Abstract
Objective
Parastomal hernia (PH) in association with an ileal conduit is a common complication that is difficult to treat. Mesh reinforcement has been suggested to improve outcomes; either as prophylaxis or for treatment of a parastomal hernia during abdominal wall reconstruction.
Patients and methods
A retrospective study was performed in consecutive patients subjected to mesh implantation between 2000 and 2016 having a concurrent or previous ileal conduit reconstruction. Postoperative and late urostomal complications, as well as hernia occurrence, were ascertained by a chart review of patients’ records.
Results
A total of 25 patients were included of whom 13 (52%) developed either a urostomal complication, a PH, or both. Complications were caused by mesh erosion in four patients, of which three were diagnosed more than five years after surgery. Four patients developed a urostomal stenosis. One out of eight patients with urostomal complications were subjected to a new ileal conduit reconstruction and another four to other types of revisional surgery.
Conclusions
Every second patient with an ileal conduit developed either a local urostomal complication, a PH, or both after abdominal wall mesh reconstruction. A careful and cautious attitude towards the use of mesh in patients with an ileal conduit is suggested.
Introduction
An ileal conduit is the most common type of urinary diversion fashioned in conjunction with radical cystectomy (RC). The surgery is either carried out with robotic-assisted laparoscopy or through a lower midline incision. Similarly, during pelvic exenteration surgery, an ileal conduit is constructed in addition to an ostomy for the bowel diversion, the latter most commonly as an end sigmoidostomy. The cystectomy itself is associated with abdominal wall-related complications such as incisional hernias in up to 20% of the patients at follow-up [Citation1,Citation2]. In addition, stoma-related complications such as protrusion of abdominal content through a local defect in the abdominal wall at the site of the ileal conduit can occur, i.e. a parastomal hernia (PH) [Citation3]. A PH does frequently cause an ill-fitting ostomy bandage, bowel and/or urinary obstruction, as well as considerable discomfort [Citation4]. Similarly, after colorectal surgery, PHs frequently occur and many patients have some type of symptoms due to their PH [Citation5]. Stoma site fascial incisions of >35mm, age >70 years, BMI >25, diabetes, and increased abdominal pressure are risk factors associated with the development of a PH [Citation6].
It has recently been demonstrated that the use of prophylactic lightweight mesh in the sublay position can reduce the cumulative incidence PH from 23% to 11% after open cystectomy with ileal conduit formation within two years of surgery [Citation7]. Both prevention and surgery for abdominal wall hernias are routinely performed using mesh implantation. This could potentially cause complications such as stomal obstruction and/or mesh erosion. Two studies reported a low risk of such mesh-related complications when a prophylactic mesh was used [Citation7,Citation8]. However, long-term ileal conduit complications related to repair of abdominal wall hernias and/or abdominal wall reconstructions using mesh implantation in association with ileal conduits are currently lacking. Furthermore, a recent randomized multicenter trial did not report any reduced risk of PH when applying a prophylactic mesh during colorectal surgery [Citation9], which together with the absence of long-term data on mesh-related complications from previously published similar randomized trials is the rationale for the current study.
The aim was to retrospectively review the panorama of complications that can occur in conjunction with mesh implantation in patients having an ileal conduit construction with simultaneous abdominal wall reconstruction or in patients already having an ileal conduit being subjected to abdominal wall hernia/parastomal hernia repair.
Patients and methods
Data collection
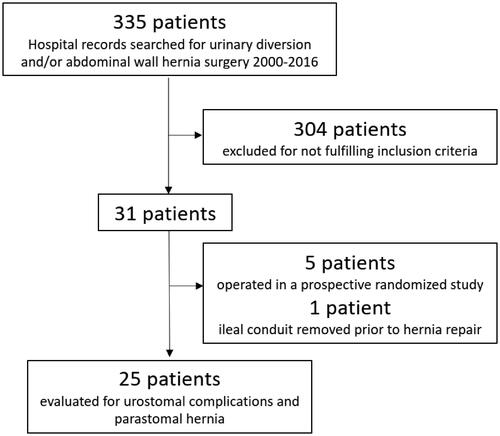
A retrospective chart review was performed on patients at Skåne University Hospital (SUS), a tertiary referral center for both radical cystectomy and abdominal wall hernia repair. Patients that had undergone abdominal wall reconstruction (PH and/or incisional hernia) with the additional criteria of previous or concurrent urinary diversion surgery between 2000 and 2016 (n = 335) were identified. To comply with study inclusion, abdominal wall mesh implantation around the conduit was placed either in conjunction with the reconstruction of an ileal conduit or at a later occasion for the treatment of a PH and/or incisional hernia. Files were reviewed, both from local hospital records and tertiary referral units, respectively. After excluding duplicates, 31 patients met the defined search criteria. Exclusions were five patients taking part in an ongoing randomized study using mesh as a prophylactic measure to decrease the risk of PH and thus not receiving the mesh during bladder wall reconstruction or surgical correction of PH and/or incisional hernia [Citation7]. An additional patient having had the ileal conduit removed before the hernia repair was also excluded. A total of 25 patients were eligible for inclusion ().
Patient characteristics, potential risk factors for complications (gender, BMI, diabetes, American Society of Anesthesiologists (ASA) score, smoking status), and indications for surgery were ascertained from a review of patient’s charts. Type of mesh and surgical technique for mesh implantation was registered. Postoperative complications within 90 days after surgery were categorized according to Clavien-Dindo [Citation10]. All surgeries were classified as clean-contaminated according to CDC (Centers for Disease Control and Prevention) wound classification [Citation11]. Information on symptoms and findings that could indicate urostomal dysfunction and complications such as stenosis, calcifications in the ileal conduit, erosion of mesh and/or pain were identified. Hernia recurrences were identified either from patient charts or from CT scans performed during follow-up (FoU).
Follow-up
Patient records were reviewed for the date of mesh implantation as starting point until June 2020. Late complications were defined as any dysfunction of the urostomy related to the mesh and/or a hernia occurrence. The last date for FoU was defined as either a physical visit or telephone contact in the surgical or urological department at either the local hospital or at the referral center.
Statistics and ethics
Descriptive statistics were used. The study was approved by the Research Ethics Board of Lund University (2014/831).
Results
A total of 25 patients (10 females and 15 males) were identified as having received both an ileal conduit in combination with an abdominal wall mesh implantation. The median follow-up was 72 months (interquartile range (IQR) 29–92) after mesh implantation. Patient characteristics are given in . The majority of patients (22/25) underwent radical cystectomy (RC) due to urological, gynecological, or colorectal malignancies. Three patients underwent RC and received an ileal conduit due to a benign urological condition. Indications and surgical characteristics are given in . Eleven patients (44%) received a prophylactic mesh in conjunction with the abdominal wall reconstruction using a vertical rectus abdominis myocutaneous flap (VRAM), 13 patients (52%) underwent a hernia mesh repair and the remaining one patient (4%) received a mesh in association with reoperation for wound dehiscence after RC.
Table 1. Patient characteristics stratified for urostomal complications and/or parastomal hernia (PH) during follow-up.
Table 2. Indications for radical cystectomy (RC), type of surgery, and Clavien-Dindo within 90 days of surgery stratified by no urostomal and urostomal complication.
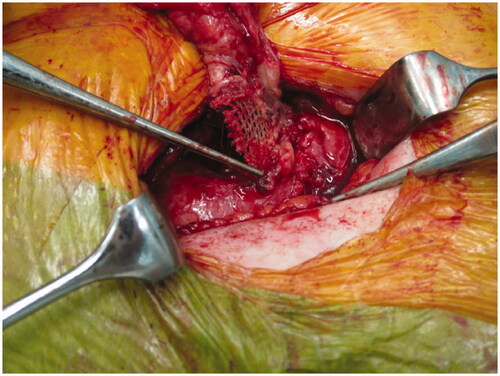
Late urostomal complications and/or occurrence of a PH were noted in 13/25 (52%) patients (). Eight patients had urostomal complications and five developed a PH. Among the patients with urostomal complications, 3/8 also developed a PH, hence in all 8/25 (32%) patients developed PHs. In total, 7/13 patients underwent a reoperation either due to urostomal complications or recurrent PH and two patients had to undergo one or two additional surgical interventions, respectively. In addition, one patient (Male, 31 in ) is awaiting surgery for his PH. Four out of the eight patients with urostomal complications developed a mesh erosion into the conduit () (Male, 43 in ), and three of these underwent open surgical revision. The other four patients with a urostomal complication developed a urostomal stenosis at the level of the mesh, and one of these had to undergo surgery with reconstruction of a new ileal conduit. In total, 5/8 patients with urostomal complications required surgical interventions, another two patients were treated with the chronic catheter in the conduit due to comorbidity, and one patient did not require any further invasive treatments. Urostomal complications occurred after hernia repair in 9/13 patients, compared to 3/11 among those receiving a prophylactic mesh.
Table 3. Thirteen patients developed urostomal complications and/or parastomal hernia (PH) during follow-up.
Mesh location varied. In 15 patients the ileal conduit was brought out through a flat mesh, and in one patient a mesh collar (‘chimney mesh’) was constructed. In another six patients, a midline retro muscular mesh reinforcement was performed, and in two patients an intraabdominal mesh was placed using the Sugarbaker technique [Citation11]. Information on mesh location was missing in one patient.
The type of mesh used during surgery also varied. The most common mesh type was DynaMesh Cicat® (FEG Textiltechnik, Aachen, Germany) (12 patients). Six out of these developed a complication and/or parastomal hernia (PH). Among the remaining patients, three received a Parietene® mesh, two a Prolene® mesh, and the remaining four patients received either a Physiomesh®, Vypro®, Proceed®, or a Premiliene® mesh. Information on mesh type was missing in four patients. Nine patients had persistent symptoms related to their urostomal complication and/or PH. In three patients persistent symptoms were present despite surgical interventions were undertaken ().
Discussion
Every second patient subjected to abdominal wall reconstruction or abdominal wall hernia repair with a mesh in conjunction with an ileal conduit developed either mesh-related urostomal complications and/or a PH during long-term follow-up. Three out of four mesh erosions occurred five years or later after mesh implantation. Nine out of 13 patients developing urostomal complications or PH suffered from persisting sequelae related to their mesh complication or a PH despite having revisional surgery was performed.
The absence of mesh-related complications was demonstrated in a randomized trial comparing stoma construction using a prophylactic flat Vypro® mesh to no mesh in conjunction with ileal conduit construction [Citation7]. Similarly, the absence of mesh-related complications and erosions were reported in a retrospective observational study [Citation8]. The use of prophylactic mesh in gastrointestinal ostomy construction is also considered safe with few long-term mesh-related complications [Citation12–15]. Considering that 9/13 of the urostomal complications in the present study occurred after hernia repair compared to 3/11 after prophylactic mesh application, suggests that the risk of urostomal complications was high, even if lower when a mesh was used as prophylaxis. It might be that the intestinal wall in an ileal conduit, exposed to urine for some time, is more fragile compared to the intestinal segment used for permanent gastrointestinal ostomies.
The low number of patients in the current study precludes any associations between preoperative factors or the type of mesh used at the surgery. However, the observation that six out of the 12 patients that received a DynaMesh® had a urostomal complication and/or a PH calls for reflection. It is unknown to what extent a sharp edge from a mesh might contribute to mesh erosion into an ileal conduit. In the current study, one patient received a mesh collar (‘chimney mesh’) to avoid such sharp edges in the proximity of the conduit. This concept of a mesh chimney is currently evaluated in gastrointestinal surgery in a randomized setting [Citation16], but the impact on urinary flow in a conduit when using a ‘chimney mesh’ construction has not been investigated so far. In theory, any obstruction of the urinary flow in a patient with an ileal conduit might increase the risk of urinary tract infections, which is the most frequent cause of hospitalization after cystectomy and ileal conduit [Citation17]. The 73-year-old female () is an example of how such obstruction could contribute to recurrent urinary tract sepsis episodes. Additionally, stenosis might have contributed to persisting symptoms with pain and urinary obstruction in another three patients suffering from persistent symptoms for their urostomal complication ().
Other methods to apply a mesh during PH repair have been described in combination with primary suturing using a shoelace technique, i.e. the Sugarbaker procedure [Citation18], or by the use of a biologic mesh [Citation19]. Also, a local PH repair using a mesh without a midline incision has been reported in 19 patients by transposing the conduit 5–10 centimeters superiorly, albeit with a 21% recurrence rate [Citation20].
The deferred use of a mesh when a PH occurs, instead of applying a prophylactic mesh at primary surgery, implies a non-negligible risk of urostomal complications according to our findings. Given the frequent occurrence of PH after RC and ileal conduit construction ranging from 17% to 68% [Citation3, Citation21,Citation22], the optimal strategy whether to use a prophylactic mesh in all patients subjected to ileal conduit diversion or in selected patients only, is to be defined. Recently, an alternative stoma construction method both for end colostomies and ileal conduits has been reported to decrease the risk of PH [Citation23]. Bypassing the intestine under the rectus abdominis muscle and passing the emerging bowel and stoma lateral to the rectus muscle, PHs were seldomly seen in this retrospective case series.
The current study is limited by its retrospective design, its limited cohort size, and the heterogenous indications for abdominal wall reconstruction or repair of PH and/or incisional hernia. Furthermore, considering the variety of mesh types used it is not possible to draw any conclusions on possible associations between type of mesh or type repair and risk of urostomal complications. Nonetheless, also few observations of serious events can be important to highlight in rare clinical settings.
Conclusions
The current study calls for a cautious attitude when using mesh about an ileal conduit. Mesh erosions seem to occur also several years after surgery. Especially, sharp mesh edges in the proximity of an ileal conduit might be related to a risk of urostomal complications.
Acknowledgments
Gösta Jönsson Research Foundation, The Foundation of Urological Research (Ove and Carin Carlsson bladder cancer donation) and Hillevi Fries Research Foundation. The funding sources had no role in the study design, data analyses, interpretation, or writing the manuscript.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- van 't Riet M, Steyerberg EW, Nellensteyn J, et al. Meta-analysis of techniques for closure of midline abdominal incisions. Br J Surg. 2002;89(11):1350–1356.
- Movassaghi K, Shah SH, Cai J, et al. Incisional and parastomal hernia following radical cystectomy and urinary diversion: the university of Southern California experience. J Urol. 2016;196(3):777–781.
- Narang SK, Alam NN, Campain NJ, et al. Parastomal hernia following cystectomy and ileal conduit urinary diversion: a systematic review. Hernia. 2017;21(2):163–175.
- Harraz AM, Elkarta A, Zahran MH, et al. Parastomal hernia after ileal conduit urinary diversion: re-visiting the predictors radiologically and according to patient-reported outcome measures. Scand J Urol. 2020;54(6):501–507.
- Hotouras A, Murphy J, Thaha M, et al. The persistent challenge of parastomal herniation: a review of the literature and future developments. Colorectal Dis. 2013;15(5):e202–14.
- Pilgrim CH, McIntyre R, Bailey M. Prospective audit of parastomal hernia: prevalence and associated comorbidities. Dis Colon Rectum. 2010;53(1):71–76.
- Liedberg F, Kollberg P, Allerbo M, et al. Preventing parastomal hernia after ileal conduit by the use of a prophylactic mesh: a randomised study. Eur Urol. 2020;78(5):757–763.
- Styrke J, Johansson M, Granåsen G, et al. Parastomal hernia after ileal conduit with a prophylactic mesh: a 10 year consecutive case series. Scand J Urol. 2015;49(4):308–312.
- Odensten C, Strigård K, Rutegård J, et al. Use of prophylactic mesh when creating a colostomy does not prevent parastomal hernia: a randomized controlled Trial-STOMAMESH. Ann Surg. 2019;269(3):427–431.
- Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Annals of Surgery. 2004;240(2):205–213.
- Horan TC, Gaynes RP, Martone WJ, et al. CDC definitions of nosocomial surgical site infections, 1992: a modification of CDC definitions of surgical wound infections. Infect Control Hosp Epidemiol. 1992;13(10):606–608.
- Jänes A, Cengiz Y, Israelsson LA. Preventing parastomal hernia with a prosthetic mesh: a 5-year follow-up of a randomized study. World J Surg. 2009;33(1):118–121.
- Correa Marinez A, Bock D, Carlsson E, et al. Stoma-related complications: a report from the Stoma-Const randomized controlled trial. Colorectal Dis. 2021;23(5):1091–1101.
- ) De Robles MS, Young CJ. Parastomal hernia repair with onlay mesh remains a safe and effective approach. BMC Surg. 2020;20(1):296.
- Cross AJ, Buchwald PL, Frizelle FA, et al. Meta-analysis of prophylactic mesh to prevent parastomal hernia. Br J Surg. 2017;104(3):179–186.
- Mäkäräinen-Uhlbäck E, Wiik H, Kössi J, et al. Chimney trial: study protocol for a randomized controlled trial. Trials. 2019;20(1):652.
- van Hemelrijck M, Thorstenson A, Smith P, et al. Risk of in-hospital complications after radical cystectomy for urinary bladder carcinoma: population-based follow-up study of 7608 patients. BJU Int. 2013;112(8):1113–1120.
- Hammond TM, Huang A, Prosser K, et al. Parastomal hernia prevention using a novel collagen implant: a randomised controlled phase 1 study. Hernia. 2008;12(5):475–481.
- Rege S, Singh A, Rewatkar A, et al. Laparoscopic parastomal hernia repair: a modified technique of mesh placement in sugarbaker procedure. J Minim Access Surg. 2019;15(3):224–228.
- Rodriguez Faba O, Rosales A, Breda A, et al. Simplified technique for parastomal hernia repair after radical cystectomy and ileal conduit creation. Urology. 2011;77(6):1491–1494.
- Donahue TF, Cha EK, Bochner BH. Rationale and early experience with prophylactic placement of mesh to prevent parastomal hernia formation after ileal conduit urinary diversion and cystectomy for bladder cancer. Curr Urol Rep. 2016;17(2):9.
- Rezaee ME, Goldwag JL, Goddard B, et al. Parastomal hernia development after cystectomy and ileal conduit for bladder cancer: results from the dartmouth ileal conduit enhancement (DICE) project. Can J Urol. 2020;27(5):10369–10377.
- Stephenson BM. The lateral rectus abdominis positioned stoma (LRAPS) in the construction of end colostomies, loop ileostomies and ileal conduits. Hernia. 2021;25(3):803–808.