Abstract
Purpose
We conducted a systematic review with meta-analysis to examine the short- and long-term effects of virtual reality training (VRT) on pain, range of motion (RoM), kinesiophobia and perceived function in patients with chronic neck pain (CNP).
Methods
We searched the PubMed, Scopus, and PEDro databases for studies assessing effect of VRT against conventional therapy in CNP patients. Separate analyzes were performed for short-term (immediately after the intervention) and long-term (at follow-up) outcomes. Risk of bias was assessed with PEDro scale and the quality of evidence was assessed according to GRADE guidelines.
Results
We found 11 studies, 8 of which were eligible for meta-analysis. Most studies had good methodological quality (6–8 points on the PEDro scale). The analysis showed significant differences in favour of VRT for neck disability index (long-term), kinesiophobia (long-term), and neck flexion RoM (short-term). No significant differences were found for pain intensity in the short- and long-term assessments. Heterogeneity between effect sizes was high in most analyzes, and the quality of evidence was low.
Conclusion
Low quality evidence suggests that VRT may contribute to long-term improvements in perceived function and kinesiophobia in CNP patients compared with conventional training programs. However, VRT and conventional training programs have similar effects on overall neck RoM and pain intensity.
Introduction
Up to 67% of people suffer from neck pain (NP) at some point in their lives [Citation1]. The majority of NP is referred to as “'nonspecific”, because it results from postural and mechanical causes rather than organic pathology [Citation2,Citation3]. In most cases, NP resolves within 4–6 weeks, but one-third of those affected later develop chronic neck pain (CNP), which affects 10%–24% of the general population, with an even higher prevalence in older adults [Citation4–7]. There are several factors that may contribute to NP or transition from acute to chronic pain status, including history of trauma, advanced age, genetics, female gender, beliefs, coping style, expectations, stress, anxiety and cognitive impairment [Citation8,Citation9]. Symptoms commonly experienced by patients with CNP (e.g. cervical spine pain, pain radiating to the back of the head/shoulders/upper limbs, headaches, stiffness, numbness or weakness in the upper limbs, balance problems) can lead to reduced work productivity, increased work absenteeism, and increased insurance costs [Citation2,Citation10].
Conventional CNP treatment include exercise (e.g. resistance exercise, mobility, muscle reeducation), physical modalities (e.g. low-level laser therapy), acupuncture, mind-body practice, medications for pain relief, pain education, manipulation, mobilisation or dry needling, but the improvement in function is small to moderate, with no long-term benefit across most interventions [Citation11–13]. Another treatment option for CNP management is virtual reality training (VRT) which has become increasingly common in clinical medicine over the past decade [Citation14]. Virtual reality (VR) allows users to view and interact with a simulated 3D virtual world (e.g. videos or games) and to immerse themselves in a multisensory experience, so that they can feel as a part of the virtual environment [Citation15,Citation16]. This sense of presence redirects individual’s attention towards stimuli emitted by VR system [Citation17]. Consequently, an individual’s ability to respond to noxious stimuli and attend to nociceptive neural signals is diminished, resulting in a lower perception of pain [Citation18]. Redirecting attention to external stimuli (rather than body movements) has also been shown to benefit motor learning and performance [Citation19,Citation20]. Immersion in the simulation is enhanced by integrating multisensory (e.g. visual, auditory, and tactile) experiences with various devices (e.g. a head-mounted display (HMD) or wearable haptic devices) [Citation16,Citation17]. Although the current evidence on VR analgesia is dominated, to a great extent, by studies on acute and procedural pain, VR has also been shown to influence pain in chronic populations, such as patients with fibromyalgia, complex regional pain syndrome, and neuropathic pain associated with spinal cord injury [Citation21–24]. A recent meta-analysis also found significant reduction in pain intensity and kinesiophobia in patients with chronic low back pain after a VR intervention and at follow-up [Citation25]. However, in their meta-analysis, Mallari et al. [Citation26] concluded that in chronic pain conditions VR is effective in reducing pain intensity during and immediately after the VR exposure, but not also in the long-term.
The use of VRT in NP patients aims to improve impaired cervical kinematics (reduced RoM, accuracy or speed of movement, smoothness and stability of neck movement) and reduce fear of movement in this population [Citation27]. In recent years, studies investigating the potential of VRT for the treatment of CNP were conducted and yielded some promising results. For instance, Rezaei et al. [Citation28] found greater improvement in visual analogue scale (VAS) and neck disability index (NDI) scores in the VRT group compared with conventional proprioceptive training in patients with CNP after 4-week intervention. Similarly, Bahat et al. [Citation29] reported that VR home training had benefits in improving disability, NP and kinematics in the short and medium term after a 4-week intervention compared with laser kinematic training. However, to the best of our knowledge, there is no systematic review on this topic in the current scientific literature. Therefore, the aim of this paper is to perform a systematic review with meta-analysis to explore the short- and long-term effects of VRT on pain, RoM, kinesiophobia and perceived function in patients with CNP. Consistent with previous evidence, we hypothesised that VRT would have only short-term beneficial effects in patients with CNP. The use of VR in pain management of patients with CNP could reduce the use of analgesics and their unwanted side effects, allow patients to self-treat in their home environment, reduce the socioeconomic burden, and contribute to patient motivation and adherence.
Methods
Search strategy and inclusion criteria
The review was conducted according to PRISMA guidelines. The review was not prospectively registered. The search was performed in January 2023. Both authors independently performed all search steps, and any disagreements were resolved by discussion. We searched the PubMed, Scopus and PEDro databases. For PubMed and Scopus, we used the following search string: (virtual reality OR virtual training OR virtual reality exposure therapy) AND (neck pain OR neck syndromes). In the PEDro database, we used the simple search option and separately entered three individual combinations of words (i.e. ‘neck pain virtual reality’, ‘virtual reality neck’ and ‘virtual training pain’ were used). In addition, we reviewed the reference lists of identified systematic reviews on the topic, and performed additional non-systematic search of the GoogleScholar database. The records were imported into Mendeley (version 1.19.8) to remove the duplicates, and then exported into Microsoft Excel software for further examination.
The inclusion criteria, structured according to the PICOS tool [Citation30], were determined as follows.
P (population): Any adult or older adult population with chronic NP (duration > 12 weeks).
I (Intervention): Exercise or physical therapy intervention using VR technology.
C (Comparison): Conventional exercise or physical therapy.
(Outcome): Outcomes describing RoM, pain (VAS), function (NDI) and kinesiophobia.
S (Study design): For meta-analysis, we included randomised controlled trials and other clinical trials with at least two groups (VR and control exercise/therapy groups). Single-group clinical studies and feasibility studies were included only in the narrative synthesis. Articles published as conference papers, editorials, opinion papers and non-scientific journals, and any articles not published in English, were excluded.
Data extraction
The data extraction was carried out independently by both authors and disagreements were resolved through additional discussion. The extracted data included: (a) baseline, post-intervention and follow-up data (means and standard deviations) for all eligible outcome measures for VR and control groups; percent changes were considered instead of pre-post data when available (b) baseline demographics of participants (sex, age, body height, body mass, body mass index); (c) intervention characteristics (VR intervention description, duration of the intervention, weekly frequency, volume (number of exercises, sets, and repetitions), breaks, and supervision). Data were carefully collected into Microsoft Excel 2016 (Microsoft, Redmond, WA, USA). If the data were presented in a graphical form, we used GetGraphDataDigitalizer software (version 2.26.0.20) to obtain the means and standard deviations. In case of missing data, the authors of the articles were contacted by e-mail and ResearchGate. A reminder was sent after 14 days, and if no reply was received after the second inquiry, the data was considered irretrievable.
Risk of bias and quality of evidence assessment
Both authors evaluated the risk of bias of the included studies using the PEDro scale which assesses study quality based on a 10 items [Citation31]. Potential disagreements between the reviewers were resolved by discussion. Studies scoring from 9 to 10 were considered as ‘excellent’, 6 to 8 as ‘good’, 4 to 5 as ‘fair’, and <4 as ‘poor’ quality. The PEDro scale was selected because it was specifically developed to evaluate the quality of clinical trial studies investigating physical therapy interventions [Citation32].
The quality of evidence was assessed according to GRADE guidelines [Citation33]. GRADE guidelines encompass 5 main domains (risk of bias, imprecision, inconsistency, indirectness, and publication bias) to categorise evidence quality. The comparisons were classified as representing either high, moderate, low or very low quality of evidence. The level of evidence was downgraded if: (a) there was a substantial heterogeneity between the studies (I2 > 50% or statistically significant heterogeneity test (inconsistency); (b) more than 25% of studies were classified as fair or poor quality (risk of bias); (c) the studies assessed the effects of the intervention indirectly (e.g. population, intervention or outcome not being representative of the research question) (indirectness), (d) when a large CI was observed, or when the total number of participants was <300 (imprecision) (e) when the study results provided differed from the original protocol or study objectives (publication bias) [Citation34].
Data analysis
The meta-analysis was carried out in Review Manager (Version 5.3, Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, London, UK). Although there is no consensus on the minimal number of studies required for a meta-analysis [Citation35], we only performed the analyses when three or more studies could be included. Before the results were entered into the meta-analytical model, the pre-post differences and pooled standard deviations were calculated according to the following formula SD = √[(SD2pre + SD2post)–(2 × r × SDpre × SDpost). The correction value (r), which represents the pre-test–post-test correlation of outcome measures, was conservatively set at 0.75. We used continuous outcomes meta-analysis with a random-effects model and inverse variance method to obtained the pooled effects. The effect sizes were expressed as standardised mean difference (SMD), with 95% confidence intervals (CI) reported alongside to provide the precision of the overall effect estimate [Citation36]. Statistical heterogeneity among studies was determined with the I2 statistics. According to Cochrane guidelines, the I2 statistics of 0% to 30% might not be important, 30 to 60% may represent moderate heterogeneity, 50–90% may represent substantial heterogeneity, and 75–100% indicates considerable heterogeneity. In case of substantial heterogeneity between the studies, a sensitivity analysis was performed by examining the effect of exclusion of studies that differed significantly from the pooled effect.
Results
General overview of the search results
We identified 147 records through a database search and 111 records through an additional search (GoogleScholar, reference lists). After duplicates were removed, 144 records were screened. In a next step, 24 articles were screened for eligibility. A total of 8 studies were eligible for meta-analysis. The detailed summary of the search process is shown in . Both men and women participated in all studies. In most studies, the participants were adults (range of means for age: 26.6–53.1 years), except in the study by Beltran-Alacreu et al. [Citation37] which examined older adults (81.8 ± 6.82 years). This study was also the only one that investigated a non-immersive type of VRT. Across studies, weekly frequency ranged from 2 to 6 and session durations ranged from 5 to 45 min. It should be noted, however, that in some programs, the program was delivered multiple times per day (e.g. 4 times per day for 5 min). Six studies also included follow-up measurements after 4 weeks to 6 months. In most studies, the control groups performed similar exercise program as the experimental group, only without VRT. In one study, the participants in the control group did not perform the exercises, but were allowed to continue with their ongoing physical therapy [Citation38]. In all studies, the participants had to report to suffer from neck pain for at least 12 weeks. In most studies (n = 7), the intervention was supervised. In addition, 2 studies [Citation29,Citation38] involved home-based exercises and in one study, the participants performed the exercises under supervision, but were also encouraged to perform the exercise at home [Citation27]. The detailed intervention descriptions are shown in , and study characteristics (patients, outcome measures, main findings) are presented in .
Figure 1. The study search and selection process.
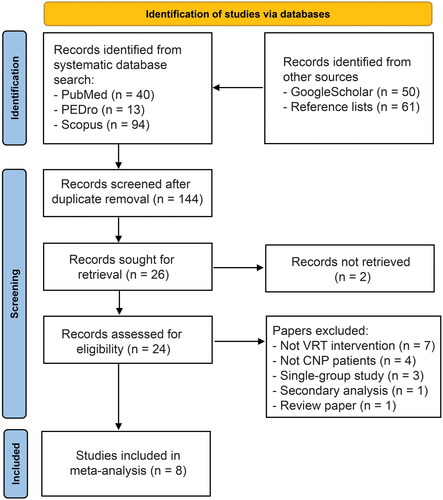
Table 1. Intervention descriptions of included studies.
Table 2. Characteristics of included studies.
Assessment of study quality
The assessment of study quality according to Pedro Scale is shown in . Most studies were of good quality, with 6 reaching a score between 6 and 8. One additional study was of fair quality (4 points) and one was of poor quality (3 points).
Table 3. Assessment of study quality with Assessment of study quality with Pedro Scale.
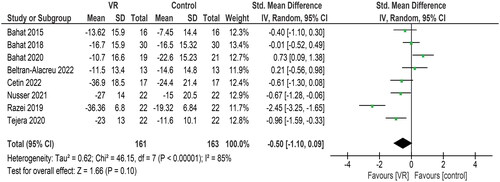
Effects of VR on neck pain (VAS)
Eight studies included in the meta-analysis (161 and 163 participants in VR and control groups, respectively) assessed neck pain with VAS scales (). Overall, there was low-quality evidence for a moderate, but non-significant (CI crossing the 0) effect of VRT (SMD = −0.50; CI = −1.10 to 0.09) The study effects were highly heterogenous (I2 = 85%). Removing studies of poor and fair quality did not affect the SMD nor the precision of the effect estimate (SMD = −0.60; CI = −1.27 to 0.16). Five studies (102 and 99 participants in VR and control groups, respectively) also included a follow up measurement. The pooled effect on VAS was not statistically significant (SMD = −0.39, CI = −0.73 to 0.15), with high heterogeneity between the studies (I2 = 89%). In summary, there is low quality evidence that VRT is not superior to conventional therapy in short-term and at follow-up assessment.
Figure 2. The meta-analysis for neck pain (VAS).
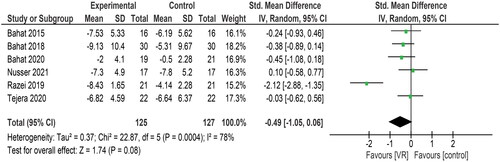
Effects of VR on neck disability index (NDI)
Six studies included in the meta-analysis (125 and 127 participants in the VR and control groups, respectively) reported NDI scores (). Overall, the studies tended to show a moderate but not significant effect VR (SMD = −0.49; CI = −1.05 to 0.06). Again, the study effects were highly heterogenous (I2 = 78%). Five out of six studies (98 and 99 participants in the VR and control groups, respectively) also reported the NDI in a follow up period. Here, the overall effect was large and statistically significant (SMD = −0.95; CI = −1.70 to −0.20), but the heterogeneity between the studies was high (I2 = 83%). In summary, low-quality evidence suggests that VRT training is not superior to conventional therapy in terms of NDI in the short term but may provide additional benefits at follow-up.
Figure 3. The meta-analysis for neck disability index (NDI).
Effects of VR on Tampa scale for kinesiophobia
Three studies included in the meta-analysis (68 participants in the VR and control groups each) reported the Tampa Scale for Kinesiophobia (TSK) scores. The overall effect was small and statistically non-significant (SMD = −0.19; CI = −0.52 to 0.15), while the studies were very heterogenous (I2 = 0%). All three studies also reported the scores at follow-up. Here, the overall effect was moderate and statistically significant (SMD = −0.69; CI = −1.34 to −0.03) with moderate heterogeneity between the studies (I2 = 67%). In summary, moderate-quality evidence suggests that VRT provides no additional benefit in the short term compared with conventional therapy, whereas low-quality evidence suggests that VRT may provide additional benefits in the follow-up period.
Effects of VR on neck RoM
Four studies included in the meta-analysis (80 and 79 participants in the VR and control groups, respectively) reported on neck RoM. For neck flexion, the studies tended to show a positive overall effect of VR (SMD = 0.53; CI = 0.01–1.06), while moderate heterogeneity between the studies was present (I2 = 67%). For the neck extension, the effect was slightly smaller and non-significant (SMD = 0.41; CI = −0.09 to 0.91), but still tended towards a positive effect of VR, while moderate heterogeneity between the studies was present (I2 = 58%). For left and right rotation RoM (SMD = 0.06 and −0.29, there was no statistically significant effect CI = −0.25 to 0.38 for left rotation, CI = −0.70 to 0.11 for left rotation). Overall, low-quality evidence suggests a possible additional benefit of VRT over conventional therapy for neck flexion RoM, and no additional benefit for other RoM measures.
Neck RoM was also assessed in a randomised clinical trial, investigating VR exercises in comparison to neck exercises without VR [Citation39]. This study was not included in the meta-analysis because they reported combined flexion and extension RoM, while the other studies reported RoM for each direction separately. While they reported a significant time effect for rotation RoM (p < 0.01), the interaction between group and time was not significant (p = 0.630), indicating no additional effect of VR over the control group. There were no statistically significant time effects (p = 0.46–0.71) nor for interactions (p = 0.18–0.99, p = 0.18, respectively) for flexion-extension and lateral flexion movements. In addition, the post-hoc tests showed no within-group differences in either group between baseline and follow up measures for rotation motion [Citation39].
Discussion
The objective of this systematic review and meta-analysis was to examine the short-term (immediately after intervention) and long-term (at follow-up) effects of VRT on pain, RoM, kinesiophobia and perceived function in patients with CNP. In the meta-analysis, we compared the short and long-term effects of VRT with conventional exercise programs, performed by control groups. Interventions included a variety of exercises, including proprioceptive training, fast and accurate head control training, cervical joint mobility exercises, strengthening or stretching of the deep neck muscles, stair climbing, aqua therapy, pedalling, pulleys and obstacle walking. Some control groups also performed exercises with lasers. The VRT groups generally performed exercises similar to those in the control groups, but in a VR environment. Eleven studies were included in this review and eight were eligible for the meta-analysis. Low-quality evidence was found to suggest possible differences in favour of the VR interventions for NDI in the long term, for TSK in the long term, and for neck flexion RoM in the short term. However, no significant differences were found in pain intensity in the short and long-term, in NDI and TSK in the short-term, in neck extension RoM in the short-term and in both rotations in the short-term. VRT may achieve significantly better results in improving perceived function and kinesiophobia in the long term compared with conventional exercise programs. However, VRT and conventional exercise programs have got similar effects on overall neck RoM and pain intensity. Most evidence found in this review was of low quality, which calls for further research. Given the high statistical heterogeneity in the meta-analysis and many differences between the studies in terms of intervention and population, future studies should specifically assess the effects of different types and applications of VRT, explore the effects of VRT with respect to patient characteristics (e.g. pain duration, pain intensity, kinesiophobia), and include longer intervention and follow-up periods.
The tasks performed in the VR interventions varied widely, but were mostly intended to improve RoM, proprioception, motion accuracy and motion speed, and extinguish the movement-pain association (see for details). Regardless of the task performed by subjects, by shifting attention to external stimuli, VRT aims to reduce pain and allow patients to experience movements they would otherwise be afraid of. With one exception [Citation28], studies have used an immersive VR system in which subjects wore head-mounted displays to engage with the VR world. The diversity of VR interventions indicates that a critical evaluation of the broader literature is needed not only in terms of treatment effects, but also in terms of the technology, user interface, and purported mechanisms by which VRT provides additional benefits over conventional movement therapy.
Effects of VR on NP
Neck pain was assessed in eight studies included in the meta-analysis. Five of these studies also included a follow-up measurement. The meta-analysis showed that the pooled effect favoured VRT over conventional exercise both in the short term and at follow-up, but the effect was small to moderate and not statistically significant. Therefore, we can conclude that VRT has similar effects on neck pain as conventional exercise (i.e. the difference between VRT and convention exercise is not significant). In one study [Citation28], the effect of VRT (relative to control group) was very large both after the intervention and at the 5-week follow-up. In this study a VRT program (a game called Cervigame®) reduced NP about twice as much as a conventional proprioceptive exercise program, performed in the control group. This larger effect compared to other studies could be due to an effective VR program, or perhaps to a sample that included relatively young participants (VRT group: 36.19 ± 9.80 years; control group: 31.23 ± 9.49 years) with only mild functional disability according to NDI. We assume that younger patients may adapt more easily to modern forms of treatment, such as VRT, which may be the reason for the better outcomes. In their study, Liu et al. [Citation42] investigated the differences in VR experience and acceptance between older adults and college students and suggested that VR headsets may be too complicated for older people to use on a daily basis. In addition, older people were more likely to report dizziness and anxiety during VR use [Citation42]. Older adults may need more time to adapt to VR [Citation43], thus, it could be hypothesised that VR would have more positive effects for them on the long-term, but the evidence for this hypothesis is currently lacking.
A study included in our meta-analysis investigated the effects of a home-based VR program in fighter and helicopter pilots with NP and showed that VR training had negative effects on VAS [Citation38]. The authors of the study suggested this may be due to the busy schedules of the pilots, which led to poor compliance in self-exercising [Citation38]. The VR home exercise program was also investigated in another study, which concluded that the benefits of using VR compared with traditional exercise were insufficient to recommend its use [Citation29]. Therefore, supervised VR programs are recommended, because they show a more significant decrease in NP compared to home-based VR programs.
Heterogeneous conclusions regarding the effects of VRT on pain intensity in CNP patients are also found in other studies not included in our meta-analysis. While Zauderer et al. [Citation44] reported a decrease in neck pain in their single-group study, Glavare et al. [Citation45] found a significant increase in pain during the VR sessions and a nonsignificant increase in pain after intervention. Furthermore, Harvie et al. [Citation46] found no differences in neck pain between baseline and post VR exercise assessment in their short-term study. Glavare et al. [Citation45] attributed the increase in pain to a lack of inhibition and enhanced excitability in central nervous system processing of pain, which is present in several chronic pain conditions. An imbalance between inhibition and excitation in the central nervous system may promote pain during treatment in this patient group [Citation45,Citation47]. Note, however, that this effect was observed only during, not after, exercise [Citation45].
Effects of VR on NDI
NDI was assessed in six studies included in the meta-analysis. Five of the six studies also reported the NDI in a follow-up period. The meta-analysis showed that the pooled effect favoured VRT compared with conventional exercise for both in the short-term and at follow-up, but the effect was statistically significant only at follow-up. Since we are mainly interested in long-term changes in patients with chronic pain, we can conclude that VRT can have a significant impact on perceived function in patients with CNP in comparison to conventional exercise. For the patients with chronic musculoskeletal conditions, the pain is an ongoing rather than a transient experience. Therefore, interventions that focus more on restoring function rather than escaping the experience of pain per se are more appropriate for them [Citation48]. We believe that the improvement in perceived function after VRT is a more important outcome than improvement in pain from the perspective of CNP patients.
Effects of VR on TSK
TSK scores were reported in three studies included in the meta-analysis. All three studies also reported TSK scores at follow-up. The meta-analysis showed that the pooled effect statistically significantly favoured VRT only at follow-up. TSK was also assessed in two single-group studies that were not included in meta-analysis. Zauderer et al. [Citation44] reported a decrease in TSK score after intervention and at follow-up, but did not indicate whether the difference was statistically significant. Glavare et al. [Citation45] came to similar conclusions, reporting a significant decrease in TSK score after the VRT intervention. In their meta-analysis, Wang et al. [Citation49] concluded that VR technology has the potential to reduce the level of kinesiophobia, especially when combined with exercise intervention. Furthermore, Asiri et al. [Citation50] found that kinesiophobia was significantly correlated with pain intensity, proprioception and functional performance in CNP patients. In chronic pain patients, reducing kinesiophobia is crucial because confronting the fear during exercise or active exercises can accelerate recovery [Citation49].
Effects of VR on neck RoM
Four studies assessed neck RoM after the VRT intervention. Meta-analysis showed that the pooled effect statistically significantly favoured VRT only for neck flexion, where the overall effect was just above the significance threshold. Neck RoM was also examined in two single-group studies that were not included in the meta-analysis. Tejera et al. [Citation39] found no additional effect of VR over the control group performing neck exercises without resistance. Zauderer et al. [Citation44] reported possible increases in neck flexion and left axial rotation, but no statistical analysis was performed in their study. From our results, we can conclude that VRT may have a positive effect on perceived function, but this does not mean that objective measures of RoM also improve significantly. Consistent with our conclusions, Rudolfsson et al. [Citation51] observed weak associations between RoM measures and greater self-reported head movement related problems, activity limitations, symptoms and lower physical activity in people with neck pain.
Strengths and limitations
According to the Pedro scale, most of the studies included in the meta-analysis (six out of eight) had good methodological quality, and only one had fair and one poor quality. However, it should be noted that studies had small sample sizes (total sample size across studies ranged from 14 to 90). Most meta-analyses favoured VRT, with no statistically significant pooled effect, which may be the consequence of underpowered studies. In addition, study effects were highly heterogeneous. For the most part, the interventions were similar across the studies, with the main differences in the exercises performed in control groups, and methods used for VRT. In addition, studies differed in regard to the level of supervision (e.g. two studies included in meta-analysis performed home-based programs). It is possible that different conclusions would have been drawn if the studies had been more homogeneous and included a larger sample size.
Conclusions
The objective of this systematic review and meta-analysis was to investigate the short-term and long-term effects of VRT on pain, RoM, kinesiophobia and perceived function in patients with CNP. Low quality evidence for effects in favour of VR interventions on NDI (long-term), TSK (long-term), and neck flexion RoM (short-term) was found. However, no significant differences were found for pain intensity for short- and long-term, for NDI and TSK for short-term, for neck extension RoM for short-term, and for both rotations for short-term. VRT can achieve significantly better results in improving perceived function and kinesiophobia in CNP patients in the long term compared with conventional training programs. However, VRT and conventional training programs have similar effects on overall neck RoM and pain intensity. The quality of evidence in this review must be considered low, mainly because of the large heterogeneity between studies and the small number of studies.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Viljanen M, Malmivaara A, Uitti J, et al. Effectiveness of dynamic muscle training, relaxation training, or ordinary activity for chronic neck pain: randomised controlled trial. BMJ. 2003;327(7413):475–470.
- Binder A. The diagnosis and treatment of nonspecific neck pain and whiplash. Eura Medicophys. 2007;43(1):79–89.
- Coulter ID, Crawford C, Vernon H, et al. Manipulation and mobilization for treating chronic nonspecific neck pain: a systematic review and meta-analysis for an appropriateness panel. Pain Phys. 2019;2(22.2):E55–E70.
- Chow RT, Johnson MI, Lopes-Martins RA, et al. Efficacy of low-level laser therapy in the management of neck pain: a systematic review and meta-analysis of randomised placebo or active-treatment controlled trials. Lancet. 2009;374(9705):1897–1908.
- Côté P, Cassidy DJ, Carroll LJ, et al. The annual incidence and course of neck pain in the general population: a population-based cohort study. Pain. 2004;112(3):267–273.
- Hogg-Johnson S, van der Velde G, Carroll LJ, et al. The burden and determinants of neck pain in the general population. J Manipulative Physiol Ther. 2009;32(2 Suppl):S46–S60.
- Peng B, Yang L, Li Y, et al. Cervical proprioception impairment in neck Pain-Pathophysiology, clinical evaluation, and management: a narrative review. Pain Ther. 2021;10(1):143–164.
- Hidalgo B, Hall T, Bossert J, et al. The efficacy of manual therapy and exercise for treating non-specific neck pain: a systematic review. J Back Musculoskelet Rehabil. 2017;30(6):1149–1169.
- Kazeminasab S, Nejadghaderi SA, Amiri P, et al. Neck pain: global epidemiology, trends and risk factors. BMC Musculoskelet Disord. 2022;23(1):26.
- Hoy D, March L, Woolf A, et al. The global burden of neck pain: estimates from the global burden of disease 2010 study. Ann Rheum Dis. 2014;73(7):1309–1315.
- Barreto TW, Svec JH. Chronic neck pain: nonpharmacologic treatment. Am Fam Physician. 2019;100(3):180–182.
- Childress MA, Stuek SJ. Neck pain: initial evaluation and management. Am Fam Physician. 2020;102(3):150–156.
- Gattie ER, Cleland JA, Snodgrass SJ. Dry needling for patients with neck pain: protocol of a randomized clinical trial. JMIR Res Protoc. 2017;6(11):e227.
- Austin PD, Siddall PJ. Virtual reality for the treatment of neuropathic pain in people with spinal cord injuries: a scoping review. J Spinal Cord Med. 2021;44(1):8–18.
- Chirico A, Lucidi F, De Laurentiis M, et al. Virtual reality in health system: beyond entertainment. A mini-review on the efficacy of VR During cancer treatment. J Cell Physiol. 2016;231(2):275–287.
- Won A, Bailey J, Bailenson J, et al. Immersive virtual reality for pediatric pain. Children. 2017;4(7):52.
- Malloy KM, Milling LS. The effectiveness of virtual reality distraction for pain reduction: a systematic review. Clin Psychol Rev. 2010;30(8):1011–1018.
- Pourmand A, Davis S, Marchak A, et al. Virtual reality as a clinical tool for pain management. Curr Pain Headache Rep. 2018;22(8):53.
- McNevin NH, Shea CH, Wulf G. Increasing the distance of an external focus of attention enhances learning. Psychol Res. 2003;67(1):22–29.
- Zachry T, Wulf G, Mercer J, et al. Increased movement accuracy and reduced EMG activity as the result of adopting an external focus of attention. Brain Res Bull. 2005;67(4):304–309.
- Ahmadpour N, Randall H, Choksi H, et al. Virtual reality interventions for acute and chronic pain management. Int J Biochem Cell Biol. 2019;114:105568.
- Chi B, Chau B, Yeo E, et al. Virtual reality for spinal cord injury-associated neuropathic pain: systematic review. Ann Phys Rehabil Med. 2019;62(1):49–57.
- Collado-Mateo D, Dominguez-Muñoz FJ, Adsuar JC, et al. Effects of exergames on quality of life, pain, and disease effect in women With fibromyalgia: a randomized controlled trial. Arch Phys Med Rehabil. 2017;98(9):1725–1731.
- Sato K, Fukumori S, Matsusaki T, et al. Nonimmersive virtual reality mirror visual feedback therapy and its application for the treatment of complex regional pain syndrome: an Open-Label pilot study. Pain Med. 2010;11(4):622–629.
- Brea-Gómez B, Torres-Sánchez I, Ortiz-Rubio A, et al. Virtual reality in the treatment of adults with chronic low back pain: a systematic review and meta-analysis of randomized clinical trials. Int J Environ Res Public Health. 2021;18(22):11806.
- Mallari B, Spaeth EK, Goh H, et al. Virtual reality as an analgesic for acute and chronic pain in adults: a systematic review and meta-analysis. J Pain Res. 2019;12:2053–2085.
- Bahat HS, Takasaki H, Chen X, et al. Cervical kinematic training with and without interactive VR training for chronic neck pain–a randomized clinical trial. Man Ther. 2015;20(1):68–78.
- Rezaei I, Razeghi M, Ebrahimi S, et al. A novel virtual reality technique (cervigame®) compared to conventional proprioceptive training to treat neck pain: a randomized controlled trial. J Biomed Phys Eng. 2019;9(3):355–366.
- Bahat HS, Croft K, Carter C, et al. Remote kinematic training for patients with chronic neck pain: a randomised controlled trial. Eur Spine J. 2018;27(6):1309–1323.
- Methley AM, Campbell S, Chew-Graham C, et al. PICO, PICOS and SPIDER: a comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Serv Res. 2014;14(1):579.
- Morton NAD. The PEDro scale is a valid measure of the methodological quality of clinical trials: a demographic study. Aust J Physiother. 2009;55:129–134.
- Elkins MR, Herbert RD, Moseley AM, et al. Rating the quality of trials in systematic reviews of physical therapy interventions. Cardiopulm Phys Ther J. 2010;21(3):20–26.
- Guyatt G, Oxman AD, Akl EA, et al. GRADE guidelines: 1. Introduction–GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64(4):383–394.
- Furlan AD, Malmivaara A, Chou R, et al. 2015 Updated method guideline for systematic reviews in the cochrane back and neck group. Spine. 2015;40(21):1660–1673.
- Borenstein M, Hedges L, Higgins J, et al. 2021. Introduction to meta-analysis. Chichester, UK: John Wiley & Sons.
- Elkins MR, Pinto RZ, Verhagen A, et al. Statistical inference through estimation: recommendations from the international society of physiotherapy journal editors. Physiother. 2022;115: A1–A6.
- Beltran-Alacreu H, Navarro-Fernández G, Godia-Lledó D, et al. A serious game for performing task-oriented cervical exercises among older adult patients with chronic neck pain: development, suitability, and crossover pilot study. JMIR Serious Games. 2022;10(1):e31404.
- Bahat HS, German D, Palomo G, et al. Self-Kinematic training for flight-associated neck pain: a randomized controlled trial. Aerosp Med Hum Perform. 2020;91(10):790–797.
- Tejera DM, Beltran-Alacreu H, Cano-De-la-Cuerda R, et al. Effects of virtual reality versus exercise on pain, functional, somatosensory and psychosocial outcomes in patients with non-specific chronic neck pain: a randomized clinical trial. Int J Environ Res Public Health. 2020;17(16):5950.
- Nusser M, Knapp S, Kramer M, et al. Effects of virtual reality-based neck-specific sensorimotor training in patients with chronic neck pain: a randomized controlled pilot trial. J Rehabil Med. 2021;53(2):jrm00151.
- Cetin H, Kose N, Oge HK. Virtual reality and motor control exercises to treat chronic neck pain: a randomized controlled trial. Musculoskelet Sci Pract. 2022;62:102636.
- Liu Q, Wang Y, Tang Q, et al. Do you feel the same as I do? Differences in virtual reality technology experience and acceptance Between elderly adults and college students. Front Psychol. 2020;11:573673 doi: 10.3389/fpsyg.2020.573673.
- Huygelier H, Schraepen B, van Ee R, et al. Acceptance of immersive head-mounted virtual reality in older adults. Sci Rep. 2019;9(1):6.
- Zauderer J, Lefèvre-Colau MM, Davoine É, et al. Exercise therapy program using immersive virtual reality for people with non-specific chronic neck pain: a 3-month retrospective open pilot and feasibility study. Ann Phys Rehabil Med. 2022;65(2):101527.
- Glavare M, Stålnacke B, Häger C, et al. Virtual reality exercises in an interdisciplinary rehabilitation programme for persons with chronic neck pain: a feasibility study. J Rehabil Med-CC. 2021;4(1):jrmcc00067.
- Harvie DS, Smith RT, Moseley GL, et al. Illusion-enhanced virtual reality exercise for neck pain: a replicated single case series. Clin J Pain. 2020;36(2):101–109.
- Lima LV, Abner TSS, Sluka KA. Does exercise increase or decrease pain? Central mechanisms underlying these two phenomena. J Physiol. 2017;595(13):4141–4150.
- Trost Z, Zielke M, Guck A, et al. The promise and challenge of virtual gaming technologies for chronic pain: the case of graded exposure for low back pain. Pain Manag. 2015;5(3):197–206.
- Wang S, Sun J, Yin X, et al. Effect of virtual reality technology as intervention for people with kinesiophobia: a meta‐analysis of randomised controlled trials. J Clin Nurs. 2022;2022:16397 doi: 10.1111/jocn.16397.
- Asiri F, Reddy RS, Tedla JS, et al. Kinesiophobia and its correlations with pain, proprioception, and functional performance among individuals with chronic neck pain. PLoS One. 2021;16(7):e0254262.
- Rudolfsson T, Björklund M, Djupsjöbacka M. Range of motion in the upper and lower cervical spine in people with chronic neck pain. Man Ther. 2012;17(1):53–59.
