A 30-year-old male patient presented to our clinic with an 18-year history of gradually aggravated fissured tongue, which had been progressively enlarged and stiffened for the past 6 months. He also experienced poor lingual agility that was occasionally accompanied by irritating pain of the tongue over the past 10 years. The patient was diagnosed with oral candidiasis in 2006 and received treatment with a 3% sodium bicarbonate solution mouth rinse and nystatin tablet for several years. However, his clinical symptoms did not show any significant improvement. Physical examination revealed deep fissures on his tongue dorsum with unclear-bordered nodular hyperplasia, as well as obvious redness and congestion. Additionally, thickened white plaques with a granular surface were observed on the stiffened dorsum and lateral border of the tongue ((A)). Irregular white lesions were also present on the palate, buccal mucosa, and lower lip, and could not be easily scrapped off. The patient did not exhibit typical cutaneous manifestations except for an erythematous plaque with adherent scaling on his antihelix ((B)). Scraping specimen of the patient’s tongue dorsum was collected, and the microscopic examination (10% KOH smear and calcofluor white fluorescent staining) confirmed the presence of pseudohyphae and hyphae. Additionally, histopathological examination of lingual mucosa biopsy specimens revealed hyperparakeratosis of the superficial mucosa, with inflammatory cell infiltration and microabscess formation ((C)). The periodic acid–Schiff staining demonstrated fungal hyphae, traversing perpendicularly through the epithelium to the spinous layer ((D)). Candida albicans was isolated from saliva culture and identified by CHROMagar Candida plates and 18S rDNA sequencing. Comprehensive assessments, including complete blood count (CBC), liver and renal function tests, blood glucose tests, and thyroid function tests (triiodothyronine, thyroxine, and thyroid-stimulating hormone tests), showed normal results. No history of consanguineous marriage was reported in his family.
Figure 1. Clinical features and IL-17RC mutations in the present case. A. Tongue dorsum displayed deep fissures with unclear-bordered nodular hyperplasia, along with thickened white plaques with a granular surface on the stiffened dorsum and the lateral border. B. The patient had no typical cutaneous manifestations except for an erythematous plaque with adherent scaling on the antihelix. C. Histopathological examination of the lingual mucosa biopsy specimens revealed superficial mucosal hyperparakeratosis, inflammatory cell infiltration, and microabscess formation (magnification: ×100). D. The periodic acid–Schiff staining demonstrated fungal hyphae traversing perpendicularly through the surface epithelium up to the spinous cell layer (magnification: ×200). E. Sanger sequencing of the IL-17RC gene in family members of the patient: *arrows indicate the mutation sites.
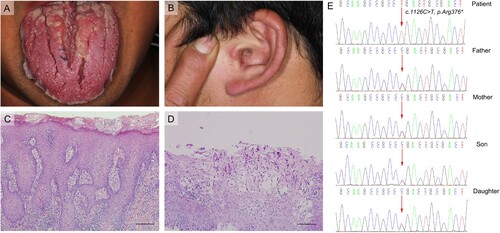
Due to the extended history of persistent oral candidiasis and the peculiar tongue lesions, genetic susceptibility was suspected, and whole-exome sequencing (WES) was performed. A homozygous nonsense mutation of the IL-17RC gene (c.1126C > T, p.Arg376*) was found in the patient. His parents, daughter, and son were healthy and heterozygous for the mutant allele, confirming autosomal recessive (AR) inheritance ((E)). Based on the patient’s medical history, clinical signs, histopathological findings, and genetic test results, a definitive diagnosis of chronic mucocutaneous candidiasis (CMC) was established. Oral fluconazole was administered at 100 mg/day (with an initial 200 mg) according to the antifungal susceptibility test. During the subsequent treatment, regular three-month follow-up assessments were conducted to monitor the antifungal susceptibility and the liver and renal function of the patient. After fluconazole therapy for 1 month, the patient’s auricular lesion healed completely, and the tongue fissures with nodular hyperplasia and white lesions subsequently recessed after 4 months. The treatment is ongoing, and the patient is under clinical follow-up.
CMC is a primary immunodeficiency disease characterized by recurrent or persistent infections of the skin, nails, oral and genital mucosae caused by Candida species, mainly C. albicans [Citation1,Citation2]. Over the past decade, many studies have highlighted the pivotal role of IL-17 related immunity in host defence against mucocutaneous Candida infections [Citation3]. Moreover, many genetic mutations have been identified to cause CMC and increased susceptibility to other fungal infections, including STAT1, STAT3, CARD9, AIRE, CLEC7A, RORC, ACT1, and the IL-17 deficiencies (IL-17A, IL-17F, IL-17RA, IL-17RC) [Citation2,Citation4]. Among them, STAT1 gain-of-function (GOF) mutations, which lead to defective Th17 responses, are found to be the most common genetic causes of CMC in China and worldwide [Citation1,Citation5,Citation6].
As key receptors mediating the IL-17 signalling pathway, IL-17RA and IL-17RC deficiencies have also been shown to be the genetic aetiologies of CMC. When mutations in either gene occurs, the binding of IL-17A and IL-17F to their receptors (the IL-17RA/IL-17RC complex) will be impeded, and inhibit the activation of the downstream pathways essential for antifungal activities [Citation3,Citation7]. Since 2011, a total of 23 patients with CMC from 13 unrelated kindreds in 7 countries have been reported to have autosomal recessive IL-17RA deficiency [Citation4,Citation8,Citation9]. There is only one study reported CMC patients with autosomal recessive IL-17RC deficiency, in which three CMC patients aged 8, 12, and 37 years from unrelated kindreds originating from Argentina and Turkey were described [Citation10]. The patients were homozygous for different nonsense alleles (c.412C > T, c.1126C > T, and c.1132C > T mutations) that prevent the expression of IL-17RC. The clinical manifestations of these patients included chronic intertrigo, skin and scalp pustules, and recurrent oral and oesophageal thrush. Unlike individuals with IL-17RA deficiency, these patients did not have any other significant infections, particularly Staphylococcus aureus skin infections, and they exhibited impaired responses to IL-17A and IL-17F, while maintaining normal responses to IL-17E/IL-25 [Citation4,Citation10].
The present case is the first reported case of inherited IL-17RC deficiency in CMC patients in the Chinese population. Compared to the previous study, the present patient was mainly characterized by oral manifestation, instead of typical dermatological manifestations of CMC. Despite the common perception of the fissured tongue as a benign condition characterized by deep fissures of varying depth, size, and number on the tongue dorsum [Citation11,Citation12], this patient mainly presented with long-term refractory fissured tongue accompanied by nodular hyperplasia, redness and congestion. However, he was initially misdiagnosed with fissured tongue and oral candidiasis, and it took 18 years until CMC was confirmed through WES analysis. Therefore, this case reminds us that young patients who develop refractory fissured tongue should be considered to screen for CMC, and a comprehensive assessment of family history, pathology examination, including PAS staining, as well as the genetic susceptibility is essential. In addition, although there is currently no adequate treatment targeting the patient’s gene mutation, appropriate antifungal therapy and close follow-up of the patient are also very critical. Furthermore, this case underscores the significance of multidisciplinary teamwork (MDT) in achieving diagnosis and developing personalized treatment strategies. Regarding potential pathogenic mechanisms, we speculate that the appearance of refractory fissured tongue may be linked to ineffective control of Candida infections and lingual mucosa hyperplasia due to chronic inflammation, although the specific mechanisms remain to be explored in future research.
Supplemental Material
Download PDF (263.6 KB)Supplemental Material
Download PDF (133.3 KB)Supplemental Material
Download PDF (611.2 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- van de Veerdonk FL, Plantinga TS, Hoischen A, et al. STAT1 mutations in autosomal dominant chronic mucocutaneous candidiasis. N Engl J Med. 2011;365:54–61. doi:10.1056/NEJMoa1100102
- Puel A, Cypowyj S, Bustamante J, et al. Chronic mucocutaneous candidiasis in humans with inborn errors of interleukin-17 immunity. Science. 2011;332:65–68. doi:10.1126/science.1200439
- Mengesha BG, Conti HR. The role of IL-17 in protection against mucosal candida infections. J Fungi (Basel). 2017;3:52. doi:10.3390/jof3040052
- Cifaldi C, Ursu GM, D’Alba I, et al. Main human inborn errors of immunity leading to fungal infections. Clin Microbiol Infect. 2022;28:1435–1440. doi:10.1016/j.cmi.2022.06.031
- Toubiana J, Okada S, Hiller J, et al. Heterozygous STAT1 gain-of-function mutations underlie an unexpectedly broad clinical phenotype. Blood. 2016;127:3154–3164. doi:10.1182/blood-2015-11-679902
- Wang X, Zhang R, Wu W, et al. New and recurrent STAT1 mutations in seven Chinese patients with chronic mucocutaneous candidiasis. Int J Dermatol. 2017;56:e30–e33. doi:10.1111/ijd.13427
- Puel A, Cypowyj S, Maródi L, et al. Inborn errors of human IL-17 immunity underlie chronic mucocutaneous candidiasis. Curr Opin Allergy Clin Immunol. 2012;12:616–622. doi:10.1097/ACI.0b013e328358cc0b
- Fellmann F, Angelini F, Wassenberg J, et al. IL-17 receptor A and adenosine deaminase 2 deficiency in siblings with recurrent infections and chronic inflammation. J Allergy Clin Immunol. 2016;137:1189–1196.e2. doi:10.1016/j.jaci.2015.07.053
- Lévy R, Okada S, Béziat V, et al. Genetic, immunological, and clinical features of patients with bacterial and fungal infections due to inherited IL-17RA deficiency. Proc Natl Acad Sci U S A. 2016;113:E8277–e8285. doi:10.1073/pnas.1618300114
- Ling Y, Cypowyj S, Aytekin C, et al. Inherited IL-17RC deficiency in patients with chronic mucocutaneous candidiasis. J Exp Med. 2015;212:619–631. doi:10.1084/jem.20141065
- Scully C. Oral and maxillofacial medicine: the basis of diagnosis and treatment. Edinburgh: Churchill Livingstone Elsevier; 2008.
- Dafar A, Çevik-Aras H, Robledo-Sierra J, et al. Factors associated with geographic tongue and fissured tongue. Acta Odontol Scand. 2016;74:210–216. doi:10.3109/00016357.2015.1087046
