ABSTRACT
The pandemic dramatically accelerated research on vaccine attitudes and uptake, a field which mobilizes researchers from the social sciences and humanities as well as biomedical and public health disciplines. The field has the potential to contribute much more, but the growth in research and the deeper connections between disciplines brings challenges as well as opportunities. This perspective article assesses the recent development of the field, exploring progress whilst emphasizing that not enough attention has been paid to national and local contexts. This lack of contextual attention limits the progress of research and hinders our capacity to learn from the COVID-19 crisis. We suggest three concrete responses: building and recognizing new publishing formats for reporting and synthesizing studies at a country level; establishing country-level interdisciplinary networks to connect research and praxis; and strengthening international comparative survey work by enhancing the focus on local contextual factors.
Introduction
The emergence of SARS-COV 2 resulted in one of the most important public health crises in decades, which vaccination played a significant role in resolving. Vaccines were developed at an unprecedented pace; for the first time the mRNA technology was widely tested; new scientific councils and/or expertise procedures were created in many countries to advise governments in a fast-evolving situation; many governments set up new forms of vaccine roll-outs to address the scale of the challenge; and many countries experimented with new or rare forms of vaccine mandates such as green passports and health passes. Today, COVID-19 remains a threat even though national responses have largely returned to business-as-usual settings. However, the new normal is unlikely to be the same as the old. In addition to the transformations arising from the crisis years, mRNA technology and other innovations in vaccinology herald a new era of product innovation and transformations into curative/therapeutic vaccines. To maximize the potential of this new age of vaccination, scholars and policymakers will need time to draw lessons and reflect on trends set in motion during the pandemic.
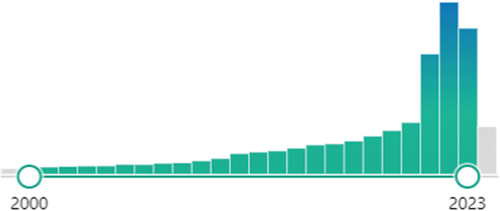
Research on vaccine attitudes and uptake is an important domain. The pandemic dramatically accelerated research in this already dynamic field (seeCitation1 and ), which mobilizes researchers from the social sciences and humanities as well as biomedical and public health disciplines. The importance of vaccination was widely recognized, including through unprecedented amounts of public research funding. The resultant proliferation of work enabled the testing of hypotheses formulated before the pandemic, the formulation of novel theories, the advancement of web-based methods to study vaccine hesitancy, and the dissemination of insights from often-overlooked countries, including from the Global South.
Figure 1. Evolution of the number of papers referenced in PubMed® on the topic of vaccine attitudes and uptake between 2000 and 2023 (max:4333 in 2022, min:82 in 2000).
This mobilization of the research community has already boosted not just scholarship on vaccine attitudes and uptake, but also connected fields such as inequality in health, misinformation, public attitudes to science, and trust in politicians and public institutions. We believe that the field has the potential to contribute much more, but the growth in research and the deeper connections between disciplines brings challenges as well as opportunities. Accordingly, this perspective article assesses the development of the field of social science of immunization during Covid-19, exploring progress whilst emphasizing a lack of attention paid to national and local contexts. This lack of contextual attention limits the progress of research in both the social sciences and humanities and in public health, and diminishes the capacity of researchers from both fields to nourish each other’s work. It also hinders our capacity to learn from the COVID-19 crisis. We suggest three concrete responses: building and recognizing new publishing formats for reporting and synthesizing studies at a country level; establishing country-level interdisciplinary networks to connect research and praxis; and strengthening international comparative survey work by enhancing the focus on local contextual factors.
Research on vaccine attitudes and uptake: between public health and the social sciences and humanities
Research on vaccine attitudes and uptake has a relatively long history. In his work on the history of vaccination in the USA during the 20th century, James Colgrove found opinion surveys conducted as far back as the 1930s, with a multiplication of such studies in the 1950sCitation2 (p133–135). This field of research subsequently expanded in phases, with some important contributions in the 1990s and further seminal work from the beginning of the 2000s following the Wakefield “controversy.” Such work drew attention to negative attitudes to vaccines and their potential public health consequences (see for instanceCitation3–10). The beginning of the 2010s saw a wider mobilization of international public health institutions on the issue, and the promotion of the vaccine hesitancy concept, which amplified dramatically during the COVID-19 epidemic.
Academic interest in vaccine attitudes and behaviors has therefore not only sprung organically from within the social science communities. It was fueled by renewed concern regarding infectious diseases in the public health community following epidemics, including the reemergence of measles in the global North and, of course, the spread of Covid-19. This real-world demand underscores the dynamic of the field’s interdisciplinarity. It attracts researchers from the various disciplines in the social sciences and humanities who are interested in advancing knowledge on individual and collective behavior. However, biomedical and public health researchers interested in improving health also contribute a significant amount of research. This peculiar form of interdisciplinarity is reflected in the concept of vaccine hesitancy, which has become the focus of the literature. The concept was popularized by a WHO SAGE Working Group formed after the H1N1 flu pandemic in a context where a growing number of countries were asking the WHO for guidance in the face of public questioning of a diverse range of vaccines. The working group, composed of an interdisciplinary panel of public health experts and social scientists, was mandated to define vaccine hesitancy and its determinants and to advise WHO on how to address it. While most previous public health research focused on enhancing access to vaccination services, the vaccine hesitancy concept brought significant attention to individual and group attitudes and behaviors. The WHO working group promoted a comprehensive framework of vaccine uptake to facilitate the design of interventions for improving vaccine coverage.
Vaccine hesitancy has had many definitions and faced criticisms from researchers in the social sciences and humanities. Critics have emphasized the concept’s theoretical ambiguities or confusions regarding, for instance, the distinctions between attitudes and behaviors, beliefs and decision-making processes, and proximal and distal factors (see for instanceCitation11,Citation12). Nevertheless, the concept has had some success in turning the public health world’s gaze away from the more radical forms of rejection to the more widespread, subtle, and qualified doubts as well as the complexity of vaccine decision-making processes. It has also helped to sensitize public health decision makers to the issue of trust in government, public institutions and the healthcare workforce, even if the tendency to attribute low uptake to individual factors rather than to social, cultural, historical or political factors has remained a major issue.Citation13 Even more importantly, the concept of vaccine hesitancy has helped to facilitate the circulation of ideas, stimulating debate between these different research communities interested in vaccination attitudes and uptake.
Vaccination has also attracted a diversity of research specialties.Citation12,Citation14 Many researchers have come to vaccine attitudes and behaviors as part of projects where vaccination was only one theme among many, while others are firmly wedded to the field. This diversity constitutes a great strength and underscores the future potential of the field. It helps vaccination social science to benefit from advances in broader domains of social and human sciences and vice versa. It has also helped to disseminate social science and humanities insights directly to public health experts and decision makers.
During COVID-19, research on vaccine attitudes and behaviours largely delivered on its promises
The field of research on vaccine attitudes and behaviors was delivering on its promises in the years before the pandemic, but this has accelerated since 2020. We saw an explosion of the volume of papers, especially questionnaire-based studies.
Before the pandemic, research focused on common trends and factors that bear upon vaccination across the world. That research sought to identify locations where hesitancy was most prevalent, and to understand the social profile of the hesitant. Scholars identified attributes associated with hesitancy in many countries e.g. being a woman, being poor, having suffered discrimination, distrust of public health authorities, and use of social media.Citation15,Citation16 The pandemic facilitated surveys testing the robustness of these findings in countries from Afghanistan to Zimbabwe (see for instanceCitation17–20), including important comparative studies conducted in many countries simultaneously.Citation21,Citation22 Many papers on vaccination published in disciplinary and interdisciplinary journals in the social science and humanities stimulated contemporary debates in these fields and vice versa, including on the circulation of disinformation and the expression of vaccine attitudes on social mediaCitation23–26, public attitudes to science,Citation27,Citation28 politicization of healthCitation29–33, and policyCitation34–36. Many public health and biomedical journals also opened their pages to articles on social and human aspects of vaccination. We also saw social scientists feature more prominently in the commentary and perspective sections of leading medical journals, presenting their insights regarding public health decision making.
Nevertheless, one important obstacle remains to the literature realizing its full potential: attention to national or even more local contexts.
Give us context!
While vaccine science is international, vaccination is implemented very differently at national and even sub-national levels. Schedules and technologies vary, as do social and cultural norms regarding health and prevention. There are also variations in the actors involved in campaigns, questions of cost, timing of vaccine availability, whether there are access barriers and for whom, whether vaccines are mandatory and how, etc. These elements bear heavily on whether vaccines become controversial, expressing wider social tensions. For instance, vaccine critical movements have been grounded in mistreatment of ethnic minorities and the poor,Citation37,Citation38 the marginalization of women’s voicesCitation39,Citation40 and public exasperation at scandals underlining the limits of modern States’ capacity to guarantee the safety of commercial goods.Citation15,Citation41 Vaccine controversies vary greatly between countries,Citation42 but also over time, as policies and society evolve. For instance, vaccine-related controversies emerged very late in France, which has since become very vaccine hesitant.Citation42,Citation43 By contrast, Great Britain was at the center of the autism scare at the turn of the 2000s, but is now amongst the least hesitant countries.Citation42,Citation44 Studies of contents posted online and on social media in particular have shown tremendous variations from one country to another.Citation45–47 Intentions to vaccinate against COVID-19 also evolved dramatically in most countries, with enormous variations within and between countries (see for instanceCitation21,Citation22,Citation33,Citation48,Citation49). During Covid-19, countries (or even sub-national regions) experienced different waves and disease prevalence. Often, differences resulted from non-pharmacological interventions (e.g. lockdowns and border closures), which then affected attitudes toward governments and vaccination programs. Every country also had preexisting experiences and policy settings informing public sentiment. Consequently, countries varied greatly in terms of how contentious the COVID-19 vaccine campaign became.
Understanding vaccine attitudes and behaviors therefore requires articulating structural and contextual factors. How universal mechanisms unfold (or don’t) in specific events and places depends upon local cultural, social, political, and policy contexts. However, context plays a marginal role in most publications, especially in public health and biomedical journals. For instance, most publications during COVID-19 present the results of a questionnaire survey carried out in one country or another, but barely mention contextual elements such as previous vaccine controversies, health scandals, relations with public authorities, or issues relating to differential access to health in local populations (equity gaps for vulnerable groups). We find ourselves in the paradoxical situation where international journals published the first papers presenting data from many countries – including many from the global south – with few of these papers helping us better understand the situation in these countries!
Another issue is that most data and scholarship emanate from high income countries, the USA in particular. This is particularly true of the literature on social media content.Citation50 Two further examples are the idea that populist parties are causing vaccine hesitancy through their public stances on vaccines, and the notion that public distrust in scientists has deepened in the past decades. Both are true for the USA, where analysis of this trend has positively influenced international scholarship, including by drawing attention to politicization, which was understudied before Covid-19. But generalizing these findings beyond the American borders requires more caution than we see in many published papers. For instance, a recent structural decline of trust in science is not that common and does not apply to some of the most vaccine hesitant countries, such as France.Citation51,Citation52 Regarding the impact of party representatives, politics seems to play a much more important role in people’s lives in the USACitation30,Citation53 compared to elsewhere; in many European countries, disengagement and disenchantment with politics are pervasive.Citation29,Citation32 Recent work conducted in Europe and even in the USA suggests that partisan identities are less important to vaccination than often stated, especially compared to trust in public authorities, disengagement with politics, and rejection of politicians altogether.Citation29,Citation32,Citation54–57
How might we explain these failings to include context and to recognize and account for global diversity and complexity? One answer may lie in the publication formats and norms of many medical and interdisciplinary journals. These include stringent word limits and a tendency to apply epidemiological or medical modes of reasoning to social issues. But this also stems from a general tendency to focus on universal cognitive explanations of vaccine hesitancy. This is seen, in particular, in the representation of socio-demographic and socio-cultural properties as uniform variables acting independently of each other and largely independent of the contexts in which people live. Scholars may play a role in this dynamic, over-generalizing the applicability of local findings as they pitch to journals with global readerships and pursue citations and impact. Yet social scientists have written extensively about the limitations of individualized approaches to behavioral issues and data.Citation4,Citation58–61
The over-emphasis on de-contextualized individuals is particularly concerning given that recent developments in research on vaccine attitudes and behaviors – including seminal work in psychology – place contextual variations at the center, something possible even when drawing on survey methodology. For example, the study of political identities has interrogated the link between structural variables (income, level of education, confidence in the health authorities) and changes in the public stances taken by party representatives.Citation31,Citation54,Citation55,Citation62,Citation63 Other work looks at national differences in perceptions of vaccination as a norm, and how this affects one’s propensity to think of vaccine hesitancy as a transgression or deviance.Citation27 Finally, many pandemic studies uncovered changes in the profile of hesitant people, or differences in profiles between countries, showing that the same factors can play out differently depending on geographical and temporal contexts.Citation29,Citation48,Citation64–66 These works greatly advanced thinking within the field on the interplay of emerging controversies, online mobilizations, individual trajectories, and structural factors such as growing distrust in institutions. Qualitative work has also underlined national and local variations in a number of dimensions that are likely to bear heavily on this interplay, such as media coverage,Citation67–69 strategies deployed by vaccine critics,Citation3,Citation40,Citation70,Citation71 the evolution of how vaccines and policies are produced and publicly debated,Citation2,Citation4,Citation41,Citation72–74 how mandates are decided upon and implemented,Citation75 or the experience of healthcare by underprivileged and marginalized groups.Citation76,Citation77
Three propositions
Covid-19 underlined the importance of national and local contexts, constituting an opportunity to advance research further by putting context at the center of our understanding of vaccine attitudes and behaviors. Indeed, dramatic variations across time and space make it easier for analysts to see the effect of contextual variations. In addition, the explosion of research has produced studies covering multiple aspects of vaccine attitudes and behaviors at different points in time and place, as well as studies documenting the evolution of public debates and online social movement mobilizations. But perhaps even more importantly, the pandemic has reinforced the connection between social science and humanities communities and the biomedical and public health communities. The latter can bring further understanding of the local specificities of vaccination campaigns, of the place of vaccination within national public health, and of the complexities of scientific discourses and controversies surrounding vaccines. All are crucial dimensions influencing both collective and individual engagement with vaccines. To improve the integration of national and local contexts in the analysis of the COVID-19 experience and future vaccination campaigns, we suggest three concrete pathways ().
Table 1. Three propositions to better integrate national and local contexts in the analysis of vaccination campaigns.
Proposition 1: create user-friendly repositories of vaccination social science and debates over vaccination at country level
Under this model, researchers would describe the issues facing vaccination locally, taking stock of available information and blind spots. This approach differs from systematic reviews, which focus on a very limited set of research questions and methodologies. Narrative reviews can work, provided they search beyond English-speaking journals where relevant. But facing short article formats, journal “vaccine saturation,” fast-evolving knowledge, and the considerable volume of available data and publications in some countries, new formats are needed. We propose reports centering on the state of research and knowledge produced on social aspects of vaccination at the national or sub-national level. Reports have become an important format in the vaccination community, widely used to disseminate information to the academic community, public institutions, decision-makers, and journalists. For instance, reports from the Vaccine Confidence Project have been landmarks in raising awareness of vaccine hesitancy across the world, as well as signaling new data in many countries.Citation78 Here, we propose a report format that is focused more on compiling all the data available, as well as offering expansive description of local vaccination contexts which are usually not presented in articles but are necessary for interpretation. In this spirit, some authors of this commentary compiled a French pandemic report drawing from peer-reviewed papers, reports, notes, book chapters, and books, enabling researchers to find pertinent information more easily. The resultant report summarizes the main findings on a wide-ranging list of topics, including the precise chronology of the evolution of attitudes to COVID-19 vaccination in France and comparisons with other countries.Citation49 Annual updates will reflect the dynamism of the French field. With a similar spirit, the ERC project Vax-Trust compiled and described in a series of reports the available data on the seven countries they studied to facilitate the understanding of the specific issues faced by each of them (https://cordis.europa.eu/project/id/965280/results). To allow such initiatives to flourish elsewhere, researchers, universities, and funders will need to find ways to resource the work and ensure the professional recognition of those who produce valuable impact outside the peer-review process.
Proposition 2: create national networks for interdisciplinary research
Better vaccination social science requires interdisciplinary debates and long-term collaborations that national networks can foster. Such networks can connect scholars who are focusing on individual behavior with those who are working on broader context (media, policymaking, mobilization, ethics), and likewise facilitate connections between those in the public health/biomedical disciplines and those in the social sciences and humanities. Such networks already exist in some countries. For example, Australia’s Collaboration on Social Science and Immunisation (COSSI) formed in 2016 to bring social science and public health researchers together with policy and program workers, facilitating collaborations and complementary projects and limiting duplication. COSSI authored several publications making best practice recommendations during the pandemic and won an Australian public health prize for their efforts.Citation79 Similarly, the Social Sciences and Humanities Network of the Canadian Immunization Research Network, launched in 2014, has conducted more than 27 research projects, creating momentum among humanities and social sciences scholars within and beyond that country. Long-term financial resources and institutional support might not be available everywhere, so less resource-intensive formats can be invented. In France, for instance, the new SHS-vaccination-France network consists of a simple website accompanied by a newsletter (https://shs-vaccination-france.com/en/). Its setup was included in a grant application, allowing researchers to access resources for its creation and maintenance. These are just three examples that can evolve and be improved upon; many other formats can be invented to suit each local research environment.
Proposition 3: strengthen investigation of local context in survey-based international comparisons
In the past decade, researchers have built, validated, and improved standardized questions to assess the prevalence of vaccine hesitancy globally (see for example.Citation12,Citation42,Citation80–82 These methodological tools have become crucial to monitor the evolution of attitudes among the public and healthcare workers. The WHO recently launched the Behavioural and Social Drivers of Immunisation (BeSD) tool suite, including qualitative questionnaires that can be modified for local usage.Citation82 However, existing instruments do not focus on public debate and discourse or consider how states create the conditions in which people do or do not vaccinate. For example, health system design and the state’s provision of other public services affect people’s attitudes toward vaccine programs.Citation83 One move forward would be to design and validate questions focusing on these aspects and integrate them into international questionnaires.
Conclusion
The boom in research on vaccine attitudes and behaviors during the COVID-19 pandemic provides an important opportunity to advance knowledge on vaccination social science and public health. With this momentum, it is crucial to capitalize on the lessons from the pandemic to better integrate social sciences and humanities expertise into public health and biomedical sciences. Research on the social aspects of vaccination should be informed by a larger reflection on equity in health, future health disaster preparedness, trust in science and information, adaptation to climate changes and many more of the current challenges the world is facing. Such research – done well and with close attention to the role of local and national contexts – can also contribute to resolving these challenges.
Acknowledgments
PPW, PV and JKW’s work is part of a project which has been labeled as a National Research Priority by the National Orientation Committee for Therapeutic Trials and other researches on COVID-19 (CAPNET project 0344). They would like to acknowledge ANRS | Emerging infectious diseases for their scientific support, the French Ministry of Health and Prevention and the French Ministry of Higher Education, Research and Innovation for their funding and support.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Acharya S, Aechtner T, Venaik S, Dhir S. Bibliometric analysis of vaccine hesitancy research from behavioural perspectives (2015–2022). J Risk Res. 2024;27(2):238–7. doi:10.1080/13669877.2024.2317318.
- Colgrove J. State of Immunity: the politics of vaccination in twentieth-century America. 1st ed. Berkeley: University of California Press; 2006.
- Hobson-West P. ‘Trusting blindly can be the biggest risk of all’: organised resistance to childhood vaccination in the UK. Sociol Health Illn. 2007;29(2):198–215. doi:10.1111/j.1467-9566.2007.00544.x.
- Leach M, Fairhead J. Vaccine anxieties: global science, child health and society. London: Earthscan; 2007.
- Brownlie J, Howson A. ‘Leaps of Faith’ and MMR: an empirical study of trust. Sociology. 2005;39(2):221–39. doi:10.1177/0038038505050536.
- Brewer NT, Chapman GB, Gibbons FX, Gerrard M, McCaul KD, Weinstein ND. Meta-analysis of the relationship between risk perception and health behavior: the example of vaccination. Health Psychol. 2007;26(2):136–45. doi:10.1037/0278-6133.26.2.136.
- Bedford H, Elliman D. Concerns about immunisation. BMJ. 2000;320(7229):240–3. doi:10.1136/bmj.320.7229.240.
- Streefland P, Chowdhury AMR, Ramos-Jimenez P. Patterns of vaccination acceptance. Soc Sci Med. 1999;49(12):1705–16. doi:10.1016/S0277-9536(99)00239-7.
- Leask JA, Chapman S. ‘An attempt to swindle nature’: press anti-immunisation reportage 1993-1997. Aust N Z J Public Health. 1998;22(1):17–26. doi:10.1111/j.1467-842X.1998.tb01140.x.
- Nichter M. Vaccinations in the third world: a consideration of community demand. Soc Sci Med. 1995;41(5):617–32. doi:10.1016/0277-9536(95)00034-5.
- Peretti-Watel P, Larson HJ, Ward JK, Schulz WS, Verger P. Vaccine hesitancy: clarifying a theoretical framework for an ambiguous notion. PLOS Curr. 2015; doi:10.1371/currents.outbreaks.6844c80ff9f5b273f34c91f71b7fc289.
- Bussink-Voorend D, Hautvast JLA, Vandeberg L, Visser O, Hulscher MEJL. A systematic literature review to clarify the concept of vaccine hesitancy. Nat Hum Behav. 2022;6(12):1634–48. doi:10.1038/s41562-022-01431-6.
- Attwell K, Hannah A, Leask J. COVID-19: talk of ‘vaccine hesitancy’ lets governments off the hook. Nature. 2022;602(7898):574–7. doi:10.1038/d41586-022-00495-8.
- Larson HJ. Defining and measuring vaccine hesitancy. Nat Hum Behav. 2022;6(12):1609–10. doi:10.1038/s41562-022-01484-7.
- Dubé È, Ward JK, Verger P, MacDonald NE. Vaccine hesitancy, acceptance, and anti-vaccination: trends and future prospects for public health. Annu Rev Public Health. 2021;42(1):175–91. doi:10.1146/annurev-publhealth-090419-102240.
- Yaqub O, Castle-Clarke S, Sevdalis N, Chataway J. Attitudes to vaccination: a critical review. Soc Sci Med. 2014;112:1–11. doi:10.1016/j.socscimed.2014.04.018.
- Ba MF, Faye A, Kane B, Diallo AI, Junot A, Gaye I, Bonnet E, Ridde V. Factors associated with COVID-19 vaccine hesitancy in Senegal: a mixed study. Human Vaccines & Immunotherapeutics. 2022;18(5):2060020. doi:10.1080/21645515.2022.2060020.
- Majid U, Ahmad M, Zain S, Akande A, Ikhlaq F. COVID-19 vaccine hesitancy and acceptance: a comprehensive scoping review of global literature. Health Promot Int. 2022;37(3):daac078. doi:10.1093/heapro/daac078.
- Mundagowa PT, Tozivepi SN, Chiyaka ET, Mukora-Mutseyekwa F, Makurumidze R, Sobh E. Assessment of COVID-19 vaccine hesitancy among Zimbabweans: a rapid national survey. PLOS One. 2022;17(4):e0266724. doi:10.1371/journal.pone.0266724.
- Nemat A, Bahez A, Salih M, Raufi N, Noor NAS, Essar MY, Ehsan E, Asady A. Public willingness and hesitancy to take the COVID-19 vaccine in Afghanistan. Am J Trop Med Hyg. 2021;105(3):713–7. doi:10.4269/ajtmh.21-0231.
- de Figueiredo A, Simas C, Karafillakis E, Paterson P, Larson HJ. Mapping global trends in vaccine confidence and investigating barriers to vaccine uptake: a large-scale retrospective temporal modelling study. Lancet. 2020;396(10255):898–908. doi:10.1016/S0140-6736(20)31558-0.
- Lazarus JV, Wyka K, White TM, Picchio CA, Gostin LO, Larson HJ, Rabin K, Ratzan SC, Kamarulzaman A, El-Mohandes A. et al. A survey of COVID-19 vaccine acceptance across 23 countries in 2022. Nat Med. 2023;29(2):366–75. doi:10.1038/s41591-022-02185-4.
- Petersen MB. Empowering audiences – against misinformation through ‘Prebunking’ – research-based insights on the problem of misinformation and steps towards its solution. Aarhuus: The future of Free speech project; 2023.
- Lincoln TM, Schlier B, Strakeljahn F, Gaudiano BA, So SH, Kingston J, Morris EMJ, Ellett L. Taking a machine learning approach to optimize prediction of vaccine hesitancy in high income countries. Sci Rep. 2022;12(1):2055. doi:10.1038/s41598-022-05915-3.
- Johnson NF, Velásquez N, Restrepo NJ, Leahy R, Gabriel N, El Oud S, Zheng M, Manrique P, Wuchty S, Lupu Y. et al. The online competition between pro- and anti-vaccination views. Nature. 2020;582(7811):230–3. doi:10.1038/s41586-020-2281-1.
- Illari L, Restrepo NJ, Johnson NF. Losing the battle over best-science guidance early in a crisis: COVID-19 and beyond. Sci Adv. 2022;8(39):eabo8017. doi:10.1126/sciadv.abo8017.
- Sturgis P, Brunton-Smith I, Jackson J. Trust in science, social consensus and vaccine confidence. Nat Hum Behav. 2021;5(11):1528–34. doi:10.1038/s41562-021-01115-7.
- Merkley E, Loewen PJ. Anti-intellectualism and the mass public’s response to the COVID-19 pandemic. Nat Hum Behav. 2021;5(6):706–15. doi:10.1038/s41562-021-01112-w.
- Stoeckel F, Carter C, Lyons BA, Reifler J. The politics of vaccine hesitancy in Europe. Eur J Public Health. 2022;32(4):636–42. doi:10.1093/eurpub/ckac041.
- Pink SL, Chu J, Druckman JN, Rand DG, Willer R. Elite party cues increase vaccination intentions among Republicans. Proc Natl Acad Sci. 2021;118:e2106559118.
- Motta MM. Republicans, not democrats, are more likely to endorse anti-vaccine misinformation. Am Polit Res. 2021;49(5):428–38. doi:10.1177/1532673X211022639.
- Ward JK, Cortaredona S, Touzet H, Gauna F, Peretti-Watel P. Explaining political differences in attitudes to vaccines in France: partisan cues, disenchantment with politics and political sophistication. J Health Polit Polic. 2024;11373758. doi:10.1215/03616878-11373758
- Jørgensen F, Bor A, Rasmussen MS, Lindholt MF, Petersen MB. Pandemic fatigue fueled political discontent during the COVID-19 pandemic. Proc Natl Acad Sci. 2022;119:e2201266119.
- Ruggeri K, Stock F, Haslam SA, Capraro V, Boggio P, Ellemers N, Cichocka A, Douglas KM, Rand DG, van der Linden S. et al. A synthesis of evidence for policy from behavioural science during COVID-19. Nature. 2024;625(7993):134–47. doi:10.1038/s41586-023-06840-9.
- Profeti S, Toth F. Climbing the ‘ladder of intrusiveness’: the Italian government’s strategy to push the Covid-19 vaccination coverage further. Policy Sci. 2023;56(4):709–31. doi:10.1007/s11077-023-09509-2.
- Sprengholz P, Felgendreff L, Böhm R, Betsch C. Vaccination policy reactance: predictors, consequences, and countermeasures. J Health Psychol. 2022;27(6):1394–407. doi:10.1177/13591053211044535.
- Frisco ML, Van Hook J, Thomas KJA. Racial/ethnic and nativity disparities in U.S. COVID-19 vaccination hesitancy during vaccine rollout and factors that explain them. Soc Sci Med. 2022;307:115183. doi:10.1016/j.socscimed.2022.115183.
- Kadambari S, Vanderslott S. Lessons about COVID-19 vaccine hesitancy among minority ethnic people in the UK. Lancet Infect Dis. 2021;21(9):1204. doi:10.1016/S1473-3099(21)00404-7.
- Durbach N. Bodily matters: the anti-vaccination movement in England, 1853–1907. Durham: Duke University Press Books; 2004.
- Reich JA. Calling the shots: why parents reject vaccines. 1st ed. NY: NYU Press; 2016.
- Conis E. Vaccine nation: America’s changing relationship with immunization. Chicago: University of Chicago Press; 2014.
- Larson HJ, de Figueiredo A, Xiahong Z, Schulz WS, Verger P, Johnston IG, Cook AR, Jones NS. The state of vaccine confidence 2016: global insights through a 67-country survey. EBioMedicine. 2016;12:295–301. doi:10.1016/j.ebiom.2016.08.042.
- Ward JK, Peretti-Watel P, Bocquier A, Seror V, Verger P. Vaccine hesitancy and coercion: all eyes on France. Nat Immunol. 2019;20(10):1257–9. doi:10.1038/s41590-019-0488-9.
- Anderberg D, Chevalier A, Wadsworth J. Anatomy of a health scare: education, income and the MMR controversy in the UK. J Health Econ. 2011;30(3):515–30. doi:10.1016/j.jhealeco.2011.01.009.
- Valdez D, Soto-Vásquez AD, Montenegro MS. Geospatial vaccine misinformation risk on social media: online insights from an English/Spanish natural language processing (NLP) analysis of vaccine-related tweets. Soc Sci Med. 2023;339:116365. doi:10.1016/j.socscimed.2023.116365.
- Zhou X, Song S, Zhang Y, Hou Z. Deep learning analysis of COVID-19 vaccine hesitancy and confidence expressed on twitter in 6 high-income countries: longitudinal observational study. J Med Internet Res. 2023;25:e49753. doi:10.2196/49753.
- Awijen H, Ben Zaied Y, Nguyen DK. Covid-19 vaccination, fear and anxiety: evidence from google search trends. Soc Sci Med. 2022;297:114820. doi:10.1016/j.socscimed.2022.114820.
- Serrano-Alarcón M, Wang Y, Kentikelenis A, Mckee M, Stuckler D. The far-right and anti-vaccine attitudes: lessons from Spain’s mass COVID-19 vaccine roll-out. Eur J Public Health. 2023;33(2):215–21. doi:10.1093/eurpub/ckac173.
- Ward JK, Privault S, Touzet H, Le Breton A, Verger P, Peretti-Watel P. Research on the human and social aspects of vaccination in France since Covid-19. 1st ed. Villejuif: CNRS-INSERM- ORS-PACA; 2024. https://shs-vaccination-france.com/en/research-on-the-human-and-social-aspects-of-vaccination-in-france-since-covid-19-1st-edition/.
- Badrinathan S, Chauchard S. Researching and countering misinformation in the global South. Curr Opin Psychol. 2024;55:101733. doi:10.1016/j.copsyc.2023.101733.
- Boy D. Attitudes toward Science in France: 1972–2005. In: Bauer M, Shukla R, Allum N. editors. The culture of science: how the public relates to science across the globe. NY: Routledge; 2012. p. 39–54.
- Bauer MW, Dubois M, Hervois P. Les français et la science 2021 - Représentations sociales de la science 1972-2020. Metz: Université de Lorraine; 2021.
- Iyengar S, Lelkes Y, Levendusky M, Malhotra N, Westwood SJ. The origins and consequences of affective polarization in the United States. Annu Rev Polit Sci (Palo Alto). 2019;22(1):129–46. doi:10.1146/annurev-polisci-051117-073034.
- Choi Y, Fox AM. Mistrust in public health institutions is a stronger predictor of vaccine hesitancy and uptake than Trust in Trump. Soc Sci Med. 2022;314:115440. doi:10.1016/j.socscimed.2022.115440.
- Enders AM, Uscinski JE. Are misinformation, antiscientific claims, and conspiracy theories for political extremists? Group Process Intergroup Relat. 2021;24(4):583–605. doi:10.1177/1368430220960805.
- Spälti AK, Lyons B, Stoeckel F, Stöckli S, Szewach P, Mérola V, Stednitz C, López González P, Reifler J. Partisanship and anti-elite worldviews as correlates of science and health beliefs in the multi-party system of Spain. Public Underst Sci. 2023;32(6):761–80. doi:10.1177/09636625231154131.
- Pennycook G, Bago B, McPhetres J. Science beliefs, political ideology, and cognitive sophistication. J Exp Psychol Gen. 2023;152(1):80–97. doi:10.1037/xge0001267.
- Diez Roux AV. Social epidemiology: past, present, and future. Annu Rev Public Health. 2022;43(1):79–98. doi:10.1146/annurev-publhealth-060220-042648.
- Emmons KM. Health behaviors in a social context. In: Berkman LF, Kawachi I, editors. Social epidemiology. Oxford: Oxford University Press; 2000. p. 242–66.
- Krieger N. Epidemiology and the web of causation: has anyone seen the spider? Soc Sci Med. 1994;39(7):887–903. doi:10.1016/0277-9536(94)90202-X.
- Singer M, Baer H. Critical medical anthropology. 2nd ed. (NY): Routledge; 1995.
- Hornsey MJ, Edwards M, Lobera J, Díaz-Catalán C, Barlow FK. Resolving the small-pockets problem helps clarify the role of education and political ideology in shaping vaccine scepticism. Br J Psychol. 2021;112(4):992–1011. doi:10.1111/bjop.12500.
- Ward JK, Alleaume C, Peretti-Watel P, Peretti-Watel P, Seror V, Cortaredona S, Launay O, Raude J, Verger P, Beck F. The French public’s attitudes to a future COVID-19 vaccine: the politicization of a public health issue. Soc Sci Med. 2020;265:113414. doi:10.1016/j.socscimed.2020.113414.
- Rughiniș C, Vulpe S-N, Flaherty MG, Vasile S. Shades of doubt: measuring and classifying vaccination confidence in Europe. Vaccine. 2022;40(46):6670–9. doi:10.1016/j.vaccine.2022.09.039.
- Vaux S, Gautier A, Nassany O, Bonmarin I. Vaccination acceptability in the French general population and related determinants, 2000–2021. Vaccine. 2023;41(42):6281–90. published online Sept 5. doi:10.1016/j.vaccine.2023.08.062.
- Liu R, Li GM. Hesitancy in the time of coronavirus: temporal, spatial, and sociodemographic variations in COVID-19 vaccine hesitancy. SSM Popul Health. 2021;15:100896. doi:10.1016/j.ssmph.2021.100896.
- Capurro G, Greenberg J, Dubé E, Driedger M. Measles, moral regulation and the social construction of risk: media narratives of “Anti-Vaxxers” and the 2015 Disneyland outbreak. Can J Soc. 2018;43(1):25–48. doi:10.29173/cjs29301.
- Court J, Carter SM, Attwell K, Leask J, Wiley K. Labels matter: use and non-use of ‘anti-vax’ framing in Australian media discourse 2008–2018. Soc Sci Med. 2021;291:114502. doi:10.1016/j.socscimed.2021.114502.
- Ward JK. Journalists and science: boundary-making in the media coverage of the 2009 pandemic flu vaccine’s safety in France. Sociologie. 2019;4:377–394.
- Cafiero F, Guille-Escuret P, Ward JK. “I’m not an antivaxxer, but … ”: spurious and authentic diversity among vaccine critical activists. Soc Networks. 2021;65:63–70. doi:10.1016/j.socnet.2020.11.004.
- Kirkland A. Vaccine court: the law and politics of injury. New York: NYU Press; 2016.
- Blume S. Immunization: how vaccines became controversial, 1er édition. London: Reaktion Books; 2017.
- Blume S. Immunization: how vaccines became controversial. Islington: Reaktion Books; 2017.
- Wailoo K, Livingston J, Epstein S, Aronowitz R. Three shots at prevention: the HPV vaccine and the politics of medicine’s simple solutions. New York: JHU Press; 2010.
- Attwell K, Navin MC, Lopalco PL, Jestin C, Reiter S, Omer SB. Recent vaccine mandates in the United States, Europe and Australia: a comparative study. Vaccine. 2018;36(48):7377–84. doi:10.1016/j.vaccine.2018.10.019.
- Dube E, Pistol A, Stanescu A, Butu C, Guirguis S, Motea O, Popescu AE, Voivozeanu A, Grbic M, Trottier M-È. et al. Vaccination barriers and drivers in Romania: a focused ethnographic study. Eur J Public Health. 2023;33(2):222–7. doi:10.1093/eurpub/ckac135.
- Jackson C, Dyson L, Bedford H, Cheater FM, Condon L, Crocker A, Emslie C, Ireland L, Kemsley P, Kerr S. et al. UNderstanding uptake of immunisations in travellIng and gypsy communities (UNITING): a qualitative interview study. Health Technol Assess. 2016;20(72):1–176. doi:10.3310/hta20720.
- Larson HJ, de Figueiredo A, Karafillakis E, Rawal M. State of vaccine confidence in the EU 2018. Bruxelles: European Commission; 2018.
- Attwell K, Wiley K, Leask J, Seale H, Carlson SJ, Cashman P, Karras J, Danchin M, Kaufman J. The collaboration on social science and immunisation (COSSI): global lessons from a successful Australian research and practice network. Vaccine. 2024;42(7):1420–3. published online Feb 9. doi:10.1016/j.vaccine.2024.01.107.
- Betsch C, Schmid P, Heinemeier D, Korn L, Holtmann C, Böhm R, Angelillo IF. Beyond confidence: development of a measure assessing the 5C psychological antecedents of vaccination. PLOS One. 2018;13(12):e0208601. doi:10.1371/journal.pone.0208601.
- Garrison A, Karlsson L, Fressard L, Fasce A, Rodrigues F, Schmid P, Taubert F, Holford D, Lewandowsky S, Nynäs P. et al. International adaptation and validation of the Pro-VC-Be: measuring the psychosocial determinants of vaccine confidence in healthcare professionals in European countries. Expert Rev Vaccines. 2023;22(1):726–37. doi:10.1080/14760584.2023.2242479.
- World Health Organization. Behavioural and social drivers of vaccination: tools and practical guidance for achieving high uptake. 2022: 98.
- Attwell K, Turvey J, Wood L. COVID-19 vaccination of at-risk and marginalised groups: recentering the state in vaccine uptake. Soc Sci Med. 2024;348:116812. doi:10.1016/j.socscimed.2024.116812.
