ABSTRACT
The main objectives of this study were to investigate the association between childhood violence and psychological distress and post-traumatic stress symptoms (PTS) among Sami and non-Sami adults, and to explore a possible mediating effect of childhood violence on any ethnic differences in mental health. This study is part of a larger questionnaire survey on health and living conditions in Mid- and Northern Norway (SAMINOR 2) which included 2116 Sami and 8674 non-Sami participants. A positive association between childhood violence and psychological distress and PTS in adulthood was found regardless of ethnicity. For women, childhood violence may have mediated some of the ethnic differences in psychological distress (53.2%) and PTS (31.4%). A similar pattern was found for men as to psychological distress (45.5%) and PTS (55.5%). The prevalence of psychological distress was significantly higher in the Sami than in the non-Sami group: 15.8% vs. 13.0% for women, and 11.4% vs. 8.0% for men. Likewise, PTS showed a higher prevalence in the Sami group, both for women (16.2% vs. 12.4%) and for men (12.2% vs. 9.1). Conclusion: A positive association between childhood violence and adult mental distress was found for both Sami and Norwegian adults. More mental problems were found among the Sami. Childhood violence may have mediated some of the ethnic differences.
Background
The World Health Organization (WHO) has recognised interpersonal violence as an important, worldwide public health issue that adversely affects both mental and physical health [Citation1]. Childhood violence is defined as all forms of physical and/or emotional maltreatment, sexual abuse, neglect, negligence and commercial or other exploitation, which result in actual or potential harm to the child`s health, survival, development or dignity in the context of a relationship of responsibility, trust or power[Citation2]. Globally, the prevalence of childhood violence varies among countries, regions, genders and ages. Approximately 20% of women and 5–10% of men report childhood sexual abuse. Nearly a quarter of adults (22.6%) suffered physical abuse as a child, and 36.3% suffered emotional abuse [Citation1]. The lifelong consequences of child maltreatment include impaired physical and mental health, poorer school performance, and job and relationship difficulties [Citation3–Citation6]. The WHO has listed a range of health risks associated with interpersonal violence in childhood [Citation7]. As for mental health, depression and post-traumatic stress disorders (PTSDs) are considered the most prevalent conditions associated with violence and abuse [Citation4,Citation8–Citation11]. Mental health problems may preclude people to realise their potential, cope with the normal stresses of life, work productively and contribute to their communities [Citation5]. People with mental disorders experiences disproportionately higher rates of disability and mortality [Citation2].
Indigenous peoples have been shown to be more prone to various types of mental health problems, such as mental distress, post-traumatic stress, and suicidal ideation and attempts, compared to the majority groups [Citation12–Citation17]. These disparities have often been linked to colonisation,forced assimilation, violence and discrimination[Citation17–Citation19].
Indigenous people in the Arctic region is home to different groups that share a common history of social injustice and oppression [Citation12,Citation20–Citation23]. Most of the indigenous Sami live in the Arctic region of the Nordic countries and Russia’s Kola Peninsula. They have traditionally been a nomadic people combining reindeer husbandry with small-scale fishing and agriculture. The Sami have their own culture and language [Citation24]. As in the other countries, the Sami in Norway have suffered under a severe assimilation policy. This policy came into effect around 1850 [Citation23] and had wide-reaching implications, including prohibition on teaching in the Sami language in schools, and limited opportunities for developing and preserving Sami culture and identity [Citation23,Citation25,Citation26]. The assimilation process had the greatest impact on Sami people living in the coastal areas. In these areas, the Sami are a minority (Sami minority areas); whereas, in the highland communities, the Sami have been a majority (Sami majority areas), and the assimilation process has not had equally severe consequences [Citation23,Citation24,Citation27].
We hypothesised that exposure to violence in childhood would be a risk factor for mental distress and post-traumatic stress symptom (PTS) in adulthood. International studies from a wide range of cultural settings show that childhood violence is associated with poorer mental health [Citation25–Citation35]. However, to our knowledge, this association has not previously been examined in a Sami population. The above-mentioned differences in living area may have an impact on mental health status, as a protective effect of a strong Sami identity on mental distress has been demonstrated [Citation28]. Further, Laestadianism (a special branch of the Christian Lutheran Church) still plays an important role in many Sami families [Citation29]. An association between sense of coherence and subjective well-being has also been demonstrated [Citation30] as well as between spirituality and health-related symptoms [Citation31]. Affiliation to the Laestadian church and living area was therefore included as a variable that could potentially protect against mental distress following childhood violence. Although, ambiguous results of mental health problems among indigenous compared to the majority groups [Citation12], we hypothesised that mental health problems might be more prevalent among the Sami than among the non-Sami participants. Finally, we hypothesised that childhood violence might mediate some of the ethnic differences in adult mental health problems.
The aims of the present study were:
to investigate whether the association between childhood violence and mental health problems (psychological distress and symptoms of PTS) differed between Sami and non-Sami adults.
to investigate whether there were any ethnic differences in the prevalence of mental health problems (psychological distress and symptoms of PTS) between Sami and non-Sami.
to investigate whether exposure to childhood violence might have any mediating effect on ethnic differences in mental health.
Materials and methods
This study is based on data from a population-based study on health and living conditions in areas with both Sami and Norwegian settlements: the SAMINOR 2 Questionnaire survey conducted in 2012. The first SAMINOR study, SAMINOR 1, was conducted in 2003/2004 and is described in detail in a previous paper [Citation32]. The SAMINOR 2 Questionnaire survey was designed as a follow-up study and was expanded to include additional health issues, including further mental health indicators and questions on interpersonal violence. The SAMINOR 2 study is described in more detail in another paper [Citation33].
Sample
All inhabitants aged 18–69 who were registered in the Central Population Registry in selected multi-ethnic municipalities (mixed Sami and non-Sami populations) received a letter of invitation to participate in the study. Out of 44,669 invitations, 1,424 were returned unopened, leaving 43,245 persons eligible for the study. Among these, 11,600 returned a completed questionnaire, yielding a participation rate of 27%. In the present study, 96 respondents were excluded due to missing information on ethnicity, 567 due to missing information on 3 or more items on the psychological distress measurement (HSCL-10), 26 due to missing information on symptoms of PTS and 121 respondents due to missing information on violence. This provides a total sample of 10,790 participants: 2,116 Sami (19.6%) and 8,674 non-Sami (80.4%).
Variables
Ethnicity
When classifying ethnicity in this study, linguistic affiliation and self-identity were used as criteria. Ethnicity was assessed by the following questions: (1) “What language do/did you use at home?” (2) “What language did your parents use at home?” (3) “What language did your grandparents use at home?” and (4) “What do you consider your own ethnicity to be?” The response options were: “Norwegian”, “Sami”, “Kven” and “Other”. Participants who chose “Sami” in response to any of the first 3 questions, and who also identified themselves as Sami, were classified as belonging to the Sami ethnic group. To use both Sami self-identification and Sami language, competency by either the participants themselves, parents or grandparents are used almost similarly by the Norwegian Sami Parliament to register voters [Citation34]. The linguistic criterion by the Sami Parliament also reaches back to great grandparents, but was not feasible in the SAMINOR 2 questionnaire. Thus, using ethnicity as a variable within research has been much discussed. Various definitions and inclusion criteria of the Sami group have been used in previously studies. The variety of definitions of Sami ethnicity is thoroughly discussed in a recent thesis by Pettersen [Citation34]. Pettersen showed that self-identification seems to be the most complex and challenging measure, but valid criterion for belonging to the Sami group [Citation34,Citation36]. Sami language has in several studies been found to be a strong ethnic identity marker [Citation37]. Norwegians, Kvens (descendants of Finnish immigrants) and “Others” were defined as non-Sami. In the non-Sami group, the vast majority defined themselves as ethnic Norwegians. The variables are described in more detail by Lund et al. [Citation32], Brustad et al. [Citation33] and Hansen et al. [Citation38].
Psychological distress (HSCL-10)
A 10-item version of the Hopkins Symptoms Check List (HSCL-10) was used to measure psychological distress [Citation39]. The HSCL-10 addresses respondents’ experiences during the previous 4 weeks of: (1) sudden anxiety, (2) anxiousness, (3) dizziness, (4) tension/stress, (5) self-blame, (6) sleeplessness, (7) sadness, (8) worthlessness, (9) finding everything burdensome and (10) hopelessness. Each item was rated on a 4-point scale, from 1 “Not at all” to 4 “Very often”. In accordance with earlier validation studies [Citation39], the mean HSCL-10 score was calculated by summing up the scores for each item and dividing the total score by 10. In a recent validation study on respondents of the SAMINOR 2 study, no significant measurement invariance between the included ethnic groups appeared [Citation40]. This indicates that the HSCL-10 response scale predominantly was used in the same way and that significantly different meanings were not ascribed to the same set of questions. The cut-off criteria of 1.85 as indicative of psychological distress based on Norwegian data, equals a score of 1.89, 1.94 and 1.92 in the Sami core, Sami affiliation and Sami background groups, respectively. Thus, the same cut-off criterion 1.85 may be safely used in all groups [Citation40]. Respondents with missing data on 3 or more items were excluded. Those participants who scored above the cut-off point of 1.85 were classified as suffering from psychological distress.
PTS (NorAQ)
PTS during the last 12 months were assessed by 3 questions, concerning (1) Intrusive memories, (2) avoidance of certain situations and (3) emotional numbness. Each question had 4 response options: “No”, “Yes, but rarely”, “Sometimes” and “Often”. Respondents who answered “Sometimes” or “Often” on 2 or 3 symptoms were classified as having symptoms of PTS. The responses “Yes, but rarely” or “Not at all” were defined as “No symptoms”. These 3 items measuring symptoms of PTS have previously been used in a study on mental health in Sweden [Citation41].
Violence
Three subsections of the SAMINOR 2 questionnaire addressed emotional, physical and/or sexual violence. Participants who responded positively to the dichotomous question “Have you experienced that someone systematically and over time has tried to repress or humiliate you?” were classified as “Having experienced emotional violence”. Participants who responded positively to the dichotomous question “Have you been exposed to physical assault/abuse?” were classified as “Having experienced physical violence”. Participants who responded positively to the question “Have you been exposed to sexual assault?” were classified as “Having experienced sexual violence”. Those who gave a positive response to any of the above questions were classified as having experienced “Any violence”. Respondents were asked whether the exposure to violence had occurred in childhood and/or in adulthood using the following alternatives: “Yes, as a child”, “Yes, as an adult” and “Yes, in the past 12 months”. Participants who reported emotional, physical and/or sexual violence as children were classified as “Having been exposed to the different types of violence in childhood”.
Other variables
Background information including level of education and household income was collected from the questionnaire. Age and gender were derived from Statistics Norway (SSB), and age was categorised into age groups of 18–34, 35–49 and 50–69 years. The following classification of education was applied: primary school (≤ 0–9 years), high school (10–12 years), higher university or college education ≤ 3 years (13–15 years) and university education > 3 years (16 years and more). Family/household income per year was categorised into 3 groups: low (< 150,000–300,000 NOK (1 NOK = 0.12 USD, 19 December 2017)), medium (301,000–600,000 NOK), and high (601,000–900,000 NOK).
Respondents were asked to indicate their affiliation with the Laestadian Church with the following questions: “Are your grandparents affiliated with the Laestadian church?”, “Is your father affiliated with the Laestadian church?”, “Is your mother affiliated with the Laestadian church?” and “Are you affiliated with the Laestadian church?”. Participants who responded positively to 1 or more of these options were classified as “Laestadianist”. Respondents with no positive response on Laestadian church affiliation were classified as “Non-Laestadianist”.
The 25 municipalities included in the SAMINOR 2 study were classified as either “Sami minority area” or “Sami majority area”. The Sami majority areas were characterised by having a Sami majority population and being long-time proponents of Sami language, culture and primary industries (including reindeer husbandry) [Citation20]. Areas in which the Sami people are considered a minority were categorised as “Sami minority areas”. More detailed information about the 25 municipalities included in the SAMINOR 2 study has been published in a previous paper [Citation33].
Ethics
The data collection and storage of data were approved by the Norwegian Data Protection Authority (Datatilsynet). Written informed consent was obtained from all participants. The study was approved by the Regional Committee for Medical and Health Research Ethics of Northern Norway (REK-Nord) and Statistics Norway (SSB).
Statistical analysis
IBM SPSS Statistics Version 22.0 and 24.9 and Stata 15 for Windows was used to conduct statistical analyses.
Frequencies and cross tabulations were used to present the distribution of socio-demographic variables, psychological distress, PTS and childhood violence by ethnicity and gender. The Chi-square test was used for the comparison between Sami and non-Sami respondents. Level of significance was set to p≤0.05.
Logistic regressions were performed to assess the association between childhood violence and psychological distress and PTS. Estimates are presented as Odds Ratios (OR) and 95% confidence intervals (95% CI). We also included living area and affiliation with Laestadianism in the model. Stratified analysis was conducted based on ethnicity and gender. Since both psychological distress and symptoms of PTS were common outcomes, OR are higher than the corresponding prevalence ratio (PR) [Citation42]. Interaction between any childhood violence and ethnicity on psychological distress and PTS was tested.
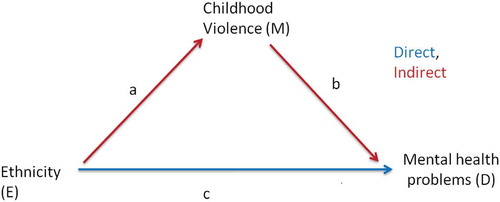
To explore whether exposure to childhood violence had a mediating effect on the ethnic differences in mental health problems, we did a mediation analysis using ethnicity as exposure, childhood violence as meditator and psychological distress or PTS symptoms as outcomes [Citation43] (). We used linear regressions for the total and direct regressions on the binary outcomes. We estimated the total effect (without the mediator in the model). Then we adjusted for the mediator to get the direct effect. The indirect effect was calculated as the total minus the direct effect. The mediated proportion is the indirect divided by the total effect. Since ethnicity does not depend on age, sex and education, we do not have ordinary confounding in the analysis, that is, we have no confounding between exposure and outcome, and no confounding between exposure and mediator. However, we may have confounding between mediator and outcome. Here we think age, education and sex are mediator-outcome confounders. We therefore stratified the mediation analysis on sex and adjusted for age and education in the direct effect model. We used Stata’s “seemingly unrelated regression” command to combine the total and direct models, thereby getting p-values and CI for the indirect effects and the mediated proportions. We did not use robust variance estimation in the linear regressions, since this is not permitted with seemingly unrelated regressions. Instead we compared standard errors with and without robust variance and found only minor (< 10%) differences.
This mediation approach is valid if there is no E-M interaction in the total model 8and we have collapsible measures). The so called controlled and natural direct (and indirect) effects coincide in this situation. Our E-M interaction terms were not significant, and the linear model gives collapsible measures.
The internal consistency between the 3 items measuring PTS was tested by the Cronbach’s alpha coefficient, and was found to be acceptable (0.75).
Results
Background characteristics, mental health and childhood violence are reported in . A higher proportion of the Sami women were younger and reported a higher educational level than non-Sami women (70% vs. 62%), whereas there were no ethnic differences in age and educational levels among men. The Sami respondents reported a lower household income than the non-Sami, and more than twice as many Sami reported affiliation with Laestadianism compared to the non-Sami.
Table 1. Background characteristics, reported childhood violence and mental health in the Sami and non-Sami population.
Childhood violence
A significantly higher proportion of Sami women than non-Sami women reported exposure to childhood violence (31.3% vs. 21.6%, p<0.001), while corresponding findings for men were 28.3% and 16.6%, respectively (p<0.001). The prevalence of childhood violence is thoroughly described in a previous publication [Citation44].
The association between childhood violence and mental health problems
When investigating the association between violence in childhood and adult mental health problems, stratified analysis by gender and ethnicity were conducted. Results are presented in and . Regardless of ethnicity, respondents who reported childhood violence were more than 3 times as likely to suffer from psychological distress (adjusted OR for women = 3.7, CI: 3.1–4.3, adjusted OR for men = 3.7, CI: 2.9–4.6) and over twice as likely to exhibit symptoms of PTS (adjusted OR for women = 3.0, CI: 2.5–3.5, adjusted OR for men = 3.5, CI: 2.8–4.3) than respondents who reported no experience of violence in childhood ( and ). In stratified analyses by gender, there were no interactions between childhood violence and ethnicity on psychological distress (p=.256 among women and .571 among men) or PTS (p=.403 among women and p=.165 among men). When adjusting for age, education, living area and religion, none of these factors had any significant impact on the estimates.
Table 2. The association between childhood violence and psycological distress in Sami and non-Sami and total sample.
Table 3. The association between childhood violence and symptoms of PTS in Sami and non-Sami and total sample.
Mental health problems
Ethnic differences in mental health were found, with a significantly higher prevalence of psychological distress among Sami than among non-Sami women (15.8% vs. 13.0%, p=.010) and among Sami compared to non-Sami men (11.4% vs. 8.0%, p=.001, ). Differences were also identified in the prevalence of PTS symptoms: 16.2% among Sami women vs. 12.4% among non-Sami women (p=.001), and 12.2% among the Sami men vs. 9.1% among non-Sami men (p=.005, ).
The impact of childhood violence on ethnic differences in mental health
The results from the mediator analysis showed that about half of the effect of ethnicity on psychological distress for men was mediated through childhood violence (mediated proportion was 45.5%), and the figure for women was 53.2%. The mediated proportion for PTS and men was 55.5 and 31.4% for women (age and education level adjusted analysis).
Discussion
This is the first study to present findings on the association between childhood violence and adult mental health in a Sami population. Moreover, we compared the prevalence in mental health problems between the 2 ethnic groups and investigated the potential mediating effect of childhood violence on ethnic differences in mental health problems between Sami and non-Sami.
Associations between childhood violence and adult mental health problems
The findings of significant associations between childhood violence and psychological distress and symptoms of post-traumatic stress in both Sami and non-Sami respondents strengthen the hypothesis that violent victimisation generally affects mental health, regardless of ethnic background [Citation45–Citation48]. As concluded in a previous systematic review and meta-analyses of child abuse [Citation45], all forms of child maltreatment should be considered important risk to health, including to a range of mental disorders. According to our study, this applies to the Sami as well. Our hypothesis that living in a Sami majority area and affiliation with Laestdianism would be protective against mental health problems was not supported by our findings. This could be because ethnic identity affiliation might not be affected by whether or not 1 is living in a minority or majority area. A possible explanation of why religious affiliation did not have any impact might be that the Laestadian church tends to advice against seeking help from the majority society [Citation49]. Such attitudes might have cancelled out the positive effect between spirituality and mental health. However, other factors that are also related to mental health was not included, such as physical activity, drug use/misuse, other life stressors (e.g. job loss, loss of partners/children), general adversity (e.g. social isolation, economic hardships), somatic illnesses, or psychological vulnerability (e.g. neuroticism or negative thinking). This must be regarded as a major limitation. Further, similar to our study, a study of violence, sexual abuse and health among the Inuit in Greenland [Citation47] found that having been victim of violence or sexual abuse was significantly associated with several health problems, including mental health problems. For the indigenous of the North, these findings highlight the importance of culturally informed preventive programmes focusing on the influence of childhood violence on mental health in these populations. Moreover, our findings support the findings of a recent study in the Norwegian population which found that different forms of childhood violence were a risk factor for victimisation in adulthood among Norwegians [Citation46]. However, our study did not examine the influence of the different forms of childhood violence on adult mental health, and a more detailed examination of the different forms of violence on mental health in a Sami population is warranted.
Mental health – cross-cultural comparisons
We found a higher prevalence of psychological distress among both Sami men and Sami women compared to the non-Sami population. Very few population-based studies are available on the prevalence and types of mental health problems among the adult Sami population [Citation50]. Moreover, the results of these studies are ambiguous [Citation12], probably due to differences in problem formulation and study design [Citation12,Citation17]. Further, the lack of differences in mental health problems between Sami and Norwegians, as presented in certain earlier papers [Citation13,Citation17], may be due to overlooked within-group differences in the Sami population. For instance, some Sami subgroups may be less vulnerable to mental health problems due to protective factors at an individual, family and/or community level [Citation28,Citation51]. Our results of a higher prevalence of psychological distress among Sami compared to the non-Sami is different from the results of the SAMINOR 1 study from 2003/2004 [Citation17], in which ethnic differences were found for men only. Both studies are population-based, but the latter study had a higher response rate (60.6%), and hence may represent a more reliable result concerning mental health prevalence estimate. Consequently, our prevalence estimate must be interpreted with caution. However, our findings are in line with other Sami studies [Citation52,Citation53]. The Swedish study by Kaiser et al. [Citation52] found that the Sami disclosed higher mean values for both depression and anxiety than the majority population, with Sami men reporting the highest rates. In a study comparing Sami adolescents to majority Norwegian adolescents, it was found that Sami adolescents, particularly those living in assimilated ethnic communities, reported more behavioural problems [Citation53].
Moreover, international studies comparing mental health among indigenous and non-indigenous people in Australia, the US and Canada, have found a higher prevalence of mental health problems among the indigenous populations [Citation54,Citation55]. It is commonly believed that inferior mental health conditions among indigenous people may be due to historical injustice and oppression [Citation50]. Our finding of a higher prevalence of PTS symptoms among the Sami than among the non-Sami may reflect more trauma exposure among the Sami compared to the majority population [Citation11,Citation56]. To our knowledge, no studies on PTSD diagnosis or PTS among indigenous Sami have previously been performed. Future studies are warranted to confirm our findings.
Mediating effect of childhood violence on ethnic differences in mental health
The results of the mediator analysis showed that a substantial part of the ethnic differences was mediated thought childhood violence. Our findings suggest that childhood violence may be an important risk factor mediating the higher level of mental health problems in the Sami population.
Strengths and limitations
The cross-sectional design limits the potential for assessing possible causal links between childhood violence and current mental distress and symptoms of PTS [Citation57]. However, since our study measures violence in childhood and its association with adult mental health, the exposures of reported violence are likely to have taken place prior to the reported mental distress condition. Hence, childhood violence probably plays a role in the development of later mental health problems.
Validation of the HSCL-10 has been performed by other researchers and has proven to be a valid and reliable instrument [Citation39,Citation40]. The 3 items measuring PTS are not sufficient to meet all the DSM-V criteria for a PTSD diagnosis. This represents a major limitation, and our findings concerning PTS symptoms should be regarded with caution. In the future, more comprehensive studies are needed in order to verify the results.
The questions that were used to assess childhood violence were taken from the NorVold Abuse Questionnaire (NorAQ), and abbreviated and modified. The validation study showed that the abuse variables in the NorAQ had good reliability and validity [Citation58]. However, the questions have not been validated in a Sami population. Thus, we cannot rule out the possibility of misinterpretation of questions and of different interpretations due to cultural and linguistic differences.
Recollection bias may relate to a general tendency among adult people to underreport childhood violence [Citation5], thus reducing the association to adult mental health problems. Another possibility is that current anxiety and depression may increase the tendency to recollect and report life events in a more negative and traumatic way [Citation59,Citation60], thus strengthening the negative association with mental health problems. However, those experiencing good times may also be inclined to report fewer adverse childhood events, thus weakening the negative association with mental health [Citation61].
Data were collected in Sami-Norwegian municipalities, which made it possible to assess ethnic differences within the same geographical area. This must be regarded as strength of the study.
When classifying ethnicity, linguistic affiliation and self-identity were used as criteria. The Sami Parliament in their registration of voters uses both criteria almost similar. Hence, misclassification of responders with respect to Sami ethnicity is not very likely. A fundamental question is whether the results change with different definitions of the Sami group [Citation62]. To answer some of the questions regarding varying definitions and potentially divergent outcomes, additional analysis have been conducted. To investigate whether the prevalence estimate of mental health problems changed with different definitions of the Sami, we conducted additional analyses. Definition II was a broader definition than we have used. In addition to our definition, it includes an affirmative response to the question “my ethnic background is Sami”. This definition is used in several papers utilising data from the SAMINOR 1 questionnaire study [Citation63]. Definition III, which is also used in other studies, Sami ethnicity was defined by Sami being the home language of grandparents, parents and respondents. Varying the definition II do not change the ethnic differences in the prevalence of mental health problems among men (psychological distress: Sami 11.5% vs. 7.7 non-Sami, p<.000, PTS: Sami 12.5% vs. 8.8% non-Sami, p<.000) or women (psychological distress: Sami 16.5% vs. 12.6 non-Sami, p<.000, PTS: Sami 16.2% vs. 12.2% non-Sami, p<.000). Varying the definition III some differences were found: Among men, the ethnic difference remained but was only significant in psychological distress (Sami 11.2% vs. 8.4% non-Sami, p=.044; PTS: Sami men 11.7% vs. 9.5% non-Sami, p=.145). For women, there were no significant ethnic difference in psychological distress (Sami 14.2% vs. 13.5% non-Sami, p=.637), but the significant differences for PTS remained (Sami 17.6% vs. 12.7% non-Sami, p=.001). Hence, other ethnic definitions do not primarily change the results of our study.
However, due to the former Norwegian assimilation policy, some who are Sami according to these criteria might have denied their Sami background [Citation23], and may have reported their ethnic background as Norwegian. This may have resulted in misclassification of exposure, and our estimated association between ethnicity and mental distress may hence be conservative.
The low participation rate in the SAMINOR 2 questionnaire study (27%) indicates that the results must be interpreted with caution. We have limited information about the non-respondents. Accordingly, selection bias is likely. Since ethnicity is not recorded in any official register in Norway, we were not able to assess whether the proportion of the non-respondents differed in the 2 ethnic groups. However, a comparison between participants in the SAMINOR 2 study and those participating in the SAMINOR 1 study has been made [Citation33]. The participation rate in SAMINOR 1 was considerably higher (60.9%) than in the present study, but the proportion of participants classified as Sami did not differ between SAMINOR 1 and SAMINOR 2. We therefore assume that the proportion of the non-respondents in SAMINOR 2 is equally distributed among the Sami and the non-Sami.
The large number of participants is the strength of our study. The same applies to the inclusion of many background variables, which enabled us to control for potential confounding factors. However, unknown potential confounders unequally distributed between Sami and non-Sami respondents may have had an impact on our results. Known risk factors associated with poor mental health, such as childhood loss (e.g. death of a parent or parental divorce) and parental mental illness, were not taken into account in our study [Citation64].
Non-respondents in our study differed from respondents with respect to gender, age and education. Participants were older and more likely to have a high education, and more women than men participated [Citation33]. This conforms well with other studies, which have found that participation rates generally increase with age, female gender and higher education level [Citation65]. The difference between respondents and non-respondents presents a socio-economic gradient that may have influenced the prevalence estimates of interpersonal violence and adult mental health problems. The prevalence may be different among the non-respondents. Since both childhood violence and mental health problems were associated with young age and low educational level in our study, the estimated prevalence between childhood abuse and mental problems may have been higher if these groups had been included. However, the prevalence estimate might also be inflated. For association measures, the risk of bias is much smaller, even when the response rate is low [Citation66]. Hence, our association measures are more reliable than our prevalence estimates.
Conclusion
In both ethnic groups, childhood violence was associated with psychological distress and symptoms of PTS in adulthood. Psychological distress and symptoms of post-traumatic stress were more prevalent in the Sami than in the non-Sami group. Childhood violence mediated some of the ethnic differences in mental health problems, both among women and men. More research on interpersonal violence and mental health among the Sami is needed.
Declarations
Ethics and consent to participate
The study was approved by the Regional Committee for Medical and Health Research Ethics of Northern Norway (REK-Nord) and based on written consent. The SAMINOR study has concession for storage of individual information and for later linkages (under the Norwegian Health Registry Law). An information letter was attached to the questionnaire. All possible linkages and further use of the data material is carefully described in the invitation letter. Persons were asked to participate in a study on health, illness and living conditions in areas with both Sami and Norwegian populations. The questionnaire was posted in both a Norwegian and a Sami version. Participants consented by returning the completed questionnaire. The project owner of the SAMINOR-project is the Arctic University of Norway, UiT, by the University Director.
Availability of data and materials
Data is stored at the Centre for Sami Health Research, UiT, The Arctic University of Norway. Website: https://uit.no/om/enhet/forsiden?p_dimension_id=88115.
Supplemental Material
Download MS Excel (35 KB)Acknowledgments
The authors wish to thank all the participants in this study. The authors also wish to thank the Northern Norway Regional Health Authority (Helse Nord) and the Sami National Centre for Mental Health and Substance Abuse (SANKS) for funding. Finally, they are grateful to the Centre for Sami Health Research, The Arctic University of Norway, UiT, for all support.
Disclosure statement
No potential conflict of interest was reported by the authors.
Supplementary material
Supplementary data for this article can be accessed here.
Additional information
Funding
References
- Krug EG, Mercy JA, Dahlberg LL, et al. The world report on violence and health. Lancet. 2002;360(9339):1083–11.
- Butchart A. Global status report on violence prevention. Geneva: World Health Organisation; 2014.
- Springer KW, Sheridan J, Kuo D, et al. The long-term health outcomes of childhood abuse. An overview and a call to action. J Gen Intern Med. 2003;18(10):864–870.
- Springer KW, Sheridan J, Kuo D, et al. Long-term physical and mental health consequences of childhood physical abuse: results from a large population-based sample of men and women. Child Abuse Negl. 2007;31(5):517–530.
- Gilbert R, Widom CS, Browne K, et al. Burden and consequences of child maltreatment in high-income countries. Lancet. 2009;373(9657):68–81.
- Sethi D, Bellis M, Hughes K, et al. European report on preventing child maltreatment. Copenhagen, Denmark: WHO Regional Office for Europe; 2013.
- WHO. The WHO multi-country study on women`s health and domestic violence against women. Geneva, Switzerland: World Health Organization; 2005.
- Kaplow JB, Dodge KA, Amaya-Jackson L, et al. Pathways to PTSD, part II: sexually abused children. Am J Psychiatry. 2005;162(7):1305–1310.
- Kaplow JB, Widom CS. Age of onset of child maltreatment predicts long-term mental health outcomes. J Abnorm Psychol. 2007;116(1):176–187.
- Maniglio R. The impact of child sexual abuse on health: a systematic review of reviews. Clin Psychol Rev. 2009;29(7):647–657.
- Nadew GT. Exposure to traumatic events, prevalence of posttraumatic stress disorder and alcohol abuse in Aboriginal communities. Rural Remote Health. 2012;12(4):1667.
- Lehti V, Niemela S, Hoven C, et al. Mental health, substance use and suicidal behaviour among young indigenous people in the Arctic: a systematic review. Soc Sci Med. 2009;69(8):1194–1203.
- Silviken A, Haldorsen T, Kvernmo S. Suicide among indigenous Sami in Arctic Norway, 1970-1998. Eur J Epidemiol. 2006;21(9):707–713.
- Omma L, Jacobsson LH, Petersen S. The health of young Swedish Sami with special reference to mental health. Int J Circumpolar Health. 2012;71:18381.
- Young TK, Revich B, Soininen L. Suicide in circumpolar regions: an introduction and overview. Int J Circumpolar Health. 2015;74:27349.
- Stoor JP, Kaiser N, Jacobsson L, et al. “We are like lemmings”: making sense of the cultural meaning(s) of suicide among the indigenous Sami in Sweden. Int J Circumpolar Health. 2015;74:27669.
- Hansen KL, Sorlie T. Ethnic discrimination and psychological distress: a study of Sami and non-Sami populations in Norway. Transcultural Psychiatry. 2012;49(1):26–50.
- Kirmayer LJ, Brass G. Addressing global health disparities among indigenous peoples. Lancet. 2016;388:105–106.
- Valeggia CR, Snodgrass JJ. Health of Indigenous Peoples. Annu Rev Anthropol. 2015;44(1):117–135.
- Hansen KL. Ethnic discrimination and health: the relationship between experienced ethnic discrimination and multiple health domains in Norway’s rural Sami population. Int J Circumpolar Health. 2015;74:25125.
- Hansen KL, Melhus M, Hogmo A, et al. Ethnic discrimination and bullying in the Sami and non-Sami populations in Norway: the SAMINOR study. Int J Circumpolar Health. 2008;67(1):97–113.
- Bjerregaard P, Young TK, Dewailly E, et al. Indigenous health in the Arctic: an overview of the circumpolar Inuit population. Scand J Public Health. 2004;32(5):390–395.
- Minde H. Assimilation of the Sami: implementation and consequences. Vol. nr 3/2005. Kautokeino: Resource Centre for the Rights of Indigenous Peoples; 2005.
- Hætta OM. SAMENE- Nordkalottens urfolk (The Sami - the people of the north). Kristiansand: Høyskoleforlaget; 2002.
- Niemi E. Kategoriens etikk og minoritetene i nord. Et historisk perspektiv (The ethics of categorise and minorities in the north. A historical perspective). Oslo: NESH De nasjonale forskningsetikse komiteer; 2002.
- Pedersen P, Høgmo A. SÀPMI slår tilbake (Sàpmi strikes back). Karasjok: Càlliid Làgàgadus; 2012.
- Aubert V. Den samiske befolkningen i Nord-Norge (the Sami population in Northern Norway). Vol. 107. Oslo: Statistisk Sentralbyrå; 1978.
- Friborg O, Sørlie T, Hansen KL. Resilience to discrimination among Indigenous Sami and Non-Sami populations in Norway: the SAMINOR2 study. J Cross Cult Psychol. 2017;48(7):1009–1027.
- Spein AR, Melhus M, Kristiansen RE, et al. The influence of religious factors on drinking behavior among young indigenous Sami and non-Sami peers in northern Norway. J Relig Health. 2011;50(4):1024–1039.
- Schneider G, Driesch G, Kruse A, et al. What influences self-perception of health in the elderly? The role of objective health condition, subjective well-being and sense of coherence. Arch Gerontol Geriatr. 2004;39(3):227–237.
- Carmody J, Reed G, Kristeller J, et al. Mindfulness, spirituality, and health-related symptoms. J Psychosom Res. 2008;64(4):393–403.
- Lund E, Melhus M, Hansen KL, et al. Population based study of health and living conditions in areas with both Sami and Norwegian populations–the SAMINOR study. Int J Circumpolar Health. 2007;66(2):113–128.
- Brustad M, Hansen KL, Broderstad AR, et al. A population-based study on health and living conditions in areas with mixed Sami and Norwegian settlements - the SAMINOR 2 questionnaire study. Int J Circumpolar Health. 2014;73:23147.
- Pettersen T, Magritt B. Sámi ethnicity as a variable. Premises and implications for population-based studies on health and living conditions in Norway. Tromsø: UiT The Arctic University of Norway; 2015.
- Bhopal RS. Concepts of epidemiology: integrating the ideas, theories, principles and methods of epidemiology. Oxford: Oxford University press; 2016.
- Pettersen T, Brustad M. Which Sámi? Sámi inclusion criteria in population-based studies of Sámi health and living conditions in Norway - an exploratory study exemplified with data from the SAMINOR study. Int J Circumpolat Health. 2013;72:21813.
- Nystad K, Spein AR, Balto AM, et al. Ethnic identity negotiation among Sami youth living in a majority Sami community in Norway. Int J Circumpolar Health. 2017;76(1):1316939.
- Hansen KL, Minton SJ, Friborg O, et al. Discrimination amongst Arctic Indigenous Sami and Non-Sami Populations in Norway - the SAMINOR 2 questionnaire study. Journal of Northern Studies. 2016;10(2):45–84.
- Strand BH, Dalgard OS, Tambs K, et al. Measuring the mental health status of the Norwegian population: a comparison of the instruments SCL-25, SCL-10, SCL-5 and MHI-5 (SF-36). Nord J Psychiatry. 2003;57(2):113–118.
- Sørlie T, Hansen KL, Friborg O. Do Norwegian Sami and non-indigenous individuals understand questions about mental health similary? A SAMINOR 2 study. Int J Circumpolar Health. Forthcoming 2018;77: 1481325.
- Wangel AM, Schei B, Ryding EL, et al. Mental health status in pregnancy among native and non-native Swedish speaking women: a Bidens study. Acta Obstet Gynecol Scand. 2012;91:1395–1401.
- Veierød M, Lydersen S, Laake P, editors. MEDICAL STATISTICS in clinical and epidemiological reseach. 1st ed. Oslo: Gyldendal Norsk Forlag; 2012.
- VanderWeele TJ. Mediation analysis: a practitioner’s guide. Annu Rev Public Health. 2016;37:17–32.
- Eriksen AM, Hansen KL, Javo C, et al. Emotional, physical and sexual violence among Sami and non-Sami populations in Norway: the SAMINOR 2 questionnaire study. Scand J Public Health. 2015;43:588–596.
- Norman RE, Byambaa M, De R, et al. The long-term health consequences of child physical abuse, emotional abuse, and neglect: a systematic review and meta-analysis. PLoS Med. 2012;9(11):e1001349.
- Thoresen S, Myhre M, Wentzel-Larsen T, et al. Violence against children, later victimisation, and mental health: a cross-sectional study of the general Norwegian population. Eur J Psychotraumatol. 2015;6:26259.
- Curtis T, Larsen FB, Helweg-Larsen K, et al. Violence, sexual abuse and health in Greenland. Int J Circumpolar Health. 2002;61(2):110–122.
- Evans-Campbell T, Lindhorst T, Huang B, et al. Interpersonal violence in the lives of urban American Indian and Alaska Native women: implications for health, mental health, and help-seeking. Am J Public Health. 2006;96(8):1416–1422.
- Norbakken E. Når ord mangler…om seksuelle overgrep i luthersk-læstadianske miljøer (when words are missing….about sexual assaults in Lutheran-Laestadian environments). Master. Oslo: Diakonhjemmets Høgskole; 2012.
- Anderson I, Robson B, Connolly M, et al. Indigenous and tribal peoples’ health (the Lancet-Lowitja institute global collaboration): a population study. Lancet. 2016;388:131–157.
- MacDonald JP, Ford JD, Willox AC, et al. A review of protective factors and causal mechanisms that enhance the mental health of Indigenous Circumpolar youth. Int J Circumpolar Health. 2013;72:21775.
- Kaiser N, Sjolander P, Liljegren AE, et al. Depression and anxiety in the reindeer-herding Sami population of Sweden. Int J Circumpolar Health. 2010;69(4):383–393.
- Kvernmo S, Heyerdahl S. Influence of ethnic factors on behavior problems in indigenous Sami and majority Norwegian adolescents. J Am Acad Child Adolesc Psychiatry. 1998;37(7):743–751.
- Cunningham J, Paradies YC. Socio-demographic factors and psychological distress in Indigenous and non-Indigenous Australian adults aged 18-64 years: analysis of national survey data. BMC Public Health. 2012;12:95.
- Barnes PM, Adams PF, Powell-Griner E. Health characteristics of the American Indian or Alaska native adult population: United States, 2004-2008. Natl Health Stat Report. 2010;20:1–22.
- Kirmayer LJ, Gone JP, Moses J. Rethinking historical trauma. Transcultural Psychiatry. 2014;51(3):299–319.
- Rothman KJ. Epidemiology n introduction. 2nd ed. New York: Oxford University Press; 2012.
- Swahnberg IM, Wijma B. The NorVold Abuse Questionnaire (NorAQ): validation of new measures of emotional, physical, and sexual abuse, and abuse in the health care system among women. Eur J Public Health. 2003;13(4):361–366.
- Jeronimus BF, Riese H, Sanderman R, et al. Mutual reinforcement between neuroticism and life experiences: a five-wave, 16-year study to test reciprocal causation. J Pers Soc Psychol. 2014;107(4):751–764.
- Ormel J, Riese H, Rosmalen JG. Interpreting neuroticism scores across the adult life course: immutable or experience-dependent set points of negative affect? Clin Psychol Rev. 2012;32(1):71–79.
- Colman I, Kingsbury M, Garad Y, et al. Consistency in adult reporting of adverse childhood experiences. Psychol Med. 2016;46(3):543–549.
- Eriksen AMA. “Breaking the silence” interpersonal violence and health among Sami and non-Sami. A population-based study in mid- and Northern Norway. Tromsø: UiT - the arctic university of Norway; 2017.
- Eriksen AMA, Javo C. “Breaking the silence” interpersonal violence and health among Sami and non-Sami. A population-based study in Mid- and Northern Norway. Tromsø: UiT The Arctic University of Norway; 2017.
- Hosman C, Janè-Llopis, E, Saxena S, editors. Prevention of mental disorders. Geneva: World Health Organization; 2004.
- Sogaard AJ, Selmer R, Bjertness E, et al. The Oslo health study: the impact of self-selection in a large, population-based survey. Int J Equity Health. 2004;3(1):3.
- Eagan TML, Eide GE, Gulsvik A, et al. Nonresponse in a community cohort study: predictors and consequences for exposure–disease associations. J Clin Epidemiol. 2002;55(8):775–781.