?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
This study aimed to evaluate how the duration of travel affects the behavior of urban and rural residents regarding free COVID-19 vaccination, and provide scientific evidence for promoting free vaccination and building an immune barrier to cope with future epidemics. From August 3, 2022 to February,18,2023, A follow-up survey was conducted in urban and rural adults in four cities in China to collect information on socio-demographic factors, vaccination status and travel time for vaccination. Propensity score matching (PSM) analysis was deployed to measure the net difference of the enhanced vaccination rate between urban and rural residents in different traffic time distribution. A total of 5780 samples were included in the study. The vaccination rate of the booster dose of COVID-19 vaccine among rural residents was higher than that of urban residents with a significant P-value (69.36% VS 64.49%,p < .001). The traffic time had a significant negative impact on the COVID-19 booster vaccination behavior of urban and rural residents. There was a significant interaction between the travel time to the vaccination point and the level of trust in doctors. Travel time had a negative impact on the free vaccination behavior of both urban and rural residents. The government should optimize and expand the number of vaccination sites and enhance residents’ trust in the medical system. This is crucial for promoting free vaccination and effective epidemic management in the future.
Introduction
Vaccination is an important tool for primary prevention of infectious diseases.Citation1 Only when the optimal vaccination level is achieved rapidly can the population immunity barrier be formed to mitigate the epidemic and negative impact of infectious diseases, particularly in key populationsCitation2–6 Since mandatory vaccination undermines democratic principles and leads to greater socio-economic issues than pandemics, it is crucial to investigate the factors that influence free vaccination in order to develop improved and more targeted health policies to address future public health emergencies,Citation7–9 The travel time spent to reach the vaccination site affects the convenience of free vaccination, which in turn affects free vaccination behavior; therefore, many studies consider travel time to be the main factor influencing people’s free vaccination.Citation10,Citation11 Prior research has consistently highlighted the significance of travel time to free vaccination sites as a major obstacle to achieving high vaccination rates, for example, in China, increased traffic time was associated with increased vaccine hesitancy, and in Ethiopia, the uptake of free vaccines tends to decline as the duration required to reach these vaccination sites increases.Citation12,Citation13
During the COVID-19 pandemic, the Chinese government has made the greatest efforts to expand the primary vaccination rate, establishing tens of thousands of temporary vaccination sites in a relatively short period of time, with the aim of reducing the travel time spent by urban and rural residents to free vaccination sites and improve the convenience of vaccination as much as possible.Citation14 However, after China has made corresponding policy adjustments whereas the SARS-CoV-2 epidemic has been reclassified from “Class B epidemic and A management” to “Class B epidemic and B management,” COVID-19 vaccination strategies do not prioritize mass vaccination; instead, residents are required to visit a specific hospital for vaccination. Travel time to free vaccination sites appears to be a major barrier to enhanced COVID-19 vaccination uptake. The COVID-19 booster vaccine is free, but administered on a voluntary basis, unlike other free vaccines (Category I vaccines).Citation15 Booster doses become more important as the virus mutate, the efficacy of the original vaccine decreases, and the Peltzman effect (increased risk behavior among residents who have received the primary dose) occurs.Citation16,Citation17 So it is hence more imperative to explore the impact of travel time on COVID-19 booster vaccination. Based on our understanding, the majority of studies in the available literature have examined the factors influencing vaccine acceptance and uptake, as well as the impact of vaccination rates on the pandemic by considering by considering variables such as socio-demographic factors, trust in the healthcare system, perception of viral infection risks, vaccine efficacy and safety, and individuals’ history of receiving influenza vaccinations in the past or present.Citation18–21 Additional research has indicated that rural residents are predominantly influenced by mostly socioeconomic factors, accessibility of transportation services, and the availability, distribution and accessibility of COVID-19 vaccination services.Citation22,Citation23 On the other hand, urban residents are primarily affected by personal psychological experiences, perceptions, and other individual-level factors.Citation24–26 Nevertheless, there is a scarcity of studies that specifically explore the impact of travel time to free vaccination sites on individuals’ behavior toward vaccination uptake.
In the process of achieving mass free vaccination, one of the most important characteristics of China is its dual social structure in urban and rural areas. This structure represents a system in which urban and rural areas are artificially separated by household registration, forming a dual social structure for urban and rural residents. About 914 million people (63.89%) lived in urban areas and 598 million people (36.11%) lived in rural areas in 2021.Citation27 Health care expenditures, allocation of resources, and allocation of facilities and professionals vary widely between rural and urban areas.Citation28 Based on this hypothesis, it is believed that there might be variations in the influence on the increased COVID-19 vaccination rate between urban and rural residents in China. Therefore, it becomes imperative to categorize the enhanced vaccination behavior for COVID-19 among urban and rural residents in China.
This study hypothesized that traffic time has an impact on the free vaccination behavior of urban and rural residents in China. Additionally, it further explored the net difference of COVID-19 vaccination behavior between urban and rural residents at different traffic hours and its influencing factors.
Methods
Sample and data
Study design and ethical aspects
We randomly selected four cities of Changzhou, Zhengzhou, Xining and Mudanjiang in China. Subsequently, within each city, more than two rural areas and two urban areas were randomly sampled from each city. In addition, within each region, households were sampled by simple random sampling. Finally, all selected family members participated in this survey (age ≥18 years) and completed online or offline questionnaires (paper questionnaires) with the assistance of the investigator. We conducted a baseline survey from March to August 2022, collecting information on 6781 subjects. Subsequently, a follow-up survey was conducted in February 2023. Based on the baseline survey, we followed 5891 participants in the study population, with a follow-up rate of 86.88%. Participants were excluded if they answered abnormal answers. Finally, 5780 participants were included in the analysis. Moreover, 3832 participants, with half from urban areas and the other half from rural areas, were matched using propensity score matching (PSM) of 1:1 k-nearest neighbor matching. PSM can achieve the post hoc randomization effect of randomized controlled trials, effectively reduce the influence of selection bias and confounding factors, and obtain the net difference of traffic time on the free vaccine behavior of urban and rural residents. None of the variables utilized in the final analysis contained missing data. The flow chart of the participants is shown in .
Measures of variables
The data we collected included four categories: (1) personal characteristics (sociodemographic information and vaccination behavior); (2) dimensions of the health care system (level of trust in physicians and vaccine manufacturers); (3) Convenience of vaccination (travel time to booster vaccination site: <15 min, 15–30 min, >30 min); (4) Awareness of the COVID-19 pandemic (severity and risk of infection). An offline questionnaire was used to evaluate whether the booster dose of COVID-19 vaccine was given to the respondents who had received the primary dose of COVID-19 vaccine questionnaires.
Models and data analysis procedure
Variables with Variance Inflation Factor higher than 3.0 were excluded from the analysis due to collinearity, as indicated in Supplementary Table S1. The chi-square test was used to test the differences in COVID-19 booster vaccination rates between urban and rural participants in different travel time periods. Binary logistic regression was used to analyze the impact of travel time and other factors on the free vaccination behavior. The formula is as following:
P is the probability of the dependent variable;1,
2…
m indicate independent variable; β0 , β1 … βm indicate regression coefficient. β0 indicate intercept.
PSM was used to minimize potential confounding bias (see Supplementary Figure S1 and Supplementary Table S7).
We used attributable risk (AR) analysis to explore the objective contribution of traffic time to the free vaccination rate of urban and rural residents. The AR formula is as following:
Notes: AR: Attribute Risk; Ie indicates the incidence of the exposed group; I0 indicates the incidence of the non-exposed group.
All statistical analyses were performed using SPSS, version 25.0, and STATA, version 17.1. A p-value of less than 0.05 was considered statistically significant.
Results
The impact of travel time on the vaccination of COVID-19 booster vaccination in urban and rural participants
A total of 5780 urban and rural residents, including 3303 urban residents (57.14%) and 2478 rural residents (42.86%) from China, were analyzed in this study. As shown in , the vaccination rate of the free booster dose of COVID-19 in urban residents was slightly lower than that in rural residents (Urban: 64.49%, 95% CI: 62.09% to 67.47%; Rural: 69.36%, 95% CI: 69.22% to 71.87%). The rate of enhanced COVID-19 vaccination among urban residents decreased with increasing travel time (>30 min:48.92%; 15-30 min:63.14%; <15 min:69.61%), which was similar in rural residents (>30 min 64.33%; 15-30 min:71.73%; <15 min:75.45%). Propensity score matching analysis showed similar results and the disparity in vaccination rates between urban and rural participants was most pronounced (14.81%) during traffic hours exceeding 30 min. This is illustrated in below. In , binary logistic regression analysis indicated that travel time had a significant negative effect and similar goodness-of-fit on the acceptance of COVID-19 booster vaccination among urban and rural participants (urban: 15–30 min: aOR = 1.65, 95%CI: 1.31–2.09; <15 min: aOR = 2.1695%CI: 0.31–0.51; Rural: 15–30 min: aOR = 1.16, 95%CI: 1.03–1.57; <15 min: aOR = 1.39, 95%CI: 1.32–1.68); (Urban: R2:0.34;Rural: R2:0.38). The results of attribution analysis showed that 19.51% of the booster dose vaccination rate in urban residents was attributed to travel time <15 min, and 9.83% in rural residents. (Urban: 19.51%,95%CI[10.04–29.61]; Rural: 9.83%,95%CI [5.62–13.14]). (See Supplementary Table S2).
Figure 2. Proportions of urban and rural residents vaccinated at different time traffic periods before and after PSM.
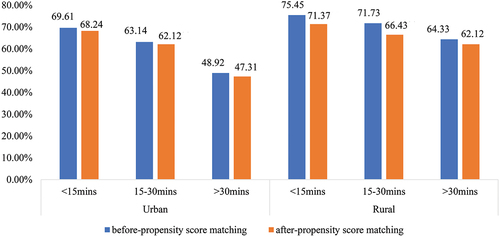
Table 1. Characteristics of Chinese urban and rural resident participants in 2023 follow-up study.
Table 2. The relationship between free vaccination and socio-demographic characteristics, subjective social status and trust in the health system among urban and rural residents.
The factors influencing the vaccination of COVID-19 booster vaccination among urban and rural residents
After adjusting for potential confounding variables, vaccination was positively associated with physician trust, and the elderly (≥60 years old) (Urban: aOR = 0.84,95%CI[0.52–0.93]; Rural: aOR = 0.81,95%CI[0.62–0.95]), and patients with chronic diseases were less likely to be vaccinated. (Urban: aOR = 0.76,95%CI[0.64–0.85]; Rural: aOR = 0.79,95%CI[0.68–0.95]). There was a significant interaction between the minimum travel time to vaccination sites (<15 min) and trust in doctors for free vaccination (Urban: aOR = 2.64,95%CI[1.27–4.76]; Rural: aOR = 3.15,95%CI[2.26–4.42]), which was also identified as an independent factor for receiving free vaccinations. (See Supplementary Table S3 and Table S4).
Discussion
Using the COVID-19 booster vaccination as an example, this study investigated the impact of the travel time spent to reach the vaccination point on the free vaccination behavior of urban and rural residents in China. Our findings showed that rural participants had higher rates of booster vaccination against COVID-19 than urban participants. Traffic time had a negative impact on the free vaccination behavior of both urban and rural residents. Trust in doctors, having a chronic disease, and being over 60 years old were significantly associated with the uptake of free vaccination among urban and rural residents. Compared with other studies, we have found that a significant interaction was found between the minimum travel time to the vaccination point (less than 15 min) and trust in doctors with regards to free vaccination behavior. According to the propensity score matching (PSM) analysis, the disparity in vaccination rates between urban and rural participants was most pronounce during traffic hours exceeding 30 min. Our study is the first to use attribution analysis to analyze the contribution of travel time to free vaccination for urban and rural residents in China (Supplementary Table 5).
This study investigates the vaccination rates and influencing factors of the free booster dose of the COVID-19 vaccine among urban and rural residents. The vaccination rate of COVID-19 booster vaccine in urban and rural residents investigated in this study was similar to that reported by the Chinese government. The actual COVID-19 enhanced vaccination rate of Chinese urban and rural residents in our study was far lower than the vaccination intention of nearly 95% in previous studies, indicating that traffic time has a great impact on the free vaccination behavior of Chinese urban and rural residents.Citation29 Our findings indicated that the travel time to the vaccination point has a similar effect on the vaccination behavior of both urban and rural residents. The more traffic hours urban participants spent, the lower the rate of booster vaccination against COVID-19. Our study is the first to use attribution analysis to analyze the contribution of travel time to free vaccination for urban and rural residents in China. If these associations were causal, and the travel time for vaccination was less than 15 min for all participants, the vaccination rate could increase by 19.51% in urban areas and 9.83% in rural areas. SWOT analysis showed that excessive population density, work stress, and traffic congestion exacerbate the impact of traffic time on the free vaccination behavior of urban residents.Citation30,Citation31 Urban population density is high, and the virus is more likely to spread.Citation32 The government must increase and optimize the distribution of vaccination sites to reduce the travel time spent by urban residents to reach the free vaccination sites and its impact, so as to quickly achieve the optimal population vaccination level and to improve the herd immunity of urban residents and maximize the benefits of vaccine immunization.Citation33,Citation34 In rural areas, governments can expand free vaccine uptake through increased health investment and economic incentives, which can improve grassroots capacity to prevent and control emerging infectious diseases in the future (Supplementary table 6). The vaccination rate of rural participants in China was much higher than that of urban participants during distant traffic hours, which may be largely due to the Chinese government’s focus on vaccination on rural populations and rural areas.Citation35
We found that older adults (aged 60 years and older) were reluctant to receive free vaccines, a trend consistent with previous studies. Older people may have more frequent mobility problems and need help getting to vaccination sites than younger people; Therefore, vaccination at home or in group settings such as residential facilities would make it easier to increase their vaccination rates.Citation36,Citation37 Older people are more likely to be frail or have chronic medical conditions, to be affected by travel time for vaccination, concerns about side effects or efficacy, and a lack of vaccine knowledge.Citation38 Therefore, we think that special vaccination policies for the elderly, such as door-to-door vaccination and free transportation, are necessary. Participants with chronic diseases are less likely to receive free vaccines, and the virus is more susceptible and harmful to people with chronic diseases, so further attention should be paid to such people.Citation39
According to the PSM analysis, the distribution of the booster vaccination rate of COVID-19 between urban and rural participants was different in different traffic times. Vaccination rates were lowest among urban and rural participants during the furthest traffic hours, the most significant disparity in vaccination rates was noted between urban and rural participants. This provides compelling evidence that travel time has a negative impact on the likelihood of urban and rural residents seeking free vaccinations. In order to mitigate this impact, it is imperative to implement appropriate policies. For instance, authorities in China should consider providing free transportation, extending vaccination periods, and offering family education to enhance vaccination coverage, particularly among individuals residing in rural and remote areas.Citation40 Transportation time has the greatest impact on free vaccination behavior among urban participants, which can be reduced by appointment for vaccination and appropriate incentive policies for vaccination.
The study discovered that trust in physicians was linked to higher vaccination rates and identified an interaction between trust in physicians and travel time. Enhancing residents’ trust in doctors could offset the negative effect of travel time on the uptake of free vaccinations for both urban and rural residents. Vaccination is, in essence, a matter of trust.Citation41 Rebuilding trust and confidence in vaccines is essential to the vaccination process in order to improve vaccination coverage.Citation42 At the same time, a previous study has shown that improving trust in the healthcare system is critical for increasing public self-efficacy in vaccination.Citation43 To increase public trust and update vaccine antigenic composition to incorporate the latest viral variants, development of novel highly effective vaccines with long-term immune persistence will be a key priority.Citation44 While improving the effectiveness of the vaccine, further public media publicity should be carried out to build trust in the whole society. This is because the same social pressures on individuals to tend to the scientific normative trust consensus in society may also encourage people to follow widely shared beliefs about the benefits and risks of vaccination.Citation45,Citation46 On the other hand, relevant government departments should promote in-depth cross-sectoral communication among health authorities, vaccine manufacturing companies, and the public in the whole city.Citation47 Such consultative communication among different stakeholders can best build the trust of urban residents in the healthcare system and free vaccination providers.
Strengths and limitations of this study
The study exhibits notable strengths, which include being the inaugural national multi-center survey conducted in China after COVID-19 was classified as a Category B disease. Moreover, it boasts a large sample size, ensuring robust statistical power and encompassing diverse populations, thereby providing comprehensive representation.
This is the first study to confirm the net difference in the effect of travel time on the free vaccination behavior of urban and rural residents in China through propensity matching analysis (PSM), and the contribution of travel time was measured by attribution analysis.
The data on travel time and free vaccination information relied on self-reporting from the participants, which may be susceptible to recall bias. Participants may have difficulty accurately remembering certain details, which could impact the reliability of the findings. In addition, the number of covariates included in the Propensity Score Matching (PSM) procedure was somewhat limited. While efforts were made to control for confounding factors, it is important to note that the comprehensive set of confounding variables may extend beyond those accounted for in the PSM analysis. Therefore, there could be additional factors influencing the relationship between different traffic periods and the free vaccination behavior of urban and rural residents that were not considered in this study.
Conclusion
The coverage of booster doses of the SARS-CoV-2 vaccine was higher among rural residents compared to urban residents. Travel time had a negative impact on the free vaccination behavior of both urban and rural residents, The government should reduce travel time by optimizing and increasing the layout of vaccination sites and other measures in order to fully maximize its objective contribution to the improvement of residents’ free vaccination behavior. This measure is essential to increase free vaccination rates for urban residents and build an immune barrier against future outbreaks. In addition to reducing travel time, it is essential to prioritize efforts in bolstering the confidence of both urban and rural residents in the healthcare system. Implementing targeted vaccination policies for the elderly and individuals with chronic illnesses, such as door-to-door vaccination services and providing free transportation, can mitigate the impact of travel time and further promote vaccination uptake.
Ethical approval
The study was deemed exempt from assessment by the ethics review Committee of the Life Sciences Ethics Review Committee of Zhengzhou University (Approval number: 2021-01-12-05).
Supplementary File.docx
Download MS Word (56.6 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplementary material
Supplemental data for this article can be accessed on the publisher’s website at https://doi.org/10.1080/21645515.2024.2352914
Additional information
Funding
References
- Miao Y, Zhang W, Li Y, Wu J, Xu D, Gu J, Wang M, Wei W, Ye B, Miao C, et al. Association between lifestyle and COVID-19 vaccination: a national cross-sectional study. Front Public Health. 2022;10:918743. doi:10.3389/fpubh.2022.918743.
- Benati I, Coccia M. Global analysis of timely COVID-19 vaccinations: improving governance to reinforce response policies for pandemic crises. Int J Health Gov. 2022;27(3):240–8. doi:10.1108/IJHG-07-2021-0072.
- Coccia M. Pandemic prevention: lessons from COVID-19. Encyclopedi. 2022;1(2):433–44. doi:10.3390/encyclopedia1020036.
- Hassan MM, Tahir MH, Ameeq M, Jamal F, Mendy JT, Chesneau C. Risk factors identification of COVID-19 patients with chronic obstructive pulmonary disease: a retrospective study in Punjab-Pakistan. Immunity Inflam Disease. 2023;11(8):e981. doi:10.1002/iid3.981.
- Muneeb HM, Ameeq M, Jamal F, Tahir MH, Mendy JT. Prevalence of COVID-19 among patients with chronic obstructive pulmonary disease and tuberculosis. Ann Med. 2023;55(1):285–91. doi:10.1080/07853890.2022.2160491.
- Coccia M. Optimal levels of vaccination to reduce COVID-19 infected individuals and deaths: a global analysis. Environ Res. 2022;204:112314. doi:10.1016/j.envres.2021.112314.
- Coccia M. Improving preparedness for next pandemics: max level of COVID-19 vaccinations without social impositions to design effective health policy and avoid flawed democracies. Environ Res. 2022;213:113566. doi:10.1016/j.envres.2022.113566.
- Coccia M. Sources, diffusion and prediction in COVID-19 pandemic: lessons learned to face next health emergency. AIMS Public Health. 2023;10(1):145–68. doi:10.3934/publichealth.2023012.
- Shi H, Goulias KG. Long-term effects of COVID-19 on time allocation, travel behavior, and shopping habits in the United States. J Transp Health. 2024;34:101730. doi:10.1016/j.jth.2023.101730.
- Mathieu P, Gautier A, Raude J, Goronflot T, Launay T, Debin M, Guerrisi C, Turbelin C, Hanslik T, Jestin C, et al. Population perception of mandatory childhood vaccination programme before its implementation, France, 2017. Euro Surveill. 2019;24(25):1900053. doi:10.2807/1560-7917.ES.2019.24.25.1900053.
- Ishida M, Mulou N, Mahal A. Travel time to health facilities in Papua New Guinea: implications for coverage and equity in child vaccinations. Vaccine. 2022;40(38):5556–61. doi:10.1016/j.vaccine.2022.07.060.
- Miao Y, Bai J, Shen Z, Li Y, Zhang W, Zhu D, Ren R, Zhang J, Guo D, Tarimo CS, et al. How urban versus rural population relates to COVID-19 booster vaccine hesitancy: a propensity score matching design study. Human Vaccines Immunother. 2024;20(1):2297490. doi:10.1080/21645515.2023.2297490.
- Okwaraji YB, Mulholland K, Schellenberg JRMA, Andarge G, Admassu M, Edmond KM. The association between travel time to health facilities and childhood vaccine coverage in rural Ethiopia. A community based cross sectional study. BMC Public Health. 2012;12(1):476. doi:10.1186/1471-2458-12-476.
- Wu J, Li Q, Silver TC, Wang M, Gu J, Wei W, Ma M, Zhao L, Mu Z, Miao Y. COVID-19 vaccine hesitancy among Chinese population: a large-scale national study. Front Immunol. 2021;12:781161. doi:10.3389/fimmu.2021.781161.
- Smith PJ, Santoli JM, Chu SY, Ochoa DQ, Rodewald LE. The association between having a medical home and vaccination coverage among children eligible for the vaccines for children program. Pediatrics. 2020;116(1):130–9. doi:10.1542/peds.2004-1058.
- Coccia M. COVID-19 vaccination is not a sufficient public policy to face crisis management of next pandemic threats. Public Organiz Rev. 2023;23(4):1353–67. doi:10.1007/s11115-022-00661-6.
- Magazzino C, Mele M, Coccia M. A machine learning algorithm to analyse the effects of vaccination on COVID-19 mortality. Epidemiol Infect. 2022;150:e168. doi:10.1017/S0950268822001418.
- Chew NWS, Cheong C, Kong G, Phua K, Ngiam JN, Tan BYQ, Wang B, Hao F, Tan W, Han X, et al. An Asia-Pacific study on healthcare workers’ perceptions of, and willingness to receive, the COVID-19 vaccination. Int J Infect Dis. 2020;106:52–60. doi:10.1016/j.ijid.2021.03.069.
- Schwarzinger M, Watson V, Arwidson P, Alla F, Luchini S. COVID-19 vaccine hesitancy in a representative working-age population in France: a survey experiment based on vaccine characteristics. Lancet Public Health. 2021;6(4):e210–21. doi:10.1016/S2468-2667(21)00012-8.
- Hassan MM, Ameeq M, Fatima L, Naz S, Sikandar SM, Kargbo A, Abbas S. Assessing socio-ecological factors on caesarean section and vaginal delivery: an extended perspective among women of South-Punjab, Pakistan. J Psychosom Obstet Gynaecol. 2023;44(1):2252983. doi:10.1080/0167482X.2023.2252983.
- Biswas RK, Afiaz A, Huq S, Farzana M, Kabir E. Public opinion on COVID-19 pandemic in Bangladesh: disruption to public lives and trust in government’s immunisation performance. Int J Health Plann Manage. 2024;39(1):119–34. doi:10.1002/hpm.3721.
- Giannouchos TV, Li Z, Hung P, Li X, Olatosi B. Rural-urban disparities in hospital admissions and mortality among patients with COVID-19: evidence from South Carolina from 2021–2022. J Community Health. 2023;48(5):824–33. doi:10.1007/s10900-023-01216-6.
- Mayuzumi Y. After the COVID-19 pandemic, are residents in rural areas happier than those in urban areas? Asia-Pac J Reg Sci. 2023;7(4):1055–90. doi:10.1007/s41685-023-00312-8.
- Thaker J, Floyd B. Shifting COVID-19 vaccine intentions in New Zealand: next steps in the vaccination campaign. Lancet Reg Health West Pac. 2021;15:100278. doi:10.1016/j.lanwpc.2021.100278.
- Zhong J, Zhong Q, Xiong H, Wu D, Zheng C, Liu S, Zhong Q, Chen Y, Zhang D. Public acceptance of COVID-19 control measures and associated factors during Omicron-dominant period in China: a cross-sectional survey. BMC Public Health. 2024;24(1):543. doi:10.1186/s12889-024-17646-3.
- Weinstein N, Schwarz K, Chan I, Kobau R, Alexander R, Kollar L, Rodriguez L, Mansergh G, Repetski T, Gandhi P. et al. COVID-19 vaccine hesitancy among US adults: safety and effectiveness perceptions and messaging to increase vaccine confidence and intent to vaccinate. Public Health Rep. 2024;139(1):102–11. doi:10.1177/00333549231204419.
- National Bureau of Statistics of China. Communiqué of the seventh national population census (No. 7). [accessed 2024 Apr 11]. https://www.stats.gov.cn/english/PressRelease/202105/t20210510_1817192.html.
- Wang T, Zeng R. Addressing inequalities in China’s health service. Lancet. 2015;386(10002):1441. doi:10.1016/S0140-6736(15)00402-X.
- Wu J, Shen Z, Li Q, Tarimo CS, Wang M, Gu J, Wei W, Zhang X, Huang Y, Ma M, et al. How urban versus rural residency relates to COVID-19 vaccine hesitancy: a large-scale national Chinese study. Soc Sci Med. 2023;320:115695. doi:10.1016/j.socscimed.2023.115695.
- Moore M, Gould P, Keary BS. Global urbanization and impact on health. Int J Hyg Envir Heal. 2003;206(4–5):269–78. doi:10.1078/1438-4639-00223.
- Weiss DJ, Nelson A, Gibson HS, Temperley W, Peedell S, Lieber A, Hancher M, Poyart E, Belchior S, Fullman N, et al. A global map of travel time to cities to assess inequalities in accessibility in 2015. Nature. 2018;553(7688):333–6. doi:10.1038/nature25181.
- Kulu H, Dorey P. Infection rates from covid-19 in Great Britain by geographical units: a model-based estimation from mortality data. Health & Place. 2021;67:102460. doi:10.1016/j.healthplace.2020.102460.
- Cameron RL, Kavanagh K, Pan J, Love J, Cuschieri K, Robertson C, Ahmed S, Palmer T, Pollock KGJ. Human papillomavirus prevalence and herd immunity after introduction of vaccination program, Scotland, 2009–2013. Emerg Infect Dis. 2016;22(1):56–64. doi:10.3201/eid2201.150736.
- Tabrizi SN, Brotherton JML, Kaldor JM, Skinner SR, Liu B, Bateson D, McNamee K, Garefalakis M, Phillips S, Cummins E, et al. Assessment of herd immunity and cross-protection after a human papillomavirus vaccination programme in Australia: a repeat cross-sectional study. Lancet Infect Dis. 2014;14(10):958–66. doi:10.1016/S1473-3099(14)70841-2.
- An Z, Wang F, Pan A, Yin Z, Rodewald L, Feng Z. Vaccination strategy and challenges for consolidating successful containment of COVID-19 with population immunity in China. BMJ. 2021;375:e066125. doi:10.1136/bmj-2021-066125.
- Veronese N, Saccaro C, Demurtas J, Smith L, Dominguez LJ, Maggi S, Barbagallo M. Prevalence of unwillingness and uncertainty to vaccinate against COVID-19 in older people: a systematic review and meta-analysis. Ageing Res Rev. 2022;72:101489. doi:10.1016/j.arr.2021.101489.
- Rahman IU, Austin A, Nelson N. Willingness to COVID-19 vaccination: empirical evidence from EU. Heliyon. 2023;9(5):e15776. doi:10.1016/j.heliyon.2023.e15776.
- Wang G, Yao Y, Wang Y, Gong J, Meng Q, Wang H, Wang W, Chen X, Zhao Y. Determinants of COVID-19 vaccination status and hesitancy among older adults in China. Nat Med. 2023;29(3):623–31. doi:10.1038/s41591-023-02241-7.
- Yang J, Zheng W, Shi H, Yan X, Dong K, You Q, Zhong G, Gong H, Chen Z, Jit M, et al. Who should be prioritized for COVID-19 vaccination in China? A descriptive study. BMC Med. 2021;19(1):45. doi:10.1186/s12916-021-01923-8.
- Ding D, Zhang R. China’s COVID-19 control strategy and its impact on the global pandemic. Front Public Health. 2022;10:857003. doi:10.3389/fpubh.2022.857003.
- Milošević ĐJ, Mari S, Vdović M, Milošević A. Links between conspiracy beliefs, vaccine knowledge, and trust: anti-vaccine behavior of Serbian adults. Social Science & Medicine. 2021;277:113930. doi:10.1016/j.socscimed.2021.113930.
- de Figueiredo A, Simas C, Karafillakis E, Paterson P, Larson HJ. Mapping global trends in vaccine confidence and investigating barriers to vaccine uptake: a large-scale retrospective temporal modelling study. Lancet. 2020;396(10255):898–908. doi:10.1016/S0140-6736(20)31558-0.
- Wu J, Xia Q, Miao Y, Yu C, Tarimo CS, Yang Y. Self-perception and COVID-19 vaccination self-efficacy among Chinese adults: a moderated mediation model of mental health and trust. J Affect Disord. 2023;333:313–20. doi:10.1016/j.jad.2023.04.047.
- Cai J, Deng X, Yang J, Sun K, Liu H, Chen Z, Peng C, Chen X, Wu Q, Zou J, et al. Modeling transmission of SARS-CoV-2 omicron in China. Nat Med. 2022;28(7):1468–75. doi:10.1038/s41591-022-01855-7.
- Sturgis P, Brunton-Smith I, Jackson J. Trust in science, social consensus and vaccine confidence. Nat Hum Behav. 2021;5(11):1528–34. doi:10.1038/s41562-021-01115-7.
- Toledo-López A, Leyva-Hernández SN, Jiménez-Castañeda JC, Avendaño-Rito MDC. Determinants for COVID-19 vaccination intention in Mexico. Heliyon. 2023;9(8):e18079. doi:10.1016/j.heliyon.2023.e18079.
- Van Oost P, Yzerbyt V, Schmitz M, Vansteenkiste M, Luminet O, Morbée S, Van den Bergh O, Waterschoot J, Klein O. The relation between conspiracism, government trust, and COVID-19 vaccination intentions: the key role of motivation. Soc Sci Med. 2022;301:114926. doi:10.1016/j.socscimed.2022.114926.