ABSTRACT
To optimize seasonal influenza control and prevention programs in regions with potentially complicated seasonal patterns. Descriptive epidemiology was used to analyze the etiology of influenza, and chi-square tests were used to compare the epidemic patterns among different influenza virus types and subtypes/lineages. From January 2010 to December 2019, a total of 63,626 ILI cases were reported in Chongqing and 14,136 (22.22%) were laboratory-confirmed influenza cases. The proportions of specimens positive for influenza A and influenza B were 13.32% (8,478/63,626) and 8.86% (5,639/63,626), respectively. The proportion of positive specimens for influenza A reached the highest in winter (23.33%), while the proportion of positive specimens for influenza B reached the highest in spring (11.88%). Children aged 5–14 years old had the highest proportion of positive specimens for influenza. The influenza virus types/subtypes positive was significantly different by seasons and age groups (P<.001), but not by gender (p = .436). The vaccine strains were matched to the circulating influenza virus strains in all other years except for 2018 (vaccine strain was B/Colorado/06/2017; circulating strain was B/Yamagata). The study showed significant variations in epidemic patterns, including seasonal epidemic period and age distributions, among different influenza types, subtypes/lineages in Chongqing. Influenza vaccines matched to the circulating influenza virus strain in nine of the ten years. To prevent and mitigate the influenza outbreaks in this area, high risk population, especially children aged 5–14 years, are encouraged to get vaccinated against influenza before the epidemic seasons.
Introduction
Influenza is an acute respiratory infectious disease caused by influenza virus. According to viral nuclear protein and matrix protein, it is divided into A, B, C and D, of which influenza A virus is the most common type.Citation1,Citation2 Each year, about 10% of adults and 20% of children worldwide are infected with influenza, resulting in an estimated one billion cases, 3–5 million hospitalizations, and 290,000–650,000 respiratory deaths globally.Citation3–5 Influenza causes an average of 88,000 additional respiratory deaths per year in China, with a vast area, complex climatic conditions, and a large population, yet the seasonality of influenza activity varies from region to region.Citation6 Previous studies have shown that the seasonality of influenza in subtropical zones is more variable.
Chongqing, located in southwest China, has a typical subtropical humid monsoon climate and is the largest municipality directly in China. According to 2023 statistics, the city’s population exceeds 32 million residents, with a per capita gross domestic product of 94,135 CNY.Citation7 Previous studies have shown that 13.3% (3,314 out of 24,868) of individuals tested positive for the influenza virus in sentinel hospitals in Chongqing, with influenza A being predominant.Citation8 Additionally, the all-cause mortality rate associated with influenza was 33.5 per 100 000 individuals.Citation5 Chongqing appears to have a more complex and irregular circulation pattern than other cities, and the disease burden is severe. However, studies comparing the epidemiology of influenza A and B infections are limited. This study aimed to compare the epidemic patterns of influenza A and B in Chongqing and to analyze the 2010–2019 epidemiological strains and vaccine matches to provide scientific evidence that is relevant to the control and prevention of influenza.
Materials and methods
Influenza surveillance
Influenza-like illness (ILI) and the proportion of specimens positive for influenza were obtained from sentinel hospitals in Chongqing, described in a previous study.Citation7 The ILI, defined as having a fever (≥38.0°C) and either cough or sore throat, was diagnosed by the outpatient and emergency departments.Citation8 In each sentinel hospital, an average of 20 respiratory specimens (throat swab, nasal swab, or nasopharyngeal swab) were collected from ILI cases per week. Samples are stored at 2°C to 8°C and sent to the territorial Center for Disease Control and Prevention (CDC) laboratory for reverse transcription-polymerase chain reaction (RT-PCR) to determine the types and subtypes/lineages of influenza virus according to the standard protocol. Meanwhile, participating physicians completed the sample information form and inputted the relevant patient data into the Chinese Influenza Surveillance Network.Citation9 The positive rate of influenza was defined as the percentage of respiratory specimens tested positive for influenza viruses. The annual positive rate of influenza is calculated as the rate of the number of influenza cases to the number of samples tested from 2010–2019. In this study, we analyzed influenza surveillance data including gender, age, date of onset and laboratory testing results from January 2010 to December 2019.
Statistical analysis
Descriptive epidemiology was used describe the frequency distribution of diseases across populations, time and regions. Histogram and line charts were used to show the time distribution of influenza cases. Chi-square tests were used to compare the differences in categorical variables. All analyses were conducted using R version 4.2.3 (R Foundation for Statistical Computing, Vienna, Austria). A two tailed p value < .05 was considered statistically significant.
Results
Overall characteristics of influenza cases
From 2010–2019, 63,626 ILI cases were recorded for specimen collection in sentinel hospitals. Among them 34,878 (54.82%, 34,878/63,626) were males and 28,748 (45.18%, 28,748/63,626) were females. A total of 14,136 ILI cases were diagnosed with laboratory-confirmed influenza. The proportion of specimens positive for influenza was 22.22% (14,136/63,626). Regarding seasonality of influenza positive rate, the highest influenza positive rate occurred in winter (December to February of the following year, 34.90%), followed by autumn (September to November, 20.92%) and spring (March to May, 18.11%). High variation was also observed in monthly positive rate, varying from zero to 62.38% (January 2019). The annual positive rate of influenza A was 13.32% (5.68%-23.82%). Stratifying by its subtypes, proportions of specimens positive for A/H1N1 and A/H3N2 were 5.73% and 7.60%, respectively. The annual positive rate of influenza B was 8.86% (2.35%-17.97%), with the proportions of specimens positive for B/Yamagata and B/Victoria at 2.04% and 4.98%, respectively. More details were provided in and .
Figure 1. Temporal trends of influenza virus activity by subtypes/lineages (a) Influenza virus; (b) Influenza A virus; (c) Influenza B virus.
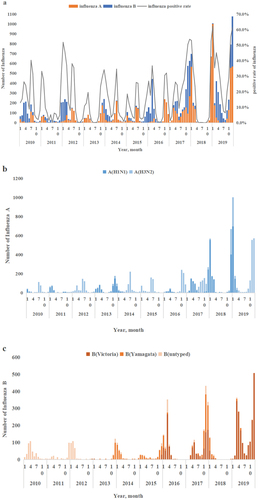
Table 1. Characteristics of influenza specimens in Chongqing, China, from 2010 to 2019.
Demographic characteristic differences among influenza virus types and subtypes/lineages
During the study period, the proportion of specimens positive for influenza varied across age groups (p < .001), with the highest among 5–14 years old (36.33%, 7,695/21,179), followed by 15–24 years old (24.41%, 1,317/5,396), 25–59 years old (19.20%, 1,957/10,194), ≥60 years old (15.12%, 438/2,896), and children 4 years and younger (11.39%, 2,729/23,961).
For influenza A virus subtypes, the proportions of specimens positive for A/H3N2 were much higher than those of A/H1N1 for most of the age groups except for the 25–59 years old group. For influenza B virus lineages, the proportions of specimens positive for B/Victoria were much higher than those of B/Yamagata for most of the age groups except for people aged ≥60 years. More details were provided in . Overall, significant differences are observed in the proportions of specimens positive for influenza virus subtypes/lineages among age groups but not between gender groups (p < .001).
Epidemic differences among influenza virus types and subtypes/lineages
Linear trend in positive influenza virus specimens infected across the years(p < .001). The highest influenza positive rate occurred in 2019 (41.85%), whereas the lowest rate occurred in 2011 (11.31%). A/H3N2, A/H1N1 and B/Victoria were predominant in 2012, 2018 and 2019. There was observed difference in the proportion of specimens positive for influenza by year. More details are provided in .
Regarding seasonal patterns, influenza A had a higher positive rate than influenza B in all seasons except spring. During the seasons of spring, summer, autumn, and winter, the influenza subtypes/lineages with the highest proportions of specimens positive were B/Victoria (8.02%, 1,360/16,967), A/H3N2 (9.52%, 1,328/13,950), A/H3N2 (11.31%, 1,669/14,995), and A/H1N1 (14.63%, 2,591/17,714), respectively. Difference was also observed in the proportion of specimens tested positive for influenza by year. More details are provided in and .
Matching of trivalent vaccine strains and circulating strains of influenza virus
During 2013–2019, the prevalent strains of influenza virus in Chongqing were matched with the trivalent influenza vaccine, except for 2018. The 2018 circulating strain was B/Yamagata whereas the vaccine strain was B/Colorado/06/2017. No data were obtained in the first three years, 2010–2012, because no influenza B specimen was typed ().
Table 2. Matching of trivalent vaccine strains and circulating strains of influenza B virus in China from 2010 to 2019.
Discussion
In this study, we compared the relative contribution and epidemic patterns of the different influenza virus types and subtypes/lineages for 10 years in Chongqing, China. The study highlights the complexity of influenza in this area.
The result showed the different proportions of specimens positive among different age groups (P<0.001). During the study period, children aged 5–14 years had the highest proportion of positive influenza specimens (36.33%) among all age groups, which was consistent with previous studies.Citation12–15 This phenomenon may stem from the majority of children aged 5–14 years being students who attend school in densely populated classrooms with limited ventilation, have poor hygiene and disease prevention awareness, and are more susceptible to influenza transmission due to their young age and weak immunity, leading to a high incidence of influenza. Therefore, influenza prevention and control measures should be prioritized at the levels of schools and childcare institutions, with a focus on strengthening health education and implementing effective protective measures including targeted influenza vaccination campaigns.Citation16–18
The level of influenza activity continued to increase during 2010–2019, which has been reflected throughout the country.Citation19–21 The surge in 2019 can be primarily attributed to the revision of the Guidelines for diagnosis and treatment of influenza, which incorporated the utilization of a rapid antigen test as a diagnostic criterion.Citation22
Our results showed that influenza A dominated over influenza B during the study period, consistent with the studies in other cities in China.Citation23–25 From 2010 to 2019, B/Victoria and B/Yamagata alternated in dominance, showing a Z-shaped pattern.Citation26 B/Victoria was more dominant than B/Yamagata in 2016, 2017, and 2019, which was consistent with previous studies on various regions across the country.Citation26–29 Our results showed that influenza epidemics in Chongqing tend to occur in spring and winter but influenza B viruses were primarily dominant in the spring season.Citation10,Citation12 During this period, the public should pay attention to non-pharmaceutical prevention measures, such as washing hands, wearing masks, opening windows for ventilation frequently.
To prevent vaccine strain and circulating strain mismatch, the World Health Organization (WHO) proposed that seasonal influenza vaccines should include two B lineage strains in 2012. Beginning from the 2013–2014 influenza season in the northern hemisphere, the recommendation for the quadrivalent vaccine was initiated.Citation30 In 2018, China approved the use of the quadrivalent vaccine. Our study found that the prevalent B-type influenza strain matched well with the B lineage included in the influenza vaccine in most years, except for 2018, consistent with earlier studies.Citation31–33 Although studies have shown that vaccination with a vaccine that does not match the prevalent strain of influenza B virus can still reduce the burden of influenza B disease to some extent, the effectiveness of the vaccine remains largely dependent on the degree of match between the two.Citation11, Citation34–36 Therefore, comprehensive and multi-level promotion of influenza vaccination in Chongqing is still necessary to enhance population protection.
The study has limitations that warrant discussion. This study was only limited to those with ILI in sentinel hospitals. Secondly, influenza B lineage identification, which differentiated B/Yamagata and B/Victoria, was not performed in some specimens during 2010–2012. In addition, the impact of influenza vaccination coverage, pandemic, environmental and climate factors on influenza epidemics was not included in this study.
Conclusion
In summary, the study showed significant variations in epidemic patterns, including seasonal epidemic period and age distributions, among different influenza types, subtypes/lineages in Chongqing. Influenza A dominated over influenza B in most years, but influenza B was more likely to be prevalent during the spring, with alternating spring epidemics of influenza B/Victoria and influenza B/Yamagata. Matched influenza strains and vaccine strains was observed from 2013 to 2019, except for the year 2018. It is urgent to promote region-specific influenza vaccination policies and other preventive measures targeting specific districts as well as high-risk groups (children aged 5–14 years) to address the complicated dynamics of influenza in this area.
Author contributions statements
XF, LQ, and JL contributed to the study concept and design; YX, JY, ZL, and SY contributed to data acquisition; XF, JL, XY and ZL contributed to data analysis; XF, JL, JY, SY and ZL contributed to the initial drafting of the manuscript, DT and LQ revised the manuscript. All authors contributed to the discussion, reviewed, and approved the final version of the manuscript.
Ethical approval
This study received appropriate approval from the ethics committee of the Chongqing Municipal Center for Disease Control and Prevention (Record number: 2021026).
Supplemental Material
Download MS Word (21.3 KB)Acknowledgments
The authors are grateful to Chongqing Science and Technology Bureau for the financial support.
This article has been preprinted [ID:https://doi.org/10.21203/rs.3.rs-3852144/v1]. However, the application has been withdrawn.
Supplementary Material
Supplemental data for this article can be accessed on the publisher’s website at https://doi.org/10.1080/21645515.2024.2363076
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data that support the findings of this study are available from the corresponding author, LQ, upon reasonable request.
Additional information
Funding
References
- Sarker A, Gu Z, Mao L, Ge Y, Hou D, Fang J, Wei Z, Wang Z. Influenza-existing drugs and treatment prospects. Eur J Med Chem. 2022 Mar 15;232:114189. doi:10.1016/j.ejmech.2022.114189.
- Rybakowski J. Infections and mental diseases: from tuberculosis to COVID-19. Psychiatr Pol. 2022 Oct 31;56(5):931–7. English, Polish. 10.12740/PP/152125.
- Iuliano AD, Roguski KM, Chang HH, Muscatello DJ, Palekar R, Tempia S, Cohen C, Gran JM, Schanzer D, Cowling BJ, et al. Global seasonal influenza-associated mortality collaborator network. Estimates of global seasonal influenza-associated respiratory mortality: a modelling study. Lancet. 2018 Mar 31;391(10127):1285–300. doi:10.1016/S0140-6736(17)33293-2.
- Paget J, Staadegaard L, Wang X, Li Y, van Pomeren T, van Summeren J, Dückers M, Chaves SS, Johnson EK, Mahé C, et al. Global and national influenza-associated hospitalisation rates: estimates for 40 countries and administrative regions. J Glob Health. 2023 Jan 27;13:04003. doi:10.7189/jogh.13.04003.
- Qi L, Li Q, Ding XB, Gao Y, Ling H, Liu T, Xiong Y, Su K, Tang WG, Feng LZ, et al. Mortality burden from seasonal influenza in Chongqing, China, 2012–2018. Hum Vaccin Immunother. 2020 Jul 2;16(7):1668–74. doi:10.1080/21645515.2019.1693721.
- Li L, Liu Y, Wu P, Peng Z, Wang X, Chen T, Wong JYT, Yang J, Bond HS, Wang L, et al. Influenza-associated excess respiratory mortality in China, 2010–15: a population-based study. Lancet Public Health. 2019 Sep;4(9):473–81. doi:10.1016/S2468-2667(19)30163-X.
- Chongqing Bureau of Statistics. Statistical bulletin on national economic and social development of Chongqing municipality. 2023. https://tjj.cq.gov.cn/zwgk_233/fdzdgknr/tjxx/sjzl_55471/tjgb_55472/202403/t20240326_13084652.html.
- Qi L, Xiong Y, Xiao B, Tang W, Ling H, Long J, Xiao D, Zhao H, Ye S, Chen S, et al. Epidemiological and virological characteristics of influenza in Chongqing, China, 2011–2015. PLOS ONE. 2016 Dec 9;11(12):e0167866. doi:10.1371/journal.pone.0167866.
- China National Influenza Center. National influenza surveillance technical guidelines. (2017 Edition)(EB/OL).(20170930).http://ivdc.chinacdc.cn/cnic/zyzx/jcfa/201709/t20170930_153976.htm.
- Zhu AQ, Li ZJ, Zhang HJ. Spatial timing of circulating seasonal influenza a and B viruses in China from 2014 to 2018. Sci Rep. 2023 May 2;13(1):7149. doi:10.1038/s41598-023-33726-7.
- Darvishian M, van den Heuvel ER, Bissielo A, Castilla J, Cohen C, Englund H, Gefenaite G, Huang W-T, la Bastide-van Gemert S, Martinez-Baz I, et al. Effectiveness of seasonal influenza vaccination in community-dwelling elderly people: an individual participant data meta-analysis of test-negative design case-control studies. Lancet Respir Med. 2017;5(3):200–11. doi:10.1016/S2213-2600(17)30043-7.
- Zhu A, Liu J, Ye C, Yu J, Peng Z, Feng L, Wang L, Qin Y, Zheng Y, Li Z. Characteristics of seasonal influenza virus activity in a subtropical City in China, 2013–2019. Vaccines. 2020 Mar 1;8(1):108. doi:10.3390/vaccines8010108.
- Sun W, Gao J, Ma Y, Li X, Gong R, Ma Y, Li T, Dong J. Epidemiological characteristics of influenza in Ningxia, 2009-2018. Chin J Dise Control. 2020;24(6):691–5+710. doi:10.16462/j.cnki.zhjbkz.2020.06.014.
- Jia G, Zhao Q, Liu K. Analysis of influenza surveillance results in Xuchang City from 2017-2019. Mod Dis Control Prev. 2020;31(7):561–3. doi:10.13515/j.cnki.hnjpm.1006-8414.2020.07.029.
- Liu W, He L, Ji J, Bai T, Ma Y, Wang L. Analysis of influenza surveillance results in Yan’an City, 2009-2020. J Yan’an Univ (Med Sci Ed). 2021;19(4):97–102. doi:10.19893/j.cnki.ydyxb.
- Benjamin-Chung J, Arnold BF, Kennedy CJ, Mishra K, Pokpongkiat N, Nguyen A, Jilek W, Holbrook K, Pan E, Kirley PD, et al. Evaluation of a city-wide school-located influenza vaccination program in Oakland, California, with respect to vaccination coverage, school absences, and laboratory-confirmed influenza: A matched cohort study. PLOS Med. 2020 Aug 18;17(8):e1003238. doi:10.1371/journal.pmed.1003238.
- Endo A, Uchida M, Hayashi N, Liu Y, Atkins KE, Kucharski AJ, Funk S. Within and between classroom transmission patterns of seasonal influenza among primary school students in Matsumoto city, Japan. Proc Natl Acad Sci USA. 2021 Nov 16;118(46):e2112605118. doi:10.1073/pnas.2112605118.
- Krishnan A, Dar L, Saha S, Narayan VV, Kumar R, Kumar R, Amarchand R, Dhakad S, Chokker R, Choudekar A, et al. Efficacy of live attenuated and inactivated influenza vaccines among children in rural India: A 2-year, randomized, triple-blind, placebo-controlled trial. PLOS Med. 2021 Apr 29;18(4):e1003609. doi:10.1371/journal.pmed.1003609.
- Song Q, Zhang L. Analysis of influenza sentinel surveillance results in Lanzhou from 2017 to 2021. Gansu Med J. 2022;41(9):825–8. doi:10.15975/j.cnki.gsyy.2022.09.023.
- Bi J, Zheng L. Analysis on joinpoint regression of influenza epidemic trends in Baoan district, Shenzhencity, Guangdong province from 2011 to 2021. Preventive Med Tribune. 2023;29(7):486–9. doi:10.16406/j.pmt.issn.1672-9153.2023.7.02.
- Lin Y, Liu H, Mao Z, Zhou Y, Wang Z, Dai M, Zhao D, Zhao Z. Analysis of epidemiological characteristics and etiological surveillance results of influenza in Kunming City From 2005 to 2021. J Preventive Med Inf. 2023;09(14):1–6. http://kns.cnki.net/kcms/detail/51.1276.R.20230809.1651.002.html.
- Wu H, Xue M, Wu C, Ding Z, Wang X, Fu T, Yang K, Lin J, Lu Q. Estimation of influenza incidence and analysis of epidemic characteristics from 2009 to 2022 in Zhejiang Province, China. Front Public Health. 2023 May 18;11:1154944. doi:10.3389/fpubh.2023.1154944.
- Zhang J, Wu A, Liu M, Chen Y, Liu J, Zhao Q. Epidemiological characteristics and trend analysis of influenza-like cases in Xuhui District of Shanghai from 2010 to 2019. Shanghai J Preventive Med. 2021;33(12):1136–40. doi:10.19428/j.cnki.sjpm.2021.20763.
- Ng H, Zhang T, Wang G, Kan S, Ma G, Li Z, Chen C, Wang D, Wong M, Wong C, et al. Epidemiological characteristics of influenza A and B in Macau, 2010–2018. Virol Sin. 2021 Oct;36(5):1144–53. doi:10.1007/s12250-021-00388-6.
- Chen C, Jiang D, Yan D, Pi L, Zhang X, Du Y, Liu X, Yang M, Zhou Y, Ding C, et al. The global region-specific epidemiologic characteristics of influenza: world health organization FluNet data from 1996 to 2021. Int J Infect Dis. 2023 Apr;129:118–24. doi:10.1016/j.ijid.2023.02.002.
- Ye C, Zhu W, Yu J, Li Z, Zhang Y, Wang Y, Gu H, Zou W, Hao L, Hu W. Understanding the complex seasonality of seasonal influenza a and B virus transmission: Evidence from six years of surveillance data in Shanghai, China. Int J Infect Dis. 2019 Apr;81:57–65. doi:10.1016/j.ijid.2019.01.027.
- WHO. Influenza Transmission Zones (EB/OL). (2018-9-14) (2019-3-20). https://www.who.int/influenza/surveillance_monitoring/updates/InfluenzaTransmissionZones20180914.pdf? ua=1.
- Gao H, Pu H, Yu J, Ling P, Duan Y, Zhang T. Epidemiological and etiological characteristics of influenza in Ganzi Tibetan regions of Sichuanfrom 2009 to 2019. Chin J Pathogenic Biol. 2023;18(8):934–8. doi:10.13350/j.cjpb.230812.
- Zhang Y, Wang X, Li Y, Ma J. Spatiotemporal analysis of influenza in China, 2005-2018. Sci Rep. 2019 Dec 23;9(1):19650. doi:10.1038/s41598-019-56104-8.
- Wang Q, Zhang M, Qin Y, Zheng J, Zhao H, Yang X, Li ZJ, Peng ZB, Feng LZ. Analysis on seasonality, age distribution of influenza B cases and matching degree of influenza B vaccine in China, 2011-2019. Chin J Epidemiol. 2020;41(11):1813–17. doi:10.3760/cma.j.cn112338-20200318-00375.
- Garten R, Blanton L, Elal AIA, Alabi N, Barnes J, Biggerstaff M, Brammer L, Budd AP, Burns E, Cummings CN, et al. Update: influenza activity in the United States during the 2017–18 season and composition of the 2018–19 influenza vaccine. MMWR Morb Mortal Wkly Rep. 2018 June 8;67(22):634–42. doi:10.15585/mmwr.mm6722a4.
- Chaves SS, Naeger S, Lounaci K, Zuo Y, Loiacono MM, Pilard Q, Nealon J, Genin M, Mahe C. High-dose influenza vaccine is associated with reduced mortality among older adults with breakthrough influenza even when there is poor vaccine-strain match. Clin Infect Dis. 2023 Oct 5;77(7):1032–42. doi:10.1093/cid/ciad322.
- Xu X, Blanton L, Elal AIA, Alabi N, Barnes J, Biggerstaff M, Brammer L, Budd AP, Burns E, Cummings CN, et al. Update: influenza activity in the United States during the 2018–19 season and composition of the 2019–20 influenza vaccine. MMWR Morb Mortal Wkly Rep. 2019 June 21;68(24):544–51. doi:10.15585/mmwr.mm6824a3.
- Drori Y, Pando R, Sefty H, Rosenberg A, Mendelson E, Keinan-Boker L, Shohat T, Mandelboim M, Glatman-Freedman A. Influenza vaccine effectiveness against laboratory-confirmed influenza in a vaccine-mismatched influenza B-dominant season. Vaccine. 2020 Dec 14;38(52):8387–95. doi:10.1016/j.vaccine.2020.10.074.
- Skowronski DM, Chambers C, De Serres G, Sabaiduc S, Winter AL, Dickinson JA, Gubbay JB, Drews SJ, Fonseca K, Charest H, et al. Vaccine Effectiveness Against Lineage-matched and -mismatched Influenza B Viruses Across 8 Seasons in Canada, 2010–2011 to 2017–2018. Clin Infect Dis. 2019 May 2;68(10):1754–7. doi:10.1093/cid/ciy876.
- Sekiya T, Ohno M, Nomura N, Handabile C, Shingai M, Jackson DC, Brown LE, Kida H. Selecting and using the appropriate influenza vaccine for each individual. Viruses. 2021 May 24;13(6):971. doi:10.3390/v13060971.
