases and review of the literature. Cancer. 1986;58(12):2656–61. doi:10.1002/1097-0142(19861215)58:12<2656:AID-CNCR2820581218>3.0.CO;2-Q.
- Geng X, Hao F, Han G, Zhang Y, Qin P. Dural and multiple brain metastases from basaloid nasopharyngeal carcinoma: case report and literature review. Front Oncol. 2021;11:665652. doi:10.3389/fonc.2021.665652.
- Fakhry C, Bajaj G, Aygun N, Westra W, Gillison M. Long-term survival of a patient with leptomeningeal involvement by nasopharyngeal carcinoma after treatment with high-dose intravenous methotrexate. Head Neck. 2012;34(2):296–300. doi:10.1002/hed.21516.
- Naidoo J, Schreck KC, Fu W, Hu C, Carvajal-Gonzalez A, Connolly RM, Santa-Maria CA, Lipson EJ, Holdhoff M, Forde PM, et al. Pembrolizumab for patients with leptomeningeal metastasis from solid tumors: efficacy, safety, and cerebrospinal fluid biomarkers. J Immunother Cancer. 2021;9(8):e002473. doi:10.1136/jitc-2021-002473.
- Montanarella M, Boldig K, Natter P, Ozdemir S. 18 F-FDG PET/CT Findings of Leptomeningeal Metastasis in Nasopharyngeal Carcinoma. Clin Nucl Med. 2023;48(2):201–2. doi:10.1097/RLU.0000000000004499.
- Beauchesne P. Intrathecal chemotherapy for treatment of leptomeningeal dissemination of metastatic tumours. Lancet Oncol. 2010;11(9):871–9. doi:10.1016/S1470-2045(10)70034-6.
- Wang N, Bertalan MS, Brastianos PK. Leptomeningeal metastasis from systemic cancer: review and update on management. Cancer. 2018;124(1):21–35. doi:10.1002/cncr.30911.
- Grossman SA, Krabak MJ. Leptomeningeal carcinomatosis. Cancer Treat Rev. 1999;25(2):103–19. doi:10.1053/ctrv.1999.0119.
- Twijnstra A, de Visser BW O, van Zanten AP. Diagnosis of leptomeningeal metastasis. Clin Neurol Neurosurg. 1987;89(2):79–85. doi:10.1016/0303-8467(87)90180-6.
- Ma ATW, Ma BBY, Teo PML, Chan ATC. A novel application of plasma and cerebrospinal fluid level of Epstein Barr virus DNA in the diagnosis of leptomeningeal metastasis from nasopharyngeal carcinoma. A case report. Oncology. 2008;74(1–2):119–22. doi:10.1159/000139140.
- Larbcharoensub N, Mahaprom K, Jiarpinitnun C, Trachu N, Tubthong N, Pattaranutaporn P, Sirachainan E, Ngamphaiboon N. Characterization of PD-L1 and PD-1 expression and CD8+ tumor-infiltrating lymphocyte in Epstein-Barr Virus-associated nasopharyngeal carcinoma. Am J Clin Oncol. 2018;41(12):1204–10. doi:10.1097/COC.0000000000000449.
- Yang Y, Qu S, Li J, Hu C, Xu M, Li W, Zhou T, Shen L, Wu H, Lang J, et al. Camrelizumab versus placebo in combination with gemcitabine and cisplatin as first-line treatment for recurrent or metastatic nasopharyngeal carcinoma (CAPTAIN-1st): a multicentre, randomised, double-blind, phase 3 trial. Lancet Oncol. 2021;22(8):1162–74. doi:10.1016/S1470-2045(21)00302-8.
- Zheng M-M, Tu H-Y, Yang J-J, Zhang X-C, Zhou Q, Xu C-R, Jiang B-Y, Yang X-N, Yang X-R, Deng J-Y, et al. Clinical outcomes of non–small cell lung cancer patients with leptomeningeal metastases after immune checkpoint inhibitor treatments. Eur J Cancer. 2021;150:23–30. doi:10.1016/j.ejca.2021.03.037.
- Zhang X, Shu X, Long B. Leptomeningeal metastasis from de novo metastatic nasopharyngeal carcinoma: a case report. Transl Cancer Res. 2022;11(9):3349–56. doi:10.21037/tcr-22-1211.
- Primdahl D, Cohen-Nowak A, Kumthekar P. Novel approaches to treatment of leptomeningeal metastases. Curr Opin Neurol. 2023;36(6):592–602. doi:10.1097/WCO.0000000000001218.