ABSTRACT
To investigate the dynamic evolution of vaccine hesitancy toward both COVID-19 and influenza in a context characterized by the compresence of SARS-CoV-2 pandemic and seasonal flu epidemics, a two times repeated cross-sectional exploratory design was performed at Udine Hospital (Italy) following a cohort of 479 adult patients with a previous history of SARS-CoV-2 infection in 2020. Vaccine attitude was assessed through standardized telephone interviews performed at 12 and 18 months after the acute illness. The first interview reported the success of the 2020/21 seasonal influenza immunization with 46.8% (224/479) of the participants showing a positive attitude, especially the elderly and people with comorbidities (p < .001), but the investigation conducted at 18 months showed a drastic drop in flu shot acceptance (30/166, 18.1%). On the other hand, a great increase in vaccinations against SARS-CoV-2 occurred after the introduction of Green Pass (26.7% vs 72.9%). The major drivers of flu vaccine skepticism were represented by the feeling of protection regardless of prevention and by concerns regarding vaccines safety and efficacy; conversely compulsory strategies seemed to play a secondary role, since only a minority of the participants identified in the restrictions induced by the certification the major incentive to get immunized against SARS-CoV-2. The focus on this peculiar historical period helps to take a step forward in the comprehension of the complexity and dynamicity of the vaccine hesitancy phenomenon. Future vaccination campaigns will need to consider the role of personal opinions and emotions, interpreted according to the social and political context.
Introduction
The experience of COVID-19 pandemic has turned the spotlight on the importance of public health measures and disease prevention. The urgent need to control the spread of the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) infection has accelerated the development of immunization strategies and, on 11 December 2020, the first COVID-19 vaccine was approved by the United States of America Food and Drug Administration.Citation1 In the same period, the seasonal influenza vaccination campaign, known to be the most effective way to protect from infection and to reduce the flu-related morbidity and mortality,Citation2 was taking place in many countries worldwide. Despite the established importance of both of these prevention measures, influenza vaccination uptake has remained low in most nations (and far from the World Health Organization’s target of 75%),Citation3 while misperceptions regarding the efficacy, the safety and the reliability of COVID-19 immunization have grown. Vaccine hesitancy is a well-known worldwide phenomenon, defined by the World Health Organization’s Strategic Advisory Group of Experts (WHO-SAGE) as a reluctance toward vaccination despite its availability.Citation4 It has been identified as one of the top ten global health threats in the 2019 WHO Report,Citation5 as can undermine the efforts of healthcare systems to reach an adequate vaccination coverage in the population.Citation6 The attitudes toward immunization are highly dynamic and have demonstrated to vary in relation with context-specific factors, involving various sociodemographic and individual determinants.Citation7 During worldwide global crisis, as experienced during the pandemics, the complex interaction of vaccine, environmental and host-specific factors may exacerbate skepticism toward immunization.Citation8,Citation9
The Italian context with regard to COVID-19 vaccination campaign
Italy was the first European country hit by SARS-CoV-2 and pandemic dynamics progressively stretched social and political stability in a scenario already fragile.Citation10
COVID-19 vaccination campaign started on 27 December 2020Citation11 and, after a first discretely enthusiastic acceptance of the immunization, an abrupt halt was observed with a decreasing trend in the daily number of vaccine recipients estimated of 39.76%.Citation12 On 30 June 2021, only 57.5% of the total population had received at last one dose of COVID-19 vaccine.Citation12 For the purpose of keeping a level of immunization coverage capable of contrasting the virus circulation, on 23 July 2021 the Italian Government adopted the European Digital Pass strategy, also called Green Pass. It consisted in a certificate that had to be displayed to enable access to all public places – work places included – and to travel.
The certificate was delivered by the Ministry of Health via app to those with recent infection (180 days validity), immunization (1 year validity) or recent negative COVID-test (2–3 days validity).Citation13 This strategy – also adopted by other countries as France, Israel and Denmark – was pursued to avoid the introduction of mandatory SARS-CoV-2 vaccination, based upon the principle that an incentive-based model would have been more tolerated.Citation10 During the first weeks after its entry into effect, Green Pass was heavily emphasized via the news with an immediate rebound on social media; bookings for vaccination skyrocketed and the immunization coverage increased (in the first week of August 2021 the cumulative count of vaccine doses administered since the beginning of the campaign reached the number of 71,071,465).Citation12 Despite the early success of this measure, many people kept their anti-vaccination beliefs and, gradually, concerns regarding the compulsory nature of Green Pass started to rise, threatening the efficacity of this strategy.Citation14 In April 2022 the need of the certificate for access to public places was dismissed, and since December 2022 it has not been required to enter hospitals as a visitor.Citation15 To date 49,526,642 people have received at least one dose of COVID-19 vaccine and 48,725,293 have completed the vaccination cycle (respectively 91.73% and 90.4% of the population over.Citation16
The Italian context with regard to seasonal influenza vaccination campaign
In COVID-19 pandemic time, the seasonal influenza vaccination (SIV) campaign took place in Italy during winters 2020–2021 and 2021–2022, starting in mid-October and ending in the month of February. Immunization was offered free of charge to people older than 60 years, to healthcare workers and to the most fragile part of the population.Citation17 The first campaign made soar the yearly escalation of vaccinal coverage, which had been steadily advancing since 2013. By the end of the winter 2021, 23.7% of the population had received the flu shot, marking an increase of 6.9% in comparison to the previous year. The subsequent SIV campaign 2021–2022 settled the end of this upward trend with a 3.2% decline in the vaccination coverage rate among general population and an even greater collapse when considering the elderly (from 65.3% in 2020–2021 to 58.1% in 2021–2022).Citation18 This trend was registered in all Italy and its determinants are yet to be clearly understood.
On these premises, we investigated the phenomenon of vaccine hesitancy in the complex background in which COVID-19 and influenza vaccination campaigns concurrently took place between 2021 and 2022.
The objective of this work was to close the gap of the unexplained decrease in the success of 2021–2022 SIV campaign. Additionally, it aimed to delineate the significance of compulsory strategies in driving vaccinal decisions and investigate the challenges arising from the potential convergence of the SARS-CoV-2 pandemic and seasonal flu epidemic in social and behavioral terms.
With this purpose, we longitudinally assessed the vaccination attitudes toward COVID-19 and influenza among a cohort of Italian patients that first experienced SARS-CoV-2 infection during the first wave, exploring the reasons behind hesitancy or acceptance. Expanding knowledge may inform the future public health strategies in this field.
Material and methods
Study design
This investigation used a two times repeated cross-sectional exploratory design to assess vaccinal attitude regarding both COVID-19 and influenza vaccination in a cohort of adult patients having in common a medical history of SARS-CoV-2 infection in 2020, during the first pandemic wave. The study was carried out between 2020 and 2022, and it was designed and conducted by the Infection Diseases Unit at the Academic Hospital of Udine (Italy), a tertiary-care teaching hospital (around of 1000 beds) that was also a referral regional center for COVID-19 attending a population of approximately 530,000 inhabitants.
Participants
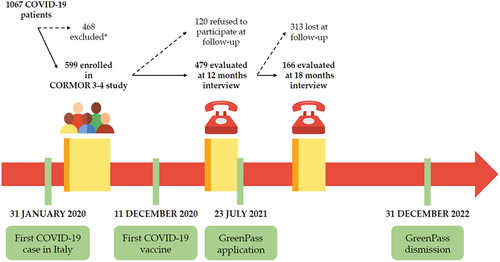
A cohort of adult (older than 18 years) in- and out-patients who had received a diagnosis of SARS-CoV-2 infection between March 2020 and April 2020, during the first COVID-19 pandemic wave, and who had taken part in the CORMOR 3–4 study,Citation19 was firstly assessed in 2021 for vaccinal hesitancy at 6 months after SARS-CoV-2 infection.Citation20 Then the survey was conducted longitudinally, exploring the vaccination hesitancy or willingness at 12 and at 18 months. Eligible patients were those (a) recruited during their first access at the Infectious Disease Department of Udine in March 2020; (b) confirmed as cases of SARS-CoV-2 infection, thus patients with a positive nucleic acid amplification test (NAAT) for SARS-CoV-2 in a respiratory tract specimen; and (c) willing to take part in telephonic interviews conducted at 12 and 18 months following the infection ().
Primary outcome and associate variables
The primary aim of the study was to assess patients’ attitude toward COVID-19 and flu vaccines at 12- and 18-months following SARS-CoV-2 infection. Attitude was considered in terms of expressed hesitancy or willingness to adhere to the vaccination campaign. The secondary aim was to identify factors associated with vaccine hesitancy and willingness.
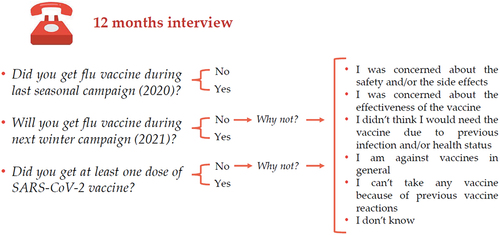
Vaccine attitude was first assessed at 12 months with the following questions “Did you get flu a vaccine during last seasonal campaign?,” “Will you get a flu vaccine next winter?” and “Did you get at least one dose of SARS-CoV-2 vaccine?.” Possible answers were yes/no. In case of negative answer, participants were asked to explain their vaccine hesitancy toward the two vaccines ().
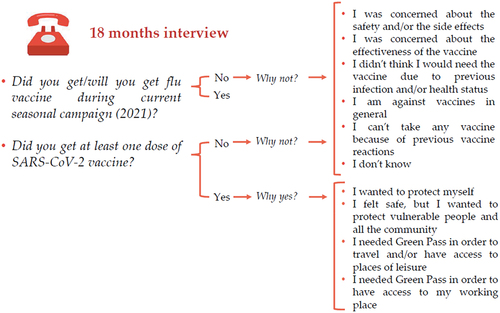
A second interview was taken at 18 months when participants were asked about their attitude toward flu vaccine and SARS-CoV-2 vaccine and were again asked to explain their vaccine hesitancy toward the two vaccines. Moreover, at 18 months participants were also asked to motivate their decision in case of positive attitude toward SARS-CoV-2 vaccine (). Since in December, the SIV campaign 2021 had not been completed, a positive answer to one of the two questions “did you get flu vaccine during current campaign?” or “will you get flu vaccine during current campaign?” was considered as an expression of vaccine acceptance.
In delineating the variables to correlate with diverse vaccination attitudes, our primary focus was on assessing the influence of previous SARS-CoV-2 infection and the presence of comorbidities. These factors were considered as potential indicators of fragility that might affect behavior toward vaccination. In terms of sociodemographic factors, we included certain variables already acknowledged as major determinants of vaccine acceptance (such as age, gender, nationality and occupation, with specific consideration given to people working in contact with public healthcare workers).Citation21 Furthermore, we aimed to incorporate smoking habit as one of the variables, to investigate potential associations between this behavior and predisposition toward vaccination.
Procedures and data collection
All eligible patients were contacted by phone by trained nurses in two different occasions, approximately in May 2021 and in December 2021. The first interview took place 12 months following participants’ SARS-CoV-2 first infection, at the end of 2020–2021 flu vaccination campaign and before Green Pass introduction. The second interview took place 18 months following participants’ SARS-CoV-2 first infection, during the 2021–2022 flu vaccination campaign and during the period when Green Pass was widely in use. We developed and pilot tested an interview guide investigating vaccine hesitancy (). In the pilot phase, conducted during the first data collection, the understandability was assessed among 10 patients and no changes were requested. The interview was also considered feasible given that lasted about 15 min. In the first interview, patients were left free to answer with their own words and to provide justifications for their vaccine attitude/hesitancy; in the second interview, the categorization of reasons emerged in the previous interview was used to structure the questions, converting open-ended into close-ended queries ().Citation20 Clinical data collected during the follow-up were extracted from the General Hospital databases, using a standardized protocol.
Nurses involved in the interview process were all advanced educated at the Master’s or at the PhD level; they were all supervised in the first five interviews by an expert researcher to ensure homogeneity and quality in the data collection process.
Ethical issues
All procedures were in accordance with the ethical standards of the University of Udine and Azienda Sanitaria Universitaria Friuli Centrale (CEUR-2020-OS-219/CEUR-2020-OS-205) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Verbal informed consent was obtained from all subjects before being contacted for the interview.
Statistical analysis and sample size
Vaccination coverage in Friuli Venezia Giulia during the latest seasonal influenza vaccination campaign has been 20%.Citation18 A sample size of 479 patients allowed to produce a two-sided 95% confidence interval of this proportion with a 3.7% precision.
Descriptive statistics included frequency analyses (percentages) for categorical variables and mean (standard deviation; SD), median and interquartile range (IQR) for quantitative variables. After the first interview, the open-ended answers concerning the vaccine attitudes/hesitation were categorized by the research team. This entailed the participation of three investigators, comprising members of the clinical infectious disease unit and the nursing team. Each of them conducted an independent analysis of the answers and categorized them though a content analysis process.Citation22 Subsequently, the findings were compared and any discordant interpretations were resolved through collaborative discussion. The resulting categorizations emerged in this initial phase served as the framework for the subsequent data collection, facilitating a comparative examination of the participants’ answers ().
Data were tested for normal distribution using the Shapiro – Wilk test. Patients were stratified by age (intervals 18–40, 40–60, >60 years old), nationality, occupation, smoking habits, presence of comorbidities, symptomatic COVID-19, hospital admission and presence of symptoms at 12 months. To explore vaccine hesitancy, the Chi-square (χ2) test or Fisher test were used to compare categorical variables among groups, as appropriate. Student t-test or Mann-Whitney U test were used to compare continuous variables among groups, depending on whether data were normally or non-normally distributed. Furthermore, a univariable and multivariable logistic regression was performed to explore variables associated to vaccine willingness, estimating the odds ratios and interval of confidence (OR; 95% CI). In the multivariable case a stabilized inverse censoring weight was considered, to address the bias of the patients lost between the 12 and 18-month follow-up.
Analyses were performed using STATA 17. A p-value <.05 was considered significant.
Results
Baseline characteristics of the population
Out of the 599 patients enrolled in the CORMOR 3–4 study,Citation19 479 patients answered the interview at 12 months (participation rate of 79.9%) and 166 of them completed the survey at 18 months (34.7%). Baseline demographic and clinical characteristics of the population are summarized in and in .
Table 1. Demographic characteristics of the study population.
Table 2. Main clinical characteristics of acute SARS-CoV2 infection of the study population.
In brief, 252/479 (52.6%) were female and the mean age was 53 (SD = 15). People working in contact with public accounted for 42.0% (186/443) of the respondents and 19.1% (81/443) were retired. About one half of the patients (249/479, 52.0%) reported at least one chronic medical condition and 47.2% (226/479) were still reporting presence of SARS-CoV-2 related symptoms at 12 months after the primary illness.
Attitude towards influenza vaccine at the first interview (12 months interview)
Overall, almost half of the respondents (210/479, 43.8%) reported having received the seasonal influenza immunization during winter 2020–2021 and, at the time of the first interview, nearly the same percentage (224/479, 46.8%) was motivated to undertake immunization again ().
Table 3. Attitudes toward influenza vaccination and COVID-19 vaccination at 12 months and at 18 months.
As shown in , a positive attitude toward vaccination was significantly associated with older age (57.6% > 60 years vs. 10.5% 18–40 years; p-value <.001), comorbidities (65.1% favorable vs. 42.6% hesitant; p-value <.001) and Body Max Index (BMI) (median 25.6 in favorable vs. 24.7 in hesitant, p-value 0.011); moreover, being retired was found to be a predictor of willingness to get influenza immunization (31.5% favorable vs. 7.7% hesitant; p-value <.001). On the other side, people whose job did not involve being in contact with public were more likely to refuse seasonal vaccination (38.1% favorable vs. 45.1% hesitant; p-value <.001). Gender and smoking habits did not show any association with influenza vaccine acceptance.
Table 4. Demographic characteristics of the study cohort according to their attitudes toward influenza vaccination at 12 months and at 18 months.
In relation to the clinical course of COVID-19, reports that only admission to ICU during the acute infection emerged as a factor promoting vaccine acceptance (p-value <.001); neither the presence of a symptomatic acute infection nor the development of post-COVID-19 syndrome shown a significant association with a positive attitude toward vaccination.
Table 5. Characteristics of acute SARS-CoV-2 infection in the study cohort according to their attitudes toward influenza vaccination at 12 months and at 18 months.
shows the reasons of hesitancy reported by those who declared to be unwilling to vaccinate against influenza in the future. The main motivation reported was the feeling of being protected – even without immunization – because of self-perceived good health status (135/200, 67.5%); only a small percentage expressed concern about the safety or the effectiveness of the vaccine (respectively 6.5% and 4.5%).
Table 6. Reasons for vaccine hesitancy.
Attitude towards influenza vaccine at the second interview (18 months interview)
At 18 months interview, a decrease in influenza vaccination acceptance was registered: only 18.1% (30/166) out of the total reported to be favorable, while the majority declared to be unwilling to be immunized.
Similarly, to the 12 months survey, a strong statistical association was found between vaccine acceptance and older age, presence of comorbidities or being retired (p-value <.05 in all cases). Among people working in contact with public, a significant proportion of vaccination refusal was registered (30% likely vs. 46.9% unlikely; p-value <.001).
No association emerged between influenza vaccine hesitancy and the clinical characteristics of acute COVID-19 infection, except for hospital admission at 12 months interview ().
As in the previous interview, the main motivation for refusal was the feeling of being protected without the need of a vaccine (72/129, 55.8%) but, at 18 months survey, a higher percentage (30/129, 23.3%) resulted skeptical about the effectiveness of the influenza vaccination ().
Attitude towards SARS-CoV2 vaccine at the first interview (12 months interview)
At the interview performed 12 months after acute COVID-19 illness, only 27.6% (132/479) reported to be vaccinated against SARS-CoV2, while the great majority of the population was hesitant.
From the analysis of the reasons for refusal (), it emerged that 56% of the participants unwilling to be vaccinated were afraid that the vaccine could have dangerous side effects; another heartfelt reason was the idea that the vaccine was unnecessary, due to previous infection, health status or age (20.0%).
Attitude towards SARS-CoV2 vaccine at the second interview (18 months interview)
The great majority of the interviewed (121/166, 72.9%) reported receipt of COVID-19 immunization at 18 months survey. Among the minority of reluctant, the main motivation for refusal was the feeling of being protected without the need of a vaccine (22/45, 48.9%).
Considering the participants with a positive attitude toward vaccination, the main reason for vaccine acceptance was the declared will to protect themselves and the community (90/121, 74.5%), while a minority (27/121, 22.3%) reported as a motivation the need to obtain Green Pass in order to have access to working and leisure places.
shows the general characteristics of the population according to the rationale that stimulated them to vaccinate; no significative associations were found between participants’ demography, habits, comorbidities or severity of the primary SARS-CoV-2 illness and the decision to be immunized because of the need to obtain Green Pass rather than the will to protect themselves and the community. The only characteristic that was proved to influence the reason behind the vaccine acceptance was to have a job, as all the participants who declared to have undertaken vaccination because of need of Green Pass were workers (100.0%; 52.0% working in contact with public, 44.0% doing works not in contact with public and 4.0% doing unspecified kind of works; p-value 0.007).
Table 7. Demographic characteristics of the study cohort according to the reason reported regarding vaccine acceptance.
Discussion
The main purpose of this research was to investigate the evolution over time of vaccinal attitudes toward influenza and SARS-CoV-2 - respectively the main epidemic and pandemic diseases co-existing in current times – in people who had experienced COVID-19 infection during the first and most impactful pandemic wave.
Some significant results emerged from our investigation: (i) self-perception of being at risk was directly correlated with the uptake of influenza vaccination, while the main reason given by participants to justify refusal of the influenza vaccine was the perception of being adequately protected without the necessity of vaccination; (ii) high adherence rates were reported during 2020–2021 seasonal influenza vaccination campaign, followed by a notable decline in influenza vaccine acceptance during the subsequent winter, likely due to the underestimation of the issue (attributable to reduced flu virus circulation and tendency to overshadowing diseases others than COVID-19) and the spreading of mistrust in vaccines; (iii) a great increase in the number of people vaccinated against SARS-CoV-2 occurred after the introduction of Green Pass, even if the great majority of the interviewed declared other reasons guiding their choice and no significative correlations were founded between the characteristics of the population and the reason behind their vaccine acceptance.
Self-perception as a potential driver of tendences towards influenza vaccination
As defined by Osterholm et al., vaccine hesitancy is a dynamic and complex issue which declines in a context-specific way depending on time, place and type of vaccine considered.Citation23
With respect to influenza vaccination, within our cohort we observed that people in favor of flu vaccination were predominantly elderly and those with chronic illnesses (68.4% aged 60 or older vs. 22.9% between 18 and 40 years and 54.6% with underlying diseases vs. 32.7% without), in line with data provided by the Italian Ministry of Health regarding the 2020–2021 SIVCitation13 and with findings emerged from surveys conducted in Italy in the same period.Citation24,Citation25 A positive correlation between flu vaccination uptake and the most vulnerable part of the population was expected, given that immunization is routinary offered to these categories due to its established effectiveness in preventing morbidity and mortality.Citation25,Citation26 Furthermore, an increased level of vaccine acceptance was observed among subjects with BMI exceeding 25. This is consistent with the evidence coming from a survey in obese population conducted by Harris et al.Citation27 and could be attributed to the perception of increased vulnerability and, consequently, higher risk for influenza complications.Citation28 The potential role of fear in promoting preventive attitudes was investigated by Cori et al., with particular emphasis on the role of COVID-19 concern in driving influenza vaccine uptake.Citation29 The findings from our research support this evidence, since we found a positive correlation between admission to ICU during acute SARS-CoV-2 infection and influenza immunization acceptance (p-value <.001). Moreover, the rate of flu vaccination coverage observed in our cohort is outstandingly higher when compared to official Italian data reported for the successful 2020–2021 influenza vaccination campaign (48.3% vs. 23.7%).Citation18 We propose that this disparity may be attributed to the baseline characteristic of our sample, wherein all participants shared a common medical history of previous SARS-CoV-2 infection during the first pandemical wave, recognized as the most severe and impactful. Expanding upon this discrepancy, it is pertinent to highlight that other surveys conducted in Italy concerning vaccine compliance throughout the 2020–2021 season reported higher coverage rate compared to national statistics.Citation24 In this context, our assessments of influenza vaccine uptake closely match the results of a study undertaken in two metropolitan cities in Italy in the same timeframe, which documented a 47.3% willingness among respondents to receive influenza vaccination.Citation30 Furthermore, considering the geographical aspect, noteworthy variations were observed among different regions of Italy in terms of vaccine acceptance, with percentages ranging from 17.9% to 31.3%, according to national estimates.Citation17 Our research was conducted in Friuli Venezia Giulia, a region that ranked among those with the highest rate of vaccine acceptance in the 2020–2021 period.Citation17
Whether the consciousness of being at risk is well recognized as a significant motivating factor in choosing vaccination, also the reverse association between low perceived risk and vaccine hesitancy is well established.Citation24,Citation31,Citation32 Evidence supporting this assertion can be identified within our survey as well. The primary rationale provided by our respondents to justify their refusal to vaccination was the feeling of being protected even without immunization, stemming from a positive self-perception of their health status.
Exploring the reasons behind the fall in SIV confidence during winter 2021–2022
The data collected during our second interview (performed during 2021–2022 SIV campaign) revealed a significant shift in attitude toward seasonal influenza immunization compared to the data gathered from interviews conducted with the same sample at 6Citation20 and 12 months after SARS-CoV-2 acute illness. According to our estimates, the percentage of people prone to be vaccinated in December 2021 was only 18.1% and was similar to the rate of 20.5% reported in the whole Italian population in the same period.Citation18
To the best of our knowledge, at present, there is no literature exploring the reasons for this fall in SIV confidence among Italians. The participants to our survey explained their hesitancy using quite the same motivations given six months before, however a great increase in concerns regarding side effects and vaccine ineffectiveness was observed. This skepticism is in line with similar studies conducted at the same timeCitation28,Citation33,Citation34 and could be related to conspiracy theories and lack of trust in the healthcare system that spread with unprecedent speed during the COVID-19 pandemic.Citation32,Citation35 In parallel, the polarization of the vaccination campaigns toward SARS-CoV-2 and the media monopolization by COVID-19 advocacy contributed to overshadowing the importance of other infectious diseases.Citation36 The underestimation of influenza might have been also driven by the declined circulation of the virus itself, due to the implementation of behavioral protective measures (face masks, physical distancing and movement restrictions) adopted to control the spread of SARS-CoV-2.Citation36 Finally, in December 2021, the Green Pass had already been in force for several months, this probably contributing to the growth of hatred for vaccination campaigns among the population.Citation14 As suggested by Mills and Rüttenauer, COVID-19 certification is a part of multiple policy levers that could be adopted to counter vaccine hesitancy, but has to be used with caution according to the context, because of the risk of ending in increased complacency.Citation37
Exploring the assumed incentive role of the Green Pass towards SARS-CoV-2 vaccination
With the present study, we highlighted a significant increase in SARS-CoV2 vaccination confidence in the interview performed in December 2021, as compared to the one performed before the introduction of Green Pass and same results have been obtained in surveys conducted in other European countries in the same period.Citation37 Surprisingly, it emerged from our work that the leading motivation declared by respondents to explain their immunization confidence was the will to protect themselves and the community, rather than the need to obtain the certification. These findings are in contrast with data coming from similar Italian studiesCitation38 and could be explained by the fact that our interviews were performed by healthcare workers, this having potentially driven the answers through altruism or health anxiety feelings rather than to the fear of social limitation. In our survey, no significant association was found between the reason behind the vaccine acceptance and the characteristics of COVID-19 previous infection or the socio-demographic characteristics of the participants. The only factor significantly linked to the will of Green Pass as an incentive for vaccination was to have a job, as it is intuitively logical. The above can be interpreted as a further demonstration that the direct association observed between Green Pass and SARS-CoV-2 vaccine uptake should be carefully interpreted considering the context and the pandemic trajectory.
Limitations and further research
In displaying our results, it is certainly necessary to consider the different limitations and discuss the strengths of the present investigation.
The first limitation of this work resides in its non-anonymous nature and in the fact that the interviews were performed by healthcare workers; this could have introduced a bias in the answers given by the participants. Secondly, in our study we had a drop off rate of about 30% at 12 months and 65% at 18 months. Although dropout in longitudinal studies in common (range 30–70%),Citation39 it has determined a suboptimal response rate and significative differences in the occupation status and comorbidities among the participants. The failure in completing the survey may have been due to the unavailability of the people during phone calls or to the loss of interest in the project once COVID-19 fear was gradually disappearing. Moreover, no compensation was provided to the survey participants, and this may have further diminished the appeal. Although we had a justifiable sample size to provide enough statistical power, a larger sampling would have strengthened our observation, especially at 18 months interview.
Another weakness in the design of our study consists in the fact that the educational level and the socioeconomic status – defined in other studies as major determinants of vaccine uptake during the pandemic period,Citation40 were not assessed. Moreover, the investigation of attitudes toward Green Pass strategy and the correlation of these data with vaccine tendency and demographic characteristics would have provide further elements to discuss the role of the Green Pass; unfortunately, this data were not assessed.
The second interview took place in December 2021, when the SIV 2021–2022 was not yet concluded. Vaccine tendency was evaluated asking the participants if they had already got a flu vaccine; in case of negative answer, they were asked about the intention to get it before the end of the campaign. Vaccination acceptance was defined by a positive answer to any of these two questions; no data regarding the actual completion of vaccination have been collected.
From a geographical perspective, this study was conducted within a single hospital, thus representing a small geographic area. On one side, this constitutes a limitation as it constrains reproducibility, yet on the other, it aligns with vaccine hesitancy as a context-dependent concept.
The main strength of this work resides in the parallel investigation, during the same interview, of tendency toward influenza and SARS-CoV-2 vaccination, considering vaccine hesitancy as a context-dependent phenomenon. Moreover, the shared common medical history of SARS-CoV-2 infection during the spring of 2020 – although it could be considered as a source of selection bias – enables us to focus on a peculiar category of population, due to the cruciality of the first pandemic wave in terms of physical, psychological and social impact.
Finally, the simplicity of the design of this study makes it easily reproducible and provides us with a clear and immediate epidemiological information.
Considering the phenomenon of vaccine hesitancy in a dynamic prospective, further efforts are needed to identify the interventions capable of promoting confidence in vaccines, by strengthening trust in the healthcare system and disrupting negative myths.
Overcoming vaccine hesitancy remains one of the main current public health challenges. The reasons behind the different choices made by the population are multiple – sometimes conflicting – and difficult to outline and summarize. Osterholm et al. have elaborated a context-specific explanation of vaccine hesitancy;Citation23 we suggest incorporating in this definition the role of the single subject, as recipient of the vaccine and protagonist of the context.
In this perspective, the findings coming from our research could help to achieve a better understanding of the evolution of vaccine hesitancy during the time of the COVID-19 pandemic, thus, to improve public health strategies.
Author contributions statement
Conceptualization, Valentina Gerussi, Maddalena Peghin, Alvisa Palese and Miriam Isola; Methodology, Maria De Martino and Miriam Isola; Software, Maria De Martino and Miriam Isola; Validation, Alvisa Palese; Formal analysis, Maria De Martino; Investigation, Alvisa Palese and Miriam Isola; Data curation, Valentina Gerussi, Elena Graziano, Stefania Chiappinotto, Federico Fonda, Giulia Bontempo, Tosca Semenzin and Luca Martini; Writing – original draft, Valentina Gerussi and Maria De Martino; Writing – review & editing, Maddalena Peghin, Alvisa Palese, Elena Graziano, Miriam Isola and Carlo Tascini; Visualization, Carlo Tascini; Supervision, Maddalena Peghin and Alvisa Palese; Project administration, Carlo Tascini.
All authors have approved the final article. All authors attest they meet the ICMJE criteria for authorship.
Acknowledgments
We would like to thank all the participants in this survey. We would also like to thank all the nurses who helped us in performing the interviews. Despite the hard period and the great amount of work, they found time for supporting us with their efficient and professional help.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data presented in this study are available on reasonable request from the corresponding author, M.P. The data are not publicly available due to privacy concerns.
Additional information
Funding
References
- U.S. Food and Drug Administration. COVID-19 vaccines. 2024 Apr 29. https://www.fda.gov/emergency-preparedness-and-response/coronavirus-disease-2019-covid-19/covid-19-vaccines.
- Petrova VN, Russell CA. The evolution of seasonal influenza viruses. Nat Rev Microbiol. 2018;16(1):47–11. doi:10.1038/nrmicro.2017.118.
- Jorgensen P, Mereckiene J, Cotter S, Johansen K, Tsolova S, Brown C. How close are countries of the WHO European region to achieving the goal of vaccinating 75% of key risk groups against influenza? Results from national surveys on seasonal influenza vaccination programmes, 2008/2009 to 2014/2015. Vaccine. 2018;36(4):442–52. doi:10.1016/j.vaccine.2017.12.019.
- World Health Organization. Report of the strategic advisory group of experts on immunization working group on vaccine hesitancy. 2024 Apr 29. https://www.who.int/docs/default-source/immunization/demand/summary-of-sage-vaccinehesitancy-en.pdf?sfvrsn=abbfd5c8_2.
- World Health Organization. Ten Threats to global health in 2019. 2024 Apr 29. https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019.
- World Health Organization. Barriers of influenza vaccination intention and behavior: a systematic review of influenza vaccine hesitancy 2005–2016. 2016 [accessed 2024 Jan 23]. https://apps.who.int/iris/handle/10665/251671.
- AlJamaan F, Temsah MH, Alhasan K, Alenezi S, Alhaboob A, Alrabiaah A, Batais M, Alshahrani F, Assiri RA, Bafaqih H. et al. SARS-CoV-2 variants and the global pandemic challenged by vaccine uptake during the emergence of the Delta variant: A national survey seeking vaccine hesitancy causes. J Infect Public Health. 2022;15(7):773–80. doi:10.1016/j.jiph.2022.06.007.
- Pertwee E, Simas C, Larson HJ. An epidemic of uncertainty: rumors, conspiracy theories and vaccine hesitancy. Nat Med. 2022;28(3):456–9. doi:10.1038/s41591-022-01728-z.
- Domnich A, Cambiaggi M, Vasco A, Maraniello L, Ansaldi F, Baldo V, Bonanni P, Calabrò GE, Costantino C, de Waure C. et al. Attitudes and beliefs on influenza vaccination during the COVID-19 pandemic: results from a representative Italian survey. Vaccines. 2020;8(4):711. doi:10.3390/vaccines8040711.
- Stefanizzi P, Bianchi FP, Brescia N, Ferorelli D, Tafuri S. Vaccination strategies between compulsion and incentives. The Italian green pass experience. Expert Rev Vaccines. 2022;21(4):423–5. doi:10.1080/14760584.2022.2023012.
- Italian Ministry of Health. Public health Italy. 2024 Apr 29. https://www.salute.gov.it/portale/home.html.
- Commissario straordinario per l’emergenza COVID-19 - Presidenza del Consiglio dei Ministri. COVID-19 opendata vaccini. 2024 Apr 29. https://github.com/italia/covid19-opendata-vaccini.
- European Parliament. Regulation (EU) 2021/953 of the European parliament and of the Council of 14 June 2021 on a framework for the issuance, verification and acceptance of interoperable COVID-19 vaccination, test and recovery certificates (EU Digital COVID Certificate) to facilitate free movement during the COVID-19 pandemic. 2021 [2024 Apr 29]. http://data.europa.eu/eli/reg/2021/953/oj.
- De Giorgio A, Kuvačić G, Maleš D, Vecchio I, Tornali C, Ishac W, Ramaci T, Barattucci M, Milavić B. Willingness to receive COVID-19 booster vaccine: associations between green-pass, social media information, anti-vax beliefs, and emotional balance. Vaccines. 2022;10(3):481. doi:10.3390/vaccines10030481.
- Italian Government. Decreto-legge 24 marzo 2022 Misure urgenti per il superamento delle misure di contrasto alla diffusione dell’epidemia da COVID-19, in conseguenza della cessazione dello stato di emergenza. 2022 [accessed 2024 Apr 29]. https://www.gazzettaufficiale.it/eli/id/2022/03/24/22G00034/sg.
- Italian Government. Report vaccini anti-COVID-19. 2024 Apr 29. https://www.governo.it/it/cscovid19/report-vaccini/.
- Istituto Superiore di Sanità. Le vaccinazioni in Italia. 2024 Apr 29. https://www.epicentro.iss.it/vaccini/dati_Ita#flu.
- Italian Ministry of Health. Vaccinazione antinfluenzale. Tavole. 2024 Apr 29. https://www.salute.gov.it/imgs/C_17_tavole_19_3_1_file.pdf.
- Peghin M, Bouza E, Fabris M, De Martino M, Palese A, Bontempo G, Graziano E, Gerussi V, Bressan V, Sartor A. et al. Low risk of reinfections and relation with serological response after recovery from the first wave of COVID-19. Eur J Clin Microbiol Infect Dis. 2021;40(12):2597–604. doi:10.1007/s10096-021-04335-x.
- Gerussi V, Peghin M, Palese A, Bressan V, Visintini E, Bontempo G, Graziano E, De Martino M, Isola M, Tascini C. et al. Vaccine hesitancy among Italian patients recovered from COVID-19 infection towards Influenza and Sars-Cov-2 vaccination. Vaccines. 2021;9(2):9. doi:10.3390/vaccines9020172.
- Joshi A, Kaur M, Kaur R, Grover A, Nash D, El-Mohandes A. Predictors of COVID-19 vaccine acceptance, intention, and hesitancy: a scoping review. Front Public Health. 2021;9:698111. doi:10.3389/fpubh.2021.698111.
- Vaismoradi M, Turunen H, Bondas T. Content analysis and thematic analysis: implications for conducting a qualitative descriptive study. Nursing & Health Sciences. 2013;15(3):398–405. doi:10.1111/nhs.12048.
- Osterholm MT, Kelley NS, Sommer A, Belongia EA. Efficacy and effectiveness of influenza vaccines: a systematic review and meta-analysis. Lancet Infect Dis. 2012;12:36–44. doi:10.1016/s1473-3099(11)70295-x.
- Giacomelli A, Galli M, Maggi S, Noale M, Trevisan C, Pagani G, Antonelli-Incalzi R, Molinaro S, Bastiani L, Cori L. et al. Influenza vaccination uptake in the general Italian population during the 2020–2021 flu season: data from the EPICOVID-19 online web-based survey. Vaccines. 2022;10(2):293. doi:10.3390/vaccines10020293.
- Lorini C, Lastrucci V, Zanella B, Gori E, Chiesi F, Bechini A, Boccalini S, Del Riccio M, Moscadelli A, Puggelli F. et al. Predictors of influenza vaccination uptake and the role of health literacy among health and social care volunteers in the province of Prato (Italy). Int J Environ Res And Public Health. 2022;19(11):6688. doi:10.3390/ijerph19116688.
- World Health Organization. Regional office for Europe. Methods for assessing influenza vaccination coverage in target groups. 2016 [accessed 2024 Apr 29]. https://apps.who.int/iris/handle/10665/345696.
- Harris JA, Moniz M, Lott B, Power R, Griggs JJ. Obesity and the receipt of influenza and pneumococcal vaccination: a systematic review and meta-analysis. BMC Obes. 2016;3(1):24. doi:10.1186/s40608-016-0105-5.
- Kharroubi G, Cherif I, Bouabid L, Gharbi A, Boukthir A, Ben Alaya N, Ben Salah A, Bettaieb J. Influenza vaccination knowledge, attitudes, and practices among Tunisian elderly with chronic diseases. BMC Geriatr. 2021;21(1):700. doi:10.1186/s12877-021-02667-z.
- Cori L, Curzio O, Adorni F, Prinelli F, Noale M, Trevisan C, Fortunato L, Giacomelli A, Bianchi F. Fear of COVID-19 for individuals and family members: indications from the national cross-sectional study of the EPICOVID19 web-based survey. Int J Environ Res And Public Health. 2021;18(6):3248. doi:10.3390/ijerph18063248.
- Montalti M, Di Valerio Z, Rallo F, Squillace L, Costantino C, Tomasello F, Mauro GL, Stillo M, Perrone P, Resi D. et al. Attitudes toward the SARS-CoV-2 and influenza vaccination in the metropolitan cities of Bologna and Palermo, Italy. Nato Adv Sci Inst Se. 2021;9(10):1200. doi:10.3390/vaccines9101200.
- Langer R, Thanner M. Pharmacists’ attitudes toward influenza vaccination: does the COVID-19 pandemic make a difference? Explor Res Clin Soc Pharm. 2023;9:100235. doi:10.1016/j.rcsop.2023.100235.
- Arda B, Durusoy R, Yamazhan T, Sipahi OR, Taşbakan M, Pullukçu H, Erdem E, Ulusoy S. Did the pandemic have an impact on influenza vaccination attitude? A survey among health care workers. BMC Infect Dis. 2011;11(1):87. doi:10.1186/1471-2334-11-87.
- Kwong EW, Lam IO, Chan TM. What factors affect influenza vaccine uptake among community-dwelling older Chinese people in Hong Kong general outpatient clinics? J Clin Nurs. 2009;18:960–71. doi:10.1111/j.1365-2702.2008.02548.x.
- McIntyre A, Zecevic A, Diachun L. Influenza vaccinations: older adults’ decision-making process. Can J Aging. 2014;33(1):92–8. doi:10.1017/s0714980813000640.
- Lazarus JV, Wyka K, White TM, Picchio CA, Gostin LO, Larson HJ, Rabin K, Ratzan SC, Kamarulzaman A, El-Mohandes A. et al. A survey of COVID-19 vaccine acceptance across 23 countries in 2022. Nat Med. 2023;29(2):366–75. doi:10.1038/s41591-022-02185-4.
- Jones N. How COVID-19 is changing the cold and flu season. Nature. 2020;588(7838):388–90. doi:10.1038/d41586-020-03519-3.
- Mills MC, Rüttenauer T. The effect of mandatory COVID-19 certificates on vaccine uptake: synthetic-control modelling of six countries. Lancet Public Health. 2022;7(1):15–22. doi:10.1016/s2468-2667(21)00273-5.
- Moccia G, Carpinelli L, Savarese G, De Caro F. Vaccine hesitancy and the green digital pass: a study on adherence to the Italian COVID-19 vaccination campaign. Int J Environ Res And Public Health. 2022;19(5):2970. doi:10.3390/ijerph19052970.
- Bell ML, Kenward MG, Fairclough DL, Horton NJ. Differential dropout and bias in randomised controlled trials: when it matters and when it may not. BMJ (Clin Res Ed). 2013;346(1):e8668. doi:10.1136/bmj.e8668.
- Deml MJ, Githaiga JN. Determinants of COVID-19 vaccine hesitancy and uptake in sub-Saharan Africa: a scoping review. BMJ Open. 2022;12(11):e066615. doi:10.1136/bmjopen-2022-066615.