Abstract
Purpose: The purpose of this study was to examine the concurrent validity of a fixated hand-held dynamometer (HHD) in comparison to a load cell in measurement of maximal isometric knee extension force in adults with congenital heart disease (CHD) and healthy adults.
Methods: Fourteen adults with CHD and fourteen healthy adults were included. Each participant was tested three times with each method and the mean of the top two results for each participant and method was used in analysis.
Results: The agreement between the two methods was excellent in both groups (intraclass correlation coefficient [ICC], 95% confidence interval [CI]) 0.98 (0.92–1.00) in the CHD group and ICC 0.99 (0.96–1.00) in the healthy group). There was a small difference of 19.5 Newton or 4.8% (p<.05) between the two methods in the CHD group. No significant difference was seen between the two methods in the healthy group (p>.05).
Conclusions: The fixated HHD demonstrated excellent concurrent validity when compared to a load cell among adults with CHD as well as in healthy adults. Thus, in a healthy population the methods can be used interchangeably, however, a small difference between the methods is seen in the CHD group.
Introduction
Adults with congenital heart disease (CHD) are a growing and aging population [Citation1]. In addition to a reduced aerobic capacity [Citation2], adults with CHD also have impaired limb muscle function, i.e. reduced muscle endurance [Citation3–5] as well as reduced static (isometric) muscle strength [Citation5], even though the latter is not a universal finding [Citation4]. Nevertheless, this is of importance as there is evidence that low isometric limb muscle strength is associated with higher risk of all-cause mortality in both healthy populations [Citation6,Citation7] as well as in populations similar to adults with CHD [Citation8,Citation9].
There are numerous different techniques and devices for assessing isometric limb muscle strength. Some of the most common ones are isokinetic dynamometers, load cells or hand-held dynamometers (HHD) [Citation10,Citation11]. The isokinetic dynamometers and load cells have shown to provide valid and reliable measurements of isometric limb muscle strength in various populations, including healthy adults as well as people with respiratory disease [Citation10–14]. Advantages of the HHD includes that it is less expensive, more commonly available and feasible to use in clinical practice and that it does not require specific training to use [Citation15–19].
Isometric measurement of limb muscle strength with a HHD is commonly performed using one of two separate methods, the break method [Citation20] or the make method [Citation21]. The make method can be done either with manual resistance or with fixation of the HHD. Even though manual resistance is the most utilised way of using a HHD [Citation19,Citation22,Citation23], the reliability and validity of this technique compared to an isokinetic dynamometer or to a load cell vary markedly between studies [Citation12,Citation19,Citation24]. This could, at least partly, be explained by a lack of a standardised test procedure [Citation19] but it could also be a result of difficulties to manually resist the force produced by the tested limb. This is in particular often a limitation when testing lower limb muscle strength, e.g. isometric knee extension, as the tester often is incapable to manually resist the force produced by the quadriceps [Citation16,Citation19,Citation25]. A better approach is by fixating the HHD, which increases the possibility to measure higher peak forces [Citation25,Citation26] and increases the reliability and validity of measurements [Citation27]. Fixating the HHD against the leg of the bunk instead of against the leg of the person being examined has shown to improve comfort [Citation28]. There is need of an easy applied objective measurement of strength in clinical practice and to the best of the author’s knowledge, a HHD has not previously been validated in a population of adults with CHD. Thus, the aim of this study was to examine the concurrent validity of using a fixated HHD in comparison with a load cell to measure maximal isometric knee extension strength in adults with CHD and healthy adults. The hypothesis was that independent of group, there would be no difference between the fixated HHD and the load cell.
Method and materials
Study design and participants
This was a cross-sectional, comparative validity study, performed at Umeå University Hospital during September–November 2017. The study sample consisted of adults with CHD and healthy controls. The adults with CHD were consecutively recruited from the centre specialised in adult CHD at Umeå University Hospital during September–November 2017. We estimated that the sample size required to calculate the ICC with 5% precision and a power of 80% with an ICC > 0.80 and a confidence interval width of 0.4 would be 14 subjects per group [Citation29] based on a study on concurrent validity of a HHD to measure knee extension strength in healthy young adults [Citation17]. The recruitment was performed as a part of an on-going research project on body composition and muscle function in patients with complex CHD. Inclusion criteria were adult age (≥18 years of age), complex CHD [Citation30] and clinically stable condition. Exclusion criteria were cognitive impairment affecting independent decision capacity, comorbidity affecting participation, e.g. rheumatoid arthritis or other circumstances affecting study participation, e.g. pregnancy. In the larger project, an age and gender-matched peer was recruited for each patient. The controls were randomly recruited via the national population registry contacted by phone and asked for participation. Those tested during September–November 2017 were included in this study and thus not perfectly matched regarding age and gender with the patients included during the same period. All participants gave their written, informed consent and the study was approved by the Regional Ethical Review Board in Umeå, Sweden (Dnr-2016-299-32M, addition to 2016-18-31M).
Procedure
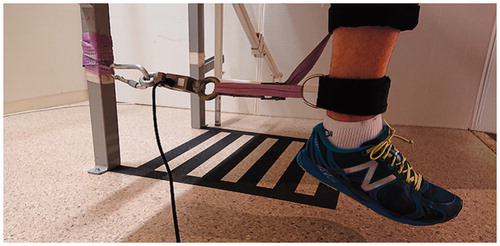
The tests were performed in a lab setting during one visit for each participant. The part of the study protocol concerning evaluation of concurrent validity took about 15 min. All tests were performed during daytime, pm. Testing of isometric knee extension strength was assessed using a fixated HHD, MicroFET2 (Hoggan Scientific LLC, Salt Lake City, UT) [Citation31] and a load cell (333 A 500 kg model, KTOYO Co., Ltd 289-7, Uijeongbusi, South Korea) [Citation32]. A load cell was used for comparison as it is one of the most commonly used devices for isometric measurements of knee extension strength [Citation11]. The load cell was considered as ‘gold standard’ in this study since measurements obtained with this device seems to be as reliable and reproducible as those obtained via computerised isokinetic dynamometry [Citation11Citation12]. The latter which often is considered the ‘gold standard’ for maximum voluntary contraction (MVC) measures [Citation10,Citation19]. The test sequence was randomly assigned by drawing a sealed envelope. Isometric knee extension strength measurements were performed on the dominant leg (decided by asking the participants which leg they would kick a ball with) and consisted of three maximal sustained (5 s) isometric contractions. Each participant was instructed and monitored by the same tester (not blinded to group allocation) and the participants performed the test in a sitting position (on a bunk) with 90° of flexion in hip and knee and their back against a backrest. After application of the test equipment and prior to initiation of the first test series the participants performed 2–3 submaximal muscle contractions in order to familiarise with the test procedure and the equipment, this was also considered to be the warm up. During the test series, the tester told the participant when to start pushing and when to stop, verbal encouragement was given by the tester (example ‘Push, push, push!’ and ‘Come on!’). Each contraction of 5 s was separated by a one-minute rest which has been shown to be enough for recovery in maximal strength assessments [Citation33,Citation34]. The rest between the two test modes, HHD and load cell, was 5 min. Fixation of the HHD () was done with a rigid belt right above the ankle at the anterior/distal part of the shin and the HHD fixated behind the bunk leg. This fixation was done in agreement with previous studies that have found the approach to be a comfortable and valid means of fixation [Citation27,Citation28]. Fixation of the load cell was done in a similar way, with a rigid strap right above the ankle at the anterior/distal part of the shin that was connected to the load cell which connected with a snaplink to another rigid belt fixated around the bunk leg (). Peak force in newton (N) was measured for each trial, for a total of three measures with each method and participant, in line with similar studies [Citation10,Citation15]. The mean of the two best measurements (i.e. the two highest results that did not differ more than 5% between each other) was used for statistical analysis. If all three measurements (contractions) differed more than 5% than the two values with the least difference was used to calculate a mean. The tests of isometric knee extension strength were as previously mentioned part of a larger study protocol, which included testing of isometric elbow flexion strength, grip strength, isometric knee extension strength, isotonic shoulder flexion and last isotonic heel-lift. All tests were performed on the participants dominant side in the order mentioned. The session of muscle tests was followed by assessment of body composition using dual energy X-ray absorptiometry, DXA (Lunar iDXA ME-200149, General Electric Healthcare, Madison, WI) and self-reported physical activity level using the International Physical Activity Questionnaire (IPAQ). The IPAQ comprises four generic items regarding time spent at different intensity levels of physical activity and a summary (vigorous, moderate, walking and total activity) in daily living during the past 7 d. This was summarised as a continuous score of metabolic equivalent of task (MET) minutes/week [Citation35]. Anthropometrical data, e.g. height and weight were collected during the same session as a part of the study protocol.
Sample size calculation and statistics
Statistical analysis was performed using the Statistical programme for the social sciences version 24 (SPSS, IBM corp., Armonk, NY). There was no missing data and all data were normally distributed, as confirmed with a Shapiro–Wilks test. Analysis of concurrent validity was conducted by comparing results from the HHD and the load cell using a two-way random, average measure interclass correlation (ICC 2.k) as well as using Pearson’s correlation (r). This approach was chosen in order to determine the association as well as the agreement between equipment’s and is in line with similar studies [Citation10,Citation17,Citation28]. Point estimates of r and ICC values were interpreted as <0.50, poor, 0.50–0.74, moderate, 0.75–0.89, high and ≥0.90 was considered excellent [Citation36]. Absolute agreement was calculated and represented with Bland–Altman plots and is presented with mean difference and lines of agreement. This was done as described by Bland and Altman [Citation37] with lines of agreement being calculated by mean difference ±1.96 * standard deviation, giving 95% limits of agreement. An analysis of variance (ANOVA) was used to decide if a fixed bias existed between methods (e.g. if one method consistently measured higher/lower values). A dependent t-test was also used to examine if the result with the HHD and the load cell differed within groups, while an independent sample t-test was used for a comparison of demographic data between the two groups as well as in a sub-analysis investigating the impact of age, gender, height, weight, BMI, level of physical activity (IPAQ) and lean mass of the tested leg on study results. The t-test analysis is presented with t-value (t) and degrees of freedom (df) as well as with 95% confidence interval (CI). Significance level was set at p<.05.
Results
A total of 28 participants were included (14 with CHD and 14 healthy controls). In the CHD group, 10 participants were men and 4 was women, in the healthy group there was 11 men and 3 women. Demographic data are presented in , and there were no differences between groups (). Most participants performed the test on their right leg, only two tested the left leg (one in each group).
Table 1. Demographics of study participants.
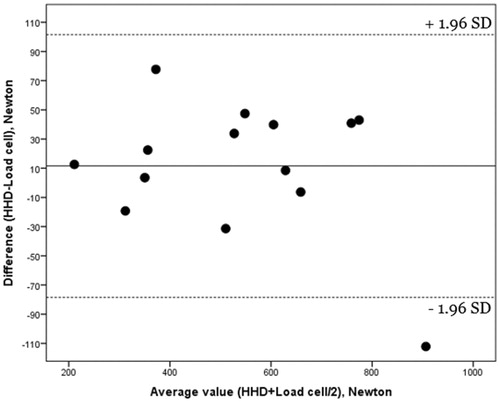
ICC in both groups was excellent (0.98 [0.92–1.00] in the CHD group and 0.99 [0.96–1.00] in the healthy group). The ANOVA analysis showed no proportional bias (i.e. there was not a trend to a fixed bias of higher or lower values) between measurement methods in either of the two groups ( and ). However, a small (4.8%), but significant, difference was seen between measurement methods in the CHD group, while no difference was observed between the HHD and the load cell among healthy adults (). A sub-analysis was performed in order to investigate possible explanatory factors for the observed difference in the CHD group. Neither age, height, weight, IPAQ nor lean mass of the tested leg had any impact on the results. However, when separating groups by gender this revealed that the observed difference in the CHD group between the two devices was seen among women (mean difference 38 N [95% CI 10–68], p=.024 [16%]), but not among (mean difference 12 N [95% CI −10–33], p=.245 [3%]). Compared to the male participants, women in the CHD group had a higher variability between contractions during the test with the load cell (mean difference 2.8% [95% CI 0.0–5.6%], p=.044).
Figure 3. Bland–Altmann plot of congenital heart disease group. Hand-held dynamometer vs. load cell.
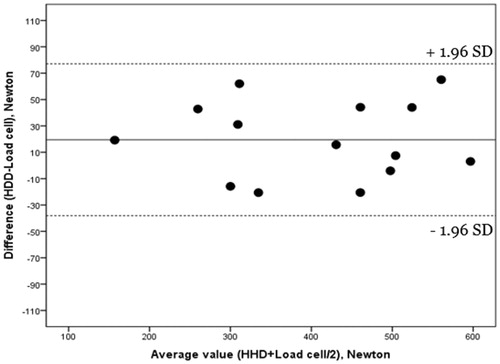
Table 2. Comparison of hand-held dynamometer and load cell.
Discussion
The aim of this study was to examine the concurrent validity of using a fixated HHD to measure isometric knee extension maximal strength in adults with CHD and healthy adults in comparison with a load cell. The hypothesis was that there would be no difference between the two measurement methods and that this would be true for both groups. This hypothesis was partially confirmed as evident by an excellent associations and agreement (r and ICC >0.90) [Citation34] between measurement methods in both groups. There was no statistical difference between the two methods in the healthy group. However, a small difference (4.8%) was observed between the two measurement methods in the CHD group.
To the best of our knowledge, this is the first study that has evaluated the concurrent validity of using a fixated HHD to measure isometric knee extension strength within a population with CHD. Furthermore, with regard to the setup of the measurements, this study is one of few studies that have utilised the strategy of fixating the HHD against the leg of the bunk () instead of against the subjects’ leg [Citation28]. With regard to the latter, Toonstra et al. [Citation12] found lower peak forces when using an HHD fixated against the subjects leg compared to a load cell in healthy adults. This is in contrast to our findings, demonstrating no difference between measurement methods among healthy controls and even higher values for the HHD among our sample of adults with CHD. The fixation of the HHD against the leg of the bunk instead of against the subjects leg could, at least partly, explain these differences as this setup has shown to be more comfortable than a fixation of the HHD against the subjects leg, possibly allowing the test subject to assert a higher peak force [Citation28]. The problem with the HHD measuring lower peak forces than other methods have also been shown in comparison with an isokinetic dynamometer [Citation38,Citation39], however, this is not a universal finding [Citation27,Citation40]. It could be that the difference between a HHD and an isokinetic dynamometer is affected by trunk stability, since when stabilising the trunk during a HHD measurement, the methods seem to measure the same [24]. Within the healthy population, similar to our findings, fixating the HHD against the bunk leg instead of the participant’s leg ensures that the results of the fixated HHD and an isokinetic dynamometer, or in our case a load cell, will not statistically differ. Thus, indicating that how the HHD is fixated is of importance for the validity of measurements, at least within the healthy population [Citation28].
As mentioned in the introduction some of the advantages of a HHD compared to an isokinetic dynamometer or load cell is that it is relatively cheap, more commonly available and it does not require specific training to use [Citation15–19]. Recently, even cheaper alternatives have been investigated with excellent reliability and validity, however, a big drawback with this new method is the limitation of maximum capacity to 50 kg [Citation41], which would not have been enough capacity in this study.
The observed difference between the two measurement methods in the group with CHD, which was not seen among healthy adults, was unexpected. This finding indicates that the two devices might not be used interchangeably and that if an HHD is used it might slightly overestimate (+4.8%) the MVC. This should not be neglected in the clinical setting. Of importance for clinicians, this observed difference between devices was only seen among women. Compared to the male participants, women in the CHD group had a higher variability between contractions during the test with the load cell which, at least partly, could contribute to this finding and suggest that more than three attempts might be necessary to achieve a valid isometric MVC among women. However, even though the sample size was sufficient for our primary analysis, these findings need to be confirmed in a larger trial with a sufficient sample size to allow for sub-group analysis. Furthermore, even though the difference was significant, it was small (<5%) and the clinical relevance of this difference needs to be further analysed.
The Bland–Altman analysis ( and ) shows visually narrower 95% limits of agreement in the CHD group than in the healthy group. One might expect that if the mean difference is smaller and non-significant in the healthy group the lines of agreement should also be narrower compared to the CHD group. The reason for this discrepancy is probably because of one of the included participants in the healthy group who stood out with a difference between the two methods almost twice the size of the largest difference in the CHD group (the second largest difference was also found in the healthy group, almost 10 N higher than the largest difference in the CHD group). These two individuals in the healthy group are probably the reason for the 95% limits of agreement being wider in the healthy group. The strengths of the study include the strictly standardised testing procedure as well as the time consumption, the whole testing procedure for one method takes about 5 min, the latter increasing the clinical applicability of utilising these measurement methods. In addition, the decision to allow no more than a 5% difference between the values that were used to calculate the mean from the isometric measurements was taken to ensure reproducibility of the efforts, which is common during isometric testing [Citation42,Citation43] even though the specific percentage used as the cut-off value could vary. This approach was selected in order to minimise the risk for potential outlier values affecting study results, which could lead to overestimations of isometric MVC values.
Limitations
Limitations of this study include, low female participation (n = 7) which makes it hard to draw conclusions regarding a female population. As previously mentioned, the subgroup analysis showed a higher variability between the contractions in females with CHD. However, the limited sample size prevents from making any clear statements about that and further studies are needed. Another limitation is the lack of standardised warm-up protocol. Although the participants did perform some submaximal contractions before their max test a more standardised way of warming up could have been preferable. The tester was not blinded to group allocation or, for obvious reasons, measuring method which could potentially have impacted the results.
Conclusion
For assessment of isometric knee extension strength, measurements using a fixated HHD demonstrate excellent concurrent validity among both adults with CHD and healthy adults. In healthy adults, the fixated HHD is, therefore, a viable option for measuring isometric knee extension strength in a clinical setting. If used in a population of adults with CHD one should take note of the small but significant difference that exists between methods and that they might therefore not be used interchangeably. The question remains if the small significant difference between the two methods in adults with CHD is clinically relevant. Before a fixated HHD could be recommended to be used in the clinical setting, the minimal detectable change, relative and absolute reliability as well as the responsiveness of the HHD needs to be established, preferably also including other muscle groups.
| Abbreviations | ||
| HHD | = | Hand-held dynamometer, CHD: Congenital heart disease, ICC: Intra class correlation, CI: Confidence interval, MVC: maximum voluntary contraction, N: newton, IPAQ: International Phyical Activity Questionnaire, MET: Metabolic equivalent of task, BMI: body mass index, ANOVA: Analysis of variance |
Disclosure statement
The authors have declared that no competing interests exist.
References
- Hoffman JI, Kaplan S. The incidence of congenital heart disease. J Am Coll Cardiol. 2002;39:1890–1900.
- Kempny A, Dimopoulos K, Uebing A, et al. Reference values for exercise limitations among adults with congenital heart disease. Relation to activities of daily life – single centre experience and review of published data. Eur Heart J. 2012;33:1386–1396.
- Sandberg C, Thilen U, Wadell K, et al. Adults with complex congenital heart disease have impaired skeletal muscle function and reduced confidence in performing exercise training. Eur J Prev Cardiol. 2015;22:1523–1530.
- Kroonström LA, Johansson L, Zetterström AK, et al. Muscle function in adults with congenital heart disease. Int J Cardiol. 2014;170:358–363.
- Greutmann M, Le TL, Tobler D, et al. Generalised muscle weakness in young adults with congenital heart disease. Heart. 2011;97:1164–1168.
- Ruiz JR, Sui X, Lobelo F, et al. Association between muscular strength and mortality in men: prospective cohort study. BMJ. 2008;337:a439.
- Ortega FB, Silventoinen K, Tynelius P, et al. Muscular strength in male adolescents and premature death: cohort study of one million participants. BMJ. 2012;345:e7279.
- Volaklis KA, Halle M, Meisinger C. Muscular strength as a strong predictor of mortality: a narrative review. Eur J Intern Med. 2015;26:303–310.
- Artero EG, Lee DC, Ruiz JR, et al. A prospective study of muscular strength and all-cause mortality in men with hypertension. J Am Coll Cardiol. 2011;57:1831–1837.
- Sinacore JA, Evans AM, Lynch BN, et al. Diagnostic accuracy of handheld dynamometry and 1-repetition-maximum tests for identifying meaningful quadriceps strength asymmetries. J Orthop Sports Phys Ther. 2017;47:97–107.
- Robles PG, Mathur S, Janaudis-Fereira T, et al. Measurement of peripheral muscle strength in individuals with chronic obstructive pulmonary disease: a systematic review. J Cardiopulm Rehabil Prev. 2011;31:11–24.
- Toonstra J, Mattacola CG. Test-retest reliability and validity of isometric knee-flexion and -extension measurement using 3 methods of assessing muscle strength. J Sport Rehabil. 2013;22:1–5.
- Kollock RO, Jr., Onate JA, Van Lunen B. The reliability of portable fixed dynamometry during hip and knee strength assessments. J Athl Train. 2010;45:349–356.
- Machado Rodrigues F, Demeyer H, Hornikx M, et al. Validity and reliability of strain gauge measurement of volitional quadriceps force in patients with COPD. Chron Respir Dis. 2017;14:289–297.
- Whiteley R, Jacobsen P, Prior S, et al. Correlation of isokinetic and novel hand-held dynamometry measures of knee flexion and extension strength testing. J Sci Med Sport. 2012;15:444–450.
- Deones VL, Wiley SC, Worrell T. Assessment of quadriceps muscle performance by a hand-held dynamometer and an isokinetic dynamometer. J Orthop Sports Phys Ther. 1994;20:296–301.
- Mentiplay BF, Perraton LG, Bower KJ, et al. Assessment of lower limb muscle strength and power using hand-held and fixed dynamometry: a reliability and validity study. PLoS One. 2015;10:1–18.
- Chamorro C, Armijo-Olivo S, De la Fuente C, et al. Absolute reliability and concurrent validity of hand held dynamometry and isokinetic dynamometry in the hip, knee and ankle joint: systematic review and meta-analysis. Open Med. 2017;12:359–375.
- Stark T, Walker B, Phillips JK, et al. Hand-held dynamometry correlation with the gold standard isokinetic dynamometry: a systematic review. PM R. 2011;3:472–479.
- Robertson JA, Kendall FP, McCreary EK. Muscles, testing and function (third edition). Br J Sports Med. 1984;18:25.
- Kim SG, Lim DH, Cho YH. Analysis of the reliability of the make test in young adults by using a hand-held dynamometer. J Phys Ther Sci. 2016;28:2238–2240.
- van der Heijden RA, Vollebregt T, Bierma-Zeinstra SM, et al. Strength and pain threshold handheld dynamometry test reliability in patellofemoral pain. Int J Sports Med. 2015;36:1201–1205.
- Muff G, Dufour S, Meyer A, et al. Comparative assessment of knee extensor and flexor muscle strength measured using a hand-held vs. isokinetic dynamometer. J Phys Ther Sci. 2016;28:2445–2451.
- Hirano M, Gomi M, Katoh M. Effects of trunk stability on isometric knee extension muscle strength measurement while sitting. J Phys Ther Sci. 2016;28:2474–2476.
- Wikholm JB, Bohannon RW. Hand-held dynamometer measurements: tester strength makes a difference. J Orthop Sports Phys Ther. 1991;13:191–198.
- Bohannon RW, Kindig J, Sabo G, et al. Isometric knee extension force measured using a handheld dynamometer with and without belt-stabilization. Physiother Theory Pract. 2012;28:562–568.
- Kim WK, Kim DK, Seo KM, et al. Reliability and validity of isometric knee extensor strength test with hand-held dynamometer depending on its fixation: a pilot study. Ann Rehabil Med. 2014;38:84–93.
- Hansen EM, McCartney CN, Sweeney RS, et al. Hand-held dynamometer positioning impacts discomfort during quadriceps strength testing: a validity and reliability study. Int J Sports Phys Ther. 2015;10:62–68.
- Wolak WE, Fairbairn DJ, Paulsen YR. Guidelines for estimating repeatability. Methods Ecol Evol. 2012;3:129–137.
- Erikssen G, Liestol K, Seem E, et al. Achievements in congenital heart defect surgery: a prospective, 40-year study of 7038 patients. Circulation. 2015;131:337–346.
- Hogganscientific.com [Internet]. Salt Lake City: Hoggan Scientific, LLC. [cited 2017 Nov 27]. Available from: http://hogganscientific.com/
- Ktoyo.com. [Internet]. Howondong, Uijeongbusi, Gyeonggido (South Korea): KTOYO co., Ltd; [cited 2017 Nov 27]. Available from: http://www.ktoyo.com/
- de Salles BF, Simao R, Miranda F, et al. Rest interval between sets in strength training. Sports Med. 2009;39:765–777.
- Parcell AC, Sawyer RD, Tricoli VA, et al. Minimum rest period for strength recovery during a common isokinetic testing protocol. Med Sci Sports Exerc. 2002;34:1018–1022.
- Craig CL, Marshall AL, Sjöström M, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–1395.
- Koo TK, Li MY. A Guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15:155–163.
- Bland JM, Altman DG. Measuring agreement in method comparison studies. Stat Methods Med Res. 1999;8:135–160.
- Bohannon RW, Bubela DJ, Wang YC, et al. Adequacy of belt-stabilized testing of knee extension strength. J Strength Cond Res. 2011;25:1963–1967.
- Katoh M, Hiiragi Y, Uchida M. Validity of isometric muscle strength measurements of the lower limbs using a handheld dynamometer and belt: a comparison with an isokinetic dynamometer. J Phys Ther Sci. 2011;23:553–557.
- Martins J, da Silva JR, da Silva MRB, et al. Reliability and validity of the belt-stabilized handheld dynamometer in hip- and knee-strength tests. J Athl Train. 2017;52:809–819.
- Romoero-Franco N, Jiménez-Reyes P, Montaño-Munuera JA. Validity and reliability of low-cost digital dynamometer for measuring isometric strength of lower limb. J Sports Sci. 2017;35:2179–2148.
- Seymour JM, Spruit MA, Hopkins NS, et al. The prevalence of quadriceps weakness in COPD and the relationship with disease severity. Eur Respir J. 2010;36:81–88.
- Nyberg A, Saey D, Martin M, et al. Test-re-test reliability of quadriceps muscle strength measures in people with more severe chronic obstructive pulmonary disease. J Rehabil Med. 2018;50:759–764.