Abstract
Objective
The most common form of urinary bladder cancer is the low and intermediate risk categories of stage Ta. This patient group has a high recurrence rate, but progression is rare. The aim of this study was to investigate recurrence and survival in a large population-based setting, with respect to possible prognostic factors and during different time periods.
Patients and methods
BladderBaSe is a database which links information from the Swedish National Register of Urinary Bladder Cancer with national healthcare and demographic registers. Between 1997 and 2014, 16,599 were diagnosed with low and intermediate risk of Ta cancer in Sweden. The times to recurrence and cancer-specific death were analysed concerning the differences in age, gender, grade, region and hospital type. For temporal analysis, we divided the material into 6-year periods.
Results
The mean age was 70 years and 75% were males. Low risk according to grade constituted 56%, whilst 44% had intermediate risk. With a median follow-up time of 63 months the recurrence rates were 47% and 59% for the respective categories and overall 52%. The rate was similar between the first two time periods, but became substantially lower in the most recent period. Five percent of patients died of the disease and risk category was the main prognostic variable.
Conclusions
The risk of recurrence decreased in the last time period. Risk category based on grade was the most important prognostic indicator for outcome.
Introduction
Urinary bladder cancer (UBC) is the third most common form of cancer among men and the ninth among women in Sweden, with around 2,500 new diagnoses and 600 deaths each year. At the time of detection, about two thirds of cases were non-muscle-invasive bladder cancer (NMIBC). Of these cases, the most common subgroups were low- and intermediate-risk, characterised by frequent recurrences. Cancer deaths are late and rare events, thus not very well studied because it requires long-term follow-up of large populations. Most reports concerning this emanate from single centres, centres of excellence or from prospective treatment studies [Citation1] – all of which are probably affected, to some extent, by selection bias. Therefore, population-based investigations on this topic are scarce and usually only use overall survival as an endpoint [Citation2].
The Bladder Cancer Data Base Sweden (BladderBaSe) is useful for these kinds of studies, as we have found when analysing the outcome of tumour types categorised as high-risk NMIBC (T1G2, TaG3 and T1G3) [Citation3].
We have earlier reported data for all risk groups of NMIBC at two earlier time points in the Swedish National Register of Urinary Bladder Cancer (SNRUBC). In the initial report, the management and outcome of patients diagnosed between 1997 and 2001 was studied, revealing a regional variation in the initial treatment [Citation4]. In the second report, the recurrence and progression of patients diagnosed in 2004–2007 were investigated 5 years after diagnosis [Citation5]. The incidence of recurrence and progression was found to be high and, as in the first analysis, important disparities in outcome related to patterns of care appeared to exist between different healthcare regions.
The aim of this new study was to examine patients with low- and intermediate-risk NMIBC to complement our earlier report on the high-risk category. Specifically, we sought to: (1) Identify these patients in a nationwide, population-based cohort. (2) Investigate the clinical profile at the time of diagnosis. (3) Determine the recurrence rate and the cancer-specific survival in relation to the initial clinical profile. (4) Analyse the possible variations in outcome due to hospital type and healthcare region.
Materials and methods
Since 1997, patients with newly diagnosed UBC have been reported to the SNRUBC. The national register has detailed data on an average 97% of bladder cancer cases diagnosed in Sweden. BladderBaSe was created in 2015 and this database links information from the SNRUBC from 1997 to 2014, with a number of national healthcare and demographic registers with personal identification numbers [Citation6]. As it is additionally linked to other national registers, information on patients’ comorbidities, socioeconomics, re-admissions, adverse effects and causes of death is also available.
The outcome was determined as recurrence, defined by a repeat transurethral resection (TURB) later than 3 months after diagnosis to discard residual tumours. Date and cause of death were obtained from the Cause of Death Register and death from bladder cancer was defined as International Classification of Disease (ICD)-10 code C67. The Research Ethics Board at Uppsala University, Sweden (DNR 2015/277) approved the project.
Selection of study sample
Between 1997 and 2014, 26,808 patients were diagnosed with NMIBC in Sweden, of which 16,599 belonged to the low- or immediate-risk tumour types. Data on age at diagnosis, date of diagnosis, healthcare region, follow-up time, bladder cancer death and other causes of death were registered. Hospital type (university, county and district) was used as an indicator of patient volumes.
Statistical methods
The start date of the study was the date of diagnosis and the last date of the study was the date of death, emigration or 31 December 2014 – whichever occurred first. The time unit used was months and Kaplan-Meier survival curves are presented to assess the absolute risk to patients.
The endpoints of the study were recurrence, as defined above, and overall and bladder cancer death. Relationships between clinical characteristics and the endpoints were analysed in cross-tables by Pearson’s statistics under the hypothesis that the rows and columns in a two-way table are independent, or using Fisher’s exact test when appropriate.
A Cox proportional hazards model was used to analyse age, gender, tumour grade, hospital type and healthcare region in relation to recurrence and survival of the disease. Statistical significance was set at p < 0.05. For temporal analysis, we used three periods, each with a 6-year duration.
Results
During the study period, 16,599 were diagnosed with low and intermediate risk of NMIBC. The median follow-up time in the study sample was 63 months and 860 (5.2%) patients died of bladder cancer and 6,019 (36%) died of other causes. The mean age at diagnosis was 70 years and 75% of patients were males. Low-risk, according to grade, constituted 56% of cases, whilst 44% had intermediate-risk. These categories displayed different characteristics, as displayed in . Intermediate risk patients were more frequently from local hospitals and became fewer during later periods of the register. Low-risk patients were significantly younger and more likely to be female.
Table 1. Characteristics of patients with low (G1) and intermediate (G2) risk NMIBC in Sweden, 1997–2014.
The recurrence rate was 52% overall and higher for the intermediate category, 59% as opposed to 47% for the low risk patients. Of those with recurrence, 39% had two, 22% had three, 13% had four and 27% had five or more repeated TURBs. The timing of first recurrences was within 1 year after the first TURB for 30% of cases. The remaining recurrences for the following years were; 2 years 10%, 3 years 4%, 4 years 2% and 5 years 1%. Less than 2% of recurrences occurred more than 5 years after the first TURB.
In a univariate Cox proportional hazards model, recurrent disease was associated with male gender, higher age, G2 disease, earlier time periods and type of hospital (non-university). Furthermore, patients treated in the southern and the western healthcare regions had an increased relative risk of recurrence ().
Table 2. Univariate and multivariate Cox regression analyses of rate of recurrence and bladder cancer death.
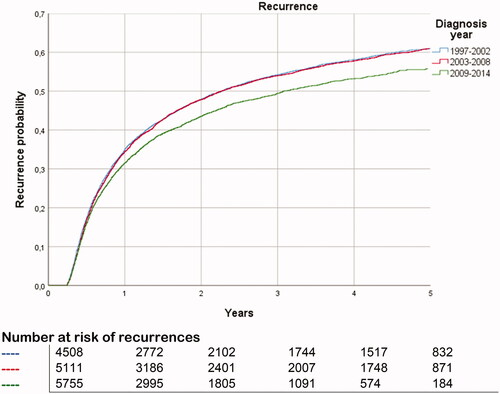
In a multivariate analysis, an increased relative risk of recurrence was found for patients with G2 disease, smaller hospital (non-university), higher age, not belonging to the south-east region and earlier time periods (). The latter is illustrated in with the first two time periods, with higher rates of recurrence than the most recent period.
Figure 1. Risk of recurrences for patients with low- and intermediate-risk stratified by time periods.
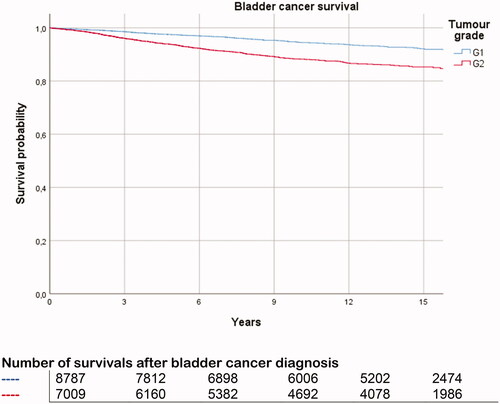
During the study period, 3.3% of those of low and 7.5% of those of intermediate-risk died of bladder cancer. The 5, 10 and 15-year cancer-specific death rates were 3.2%, 4.7% and 5.1%, respectively ().
In a univariate analysis, bladder cancer death was associated with higher age, male gender, smaller hospital and G2 disease (). The corresponding risk in a multivariate analysis was male gender, higher age, grade 2, smaller hospital, and not treated in the western region.
Discussion
In this study, we found that the risk category – based on histological grade – predicted long-term outcome, both regarding recurrence risk and cancer-specific survival. Around half of patients with low- and intermediate-risk bladder cancer have a recurrence that most commonly occurs early within the follow-up period. Recurrence is high in the first 2 years after diagnosis and very rare after 5 years. It was also evident that this high recurrence rate became lower during the most recent time period. Bladder cancer mortality is late and rare compared to other mortalities in these patients.
The main strengths of our study are the prospective registration, the large number of patients observed, the quality of the data, and the nationwide recruitment base. We had access to several high-quality nationwide registers with data on tumour characteristics, treatment and covariates, which provided an analysis of the possible variations in outcome due to hospital type and healthcare regions.
As in all registry trials, there are limitations to this study. The capture rate of quality registers and how representative they are requires assessment to ensure that the data is generalizable. A caveat is that other important tumour characteristics such as size and multiplicity were not registered.
Another shortcoming is the absence of histological reviews of tumour grade and stage. Data on postoperative chemotherapy instillations are lacking but, to our knowledge, this was seldom used during the study period among these patients.
Furthermore, the definition of recurrence could be questioned. As this was not registered from the start of the registry, we chose to select the TURB later than 3 months after diagnosis as the endpoint. This definition has two weaknesses working in opposing directions. First, recurrences could be missed if they were treated in the outpatient department with biopsy or ablation only. On the other hand, the TURB could occur without findings of malignancy. The latter was found in one-third of these procedures in a recent Danish study [Citation7]. However, their diagnostic policies differed from ours in many ways, for example, not using cytology in suspicious cases.
That study focused on long-term treatment and outcome in 10,197 patients with up to 16-years follow-up. Their risk grouping was in low- and high-grade Ta tumours, and thus not directly comparable to our grouping criteria. However, an interesting finding in their results was that repeated transurethral procedures under general anaesthesia appear to be associated with increased risk of overall death in patients with NMIBC. Unfortunately, the present Swedish database does not have a control population necessary for this type of analysis. This population is included in the upcoming version and will be possible to study in the future.
Most publications have found that female gender is associated with higher risks, which seems contrary to our findings. In fact when looking at the highest risk of NMIBC (grade 3), not part of this study, the same relation exists (data not shown). The previous literature on this issue does not stratify for different stages, thus further analysis of this should be of interest.
Progression is often reported in the literature and in nomograms but was not registered in the early years of the registry. Consequently, we could not evaluate this in the present analysis. The 5-year progression rate in the previous study from the registry covering the period 2004 to 2007 was 5% and 8% in the respective risk groups.
Cancer-specific survival could be considered as a non-issue, especially in low risk patients, but the dismal outcome of progressing patients indicate that mortality is occurring even in non-high- risk patients. When compared to other mortality, it is low for this relatively high age group.
A European study, which had the same categorisation as in our study, found that the overall 10-year survival in G1 patients was 68% and in G2 patients around 59%, but they did not have data on cancer-specific survival [Citation2]. Holmäng et al. [Citation8] found an 11% 20-year cancer-specific mortality among patients with stage Ta treated between 1963 and 1972 but also included grade 3 tumours. The above-cited Danish study used relative survival and reported a 6% mortality at 5-years for Ta LG patients.
In a systemic analysis of two EORTC trials, the subgroup of patients with TaG1 had a 5-year cancer mortality rate of 13% but the patients were treated with BCG, indicating that selection factors were probably involved [Citation9]. The reason why these tumours with low potential for disseminating disease lead to metastases and death is unknown. Is it because of incomplete resection at initial TURB and further tumour growth facilitating development of new mutations? Alternatively, has a new tumour type evolved as a separate entity? Clearly, this is an interesting question for future research.
As Liedberg et al. [Citation5] reported, important disparities in recurrences related to care strategies appear to exist between different healthcare regions in Sweden. In contrast to the present study, high-risk tumours were included where adjuvant therapies are recommended. They found that hospital type influences recurrence risk with outcome better in high volume settings and we can now add that cancer-specific mortality was lower in these hospitals. Management of patients with muscle-invasive cancers has become more centralised during later years in Sweden. This is not practical regarding low- and intermediate-risk bladder cancer due to the high number of patients. The reason for the differences in outcome for these categories is not possible to further analyse in the present registry data. However, the examples of improved quality with the introduction of standardised protocol and reducing the number of surgeons for primary treatment of all NMIBC in a regional Swedish study could be adopted on a national level to decrease regional disparities in outcome [Citation10].
The lower recurrence rates in the most recent period are promising and may be due to improved quality of surgery, by better education of surgeons and more use of single-dose postoperative chemotherapy instillation. Furthermore, the common use of blue light at cystoscopy could also have been beneficial [Citation11]. It would be interesting to explore this in more detail in the future.
Conclusion
In conclusion, the majority of patients with NMIBC belong to the studied category. Among those patients, grade was the most important prognostic indicator for long-term outcome. Recurrence rates were high in the first 2 years after diagnosis, whilst they were very rare after 5 years of follow-up.
Rates decreased in the last time period studied. Mortality was low and mostly due to non-bladder cancer related disease.
Acknowledgements
We would like to thank the steering committee of Bladderbase; Staffan Jahnson, Abolfazl Hosseini, Fredrik Liedberg, Oskar Hagberg, Amir Sherif, Viveka Ströck, Karin Söderkvist, Anders Ullen, Christel Häggström, Lars Holmberg and Firas Aljabery for support.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Rieken M, Xylinas E, Kluth L, et al. Long-term cancer-specific outcomes of TaG1 urothelial carcinoma of the bladder. Eur Urol. 2014;65(1):201–209.
- Balan D, Martha O, Chibelean CB, et al. Comparison of 10-year overall survival between patients with G1 and G2 grade Ta bladder tumors. Medicine (Baltimore). 2018;97(16):e0522.
- Wang EY, Larsson U, Gårdmark T, et al. Radical cystectomy compared to intravesical BCG immunotherapy for high-risk non-muscle invasive bladder cancer - is there a long-term survival difference? A Swedish nationwide analysis. Scand J Urol. 2021;55(1):46–52.
- Gårdmark T, Bladström A, Hellsten S, et al. Analysis of clinical characteristics, management and survival of patients with Ta T1 bladder tumours in Sweden between 1997 and 2001. Scand J Urol Nephrol. 2006;40(4):276–282.
- Liedberg F, Hagberg O, Holmäng S, et al. Local recurrence and progression of non-muscle-invasive bladder cancer in Sweden: a population-based follow-up study. Scand J Urol. 2015;49(4):290–295.
- Häggström C, Liedberg F, Hagberg O, et al. Cohort profile: the Swedish National Register of Urinary Bladder Cancer (SNRUBC) and the Bladder Cancer Data Base Sweden (BladderBaSe). BMJ Open. 2017;7(9):e016606.
- Erikson MS, Petersen AC, Andersen KK, et al. National incidence and survival of patients with non-invasive papillary urothelial carcinoma: a Danish population study. Scand J Urol. 2018;52(5–6):364–370.
- Holmäng S, Hedelin H, Anderström C, et al. The relationship among multiple recurrences, progression and prognosis of patients with stages Ta and T1 transitional cell cancer of the bladder followed for at least 20 years. J Urol. 1995;153(6):1823–1826.
- Cambier S, Sylvester RJ, Collette L, et al. EORTC nomograms and risk groups for predicting recurrence, progression, and disease-specific and overall survival in non-muscle-invasive stage Ta-T1 urothelial bladder cancer patients treated with 1–3 years of maintenance Bacillus Calmette-Guérin. Eur Urol. 2016;69(1):60–69.
- Sörenby A, Baseckas G, Bendahl PO, et al. Reducing recurrence in non-muscle-invasive bladder cancer by systematically implementing guideline-based recommendations: effect of a prospective intervention in primary bladder cancer patients. Scand J Urol. 2019;53(2–3):109–115.
- Malmström PU, Grabe M, Haug ES, et al. Role of hexaminolevulinate-guided fluorescence cystoscopy in bladder cancer: critical analysis of the latest data and European guidance. Scand J Urol Nephrol. 2012;46(2):108–116.