Abstract
Aim
To investigate the beliefs of healthcare students about how harmful common daily activities are perceived to be for their lower back.
Method
A cross-sectional survey of Physiotherapy, Occupational Therapy and General Nursing pre-registration students in Ireland. Two hundred and forty two students completed the modified Photograph Series of Daily Activities survey to ascertain their low back pain beliefs. Beliefs were compared between those in different programmes using one-way ANCOVA (post hoc Bonferroni).
Results
Physiotherapy students (n = 115) had significantly more positive beliefs (lower scores) than Occupational Therapy (n = 48) and General Nursing (n = 79) students (p < .001). No significant difference was found between Occupational Therapy and General Nursing students (p = .054). Males had significantly more positive beliefs than females (p = .043), while there were no differences according to low back pain status (p = .383).
Conclusions
Physiotherapy students considered common daily activities less harmful for their lower back than Occupational Therapy and General Nursing students. Considering the relationship between low back pain beliefs and disability, negative beliefs among healthcare students need to be addressed. Healthcare students from different disciplines have different beliefs about the harmfulness of common daily activities for their own back. This has the potential to affect their practice and the outcomes of low back pain patients they encounter.
Introduction
Low back pain (LBP) is a disabling, prevalent and costly global health problem [Citation1–3]. Approximately 10–20% of patients who experience acute LBP will go on to develop persistent LBP [Citation4,Citation5]. In our opinion, there is a long-held belief that certain physical activities (e.g. lifting, bending, twisting) are harmful for the spine and cause LBP. However, while these activities can trigger acute LBP [Citation6], there is no clear evidence that these activities cause ongoing disabling LBP [Citation7–9]. Furthermore, we are of the opinion that many people with acute LBP cannot recall a physical trigger. The belief that physical activities are harmful for LBP contradicts clinical guidelines that encourage people with LBP to remain active, and return to all daily activities as soon as possible [Citation10–13].
Beliefs that certain activities should be avoided by people with LBP are common not only among the general public and patients but also among healthcare professionals (HCPs) [Citation14,Citation15]. Patients report that HCPs have the strongest influence on their attitudes and beliefs about LBP including their understanding of the source and meaning of their symptoms and their prognostic expectations [Citation16]. The beliefs HCPs hold about LBP influence their clinical practice [Citation15,Citation17]. For example, physiotherapists who score higher on biomedical orientation to LBP treatment are more likely to advise patients to delay returning to work and physical activity on the basis that these activities are a threat to the patient [Citation17].
The prevalence of erroneous and fearful beliefs about LBP among HCPs is concerning as fear of physical activities correlates with poor outcomes and persistent disability in people with LBP [Citation18]. Unfortunately, changing clinicians’ beliefs and behaviours has proven to be very difficult across clinical areas [Citation19]. Changing experienced clinician’s beliefs may be even more challenging, as experienced clinicians who have been predominantly utilising biomedical models to work with patients with LBP have been shown to be less adherent to current LBP guidelines [Citation20]. It has been proposed that fostering more positive beliefs regarding LBP during entry-level training could ensure future HCPs hold more evidence-based views [Citation21]. The recent Lancet series on LBP [Citation22] proposed healthcare training reform and changes in curricula to endow students with more positive LBP beliefs. The need for HCP educational reform on LBP is highlighted by data showing that LBP beliefs differ between HCPs [Citation23,Citation24] with wide variation in the time spent on pain education across the various HCP curricula [Citation25]. Previous research among healthcare students has shown considerable variation in their LBP beliefs, with these beliefs possibly varying according to their programme of study [Citation24,Citation26], year of study [Citation23,Citation27], sex [Citation24,Citation26] and previous experience of LBP [Citation23,Citation28]. Most of this research on the LBP beliefs of healthcare students has focussed on physical functioning [Citation26,Citation27,Citation29,Citation30], and the perceived inevitable consequences of LBP [Citation23,Citation24,Citation28]. However, we know of no existing study which has evaluated the beliefs of healthcare students regarding the perceived harmfulness of common daily activities.
Therefore, the primary aim of this study was to investigate the beliefs of students from different healthcare programmes about how harmful common daily activities are for their back. Secondary aims were to evaluate the role of other factors (e.g. sex, age, LBP status) on their beliefs.
Materials and methods
The manuscript has been written in line with the STROBE statement [Citation31].
Study design
A cross-sectional survey of Physiotherapy, Occupational Therapy and General Nursing pre-registration students in Ireland.
Setting
Classrooms within the University of Limerick, Ireland. Data collection occurred in 2016.
Participants
Any student aged >18 years currently enrolled in one of three entry-level healthcare degree programmes at the University of Limerick, Ireland: four-year undergraduate degrees in Physiotherapy (PT) and General Nursing (GN), and a two-year postgraduate Masters in Occupational Therapy (OT).
After contacting the directors of each programme, individual lecturers gave permission to enter classrooms seeking participation. Students were provided with information regarding the study prior to providing written informed consent. Students returned questionnaires (completed or blank) either immediately to the investigator or placed them in a box at the exit of the class.
Outcome measures
Modified photograph series of daily activities (mPHODA)
The mPHODA used in this study is a shortened version of the original PHODA [Citation32]. The original PHODA consists of 100 photographs of people performing common daily activities such as gardening or cleaning [Citation33]. Participants look at each photograph and mark on a 0–100 Likert scale how harmful they believe each activity is for their back (0 = not harmful at all, 100 = extremely harmful). This establishes a visual fear hierarchy of the activities indicating a person’s fear-avoidance beliefs, with lower scores indicating more positive beliefs [Citation32]. We chose to use the PHODA rather than other questionnaires asking about beliefs more generally, as there is emerging evidence that these different options measure different aspects of beliefs, with task-specific measures possibly being more useful [Citation34]. Due to our need to limit data collection within classes to less than 15 minutes, and wanting to pick those PHODA images which we felt based on clinical experience were likely to best reflect a breadth of spinal postures and loads, we selected a sub-sample of 12 images depicting specific lifting, carrying and bending activities of the back for our mPHODA. These tasks were chosen after discussion amongst two authors due to these activities commonly being linked to LBP, and a desire to reduce the burden on participants.
Participant characteristics
Participants were required to provide details on their programme of study, year of study, age, sex and their LBP status. To determine the significance of any reported LBP, participants were asked if back pain caused them to (a) reduce activity levels? (b) receive treatment? or (c) take medication? LBP was defined as significant if at least two of these three questions were affirmative, whereas LBP was considered mild if only one question was affirmative [Citation28].
Data analysis
SPSSv21 was used to analyse data. The internal consistency of the mPHODA was evaluated using Cronbach’s alpha. mPHODA data were normally distributed, based on visual inspection of the data, and Kolmogorov-Smirnov testing. mPHODA scores were compared in different programmes of study using a one-way ANCOVA, after controlling for confounders including age, sex, year of study and LBP status. Post hoc Bonferroni were applied between programmes of study. One-way ANOVA was used to compare students according to LBP status (none, mild, significant).
An independent t-test was used to compare male and female mPHODA scores. Age was correlated with mPHODA using Spearman’s correlation, as age was not normally distributed. Correlations were rated as small (r = 0.10 to 0.29), medium (r = 0.30 to 0.49) or large (r = 0.50 to 1.0) [Citation32].
Results
Survey completion rates and characteristics
The total number of students across the three programmes was 386 (PT = 124, GN = 200, OT = 62). Due to logistical considerations (students from two GN classes (n = 100) being away on clinical placement), the maximum eligible sample at the time of testing was 286. Two hundred and forty two students completed the survey (response rate = 85.7%), as 41 students either were not present in class or did not complete the questionnaires. Finally, three responses were excluded as participants provided mPHODA scores for <5 activities, leaving a total valid sample of 242 students. The internal consistency of the mPHODA using Cronbach’s alpha was 0.92.
illustrates the characteristics of the total sample and of each programme. The majority of the sample were female (77.8%), PT students (47.5%) with no LBP (41.2%).
Table 1. Participant characteristics across each programme of study.
mPHODA scores across programmes
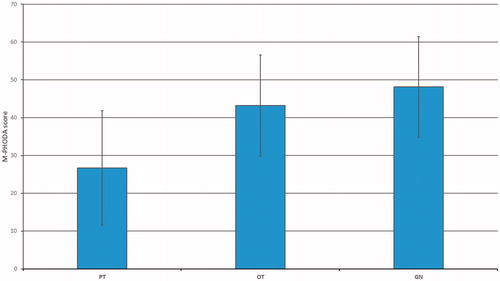
The mean(SD) mPHODA score across all students was 37.0(17.4). mPHODA scores differed significantly between programmes of study (F2, 2 4 0 = 57.93, p < .001). PT students had the lowest mPHODA scores (most positive beliefs), followed by OT students and finally, GN students (). Post hoc comparisons revealed significant difference in mPHODA scores between PT and OT students (mean difference = 13.91, p < .001) and between PT and GN students (mean difference = 20.68, p < .001) but not between OT and GN students (mean difference = 6.77, p = .054).
Figure 1. Mean ± SD mPHODA scores across each course of study. PT: physiotherapy; OT: occupational therapy; GN: general nursing.
Mean (SD) scores on the mPHODA were significantly lower (more positive beliefs) for males 32.8(17.4) than females 38.2(17.7) (mean difference = 5.41, t(241)=2.03, p = .043), but did not differ according to LBP status (F2,2 4 0 = 0.963, p = .383), while there was no significant correlation between age and mPHODA scores (r2 = 0.098, p = .128).
also presents the mean mPHODA score according to year of study in the different programmes. Differences in the number of years, and the availability of classes, between the three programmes prevented formal analysis of whether mPHODA scores evolved differently across the different programmes. However, it appeared that PT students in later years of the programme had lower (more positive) mPHODA scores than those students who had just commenced the programme. In contrast, students in the OT and GN programmes did not have lower (more positive) beliefs later in their programmes.
Discussion
In this study, PT students had significantly lower (more positive) beliefs about the harmfulness of common daily activities for an individual’s back than OT and GN students. No significant differences in beliefs were found between OT and GN students. Males had significantly more positive beliefs than females overall. Age and LBP status were not significantly related to mPHODA scores.
Differences between healthcare student groups
Our data are consistent with studies suggesting PT students hold more evidence-based beliefs about LBP than other healthcare students [Citation23,Citation24,Citation35]. For example, we have previously shown that PT students are less fear-avoidant about LBP than GN students [Citation35]. Several other studies comparing healthcare students have also demonstrated that the beliefs of PT students are less negative or fearful regarding physical functioning [Citation26,Citation29,Citation30,Citation35] and the perceived inevitable consequences of LBP [Citation23,Citation24,Citation28,Citation35].
While we are not aware of other studies which have examined the beliefs of healthcare students using the mPHODA specifically, our results are consistent with a large body of evidence suggesting that the beliefs of healthcare students are suboptimal in preparing them to address the needs of people with LBP and other painful conditions [Citation36]. A recent review of 20 studies that analysed student knowledge, skills, attitudes or beliefs regarding pain across medicine, GN, PT and OT curricula found that students lacked key knowledge and skills, and that many had negative attitudes and beliefs regarding pain [Citation37]. A lack of normative data on the PHODA, or the different versions of it, limit our ability to interpret precisely how poor the current student scores are. Trost et al. [Citation38] used a longer PHODA version (PHODA-M) with people with LBP and categorised scores into low and high fear. The mean PT student score in our study falls within the low fear category used by Trost et al. [Citation38], while the scores of the OT and GN students fall within the high fear category [Citation38]. In that previous study [Citation38], the LBP patients with more negative PHODA scores reported a higher perception of harm and pain after a controlled activity, reinforcing the proposal that the PHODA is a useful indicator of how harmful activities are perceived to be.
The reasons for varying LBP beliefs across programmes are unclear. One possibility is that the observed beliefs reflect the amount of education relating to contemporary pain science across programmes. For example, PT students typically receive more education about pain than OT and GN students [Citation23,Citation24], and a greater amount of education on LBP in psychology lectures than other healthcare students [Citation25]. The relatively poor beliefs of nursing students are consistent with other data on poor pain knowledge among nursing students [Citation39,Citation40].
The aforementioned differences between programmes, and the non-availability of some year groups in GN, warrants caution in interpreting how LBP beliefs evolved within programmes over the course of study. However, a simple visual inspection of suggests that students in the later years of the PT programme have more positive beliefs than PT students commencing the programme, unlike the OT and GN students. Notwithstanding the preliminary nature of this finding, it is consistent with other studies reporting that PT students in later years of study have significantly more positive beliefs than first year PT students, without this pattern being seen in nursing students [Citation23,Citation27,Citation35]. Similarly, multiple studies have shown significant improvement in students’ knowledge, skill, attitudes and beliefs regarding pain as a result of curricula that overtly incorporate pain education into their training [Citation37].
Student characteristics and LBP beliefs
Data on whether male students have more positive LBP beliefs than females is conflicting. Some data suggests male students may be less pessimistic about the inevitable consequences of LBP [Citation35], yet many studies show no sex differences [Citation27,Citation38]. Interestingly, we are aware of no studies reporting poorer pain beliefs in males. The societal acceptability of expressing pain has been reported as being greater among females [Citation41], which may partly explain these differences in beliefs and that females are more likely to report greater pain-related disability than males [Citation42]. Interestingly, a qualitative study [Citation43] found that clinicians are more likely to advocate avoidance of activity for women with persistent spinal pain, based on stereotypes such as the belief that strength is a characteristic of males more than females.
We found that LBP status had no significant relationship with student beliefs. This is consistent with most [Citation23,Citation26,Citation28–30] but not all [Citation35], previous studies of healthcare students. LBP status has been found to be associated with LBP beliefs in qualified healthcare professionals [Citation44], as well as LBP patients [Citation45]. One proposed reason [Citation28] for the lack of a similar association among students is the relatively good health and mostly painfree status of these populations, with 41% reporting no LBP whatsoever.
Dominance of the ‘tissue injury’ model
The traditional perspective is that LBP is caused by activities involving large spinal loads such as bending and lifting, and attempts to prevent or treat LBP should avoid or reduce exposure to these loads. Such beliefs are pervasive, amongst people with and without LBP [Citation16,Citation46,Citation47]. However, the evidence demonstrates that persistent LBP is not simply caused by exposure to high loads [Citation7–9], nor is it necessarily best treated by approaches which seek to ‘protect’ the back from high loads, such as ergonomics interventions and manual handling training [Citation48]. There is even preliminary evidence that manual handling education causes further deterioration in LBP beliefs [Citation32,Citation49]. While an isolated episode of LBP might be triggered by a daily activity such as bending [Citation6], it is clear that persistence and recurrence is related to many other factors including unhelpful cognitions about the safety of activity and loading the spine, and other biopsychosocial factors which can ‘sensitise’ the person [Citation50]. Rather than trying to avoid common daily activities, people may benefit – in terms of LBP as well as general health – from being encouraged to practice such activities, and develop their strength and confidence.
Enhancing LBP beliefs among healthcare students and professionals
These findings have implications for the healthcare students personally, in terms of how they respond to episodes of LBP they will likely develop during their life. There are also important implications for their clinical practice and the advice provided to patients with LBP encountered professionally. The manner in which we convey concerns about the nature of a person’s LBP, and their ability to do common daily activities, can have significant impact [Citation43,Citation51]. Furthermore, healthcare professionals with more negative LBP beliefs are more likely to provide non-evidence-based care such as recommending avoidance of activity [Citation14,Citation15,Citation52].
To address inaccurate student beliefs about the safety of activities, and by extension the vulnerability of the spine, radical educational reform is urgently needed. An initial starting point is comprehensive education about what pain does, and does not, indicate, as this has been shown to modify the LBP beliefs of both healthcare students [Citation30,Citation53,Citation54] and professionals [Citation55–57], and may reflect the beliefs of PT students consistently being higher than other student groups. However, considering the variation in LBP beliefs between healthcare groups [Citation58], and the increasing importance of multi-disciplinary management of people with chronic health complaints such as LBP and associated comorbidities such as depression and obesity, better and more consistent pain education across healthcare disciplines is needed. This education would ideally overlap between different professional groups, both in academic and clinical environments, to ensure that HCP advice does not further disable or distress the person with LBP. Interprofessional education (IPE) is increasingly proposed as a means of preparing HCPs to collaboratively provide patient–centred clinical care for patients with pain [Citation59,Citation60], with some preliminary evidence demonstrating positive outcomes from pain-focussed IPE [Citation61–64].
The translation of LBP beliefs into activity advice is critical as it is clear that neither changes in LBP beliefs, nor changes in stated management practice based on case vignettes, after additional training appear to alter either how HCPs practice or improve outcomes [Citation56,Citation65]. This inability to change practice likely reflects feelings of professional inadequacy, as musculoskeletal clinicians are often trained in a ‘tissue injury’ model rather than a truly biopsychosocial model [Citation66,Citation67]. As such, changing how LBP is managed likely requires a radical overhaul of both pre-qualification and post-qualification training programmes, and the care pathways offered for LBP [Citation68,Citation69].
Finally, there may well be a need for greater community and public health education to transform alter how wider society views LBP [Citation47,Citation70]. We are aware that the scale of such a task is considerable, requiring the collaboration of multiple professional groups and sectors, yet we argue it is necessary considering the scale of the burden of LBP.
Limitations
The observational study design used cannot determine causal relationships. Convenience sampling from one university in one country limits the generalisability of the results and makes the study prone to selection bias [Citation71]. Generalisability is also reduced as most students were female (78%), though this is largely reflective of the professions studied in that country. A key limitation is that the psychometric properties of the specific 12-item mPHODA version used in our study have not been established. While longer versions of the PHODA survey have been shown to be reliable and valid [Citation14,Citation72], and the internal consistency of our version appears similar to other versions [Citation14,Citation73,Citation74], the lack of established validity must be considered when interpreting these findings. There is no known value, or cut-off, which signifies optimal beliefs regarding these common daily activities on the mPHODA. Bending in a more rounded posture is considered more dangerous than bending in a more upright posture [Citation58,Citation75,Citation76], and while such a belief is not strongly supported by data, it must be acknowledged that the mPHODA does not discriminate between these bending styles. The definition of significant LBP used was narrow, such that other functional limitations may have been missed. The extent to which other factors such as lecturer and practice educator beliefs, or other previous education, influenced mPHODA scores was not evaluated.
Conclusion
LBP beliefs about the harmfulness of common daily activities for the back differ between students on different healthcare programmes. PT students have significantly more positive beliefs than OT and GN students, with no significant difference between OT and GN beliefs. The implications of such variation in LBP beliefs on the advice provided to patients, and how these might be enhanced, is worthy of further study. Despite considerable progress in our understanding of pain, the beliefs of student healthcare professionals regarding pain still requires considerable enhancement.
Ethics approval
The study was approved by the University of Limerick (U.L.) Research Ethics and Governance Committee (2015-05-18-EHS). Participating students gave written informed consent by choosing to complete the questionnaire.
Acknowledgements
Thanks to the students, course directors and staff of the relevant programmes for facilitating this study. This study was not funded. The publication of this article was funded by the Qatar National Library.
Disclosure statement
No potential conflict of interest was reported by the authors.
Correction Statement
This article has been republished with minor changes. These changes do not impact the academic content of the article.
References
- Hartvigsen J, Hancock MJ, Kongsted A, et al. What low back pain is and why we need to pay attention. Lancet. 2018;391:2356–2367.
- Maher C, Underwood M, Buchbinder R. Non-specific low back pain. Lancet. 2017;389:736–747.
- Hoy D, March L, Brooks P, et al. The global burden of low back pain: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis. 2014;73:968–974.
- Stanton TR, Henschke N, Maher CG, et al. After an episode of acute low back pain, recurrence is unpredictable and not as common as previously thought. Spine. 2008;33:2923–2928.
- Menezes Costa LDC, Maher CG, Hancock MJ, et al. The prognosis of acute and persistent low-back pain: a meta-analysis. Can Med Assoc J. 2012;184:E613–E624.
- Steffens D, Ferreira ML, Latimer J, et al. What triggers an episode of acute low back pain? A case–crossover study. Arthritis Care Res. 2015;67:403–410.
- Roffey DM, Wai EK, Bishop P, et al. Causal assessment of workplace manual handling or assisting patients and low back pain: results of a systematic review. Spine J. 2010;10:639–651.
- Wai EK, Roffey DM, Bishop P, et al. Causal assessment of occupational bending or twisting and low back pain: results of a systematic review. Spine J. 2010;10:76–88.
- Wai EK, Roffey DM, Bishop P, et al. Causal assessment of occupational lifting and low back pain: results of a systematic review. Spine J. 2010;10:554–566.
- Traeger A, Buchbinder R, Harris I, et al. Diagnosis and management of low-back pain in primary care. Can Med Assoc J. 2017;189:E1386–E1395.
- National Institute for Health and Care Excellence (NICE). Low back pain and sciatica in over 16s: assessment and management. NICE guideline [NG59]. London: NICE; 2016. [cited 2018 June] Available from: https://www.nice.org.uk/guidance/ng59
- Stochkendahl MJ, Kjaer P, Hartvigsen J, et al. National Clinical Guidelines for non-surgical treatment of patients with recent onset low back pain or lumbar radiculopathy. Eur Spine J. 2018;27:60–75.
- Qaseem A, Wilt TJ, McLean RM, et al. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2017;166:514–530.
- Houben RM, Ostelo RW, Vlaeyen JW, et al. Health care providers' orientations towards common low back pain predict perceived harmfulness of physical activities and recommendations regarding return to normal activity. Eur J Pain. 2005;9:173–183.
- Coudeyre E, Rannou F, Tubach F, et al. General practitioners' fear-avoidance beliefs influence their management of patients with low back pain. Pain. 2006;124:330–337.
- Darlow B, Dowell A, Baxter GD, et al. The enduring impact of what clinicians say to people with low back pain. Ann Fam Med. 2013;11:527–534.
- Gardner T, Refshauge K, Smith L, et al. Physiotherapists’ beliefs and attitudes influence clinical practice in chronic low back pain: a systematic review of quantitative and qualitative studies. J Physiother. 2017;63:132–143.
- Wertli MM, Rasmussen-Barr E, Weiser S, et al. The role of fear avoidance beliefs as a prognostic factor for outcome in patients with nonspecific low back pain: a systematic review. Spine J. 2014;14:816–836. e4.
- Grimshaw JM, Eccles MP, Lavis JN, et al. Knowledge translation of research findings. Implement Sci. 2012;7:50.
- Darlow B, Fullen BM, Dean S, et al. The association between health care professional attitudes and beliefs and the attitudes and beliefs, clinical management, and outcomes of patients with low back pain: a systematic review. Eur J Pain. 2012;16:3–17.
- Foster NE, Delitto A. Embedding psychosocial perspectives within clinical management of low back pain: integration of psychosocially informed management principles into physical therapist practice-challenges and opportunities. Phys Ther. 2011;91:790–803.
- Buchbinder R, van Tulder M, Öberg B, et al. Low back pain: a call for action. Lancet. 2018;391:2384–2388.
- Burnett A, Sze CC, Tam SM, et al. A cross-cultural study of the back pain beliefs of female undergraduate healthcare students. Clin J Pain. 2009;25:20–28.
- Briggs A, Slater H, Smith A, et al. Low back pain‐related beliefs and likely practice behaviours among final‐year cross‐discipline health students. Eur J Pain. 2013;17:766–775.
- Ali N, Thomson D. A comparison of the knowledge of chronic pain and its management between final year physiotherapy and medical students. Eur J Pain. 2009;13:38–50.
- Ferreira PH, Ferreira ML, Latimer J, et al. Attitudes and beliefs of Brazilian and Australian physiotherapy students towards chronic back pain: a cross‐cultural comparison. Physiother Res Int. 2004;9:13–23.
- Ryan C, Murphy D, Clark M, et al. The effect of a physiotherapy education compared with a non-healthcare education on the attitudes and beliefs of students towards functioning in individuals with back pain: an observational, cross-sectional study. Physiotherapy. 2010;96:144–150.
- Mitchell T, O'Sullivan PB, Smith A, et al. Biopsychosocial factors are associated with low back pain in female nursing students: a cross-sectional study. Int J Nurs Stud. 2009;46:678–688.
- Morris H, Ryan C, Lauchlan D, et al. Do medical student attitudes towards patients with chronic low back pain improve during training? A cross-sectional study. BMC Med Educ. 2012;12:10.
- Latimer J, Maher C, Refshauge K. The attitudes and beliefs of physiotherapy students to chronic back pain. Clin J Pain. 2004;20:45–50.
- Von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg. 2014;12:1495–1499.
- Horgan D. Investigation of the impact of people manual handling training on back beliefs [MSc Thesis]. University of Limerick; 2015.
- Kugler K, Wijn J, Geilen M, et al. The photograph series of daily activities (PHODA). Heerlen: The Netherlands; 1999.
- Matheve T, De Baets L, Bogaerts K, et al. Lumbar range of motion in chronic low back pain is predicted by task‐specific, but not by general measures of pain‐related fear. Eur J Pain. 2019. DOI:10.1002/ejp.1384
- Kennedy N, Healy J, O'Sullivan K. The beliefs of third-level healthcare students towards low-back pain. Pain Res Treat. 2014;2014:675915.
- Ung A, Salamonson Y, Hu W, et al. Assessing knowledge, perceptions and attitudes to pain management among medical and nursing students: a review of the literature. Br J Pain. 2016;10:8–21.
- Thompson K, Johnson MI, Milligan J, et al. Twenty-five years of pain education research—what have we learned? Findings from a comprehensive scoping review of research into pre-registration pain education for health professionals. Pain. 2018;159:2146–2158.
- Trost Z, France CR, Thomas JS. Examination of the photograph series of daily activities (PHODA) scale in chronic low back pain patients with high and low kinesiophobia. Pain. 2009;141:276–282.
- Chiu LH, Trinca J, Lim LM, et al. A study to evaluate the pain knowledge of two sub-populations of final year nursing students: Australia and Philippines. J Adv Nurs. 2003;41:99–108.
- Chow K, Chan JC. Pain knowledge and attitudes of nursing students: a literature review. Nurse Educ Today. 2015;35:366–372.
- Leung SM, Chung J. Beliefs about appropriate pain behaviour: gender differences between health care professionals and non‐health care professionals in Hong Kong. J Clin Nurs. 2008;17:2987–2992.
- Stubbs D, Krebs E, Bair M, et al. Sex differences in pain and pain-related disability among primary care patients with chronic musculoskeletal pain. Pain Med. 2010;11:232–239.
- Stenberg G, Fjellman-Wiklund A, Ahlgren C. ‘I am afraid to make the damage worse’ – fear of engaging in physical activity among patients with neck or back pain – a gender perspective. Scand J Caring Sci. 2014;28:146–154.
- Buchbinder R, Jolley D, Wyatt M. 2001 Volvo award winner in clinical studies: effects of a media campaign on back pain beliefs and its potential influence on management of low back pain in general practice. Spine. 2001;26:2535–2542.
- Camacho-Soto A, Sowa GA, Perera S, et al. Fear avoidance beliefs predict disability in older adults with chronic low back pain. Phys Med Rehabil. 2012;4:493–497.
- Darlow B, Perry M, Dean S, et al. Putting physical activity while experiencing low back pain in context: balancing the risks and benefits. Arch Phys Med Rehabil. 2016;97:245–251.e7.
- O’Keeffe M, Maher CG, Stanton TR, et al. Mass media campaigns are needed to counter misconceptions about back pain and promote higher value care. Br J Sports Med. 2018;pii: bjsports-2018-099691.
- Verbeek JH, Martimo KP, Karppinen J, et al. Manual material handling advice and assistive devices for preventing and treating back pain in workers. Cochrane Database Syst Rev. 2011;6:CD005958.
- Driessen MT, Proper KI, van Tulder MW, et al. The effectiveness of physical and organisational ergonomic interventions on low back pain and neck pain: a systematic review. Occup Environ Med. 2010;67:277–285.
- O'Sullivan P, Caneiro JP, O'Keeffe M, et al. Unraveling the complexity of low back pain. J Orthop Sports Phys Ther. 2016;46:932–937.
- Darlow B, Dean S, Perry M, et al. Easy to harm, hard to heal: patient views about the back. Spine. 2015;40:842–850.
- Kennedy N, Condon E, O'Sullivan K. Physiotherapy practice educators' beliefs towards low back pain and influence on student beliefs. Pain Rehabil J Physiother Pain Assoc. 2014;2014:4–10.
- Domenech J, Sánchez-Zuriaga D, Segura-Ortí E, et al. Impact of biomedical and biopsychosocial training sessions on the attitudes, beliefs, and recommendations of health care providers about low back pain: a randomised clinical trial. Pain. 2011;152:2557–2563.
- Shaheed CA, Maher CG, Mak W, et al. The effects of educational interventions on pharmacists’ knowledge, attitudes and beliefs towards low back pain. Int J Clin Pharm. 2015;37:616–625.
- O'Sullivan K, O'Sullivan P, O'Sullivan L, et al. Back pain beliefs among physiotherapists are more positive after biopsychosocially orientated workshops. Physiother Pract Res. 2013;34:37–45.
- Overmeer T, Boersma K, Main CJ, et al. Do physical therapists change their beliefs, attitudes, knowledge, skills and behaviour after a biopsychosocially orientated university course?. J Eval Clin Pract. 2009;15:724–732.
- Monnin D, Courvoisier DS, Genevay S. Modifying beliefs about back pain: A pilot study among healthcare professionals. Patient Educ Couns. 2016;99:665–670.
- Nolan D, O'Sullivan K, Stephenson J, et al. How do manual handling advisors and physiotherapists construct their back beliefs, and do safe lifting posture beliefs influence them? Musculoskelet Sci Pract. 2019;39:101–106.
- Gordon DB, Watt-Watson J, Hogans BB. Interprofessional pain education—with, from, and about competent, collaborative practice teams to transform pain care. Pain Rep. 2018;3:e663.
- Hogans BB, Watt-Watson J, Wilkinson P, et al. Perspective: update on pain education. Pain. 2018;159:1681–1682.
- Irajpour A. Interprofessional education: a facilitator to enhance pain management? J Interprof Care. 2006;20:675–678.
- Hadjistavropoulos HD, Juckes K, Dirkse D, et al. Student evaluations of an interprofessional education experience in pain management. J Interprof Care. 2015;29:73–75.
- Hunter JP, Stinson J, Campbell F, et al. A novel pain interprofessional education strategy for trainees: assessing impact on interprofessional competencies and pediatric pain knowledge. Pain Res Manag. 2015;20:e12–e20.
- Salam T, Saylor JL, Cowperthwait AL. Attitudes of nurse and physician trainees towards an interprofessional simulated education experience on pain assessment and management. J Interprof Care. 2015;29:276–278.
- Overmeer T, Boersma K, Denison E, et al. Does teaching physical therapists to deliver a biopsychosocial treatment program result in better patient outcomes? A randomized controlled trial. Phys Ther. 2011;91:804–819.
- Synnott A, O’Keeffe M, Bunzli S, et al. Physiotherapists may stigmatise or feel unprepared to treat people with low back pain and psychosocial factors that influence recovery: a systematic review. J Physiother. 2015;61:68–76.
- Synnott A, O’Keeffe M, Bunzli S, et al. Physiotherapists report improved understanding of and attitude toward the cognitive, psychological and social dimensions of chronic low back pain after Cognitive Functional Therapy training: a qualitative study. J Physiother. 2016;62:215–221.
- International Association for the Study of Pain (IASP). International Association for the Study of Pain: IASP pain curricula. [cited January 5, 2019] Available from: https://www.iasp-pain.org/Education/CurriculumDetail.aspx?ItemNumber=2055
- Hush JM, Nicholas M, Dean CM. Embedding the IASP pain curriculum into a 3-year pre-licensure physical therapy program: redesigning pain education for future clinicians. Pain Rep. 2018;3:e645.
- Buchbinder R, Jolley D. Population based intervention to change back pain beliefs: three year follow up population survey. BMJ. 2004;328:321.
- Yu I, Tse S. Workshop 6 - sources of bias in cross-sectional studies; summary on sources of bias for different study designs. Hong Kong Med J. 2012;18:226–227.
- Kugler K, Wijn J, Geilen M, et al. The photograph series of daily activities (PHODA). CD-ROM Version 1. Heerlen, The Netherlands: Institute for Rehabilitation Research and School for Physiotherapy; 1999.
- Leeuw M, Goossens ME, van Breukelen GJ, et al. Measuring perceived harmfulness of physical activities in patients with chronic low back pain: the Photograph Series of Daily Activities—short electronic version. J Pain. 2007;8:840–849.
- Oliveira CB, Franco MR, Demarchi SJ, et al. Psychometric properties of the photograph series of daily activities-short electronic version (PHODA-SeV) in patients with chronic low back pain. J Orthop Sports Phys Ther. 2018;48:719–727.
- Nolan D, O'Sullivan K, Stephenson J, et al. What do physiotherapists and manual handling advisors consider the safest lifting posture, and do back beliefs influence their choice? Musculoskelet Sci Pract. 2018;33:35–40.
- Caneiro JP, O'Sullivan P, Lipp OV, et al. Evaluation of implicit associations between back posture and safety of bending and lifting in people without pain. Scand J Pain. 2018;18:719–728.
