Abstract
Objective
To investigate physiotherapists’ views on suitability, usability and factors affecting the use of remote physiotherapy in Finland.
Design
A cross-sectional, web-based questionnaire study.
Subjects
Members of the Finnish Association of Physiotherapists and a private physiotherapy organisation.
Methods
The questionnaire included questions on remote physiotherapy′s suitability (0 = not suitable at all to 10 = fully suitable) for different physiotherapy tasks (consultation, guidance and counselling, exercise, assessment and corrective act at the workplace), a reason to implement remote physiotherapy, how often remote physiotherapy is used at different stages of the physiotherapy process and factors affecting the use of remote physiotherapy.
Results
The response rate was 9.9% (N=662/6525; 76.1% female). The mean suitability ‘score’ for remote physiotherapy differed from 7.6 (consultation, guidance and counselling) to 3.8 (corrective act at a workplace). Physiotherapists with at least one year experience of working with remote physiotherapy reported that it is better suited to consultation, guidance and counselling, exercise and assessment (p-values <.05) than did those with less experience. Of the responders (physiotherapists), 72.5% used conventional physiotherapy, 7.2% used remote physiotherapy and 20.2% used a combination of the two as primary work method.
Conclusion
Physiotherapists stated that remote physiotherapy suits especially for consultation, guidance and counselling, but it is still minimally used as primary work method in different stages of the physiotherapy process.
Introduction
Remote physiotherapy (RP) has been used more frequently in the last few years due to the COVID-19 pandemic, which has forced healthcare organisations to use RP as part of physiotherapists’ daily practices [Citation1–3]. Physiotherapy is a profession with expertise in health, movement, mobility, and function. Physiotherapy’s evidence-based foundation is strong and promotes the development of a scientific approach. Optimal outcomes can be achieved by adopting an evidence-based approach which combines the best available research data with the physiotherapist’s clinical experience and the rehabilitees perceptions [Citation4,Citation5]. For many physiotherapists, the rapid implementation of RP came with limited preparation and a lack of continuing education [Citation6]. RP refers to physiotherapy services delivered to rehabilitees through information and communication technology (ICT), and it can improve the availability of physiotherapy rehabilitation [Citation7–11]. RP allows rehabilitees and physiotherapists to connect with each other from different places and communicate using ICT in real-time, or even not in real-time, with ICT providing feedback and support for rehabilitees [Citation12]. In this article, we use the term RP to describe how conventional physiotherapy is delivered remotely using ICT. The term rehabilitee is defined as a patient, client, customer or group.
There is some evidence that RP might be as effective as and comparable with conventional physiotherapy [Citation13], for example in rehabilitation involving total knee arthroplasty [Citation14], heart diseases [Citation10,Citation15], multiple sclerosis [Citation16] and stroke [Citation17]. RP can offer easier access to therapy for rehabilitees, for example in rural areas where the population density is lower compared to cities, by reducing travel times, waiting times [Citation18] and costs [Citation19]. Other studies have also reported that RP can motivate rehabilitees to become more physically active, but this positive effect does not last over time [Citation10,Citation15].
The promoting factors for the use of RP include the flexible arrangements offered by RP for physiotherapists’ daily practices [Citation20], the easy integration of therapeutic exercise into daily life, flexible exercise hours for rehabilitees [Citation21], the possibility to monitor rehabilitees’ progress [Citation22] and an opportunity to give personal feedback [Citation23]. Despite these advantages, several critical aspects of recent RP or rehabilitation research findings suggest caution to not overestimating the strength of the findings, such as small sample sizes, short follow-up periods [Citation10,Citation17,Citation24,Citation25] and a high degree of heterogeneity in the meta-analysis results of systematic reviews [Citation23].
In prior interview studies, physiotherapists have mentioned certain barriers to the successful use of RP, including communication difficulties when communicating through a screen, a lack of physical contact, such as hands-on methods, the lack of appropriate rehabilitation equipment in rehabilitees’ homes, inadequate resources to resolve technical difficulties [Citation3,Citation18] and rehabilitees’ lack of digital literacy skills [Citation26]. Researchers have also discussed patient safety factors, especially among neurological rehabilitees [Citation27], the need for more individualised, user-friendly approaches [Citation17] and resistance to change with respect to RP [Citation28]. Furthermore, physiotherapist experience of working with RP [Citation29], older age [Citation2] and inadequate guidance and continuing education in RP, both for physiotherapists [Citation2,Citation3,Citation18] and rehabilitees [Citation9], have been seen as barriers.
There is some evidence that RP has been used more frequently in the last few years due to the COVID-19 pandemic [Citation1–3]. However, our knowledge of suitability, usability and factors affecting the use of RP in Finland is limited. The aim of this study was to increase knowledge of physiotherapists’ perceptions and experiences of RP with regard to suitability, implementation, use and promoting and inhibiting factors in Finland. This article is a sub-study of our earlier study of Hellstén et al. [Citation1].
Methods
Study design
In this sub-study, we used a quantitative, cross-sectional, web-based questionnaire. Physiotherapists responded anonymously to the questionnaire. We adhered to the Template for Intervention Description and Replication (TIDieR) checklist and guide [Citation30] and The STROBE Statement [Citation31].
The term remote physiotherapy (RP) was defined in this sub-study as a physiotherapy intervention that includes remote technology, such as telephone, smartphone, computer, tablet, activity trackers, computer vision (CV, camera attached to a computing device to analyse motion), artificial intelligence (AI), virtual reality (VR) or robotics, in a manner in which the physiotherapist is physically in a different place than the rehabilitee [Citation8]. The research ethics committee of the Faculty of Medicine at the University of Helsinki granted ethical approval in February 2021 for the study.
Subjects
A questionnaire was mailed to physiotherapists of working age in the Finnish Association of Physiotherapists (N = 5905) and in one private physiotherapy organisation (N = 620). The physiotherapists were contacted in March 2021 (Finnish Association of Physiotherapists) and May 2021 (private physiotherapy organisation) via an information letter that included an electronic link to the questionnaire. The questionnaire had a five-week deadline, during which time two reminders were sent: the first reminder after one week, and the second two weeks after the first. At the beginning of the COVID-19 pandemic, the Social Insurance Institution of Finland temporarily restricted conventional physiotherapy, and clinics and hospitals were thus required to use RP. Social restrictions in Finland in spring 2021 were mainly set towards adults (>18), there was short regional interruption in hobbies and travelling was not recommended, where as schools and daycares were kept normally open [Citation32].
The questionnaire
A questionnaire was constructed by the research team and co-workers (e.g. medical doctors, physiotherapists, nurses, researchers, lecturers) working either at a university hospital, city health centre, university, university of applied sciences (UAS) or Finnish physiotherapy association. The questionnaire included items based on previous studies in the field of physiotherapy and rehabilitation [Citation11,Citation18,Citation33–35] and the opinions of the research team and co-workers. The questionnaire was piloted by 28 subjects from different physiotherapy fields and geographical locations in Finland. At the pilot stage, we asked participants about any unclear questions and suggestions for corrections. Based on this feedback, two questions were changed from compulsory to optional and minor changes were made to the word choices.
The questionnaire included 32 questions (31 close-ended questions and one open question) divided into nine question groups (background, suitability of RP, education in RP, present state of RP, selection of rehabilitees, suitability of RP in different physiotherapy tasks, facilities and devices for RP, methods and usage of RP, implementation of RP). If the physiotherapist had no experience in RP, the physiotherapist answered the first three questions groups (background, suitability of RP, education in RP). The answers were automatically collected when a physiotherapist had answered all questions in a question group. To answer our research question for the purposes of this sub-study, seven questions were included that addressed the following: the suitability of RP in different physiotherapy work tasks (consultation, guidance and counselling, exercise, assessment and corrective act at workplace), the reasons for implementing RP, the method that physiotherapists primarily put into practice in individual physiotherapy sessions, the three most central factors that promote or inhibit RP, criteria for using RP and amount of education in the field of RP. In our earlier study [Citation1], we used the following five questions: suitability of RP in different diseases and patients with pain, how much of your practice time have you spent on RP in the month before the survey, how much of your practice time have you spent on RP just before the COVID-19 pandemic (early 2020), do you use real-time methods or methods not tied to time in RP, and which of the following technology solutions do you use weekly in RP.
With respect to the question about the suitability of RP in different physiotherapy tasks, we used an eleven-point numeric scale (0 = not suitable at all, 10 = fully suitable) and grouped the questions into five themes (consultation, guidance and counselling, exercise, assessment and corrective act at workplace). The numeric rating scale (NRS) was chosen because it is most commonly used in the field of physiotherapy [Citation36]. The questions pertaining to each theme were selected based on Finnish physiotherapy nomenclatures, which are a number of coded classifications referring to physiotherapeutic services and physiotherapy work [Citation37]. A question about physiotherapeutic consultations was included under the consultation theme, whereas questions about the type of guidance and counselling that promote proper functioning and the type of guidance and counselling that promote the ability to work were included under the guidance and counselling theme. The exercise theme included questions related to physical functioning exercises and movement exercises. The assessment theme included questions about the rehabilitee’s employment and functional assessment, assessment of movement, assessment of pain, assessment of the need for devices and equipment and assessment of the ability to manage in the living environment. Corrective act at workplace theme included questions assessing the rehabilitee’s ability to work.
To study the method physiotherapists primarily put into practice in different stages of the physiotherapy process when conducting individual physiotherapy, the question had three answer alternatives: RP only, conventional physiotherapy only or a combination of the two methods. We followed the process definition of physiotherapy devised by the World Confederation for Physical Therapy [Citation4].
We used three themes, physiotherapist-based, technology-based or management-based factors, to investigate the overall factors that promote or inhibit RP. The physiotherapist-based factor theme included questions about the physiotherapist’s attitude and competence and experience in RP. The technology-based factor theme included questions about the functionality of the hardware and software and internet connection, while the management-based factor theme included questions about education in RP, technical support, facilities for RP and work-time resources. Physiotherapists could choose between nine questions. If a physiotherapist did choose one of the subtheme questions, then the response was included in the findings for the theme in question. We calculated the proportional responses for the various themes based on what each physiotherapist wrote in the questionnaire.
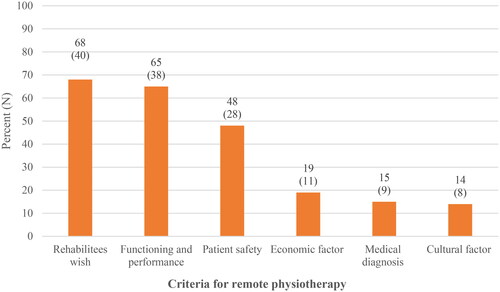
With respect to the criteria for using RP, we grouped the questions into five themes: functioning and performance, cultural factors, rehabilitees’ wishes, economic factors, medical diagnosis and patient safety. The functioning and performance theme included questions about physical functioning and performance, psychic functioning and performance, social functioning and performance, and cognitive functioning and performance. The cultural factors theme included questions about language skills, various cultural factors and the age of the rehabilitee (children, young persons, working-age people, elderly), while the rehabilitees’ wishes theme included questions about the difficulty for the rehabilitee to come to the appointment and rehabilitees’ wishes in general. The economic factors theme included questions about whether or not to intensify physiotherapy by increasing the amount of daily work for the rehabilitee and payer recommendations. Finally, the questionnaire included a question on the rehabilitee’s medical diagnosis and about patient safety. If the physiotherapist did choose one of the subtheme questions, then the response was included in the findings for the theme in question. We calculated the proportional responses to the criteria for using RP based on what each physiotherapist wrote in the questionnaire.
Statistical methods
Statistical analyses were performed using SPSS software (IBM Corp. Released 2020. IBM SPSS Statistics for Windows, Version 27.0. Armonk, NY: IBM Corp). Frequency distributions, percentages and means are given as descriptive statistics, while χ2 statistics and Student’s t-test were applied to calculate statistical differences based on gender, age, experience working with RP and population density (number of people per square kilometre) groups. A two-tailed p-value threshold of less than .05 was considered statistically significant. To analyse factors affecting different reasons to use RP we calculated odds ratios (OR) and their 95% confidence intervals (95% CI) with binary logistic regression analysis.
Results
Six hundred and sixty-two out of 6525 (9.9%) physiotherapists completed the questionnaire. Physiotherapy students, retired physiotherapists, lecturers and researchers were excluded; the final study group included 579/6525 (8.9%) subjects. Of the total, 482 (83.2%) were female (mean age 49.3, SD 11.9 years) and 97 (16.8%) were male (mean age 46.2, SD 12.2 years). Of the physiotherapists, 440/579 (76%) had more than ten years of work experience in physiotherapy. More detailed results about the characteristics of the study participants (physiotherapists) can be found in .
Table 1. Characteristics of the study physiotherapists.
Suitability of RP
The mean suitability ‘score’ for RP in terms of different physiotherapy tasks ranged from 3.8 (corrective act at workplace) to 7.6 (consultation, guidance and counselling). In view of physiotherapists, 24.9% (59/237) gave consultation a full score of ten and 18.5% (44/238) gave guidance and counselling a full score of ten for RP. In contrast, 16.3% (32/196) considered RP not suitable at all (score 0) as a corrective action at work. Physiotherapists with at least one year experience of working with RP reported that RP is better suited to all tasks (all p-values <.05) except as a corrective action at work compared to physiotherapists with less experience in RP. Detailed results are shown in .
Table 2. Suitability score (0 = not suitable at all to 10 = fully suitable) for remote physiotherapy (RP) in different physiotherapy tasks.
Reason to implement RP
One out of every two of the respondents reported that the reason for implementing RP is the ‘wish of the rehabilitee’ or as ‘one alternative among many’. Experience working with RP was associated with the reasons for implementing RP. A larger proportion of physiotherapists with at least one year experience of working with RP noted it as being the “wish of the rehabilitee” than did physiotherapists with less experience in RP (62.8% vs. 39.6%, p=.001). After adjustment for gender, age, and population density, physiotherapists with at least one year experience of working with RP, had a higher tendency to choose “wish of the rehabilitee" compared to others (OR 2.6, 95% CI 1.4 to 4.6, p=.002). Likewise, a higher proportion of physiotherapists with longer experience of working with RP reported “improves accessibility” as a reason for choosing RP compared to their less experienced counterparts (48.1% vs. 33.1%, p=.015). However, after adjustment for gender, age and population density there was no difference between these groups (OR 1.6, 95% CI 0.9 to 2.9, p=.12). More detailed results can be found in .
Table 3. Reason why physiotherapists implement remote physiotherapy (RP) depending on characteristics of physiotherapist or population density.
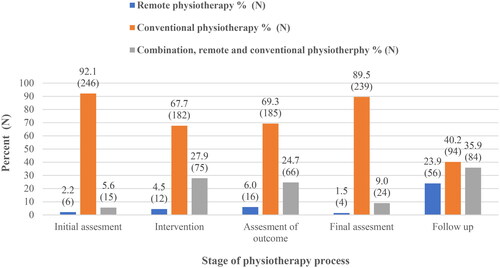
Portion of RP, conventional physiotherapy and a combination of these methods in the physiotherapy process
When studying the methods that physiotherapists primarily put into practice at different stages of the physiotherapy process, they reportedly use conventional (face-to-face) physiotherapy most often at all stages of individual physiotherapy. The proportion of physiotherapists who reported choosing conventional physiotherapy was 72.5%, while the corresponding percentages for those choosing just RP were 7.2% and 20.2% for those choosing a combination of the two methods. Those employing RP as the primary method reportedly use it, especially at follow-up (23.9%, N = 56), but only a few physiotherapists reportedly use RP in other stages of the physiotherapy process. More detailed results are shown in .
Figure 1. Proportion of physiotherapists choosing primarily remote physiotherapy (RP), conventional physiotherapy or a combination of both at different stage of the physiotherapy process.
Promoting and inhibiting factors for RP
In the view of the physiotherapists, technology-related factors (84.5%) best promote the use of RP, with physiotherapist-related factors being at almost the same level (76.5%). Only one out of two of the physiotherapists reported that management-related factors promote the use of RP ().
Table 4. Factors promoting or inhibiting the implementation of remote physiotherapy (RP).
Two-thirds of all physiotherapists reported that technology-related factors inhibit RP. A higher proportion of physiotherapists with less than one year experience of working with RP noted the inhibiting role of technology compared to physiotherapists with more experience (86.6% vs. 70.2%, p=.001). On the other hand, physiotherapists with less than one year of experience working with RP reportedly view management-related factors as more inhibiting than those with more experience (63.0% vs. 45.6%, p=.002). Furthermore, a higher number of males reported that physiotherapist-based factors inhibit the use of RP (77.2% vs. 61.0%, p=.007).
When studying all physiotherapists in relation to the subthemes, the three most common promoting factors mentioned include the functionality of hardware and software (71.0%), a physiotherapist’s positive attitude towards RP (58.0%) and a functioning internet connection for physiotherapists (39.4%). A higher proportion of younger physiotherapists (< 45 years) reported having a more positive attitude towards promoting the use of RP than older (≥ 45 years) ones (65.9% vs. 53.9%, p=.011). Further, physiotherapists with less than one year experience of working with RP highlighted the need for education to promote the use of RP compared to others (22.1% vs. 13.4%, p=.045) ().
With respect to the subthemes, the three most common inhibiting factors mentioned include a lack of functioning hardware and software (56.1%), a negative attitude towards RP (37.6%) and the lack of a working internet connection (34.9%). Physiotherapists with at least one year experience of working with RP more frequently reported a lack of functioning hardware and software (67.8% vs 55.8%, p=.031) and the lack of a working internet connection (53.7% vs. 36.5%, p=.002) as inhibiting factors than did those with less experience in RP. In contrast, physiotherapists with less than one year of work experience more often listed education and competence in relation to RP as inhibiting factors than did physiotherapists with more experience in RP (29.8% vs 11.4%, p=.001, for education and 21.0% vs. 12.1%, p=.039, for competence). More detailed results are shown in .
Only 18.6% (59/318) of physiotherapists reported that their workplace has agreed on pre-criteria for using RP. Of these physiotherapists (N = 59), most (68%, 40/59) reported using it based on a rehabilitee’s wish to do so, while the fewest (14%, 8/59) reportedly use it for cultural reasons. Detailed results are shown in .
Figure 2. Proportion of physiotherapists choosing criteria for remote physiotherapy (RP).
Of the physiotherapists, 62.4% (309/495) reported that they had not participated in RP education in the last year. Overall, more female than male physiotherapists (40.0%, 167/417 vs. 24.3%, 19/78, p=.010) and more physiotherapists with at least one year experience of working with RP compared to less experienced ones (58.0%, 83/143 vs. 43.8%, 78/178, p=.013) had participated in RP education in the last year. Furthermore, only 8.9% (44/495) of the physiotherapists had reportedly taken entry-level courses in RP.
Discussion
Principal findings
This study investigated physiotherapists’ views on suitability and usability and the factors affecting the use of RP in Finland, as the ongoing COVID-19 pandemic has increased the use of RP in everyday practice [Citation1,Citation2]. In Finland, the use of RP is still limited to different stages of the physiotherapy process, with it mostly being used in follow-ups. In the view of the physiotherapists, RP is best suited to physiotherapy-based communication, such as consultation, guidance and counselling, and the main reason for implementing RP is in response to rehabilitees’ wishes. Technology-based factors mostly promote the use of RP, followed by physiotherapist-related factors. At the time of the survey, in the year 2021, continuing education in the field of RP was at a low level in Finland.
Our results show that RP is mostly used for consultation, guidance, counselling and exercise purposes, as also demonstrated in the studies by Rausch et al. [Citation2] and Malliaras et al. [Citation3]. One interesting finding is that physiotherapists with more experience of working with RP feel RP is better suited to different physiotherapy tasks than physiotherapists with less experience in RP. Even if allowing for no statistical differences between the different physiotherapy tasks, the suitability score was systematically higher for those physiotherapists with more experience in RP. This observed finding is in line with evidence presented by Lawford et al. [Citation29], who concluded that experience of working with RP is associated with more convenient use of RP in clinical practice. The finding suggests that physiotherapists in the field of RP learn by doing and that experience in RP may affect their mode of action. Such a response is understandable given the fact that the COVID-19 pandemic led to the rapid implementation of RP and that physiotherapists may have felt challenged in reaching the required standards for conventional physiotherapy with RP. However, the optimal outcome in physiotherapy can be achieved when adopting an evidence-based approach which combines the best available research data with physiotherapists' clinical expertise and rehabilitees perception. Verbal communication as a form of guidance and counselling is a key element in the physiotherapy process [Citation4,Citation5], and, based on our study, it seems that RP is best suited at the moment to these kinds of physiotherapy tasks and should be part of the physiotherapy process. But previous studies have shown that RP can also be used for assessment when observing rehabilitees, e.g. how they balance tasks, their gait, their joint range of motion [Citation3,Citation28], their self-assessed palpation and performance on specialised tests [Citation3], as well as how they respond to validated questionnaires [Citation38].
The most important reasons for implementing RP in the opinion of the physiotherapists was to honour the wish of the rehabilitee, to use it as one alternative physiotherapy method among many and because RP improves accessibility. On the other hand, they did not mention the fact that RP saves social costs, increases equality or deepens therapy relationships as important reasons for using it. Even if prior studies had mentioned that RP can offer easier access to therapy for rehabilitees, for example in rural areas, by reducing travel times and waiting times [Citation18,Citation20,Citation39,Citation40], be a cost-effective means of accessing physiotherapy [Citation41] and that RP deepens the relationship between the physiotherapist and rehabilitee [Citation42], our study did not yield such findings. It may be that the physiotherapists in our study felt they had been forced to implement RP in everyday practice during the COVID-19 pandemic and that they had done so for practical reasons in these kinds of circumstances, only being able to offer physiotherapy to those rehabilitees who needed it and were unable or unwilling to visit a hospital or clinic. However, it is important for physiotherapists to recognise that rehabilitees who are not interested in or who are unfamiliar with RP may need more conventional physiotherapy than enthusiastic rehabilitees [Citation9].
Physiotherapy has traditionally been a hands-on profession with strong manual and face-to-face interactions between the rehabilitee and physiotherapist. Overall knowledge, on the suitability of RP at different stages of the physiotherapy process is still limited. In our study, conventional physiotherapy is mostly used in all stages of the physiotherapy process and especially in the initial and final assessment of rehabilitees. RP is typically used in follow-ups, whereas physiotherapists rarely use it in other stages of the physiotherapy process. It seems that physiotherapists prefer to meet rehabilitees face to face at clinics or in hospitals at some stage of the physiotherapy process. However, RP can be seen these days as a necessary part of the physiotherapist’s professional role, depending on a physiotherapist’s willingness [Citation5] and confidence in implementing RP in the physiotherapy process [Citation3,Citation18], though most physiotherapists feel that RP cannot be used as a replacement for contact between the rehabilitee and physiotherapist [Citation2,Citation15]. RP is mostly used in physiotherapy when, e.g. rehabilitees perform exercises [Citation18] and in follow-ups [Citation43], a finding highlighted in other studies as well.
RP requires new skills and a new mindset from both physiotherapists and rehabilitees for it to be successful, but it also requires technical equipment that is easy to use and that works well. In our study, technology-related factors were the factors that most promoted the use of RP, followed by physiotherapist-related factors and management-related factors. Even though younger people are usually more familiar with using technical equipment, a higher proportion of younger physiotherapists with less experience in our study felt less positive about using RP compared to older ones. On the other hand, experience working with RP was not seen as an important factor in promoting the use of RP. Factors identified in other studies as promoting the use of RP include the increasing flexibility of physiotherapists in their daily practice [Citation20] and new professional skills [Citation18]. Also, the possibility to follow up on rehabilitees’ progress [Citation22], the opportunity to give individual feedback [Citation23], integrating guidance, counselling and therapeutic exercises into daily life, and providing flexible exercise hours for rehabilitees [Citation21] have been discussed. Promoting and inhibiting factors have been studied in qualitative studies and discussed in the existing literature. We used a quantitative, cross-sectional, web-based questionnaire to study these factors, and our study, therefore, offers important new knowledge about RP in Finland that can, with a certain amount of caution, be generalised.
There are several barriers preventing the widespread use of RP. Our study reveals that technology-based factors strongly inhibit the use of RP, especially among physiotherapists with less experience working with RP. Similarly, Damhus et al. [Citation18] concluded in their study that a lack of technical support and physiotherapists’ concern about fixing technical issues are also barriers. Technical issues commonly occur when using digital devices, and such barriers should be resolved before implementing RP. Other barriers include the physiotherapist’s competence in using technical equipment, resistance to RP, the cost of investing in technical equipment [Citation44], a lack of environmental space to implement RP and infrastructural challenges, such as bandwidth capacity [Citation45]. Furthermore, some physiotherapists have suggested that limited physical contact with the rehabilitee hinders clinical reasoning [Citation3]. The physiotherapists taking part in our study also mentioned each of these barriers except for investment cost and clinical reasoning. One interesting finding in our study was that the same factors both promote and inhibit the use of RP. Therefore, we can conclude that technology-based, physiotherapist-based and management-based factors are all essential in order to successfully implement RP. Overall, knowledge about promoting and inhibiting factors in RP is still limited, and more high-quality studies on these factors are essential.
We also noted a lack of education in the field of RP in our study, similar to Jonas et al. [Citation46], even though RP was first introduced in the late 1990s [Citation7]. The COVID-19 pandemic increased the use of RP [Citation1,Citation2], and therefore, to better meet the standard of conventional physiotherapy in RP, a framework for how physiotherapists can successfully deliver quality RP has been developed [Citation6]. Based on the results, in Finland, the use of RP is mostly based on learning by doing, however, RP should follow an evidence-based approach, which combines the best available research data with physiotherapists' clinical experience and rehabilitation perception [Citation4,Citation5]. It is important for physiotherapists to recognise their own competence and its limits when seeking to successfully implement RP in daily practice. In addition, this study brings out the absence of evidence-based reasons to use RP. For example, only two out of ten physiotherapists reported that their workplace has agreed on pre-criteria for using RP, which might be one way to increase the use of evidence-based RP in clinical settings. In future, more attention should be paid to increasing the use of evidence-based activities of RP in clinical settings, but also increasing research work in implementation studies on this issue.
Strengths and limitations
A strength of this study is the number of physiotherapists (N = 662) who answered the survey, even if only a total of 9.9% (662/6525) answered. The physiotherapists were recruited from all municipalities in Finland and included physiotherapists with limited and extensive clinical experience. The study findings can somehow be generalised to the broader Finnish physiotherapy workforce, where 80% of employed physiotherapists are female and the mean age is 44 years. Our study also has some limitations. We collected the survey data in Finland, and our findings may not be generalisable to other countries, where physiotherapists may have more experience in RP. One limitation of our study may be non-participation bias. We recruited the participating physiotherapists from the Finnish Association of Physiotherapists and from a private physiotherapy organisation, but we had to collect the data anonymously. Therefore, it was not possible to analyse whether the respondents differ significantly from non-responders and whether these possible differences may have influenced the results of the study. In our study, the physiotherapist that answered the whole questionnaire (experience of working with RP) were on average slightly younger than those who only answered the first three questions groups (background, suitability of RP, education in RP). This finding is in line with Rausch et al. [Citation2], but further complicates the generalisation of the results.
Further, some of the physiotherapists from the private physiotherapy organisation were also members of the Finnish Association of Physiotherapists and had the possibility to respond twice to the questionnaire. To avoid such an overlap, we recommended in the information letter not to respond twice. The use of a scientifically unvalidated questionnaire, that physiotherapists were not forced to answer the whole questionnaire, that answers were automatically collected when a physiotherapist had answered all questions in a question group and that we had physiotherapists with and without experience working with RP included can be seen as a limitation. Lastly, a limitation may be that we did not use a theoretical model when developing the questionnaire, and used a web-based questionnaire, which often has a low response rate [Citation47]. However, the questionnaire included the main domains in the NASSS (non-adoption, abandonment, scale-up, spread, sustainability) framework [Citation48], the consensus in a broad expert group and essential literature in the field, and it was first piloted and tested. Despite these limitations, our results highlight important new information about RP, which is important in the development of professional competence but also in terms of education and management.
Conclusion
In conclusion, the suitability of RP for different physiotherapy work tasks varies. In the view of the participating physiotherapists, RP is best suited for physiotherapy-based communication as a form of consultation, guidance and counselling. While the physiotherapists reported using conventional physiotherapy most often at all stages in the physiotherapy process, they use RP most often in follow-up, otherwise, their reported use of RP is minimal. Technology-related factors mostly promote the use of RP in a physiotherapist’s daily practices. Education in the field of RP is at a low level, and physiotherapists reportedly only use RP pre-criteria infrequently. These results may help physiotherapists and organisations in implementing RP in everyday practice. RP should be implemented in areas where the benefit has been shown.
Authors contributions
TH, JA and JK helped design the research. All authors were involved in compiling the questionnaire and in editing, reviewing and approving the final manuscript.
Acknowledgments
The authors wish to thank Erik Hieta for the language editing of this article.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Data not available - participant consent.
Additional information
Funding
References
- Hellstén T, Arokoski J, Sjögren T, et al. The current state of remote physiotherapy in Finland: cross-sectional web-based questionnaire study. JMIR Rehabil Assist Technol. 2022;9(2):e35569. doi: 10.2196/35569.
- Rausch A-K, Baur H, Reicherzer L, et al. Physiotherapists’ use and perceptions of digital remote physiotherapy during COVID-19 lockdown in Switzerland: an online cross-sectional survey. Arch Physiother. 2021;11(1):18. doi: 10.1186/s40945-021-00112-3.
- Malliaras P, Merolli M, Williams C, et al. ‘It’s not hands-on therapy, so it’s very limited’: telehealth use and views among allied health clinicians during the coronavirus pandemic. Musculoskelet Sci Pract. 2021;52:102340. doi: 10.1016/j.msksp.2021.102340.
- The World Confederation for Physical Therapy (WCPT): Description of physical therapy Policy statement. 2019. [cited 2022 Oct 10]. Available from: https://world.physio/sites/default/files/2020-07/PS-2019-Description-of-physical-therapy.pdf.
- Finnish Association of Physiotherapists: The corecompetences of a physiotherapist. 2016 cited. 2022 Sept 19] Available from: https://www.suomenfysioterapeutit.fi/wp-content/uploads/2018/04/CoreCompetencies.pdf.
- Davies L, Hinman RS, Russell T, et al. An international core capability framework for physiotherapists to deliver quality care via videoconferencing: a Delphi study. J Physiother. 2021;67(4):291–297. doi: 10.1016/j.jphys.2021.09.001.
- Burns RB, Crislip D, Daviou P, et al. Using telerehabilitation to support assistive technology. Assist Technol. 1998;10(2):126–133. doi: 10.1080/10400435.1998.10131970.
- Salminen AL, Hiekkala S, Stenberg JH. Etäkuntoutus. Tampere: Juvenes Print; 2016, p. 11–12. ISBN 978-952-284-005-9
- Anttila M-R, Kivistö H, Piirainen A, et al. Cardiac rehabilitees’ technology experiences Before remote rehabilitation: qualitative study using a grounded theory approach. J Med Internet Res. 2019;21(2):e10985. doi: 10.2196/10985.
- Hakala S, Kivistö H, Paajanen T, et al. Effectiveness of distance technology in promoting physical activity in cardiovascular disease rehabilitation: cluster randomized controlled trial, a pilot study. JMIR Rehabil Assist Technol. 2021;8(2):e20299. doi: 10.2196/20299.
- Hakala S, Rintala A, Immonen J, et al. Effectiveness of physical activity promoting technology-based distance interventions compared to usual care. Systematic review, meta-analysis and meta-regression. Eur J Phys Rehabil Med. 2017;53(6):953–967. doi: 10.23736/s1973-9087.17.04585-3.
- Werneke MW, Deutscher D, Grigsby D, et al. Telerehabilitation During the COVID-19 pandemic in outpatient rehabilitation settings: a descriptive study. Phys Ther. 2021;101(7):1–11. doi: 10.1093/ptj/pzab110.
- Hawley-Hague H, Lasrado R, Martinez E, et al. A scoping review of the feasibility, acceptability, and effects of physiotherapy delivered remotely. Disability and Rehabilitation. 2022;2:1–17. doi: 10.1080/09638288.2022.2138574.
- Moffet H, Tousignant M, Nadeau S, et al. In-home telerehabilitation compared with face-to-face rehabilitation after total knee arthroplasty: a noninferiority randomized controlled trial. J Bone Joint Surg Am. 2015;97(14):1129–1141. doi: 10.2106/JBJS.N.01066.
- Spindler H, Leerskov K, Joensson K, et al. Conventional rehabilitation therapy Versus telerehabilitation in cardiac patients: a comparison of motivation, psychological distress, and quality of life. IJERPH. 2019;16(3):512. doi: 10.3390/ijerph16030512.
- Turner AP, Hartoonian N, Sloan AP, et al. Improving fatigue and depression in individuals with multiple sclerosis using telephone-administered physical activity counseling. J Consult Clin Psychol. 2016;84(4):297–309. doi: 10.1037/ccp0000086.
- Rintala A, Paivarinne V, Hakala S, et al. Effectiveness of technology-based distance physical rehabilitation interventions for improving physical functioning in stroke: a systematic review and meta-analysis of randomized controlled trials. Arch Phys Med Rehabil. 2019;100(7):1339–1358. doi: 10.1016/j.apmr.2018.11.007.
- Damhus CS, Emme C, Hansen H. Barriers and enablers of COPD telerehabilitation – a frontline staff perspective. Int J Chron Obstruct Pulmon Dis. 2018;13:2473–2482. doi: 10.2147/COPD.S167501.
- Cottrell M, Judd P, Comans T, et al. Comparing fly-in fly-out and telehealth models for delivering advanced-practice physiotherapy services in regional Queensland: an audit of outcomes and costs. J Telemed Telecare. 2021;27(1):32–38. doi: 10.1177/1357633X19858036.
- Turolla A, Rossettini G, Viceconti A, et al. Musculoskeletal physical therapy during the COVID-19 pandemic: is telerehabilitation the answer? Phys Ther. 2020;100(8):1260–1264. doi: 10.1093/ptj/pzaa093.
- Cranen K, Groothuis-Oudshoorn CGM, Vollenbroek-Hutten MMR, et al. Toward patient-centered telerehabilitation design: understanding chronic pain patients’ preferences for web-based exercise telerehabilitation using a discrete choice experiment. J Med Internet Res. 2017;19(1):e26. doi: 10.2196/jmir.5951.
- Galea MD. Telemedicine in rehabilitation. Phys Med Rehabil Clin N Am. 2019;30(2):473–483. doi: 10.1016/j.pmr.2018.12.002.
- Lahtio H, Rintala A, Immonen J, et al. The effectiveness of physical activity-promoting web- and mobile-based distance weight loss interventions on body composition in rehabilitation settings: systematic review, meta-analysis, and meta-regression analysis. J Med Internet Res. 2022;24(3):e25906. doi: 10.2196/25906.
- Sakai T, Hoshino C, Yamaguchi R, et al. Remote rehabilitation for patients with COVID-19. J Rehabil Med. 2020;52(9):0. doi: 10.2340/16501977-2731.
- Marwaa MN, Guidetti S, Ytterberg C, et al. The use of mobile and web-based applications to support rehabilitation after stroke: a scoping review. JRM. 2022;54:jrm00269. doi: 10.2340/jrm.v54.452.
- Levine M, Richardson JE, Granieri E, et al. Novel telemedicine technologies in geriatric chronic non-cancer pain: primary care providers’ perspectives. Pain Med. 2014;15(2):206–213. doi: 10.1111/pme.12323.
- Kim H, Choi W, Lee K, et al. Virtual dual-task treadmill training using video recording for gait of chronic stroke survivors: a randomized controlled trial. J Phys Ther Sci. 2015;27(12):3693–3697. doi: 10.1589/jpts.27.3693.
- Cottrell MA, Russell TG. Telehealth for musculoskeletal physiotherapy. Musculoskelet Sci Pract. 2020;48:102193. doi: 10.1016/j.msksp.2020.102193.
- Lawford BJ, Bennell KL, Kasza J, et al. Physical therapists’ perceptions of telephone‐ and internet video–mediated service models for exercise management of people With osteoarthritis. Arthritis Care Res (Hoboken). 2018;70(3):398–408. doi: 10.1002/acr.23260.
- Hoffmann TC, Glasziou PP, Boutron I, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ. 2014;348:g1687. doi: 10.1136/bmj.g1687.
- von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–349. doi: 10.1016/j.jclinepi.2007.11.008.
- Kuitunen I, Artama M, Haapanen M, et al. Respiratory virus circulation in children after relaxation of COVID-19 restrictions in fall 2021 – a nationwide register study in Finland. J Med Virol. 2022;94(9):4528–4532. doi: 10.1002/jmv.27857.
- Sjögren T, von Hedenberg L, Parikka E, et al. The core competences of Finnish physiotherapists in the light of research data. Physiotherapy. 2016;102:e28–e29. doi: 10.1016/j.physio.2016.10.040.
- Caughlin S, Mehta S, Corriveau H, et al. Implementing telerehabilitation after stroke: lessons learned from Canadian trials. Telemed J E Health. 2020;26(6):710–719. doi: 10.1089/tmj.2019.0097.
- Salminen AL, Hiekkala S. Kokemuksia etäkuntoutuksesta. Kelan etäkuntoutushankkeen tuloksia. Helsinki: Erweko; 2019, p. 206–227. ISBN 978-952-284-066-0
- Hartrick CT, Kovan JP, Shapiro S. The numeric rating scale for clinical pain measurement: a ratio measure? Pain Pract. 2003;3(4):310–316. doi: 10.1111/j.1530-7085.2003.03034.x.
- Savolainen T, Partia R. Fysioterapianimikkeistö. Helsinki: Suomen Kuntaliitto; 2018. ISBN 978-952-293-579-3
- Truter P, Russell T, Fary R. The validity of physical therapy assessment of low back pain via telerehabilitation in a clinical setting. Telemed J E Health. 2014;20(2):161–167. doi: 10.1089/tmj.2013.0088.
- Odole AC, Afolabi KO, Ushie BA, et al. Views of physiotherapists from a low resource setting about physiotherapy at a distance: a qualitative study. Eur J Physiother. 2020;22(1):14–19. doi: 10.1080/21679169.2018.1549272.
- The Chartered Society of Physiotheraphy. Understanding the opportunities and challenges of remote physiotherapy consultations and rehabilitation during the Covid-19 pandemic; 2021. [cited. 2023 Apr 24] Available from: https://www.csp.org.uk/system/files/documents/2022-2/csp_remote_pt_evaluation_final_report.pdf.
- Cottrell MA, Hill AJ, O'Leary SP, et al. Clinicians’ perspectives of a novel home-based multidisciplinary telehealth service for patients with chronic spinal pain. Int J Telerehabil. 2018;10(2):81–88. doi: 10.5195/ijt.2018.6249.
- Pastora-Bernal JM, Martín-Valero R, Barón-López FJ, et al. Evidence of benefit of telerehabitation after orthopedic surgery: a systematic review. J Med Internet Res. 2017;19(4):e6836. doi: 10.2196/jmir.6836.
- Polastri M, Ciasca A, Nava S, et al. Two years of COVID-19: trends in rehabilitation. Pulmonology. 2022;20:1–3. doi: 10.1016/j.pulmoe.2022.01.012.
- Scott Kruse C, Karem P, Shifflett K, et al. Evaluating barriers to adopting telemedicine worldwide: a systematic review. J Telemed Telecare. 2018;24(1):4–12. doi: 10.1177/1357633X16674087.
- Hale-Gallardo JL, Kreider CM, Jia H, et al. Telerehabilitation for rural veterans: a qualitative assessment of barriers and facilitators to implementation. J Multidiscip Healthc. 2020;13:559–570. doi: 10.2147/JMDH.S247267.
- Jonas CE, Durning SJ, Zebrowski C, et al. An interdisciplinary, multi-institution telehealth course for third-year medical students. Acad Med. 2019;94(6):833–837. doi: 10.1097/ACM.0000000000002701.
- Eysenbach G improving the quality of web surveys: the checklist for reporting results of internet E-surveys (CHERRIES). J Med Internet Res. 2004;6(3):e34. doi: 10.2196/jmir.6.3.e34.
- Greenhalgh T, Wherton J, Papoutsi C, et al. Beyond adoption: a new framework for theorizing and evaluating nonadoption, abandonment, and challenges to the scale-up, spread, and sustainability of health and care technologies. J Med Internet Res. 2017;19(11):e8775. doi: 10.2196/jmir.8775.
