Abstract
Purpose: To evaluate the long-term effects from a 12-week balance-training programme on self-rated physical function and disability in healthy older adults with a tendency to fall and fear of falling.
Method: RCT, 59 participants, 67–93 years (42 women). The participants were randomised to an exercise group (n = 38) and a control group (n = 21). The intervention consisted of a specific and progressive balance-training programme three times/week for 12 weeks and was evaluated using the Late-Life Function and Disability Instrument (LLFDI) before training, directly after the training period and 6 and 12 months thereafter training. Data were analysed using a mixed model.
Results: Significant effects were found regarding physical function:
‘Functioning total’, ‘Basic lower extremity’ and ‘Advanced lower extremity’ in favour for the Exercises group. The exercise group improved significantly from baseline to directly after the training. At the 6 months follow-up, the effects had decreased to values similar to before the training, and remained unchanged until the 12 months follow-up. No significant effects regarding disability were found. The control group remained unchanged over time.
Conclusion: No long-term effects were found for physical function or disability assessed with the LLFDI after participation in a specific and progressive balance-training programme for healthy older adults.
Keywords:
Introduction
According to the International Classification of Functioning (ICF) [Citation1], functioning is an umbrella term for unproblematic or neutral aspects of health and health-related conditions. This includes body functions (physiological and psychological functions), body structures (anatomical parts of the body), activities (implementation of a document) and participation (involvement in a life situation). Disability is an umbrella term that can detect problems, that is, impairments, structural abnormalities, activity limitations and participation restrictions. A person’s functioning depends on the person’s health and how this interacts with environmental factors and personal factors, known as contextual factors. Environmental factors refers to the physical, social and attitudinal environment. These can either facilitate or inhibit the individual’s functioning.
It is well known that older people are strongly influenced by the physical design of the outdoor environment in their residential area. For example, inclined sidewalks and high curbs may create a major limitation for many elderly. Access to public transportation close to home and placed benches can however reduce the individual’s disability [Citation2].
The body changes with increased age, and these changes may lead to impairment in fitness, muscle strength and balance ability, which leads to decreased movement ability and a reduction of activity in daily living [Citation3].
Balance control is the foundation of our ability to move and function independently. Balance problems increase with age and increase the risk of loss of balance and falls. Balance control is based on a complex interaction among several systems and can be defined as a task-specific multi-joint skill that relies on the interaction of several physiological systems, including musculoskeletal, neuromuscular, visual, vestibular and sensory [Citation4].
Fear of falling is defined as a long-standing concern that a fall may lead to the person in question avoiding activities that he or she is still capable of performing [Citation5]. Female gender, old age, self-reported low or moderate health as well as a history of falls had a connection with fear of falling and activity avoidance [Citation6]. Several studies have shown that people with a high fear of falling have greater difficulties in performing activities of daily living and that they have a lower level of activities than those with a low fear of falling [Citation7]. This may lead to both a restriction in functioning and disability according to the ICF classification.
There is evidence to suggest that a combined exercise programme in a group reduces both the risk of falls and the number of falls in older populations [Citation8]. Therefore, a research group at Karolinska Institutet developed an individually adjusted and progressive balance group training programme for older people with fear of falling and tendency to fall. This programme has already been described and evaluated by Halvarsson et al. [Citation9]. They found that the programme was appreciated and feasible, reduced fear of falling, improved walking speed and reduced the time to take a rapid step forward with divided attention, a so-called dual task. The effects were maintained six months after the training period had stopped. The authors also found that the participants who completed the training immediately after this had improved in self-rated physical functioning, especially regarding lower extremities [Citation10]. However, the long-term effects of the balance-training programme on self-rated physical function and disability are still unclear.
The aim of this study was to evaluate the long-term effects of a 12-week an individually adjusted specific and progressive balance training programme on self-rated physical function and disability in healthy older adults with fear of falling and a tendency to fall and compare this to a control group.
Method
This is a randomised controlled study within a larger research studying the different effects of a balance-training programme directly after a balance training period and six and 12 months after the intervention. Sample size calculation was performed based on the primary outcome measure for the larger research project and sample size was set to 20 subjects/group [Citation9].
The participants were recruited by advertising in local newspapers, delivered free of charge to all households in selected districts of Stockholm, Sweden. The volunteers were contacted by phone by the researchers and interviewed to find out if they were eligible according to the following inclusion criteria: Age 65 years or older, community-dwelling, able to walk without walking devices indoors, at least one fall incident during the last six months and/or self-reported fear of falling. Fear of falling was assessed with a single-item question regarding fall-related fear [Citation11]. Exclusion criteria were the following: Reduced cognitive function according to the Mini Mental State Examination test [Citation12] (≥24 points were required for participation in the study), vertigo requiring medical care, neurological injury/illness, serious pain that might influence participating in the training programme or serious cancer, heart disease or lung disease.
Randomisation was performed by the participants themselves drawing an allocation slip from a sealed envelope with group allocation 2:1, that is, two to balance training and one to control group due to logistics reasons, after the baseline testing. The sealed envelope was prepared in advance by a research assistant that was not involved in the baseline testing.
The training group received progressive balance training for 12 weeks, 45 minutes three times a week, performed at the Physiotherapy Department at Karolinska University Hospital in Stockholm, Sweden. The balance training was supervised by two physiotherapists to ensure safety and individual adjustments for all participants. There were six or seven participants in each group. All sessions began with a warm-up and ended with stretching and breathing exercises. Participation in the study required at least 67% attendance at training sessions, that is, two out of three sessions/week to ensure that the possible positive effects could be derived from participation in the training [Citation13].
The balance programme consisted of exercises in sitting, standing and walking as well as reacting to loss of balance. It also included exercises with divided attention, so-called dual tasking and multitasking, in which advanced balance exercises were combined with cognitive and motor exercises, for example reading a newspaper, balancing a ball on a tray or reciting cities/flowers/animals. The exercises were adjusted individually by variations of speed or the support base, or by adding head movements or changing arm positions [Citation14].
The participants in the balance-training group did not receive any further instructions concerning training after the intervention period, than to resume previous physical activity level. Immediately after the randomisation, the control group was asked to maintain the same activity level as usual. Later, when all assessments were completed after the 12 months follow-up, the control group was offered the opportunity to participate in the same balance programme.
Data collection
Data were collected from year 2010 and 2013. Assessments were performed on four occasions: Before exercise (baseline), directly after the exercise programme (3 months) and six and 12 months after the end of the training period. The assessments were performed at the Department of Physiotherapy at Karolinska University Hospital in Stockholm, Sweden. Self-rated function and disability were assessed using the Late-Life Function and Disability Instrument (LLFDI) [Citation15].
The late-life function and disability instrument (LLFDI)
The Late-Life Function and Disability Instrument (LLFDI) is a self-assessment protocol with two components: function [Citation16] and disability [Citation16]. The function component contains 32 questions beginning with ‘How much difficulty do you have…’, for example ‘holding a full glass of water in one hand’ or ‘opening a heavy, outside door’. The answers are graded 1–5, ‘Cannot do, Quite a lot, Some, A little, None’.
Additionally, there is a part with eight questions for persons who use walking devices. This part was not used in the present study. The Function component can be summed up as ‘Overall Function’ or in the three subscales: ‘Upper extremity functioning domain’, ‘Basic lower extremity functioning domain’ and ‘Advanced lower extremity functioning domain’.
The disability component contains 16 items with two questions each: ‘How often do you…’ and ‘To what extent do you feel limited in…’, for example ‘Visiting friends and family in their homes’ or ‘Taking care of household business and finances’. The first question is graded 1–5 with the answers ‘Never, Almost never, Once in a while, Often, Very often’.
The second question is graded 1–5 with the answers ‘Completely, A lot, Somewhat, A little, Not at all’. The disability component can be summed up as ‘Total frequency dimension’ and ‘Total limitation dimension’. ‘Total frequency dimension’ can be split into the subscales ‘Social role domain’ and ‘Personal role domain’, while ‘Total limitation dimension’ can be split into the subscales ‘Instrumental role domain’ and ‘Management role domain’.
Summary scores were calculated by adding the item scores from each dimension and their subscales, and transformed to linearly scaled scores (0–100) based on a one-parameter Rasch model. High scores imply better function and less disability [Citation16,Citation17].
Psychometric proprieties of the Swedish version of LLFDI has been tested for older adults with self-reported fear of falling and balance deficits with very good test–retest reliability, that is, ICC2.1 values of 0.87–0.91 in the function component and 0.82–0.91 in the disability component. Measurement error on group level (SEM), that is, clinical relevant change on group level, was 2.9–5.1 (5–9%) for the function component and 2.6–4.1 (5–6%) for the disability component [Citation15].
The study was approved by the Local Ethics Committee in Stockholm, Sweden, Dnr.: 2006/151-31. All subjects signed an informed consent for participation in the study and they were informed that they could end their participation without declaring any reason for their decision.
Statistical analyses
The statistical analyses were performed using IBM SPSS Statistics, version 22 (SPSS Inc., Chicago, IL). Descriptive statistics were presented with number (n), percent (%), minimum–maximum (min–max), median, mean, and 95% confidence interval (95% CI). The demographic data were analysed with unpaired t-test for age, chi-square test for sex, living and diagnoses. The Mann–Whitney U-test was used for non-parametrical data such as body mass index, Mini Mental State Examination test and number of medications.
The LLFDI outcome was analysed parametrically using a mixed model with SIDAK’s post hoc test to study interactions on group and time according to intention-to-treat and per protocol, on both total scores and for all subscales. Significance level was set to p ≤ .05
Occasional missing values in the form were replaced with the mean of the remaining values in the same subscale. If half of the values were missing, that person’s subscale was excluded from the assessment (2 person’s at the assessment after the exercise programme (Function) and 1 at the assessment six months later (Disability)).
Results
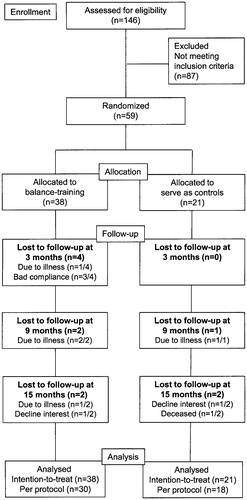
Out of 146 volunteers, 59 met the inclusion criteria and were randomised into the exercise group (n = 38) or the control group (n = 21). At the last follow-up, 12 months after the balance training programme, 48 persons remained in the study. See flow chart () for details of randomisation and follow-ups.
Figure 1. Flow chart, number of persons who reported an interest in the study, randomisation and number of participants with follow-up directly after the intervention and at six and 12 month after the intervention.
The balance training programme attendance was 87% (71–100%). No participant was injured during the training. In spite of many reminders, some participants were not able to keep group allocation a secret from the test leaders, and thus, the blinding to group allocation was not completely successful.
There were no significant differences in demographic variables () or LLFDI outcome between the exercise group and the control group at baseline. All participants were community dwelling and did not require any assisted living.
Table 1. Demographic data for the participants in the exercise group and the control group.
Function
The statistical analyses using a mixed model showed significant interactions on ‘Overall Function’, ‘Basic lower extremity functioning domain’ and ‘Advanced lower extremity functioning domain’ in favour for the exercise group, see and . The result analysed according to intention-to-treat () is equivalent to the result per protocol ().
Table 2. Intention-to-treat analysis including all randomised participants (n = 59) with a mixed model with SIDAK’s post hoc test.
Table 3. Per protocol analysis including the number of participants who full completed the whole study period and participated in all follow-ups (n = 48) with a mixed model with SIDAK’s post hoc test.
The post hoc tests showed that the exercise group improved significantly between the assessments before and after the balance training programme () in ‘Overall Function’ (p < .001, 5.7 points), ‘Basic lower extremity functioning domain’ (p < .001, 7.9 points) and ‘Advanced lower extremity functioning domain’ (p < .001, 7.8 points).
Figure 2. Mean and 95% confidence interval for Overall function, Basic lower extremity function and Advanced lower extremity function which showed significant interaction over time.
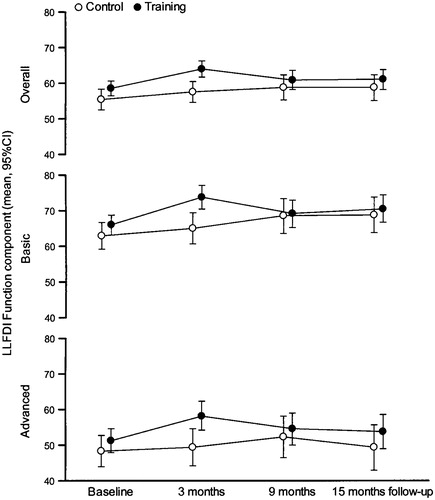
At follow-up six months after the balance-training programme, there was a significant decrease towards baseline in ‘Overall Function’ (p = .005, 3.1 points), ‘Basic lower extremity functioning domain’ (p = .031, 4.5 points) and ‘Advanced lower extremity functioning domain’ (p = .046, 4.1 points). At follow-up 12 months after the programme, there was no significant change compared to the follow-up at six months after the programme, .
The control group showed an improvement in ‘Basic lower extremity functioning domain’ from the assessment at baseline to the assessment after the balance-training programme (p = .564, 2.1 points) and the improvement continued until the assessment six months later (p = .93, 3.8 points). The result remained between the assessments at six and 12 months after the programme.
Comparisons between the groups showed that the exercise group performed significantly better than the control group at the follow-up immediately after the balance-training programme in terms of ‘Overall Function’ (p = .001, 64.1 (61.5–66.6) vs. 57.4 (54.6–60.3)), ‘Basic lower extremity functioning domain’ (p = .002, 73.8 (69.9–77.7) vs. 64.9 (61.4–68.3)) and ‘Advanced lower extremity functioning domain’ (p = .009, 58.9 (54.7–63.0) vs. 49.3 (43.9–54.6)). No differences were seen at the other follow-ups.
Disability
The statistical analyses using a mixed model showed no significant interactions on disability. The result analysed according to intention-to-treat is equivalent to the result per protocol.
Discussion
The aim of this study was to evaluate the long-term effect of a 12-week balance-training programme regarding self-reported physical function and disability using the Late Life Function and Disability Instrument (LLFDI). The analysis was performed using a mixed model according to intention-to-treat and per protocol approach.
Improvements were seen immediately after the training period on the three subscales related to the function of the lower extremities in the Function component, which agrees well with the earlier analysis of Roaldsen, Halvarsson, Sahlström and Ståhle [Citation10] performed per protocol. The changes can also be considered to be clinically significant since the values exceeded the measuring instrument method error, the standard error of measurement (SEM). However, no improvements remained in long-term follow-ups at six and 12 months after training. No effect/change was found regarding disability.
A previous study has shown that fear of falling and important balance parameters were improved by the intervention, and that the effect persisted six months after the training ended [Citation18]. It is unclear why the effect on physical function did not last as long. A possible reason could be that it is difficult to change habits and views on various activities even if the physical conditions have changed, for example, with improved balance.
Within the disability component, there were no changes between the groups. The reason for this may be that the issues raised in the instrument are not directly related to the balance ability. It may be unreasonable to expect improvements after balance training, for example in the activities ‘keep in touch with others by letter, phone or e-mail’, ‘take care of household finances’ and ‘go out with others in public places like a restaurant or the movies’. On the other hand, there are many issues where impaired balance and/or fear of falling could be a limiting factor, such as ‘take care of your home, household, laundry, cleaning and minor repairs’, ‘invite family and acquaintances to dinner’ and ‘participate in any regular physical activity’.
The participants were a group of relatively healthy older people with good cognitive skills who walked without aids and managed their everyday activities without help or other assistance from the community. Participants in both groups had only some or no functional limitations measured using the LLFDI before the balance training [Citation17], which means that the possibility for improvement was limited.
Both the training group and the control group remained at the same level of functioning and disability at the 12 month follow-up compared to baseline values.
The control group improved their ‘Basic functions of the lower extremities’ from baseline to follow-up directly after training and follow-up six months thereafter. Perhaps the control group experienced improvements because they were more physically active during the study period than before. Unfortunately, this is beyond our knowledge because no measurements of physical activity were included in the study. Another possible explanation could be that the participants in the control group became more aware of their situation since they took part in the study. The fact that both groups remained at the same level in terms of both function and disability at 15 months after entering in the study compared to baseline can possibly be explained by the fact that the participants were relatively healthy or due to changes in their physical activity levels.
The internal validity was limited since the test leaders were not blinded to the participants’ group allocation. Although the participants were instructed not to reveal their group allocation, the balance training participants were very enthusiastic and could not resist commenting on their experiences of the training and by that revealed group allocation for the test leaders.
One strength regarding the internal validity was that both the training programme and the test procedure were standardised and that attendance at the balance training was high (71–100%) [Citation19]. During the assessment, a test leader went through the questions in the LLFDI, which reduced the risk of misinterpretation and missing data.
The external validity is limited to all participants living in urban areas or in the suburbs. This is a limitation in that the degree of disability is influenced by how the physical environment is designed, for example, access to public transportation close to home or walkways that are easy to reach and use [Citation2], which may differ considerably between urban and rural areas. Another limitation is that a large group of elderly people were excluded from the study, such as those with cognitive disabilities and those who cannot walk without assistance. However, the studied group of older people with fear of falling and tendency to fall represents a large group of older people in society so the results are still generalisable to many individuals.
The results were analysed according to both intent-to-treat and per protocol with equivalent results. Intention-to-treat is recommended, in order not to overestimate the result of the study if a large proportion of participants dropped out from the study [Citation20]. This method also increases the generalisability because it gives a picture of what the overall outcome of the intervention will be. However, it may also be important to perform an analysis per protocol as additional information to find out how the intervention affected those who actually completed the study [Citation19].
Conclusions
A 12-week specific and progressive balance training programme for older people with tendency to fall and fear of falling gave no long-term effects related to self-reported physical function and disability assessed with the Late-Life Function and Disability Instrument. Improvements were seen immediately after the training period in the function component in the ‘Total’ function subscales and in ‘Basic functions of the lower extremities’ and ‘Advanced functions of the lower extremities’. No effect persisted at follow-up after six and 12 months. To improve and influence long-term effects, future research should aim to investigate if repeated training periods may influence the effects and when and how often exercise periods needs to be repeated.
Trial registration
The present study has not been registered since the first participant was enrolled in spring 2008 and at that time it wasn´t mandatory to register trials.
The authors have adhered to TIDieR intervention checklist and CONSORT checklist.
Acknowledgements
The authors would like to thank all the physiotherapists, test leaders, and participants in the study. A special thank you goes to Lisbet Broman at Karolinska Institutet for guidance and help with data collection.
Disclosure statement
The authors have no declaration of interest to report.
References
- World Health Organization. International classifications of functioning, disability and health. 2017. [Internet] Available from: http://www.who.int/classifications/icf/en2001.
- Keysor JJ, Jette AM, LaValley MP, the MOST group, et al. Community environmental factors are associated with disability in older adults with functional limitations: the MOST study. J Gerontol. 2010;65A:393–399.
- Spirduso WW, Francis KL, MacRae PG. Physical dimensions of aging. 2nd ed. Champaign (IL): Human Kinetics; 2005.
- Woollacott MH. Systems contributing to balance disorders in older adults. J Gerontol A Biol Sci Med Sci. 2000;55:M424–M428.
- Deshpande N, Metter EJ, Lauretani F, et al. Interpreting fear of falling in the elderly: what do we need to consider? J Geriatr Phys Ther. 2009;32:91–96.
- Zijlstra GA, van Haastregt JC, van Eijk JT, et al. Prevalence and correlates of fear of falling, and associated avoidance of activity in the general population of community-living older people. Age Ageing. 2007;36:304–309.
- Li F, Fisher KJ, Harmer P, et al. Fear of falling in elderly persons: association with falls, functional ability, and quality of life. J Gerontol B Psychol Sci Soc Sci. 2003;58:P283–P290.
- Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012;9:CD007146.
- Halvarsson A, Oddsson L, Olsson E, et al. Effects of new, individually adjusted, progressive balance group training for elderly people with fear of falling and tend to fall: a randomized controlled trial. Clin Rehabil. 2011;25:1021–1031.
- Roaldsen KS, Halvarsson A, Sahlstrom T, et al. Task-specific balance training improves self-assessed function in community-dwelling older adults with balance deficits and fear of falling: a randomized controlled trial. Clin Rehabil. 2014;28:1189–1197.
- Yardley L, Smith H. A prospective study of the relationship between feared consequences of falling and avoidance of activity in community-living older people. Gerontologist. 2002;42:17–23.
- Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician”. J Psychiatr Res. 1975;12:189–198.
- Howe TE, Rochester L, Neil F, et al. Exercise for improving balance in older people. Cochrane Database Syst Rev. 2011;11:CD004963.
- Halvarsson A, Dohrn IM, Stahle A. Taking balance training for older adults one step further: the rationale for and a description of a proven balance training programme. Clin Rehabil. 2015;29:417–425.
- Roaldsen KS, Halvarsson A, Sarlija B, et al. Self-reported function and disability in late life - cross-cultural adaptation and validation of the Swedish version of the late-life function and disability instrument. Disabil Rehabil. 2014;36:813–817.
- Haley SM, Jette AM, Coster WJ, et al. Late life function and disability instrument: II. Development and evaluation of the function component. J Gerontol A Biol Sci Med Sci. 2002;57:M217–M222.
- Jette AM, Haley SM, Coster WJ, et al. Late life function and disability instrument: I. Development and evaluation of the disability component. J Gerontol A Biol Sci Med Sci. 2002;57:M209–M216.
- Halvarsson A, Franzen E, Faren E, et al. Long-term effects of new progressive group balance training for elderly people with increased risk of falling – a randomized controlled trial. Clin Rehabil. 2013;27:450–458.
- Carter R, Lubinsky J, Domholdt E. Rehabilitation research: principles and applications. 4th ed. Philadelphia: Saunders; 2011.
- Moher D, Schulz KF, Altman DG. The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomized trials. JAMA. 2001;285:1987–1991.
