ABSTRACT
Background: The ageing Arctic populations raise the need for work-up of cognitive function that reflects language and cultural understandings.
Aim: To translate and evaluate tools for work-up of cognitive impairment in Greenland.
Methods: Step A: An expert panel was established to select tools suitable for the work-up of cognitive impairment at three different settings in Greenland. Step B: Tools were translated in a multiple-step process of independent translations with back-translation and adaptations by two independent translators and two Greenlandic physicians. Step C: a testing and validation process of the tools at three locations: the national hospital in the capital city; regional hospital in a town; health care centre in a small town.
Results: Tools selected were Mini-Cog and RUDAS. Participants for testing of tools were 43 of 61 invited, of which six had dementia. RUDAS and Mini-Cog scores were associated (p < 0.001). The smoothed AUC was 0.87 (95%-CI, 0.65–0.95) for Mini-Cog and 0.90 (95%-CI, 0.76–0.97) for RUDAS. The sensitivity of Mini-Cog with a cut-off at ≤3 was 83.3%, and specificity was 62.2%. For RUDAS with a cut-off at ≤23, these were 100% and 75.7%, respectively.
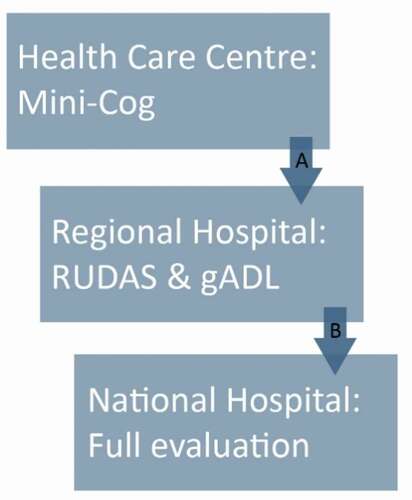
Conclusion: Requested tools have been translated for assessing cognitive function in the native Arctic setting. Small town residents with a Mini-Cog score of 3 or lower should be referred to a regional hospital for RUDAS, and a score of 23 or less should cause referral to the national hospital for a full work-up of cognitive function.
Introduction
Dementia is a clinical syndrome characterised by symptoms and signs of difficulties in memory function, language disturbances, impairments in orientation, planning, judgement, and abstraction. It is a debilitating condition characterised by a slow progression of memory function loss [Citation1]. The common causes of dementia are Alzheimer’s disease (AD) (50%), vascular dementia (25%), mixed Alzheimer’s disease and vascular dementia (included in the above, 25%), Lewy body dementia (15%), and other forms (about 5% combined) [Citation2].
The risk of cognitive impairment increases with age, and the populations of developing societies are ageing. Greenlandic societies have seen a rapid transition over the past decades, accompanied by a steep rise in life expectancy [Citation3].
Mapping of dementia in Greenland found 254 registered with such diagnosis in 2011. However, the diagnostic work-up was often concluded without medical consultancy, and the diagnosis was made by the nursing home staff, which is a heterogeneous group [Citation4].
Presently, work-up of suspected dementia is performed in regional hospital/ health care centres. This allows people to remain in known surroundings. Referral to the national hospital only occurs with other causes of cognitive impairment, while support to rural health care including a pathway for referral is needed [Citation5]. Moreover, the work-up for dementia uses tools, which are not validated for use amongst Greenlanders.
This led us to translate tools for the work-up of cognitive impairment in Greenland. We considered the restrictions caused by Greenland’s vast geography, and thus we constructed an algorithm for assessing cognitive function in the work-up of suspected dementia. The tools’ feasibility was evaluated, and the tools were validated for use in the Arctic setting.
Material and methods
Population and setting
Greenland is sparsely populated, with a population of 56.081 inhabitants in 2020. Among these, 3,397 are 65–74 years old, and 1,488 are aged above 75 years. This is an increase of 126% since 2000 [Citation3]. Inhabitants are scattered along the world’s largest island’s vast coastline with 2,166,086 km2, where 85% of Greenland is covered by ice. No cities are connected by road or rail. All transport is either by boat/ship or by air and only if the weather conditions allow it [Citation6].
Greenland’s health care system is divided into five regions by geography. Each region hosts one regional hospital, a number of health care centres with educated health care staff in smaller towns, and health care stations in villages, where staff often have no health care education. The total number of health care centres and stations is 74. The capital city (Nuuk) has the national hospital, Queen Ingrid’s Hospital, which delivers specialised diagnostics and treatment to all Greenland citizens [Citation7].
Expert panel and selection of tools
An expert panel was constructed. It consisted of a geriatrician, neurologist, psychiatrist, and experienced physiotherapist, and a nurse with years of experience in the Greenlandic Health Care system. The final member of the expert panel was a Greenlandic doctor one year into the clinical training (IK). This doctor grew up at a sheep farm in southern Greenland, and all education up until university was in three different parts of Greenland. Thus, this doctor has advanced skills in Greenlandic language and culture.
The first author (IK) presented tools for work-up of dementia to the expert panel. The tests included for in-depth discussions were Mini-Cog, MMSE, MoCA, RUDAS, and ACE-R. Pros and cons were discussed, aiming at a consensus for which tool was most suitable for use in Greenland. Criteria for selecting tools included that the test was simple to use, had a low risk of misinterpretations, usefulness in various settings, translated into several languages and used internationally, and a consideration of time consumption. Additionally, the selection of the test to be used in small towns was based on validation for use by evaluators without extensive training.
Tools and translation
Two tools were selected for the translation process, the Mini-Cog and the Rowland Universal Dementia Assessment Scale (RUDAS). RUDAS was already used in Greenland n a Danish version as Danish is the language spoken by health care staff in Greenland. Thus, the source language was Danish for the RUDAS and English for the Mini-Cog, and the target language was Greenlandic. The translation process is illustrated in .
Figure 1. A schematic presentation of the translation process
First, a Greenlandic translator from the Therapy Department at Queen Ingrid’s Hospital translated source language versions to Greenlandic (1). This translator had some routine in conducting tests for cognitive impairment. The first version in Greenlandic (1) was reviewed by a Greenlandic doctor (author IK) to ensure the translation fits the Greenlandic context (2). A second certified translator translated Greenlandic (2) to Danish (2). This translator was blinded to the original versions. A second Greenlandic doctor (author PN) reviewed the process () and adjusted the final Greenlandic (3) based on Danish (2) and Greenlandic (2). The certified translator performed back-translation of Greenlandic (3) to Danish (3). The first Greenlandic author (IK) compared the final version of the tools with the originals and approved Greenlandic (3) before implementation. All four who were involved in translation are trilingual in Greenlandic, Danish, and English.
Mini-Cog
The Mini-Cog tool includes two components. First, mentioning three items to recall later, second, drawing of a clock, followed by recalling the three items mentioned initially. It required only a few minutes to administer and can be used by any healthcare professional, and its administration and scoring do not require extensive training. The maximum score is five [Citation8–10]. A cut-off of ≤2 is validated and suggested for dementia screening, but if greater sensitivity is desired, a cut-off ≤3 is recommended [Citation8–10].
The Rowland Universal Dementia Assessment Scale (RUDAS)
RUDAS has six items, and the domains covered are memory recall, body orientation, praxis, drawing, judgement, and language. It takes about 10 minutes to administer. It has a score interval of 0–30 points. A total score below 23 suggests dementia [Citation11,Citation12]. RUDAS was translated from the version validated for use in a Danish memory clinic [Citation13].
Activities of daily living (ADL)
In Nuuk, facilities are available for direct observational assessment of ADL. It includes a modern kitchen. The kitchen has tap water and conveniences allowing patients to demonstrate almost everything they do in their kitchen. This could be making coffee or breakfast, washing up, and using a broom and vacuum cleaner. Health care centres outside Nuuk do not have facilities for direct observational ADL assessment. At present, it is done in the consultation room, where the patient can be observed while hoovering, sweeping the floor, dusting off shelves and windowsills. This Greenlandic ADL (gADL) was used in the rural setting.
Participants
Invitation for participation was based on a randomised selection among inhabitants aged 65 years or above in three different places. The names and dates of birth were provided in compliance with ethical approval and Greenlandic legislation, and contact information was available from the local hospital. We selected subjects for participation using www.randomised.com. Participants were contacted by phone and informed about the project based on the information sheet for participants approved by the ethics committee. They were then asked if they were interested in participating. If a diagnosis of dementia was recorded, consent was provided by a carer or nearest relative.
In the capital with a national hospital (Nuuk), 14 were invited for the investigation. One refused participation, one cancelled participation, and one did not show up for the appointment. The final sample comprised 11 participants.
In the town with a regional hospital (Qaqortoq), 26 were invited, 6 refused participation, four did not show up for the appointment. Thus, the final sample was 16 participants, five of which were recorded as having a dementia diagnosis.
In the small town with a health care centre (Narsaq), 21 were invited, one refused participation, and three did not show up for the appointment. One was excluded because of the language (Greenlandic, not the first language). The final sample in the small town comprised 16 participants, of which one had a dementia diagnosis.
In accordance with inclusion criteria, all were over 65 years, and Greenlandic was their first language.
Care homes for older adults gather information and keep a list of who had a dementia diagnosis. However, the source of information for this list is unclear.
The investigation included taking a history, a full neurological examination, completing the two tools in Greenlandic and ADL/gADL. The examination took about one hour.
Training of testing
Seven older subjects in Nuuk were included in a training session for the data collector (IK). In addition, the feasibility of RUDAS and ADL/gADL and the time consumption were estimated to guide the planning of data collection. These results were not included in the final analysis, while the guiding information in Greenlandic to each test was adjusted following pilot testing.
Ethics approval
Ethical approval was granted by the Committee for Scientific Research in Greenland (KVUG 2018–20) before the commencement of the study, and the health authorities in Greenland sanctioned the study. Participants signed informed consent before investigational procedures.
Statistics and data analysis
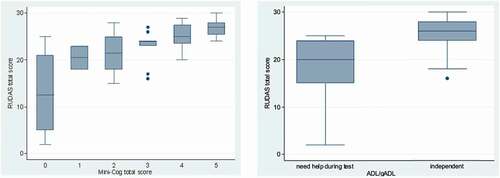
Continuous data on participants were described using medians and interquartile ranges (IQR) and mean and standard deviation (SD). Categorical data on participants were given as numbers and percentages. Results from the Mini-Cog and gADL were compared to RUDAS results graphically using Box Plots. Associations were tested using Spearman’s correlation coefficient and Fisher’s Exact test as appropriate. These analyses were performed using Stata version 16.1.
Smoothed receiver-operating characteristic (ROC) curves of Mini-Cog and RUDAS performance at identifying participants with and without dementia were plotted. Area under the curve (AUC) values with 95% confidence intervals for each curve were determined using 2000 bootstrapped samples. The Youden index was calculated for each test to determine the optimal cut-off value. Confidence intervals for sensitivities and specificities were calculated using 2000 bootstrapped samples. A similar analysis was made for the Mini-Cog’s ability to discriminate around the optimal cut-off of RUDAS. ROC curves and bootstrapped analyses were made using the pROC package in R version 4.03 (R Core Team (2020). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/).
Results
Participant characteristics are given in . The final sample (N = 43) included more women (N = 23) than men (N = 20). The median age was 74 years, with the youngest being 65 years and the oldest 85 years. The majority were community-dwelling, with only five living in a retirement home. Only 5% had not finished primary school. Nearly half had completed post-primary school. The median number of drugs dispensed was four and, the median number of diagnoses was two.
Table 1. Participant demographic data overall and by each geographical location. City: Nuuk; town: Qaqortoq; small town: Narsaq
illustrates the association between test results using RUDAS and Mini-Cog (left panel) and the association between RUDAS and ADL/gADL (right panel). Mini-Cog and RUDAS scores were associated (rs = 0.65, p < 0.001). Participants with scores of three or less using Mini-Cog were likely to have 23 or lower total scores using RUDAS (p = 0.001). Moreover, independence, as per the ADL/gADL, was associated with scores above 23 on the RUDAS (p = 0.004), with 25 (58.1%) of participants being both independent and having a RUDAS score above 23, while 8 (18.6%) having a score of 23 or less and being classified as dependent. RUDAS scores were associated with age (rs = −0.40, p = 0.0074), but not education (test statistic 0.52, p > 0.10). Mini-Cog scores were not associated with age (rho −0.26, p = 0.09) or education (test statistic 0.76, p > 0.10).
Performance of the tests to discriminate cognitive impairment is illustrated in the ROC curves in . The smoothed AUC is 0.87 (95%-CI, 0.65–0.95) for Mini-Cog and 0.90 (95%-CI, 0.76–0.97) for RUDAS.
shows the sensitivity and specificity to discriminate dementia cases using different RUDAS cut-offs. RUDAS has a sensitivity of 100% and specificity of 75.7%, with a cut-off at the statistically optimal level of 23.
Table 2. Sensitivity and specificity of RUDAS at different cut-offs for detecting cognitive impairment among participants with a recorded diagnosis of dementia versus controls
shows the sensitivity and specificity of the Mini-Cog to discriminate dementia cases and to discriminate participant’s cognitive performance with scores below and above the optimal RUDAS cut-off using different Mini-Cog cut-off levels. The optimal cut-off for Mini-Cog to discriminate dementia cases was ≤2, while it was ≤3 to detect a RUDAS score of ≤23. Further, the AUC of Mini-Cog to detect a RUDAS score at ≤23 RUDAS was 0.86 (95% CI: 0.75–0.96).
Table 3. Mini-Cog’s sensitivity and specificity at different cut-offs for detecting cognitive impairment among participants with a recorded diagnosis of dementia versus controls and a RUDAS score below or equal to 23
Discussion
We translated two tools for assessing dementia through a five-step translation process, and we modified ADL to be applied in a Greenlandic setting. Furthermore, we validate the tools for work-up of impaired cognitive function and dementia in three different locations in Greenland. This is the first translation and validation of these two widely used tools for dementia screening among older adults in Greenland. We found that both tools were applicable in the settings intended, and apathway for work-up of cognitive impairment can be constructed.
We found an association between tools, and both were useful, as documented by a smoothed AUC of 0.87 for Mini-Cog and 0.90 for RUDAS. We calculated smoothed AUC because of the limited number of cases and were similar to the non-smoothed AUC of 0.86 for Mini-Cog and 0.93 for RUDAS. Therefore, AUC values suggest excellent and outstanding performance as interpreted according to Hosmer and Lemeshow’s classification (0.7–0.8/0.8–0.9/>0.9 acceptable/excellent/outstanding discrimination) [Citation14].
Mini-Cog is useful in a health care centre. A cut-off at ≤2 is suggested when screening for dementia, but if greater sensitivity is desired, a cut-off at ≤3 may be recommended [Citation10]. Based on our results, we suggest using a cut-off at ≤3. Cases were detected with a higher specificity using a cut-off at ≤2. However, we aim for higher sensitivity in the Mini-Cog, and the cut-off at ≤3 was superior for discriminating low RUDAS scores as recommended [Citation8–10]. This is also illustrated by the individual data presented in , left panel.
The original validation study of RUDAS suggests that the score is not influenced by gender, preferred language, or education [Citation11]. However, some studies reported an effect of education on RUDAS scores [Citation15–19]. In our study, education was not associated with RUDAS score irrespective of the cut-off value.
The original RUDAS study with a cut-off of 23 had sensitivity and specificity of 89% and 98% [Citation11,Citation12]. A systematic review and meta-analysis [Citation20] showed that the performance of RUDAS varied with cut-off values and between studies. As evaluated from the Youden index, our data suggest a cut-off at ≤23 for detecting cognitive impairment, supported by best-combined sensitivity and specificity at 100% and 75.7%, respectively. Specific requirements for sensitivity and specificity may influence choices for cut-off values that overrule the calculated cut-off for optimal performance. However, we consider the sensitivity and specificity supported by cut-offs calculated from our population to be helpful.
Direct ADL assessment can be performed in the national hospital, where there is a fully equipped kitchen. In other settings in Greenland, the facilities are limited. The gADL in rural Greenland is performed in the consultation room by demonstrating basic housekeeping procedures. This causes variations and uncertainty in evaluations of ADL, and it is relevant to develop a gADL.
Brislin’s model for translating and back-translating [Citation21,Citation22] is a well-known and much-used method of preparing valid and reliable cross-cultural research tools. According to this model, one bilingual translator will translate from the source language to the target language. The second bilingual translator conducts a back-translation while being blinded to the original versions. Back translated, and the original version is then compared. Suppose there is an error in the meanings in comparison, the terms will be re-translated, and a third bilingual translator will perform a back-translation. This process is repeated until no error in meaning occurs. A new bilingual translator should be used for every iteration. Our method differed slightly to accommodate the available linguistic resources. However, this is considered acceptable as there is no gold standard [Citation23–26]. The way we reviewed Greenlandic (1) and Greenlandic (2) was different from Brislin’s model, and we did a back-translation after re-translation from the target language. We also used bilingual translator no. 2 twice, instead of a third bilingual translator for back translations as translator resources are limited.
Mini-Cog is not validated in Danish, so we used the English version as the source version. RUDAS is translated and validated for Danish memory clinics, and we used the Danish version as the source version. The translation is strengthened by the fact that all four, who had been involved in the translation process, are trilingual and fluent in Greenlandic, Danish, and English. We did not make any change in the structure or the format of any items in the tools. Interestingly, the clock-drawing test was considered useful in a Greenlandic setting, and that also the three words for recall could be translated for valid use in Greenlandic. This may be due to the universal themes of family, food, housing, nature, and geography used for recall in the Mini-Cog. However, these components should be evaluated in a validation study in another sample of the population.
It is a major limitation that we only have six cases, among which we have no information on the work-up of the dementia diagnosis. Among the six cases, three had a dementia diagnosis in their electronic healthcare record, while all six had the diagnosis recorded at the nursing home. Due to this limitation, we could not be confident that a Mini-Cog cut-off at ≤2 in the small-town setting would be sufficiently sensitive to detect all actual dementia cases. To accommodate this uncertainty, we chose to analyse the ability of Mini-Cog to detect poor performance on RUDAS. This analysis led us to suggest a cut-off at ≤3 for Mini-Cog.
We did not perform power calculations but rather followed recommendations for simple choices based on cost and feasibility [Citation27]. The sparse and scattered populations in the Arctic may necessitate such an approach in Arctic health research.
The limited sample size prevents a detailed analysis of the influence of age on the performance of the two tests. This is a topic for future evaluation among the growing group of older subjects in Greenland. Moreover, the scheme for work-up needs to be validated in another sample of the population to validate classification performance. Such cross-validation should be performed in a future study.
A decision on a work-up scheme for cognitive impairment in Greenland needs to consider both geography and resources at the different health care facilities. With this in mind, we performed clinical and statistical evaluations on the translated tools to support the work-up of cognitive function among Greenlanders. We thus propose a diagnostic pathway as illustrated in . This is based on a simple test in a health care centre, a more advanced test at the regional hospital, and cut-offs for referral for the next step in cognitive function work-up at the national hospital in Nuuk. This supports that only relevant cases are referred to the national hospital for a full work-up of cognitive function.
Conclusion
Much needed and requested tools have been translated for the assessment of cognitive function among Greenlanders. A new national dementia diagnostic pathway, using tools we have translated and validated, is being proposed for Greenland, taking into account the geographical constraints, the health care resources, and local facilities. This scheme proposes that small town (with a health care centre) residents with a Mini-Cog score of 3 or lower should be referred to a regional hospital for RUDAS and gADL. A RUDAS score of 23 or less and gADL suggesting dependency should lead to work-up at the national referral hospital. Adding clinical judgement and non-invasive methods are likely to support higher classification performance. We suggest including clinical judgement and information from the caregiver when deciding who should be referred. Finally, we recommend validation in a different subgroup of the population and monitoring and evaluating the outcomes when implementing the tools and the algorithm proposed.
Availability of data and materials
The translated tools are readily available in the supplement, while the dataset with individual patients used during the current study is based on a small population, and hence there are constraints on availability for ethical reasons.
Acknowledgments
We would like to thank the staff and residents in Nuuk, Qaqortoq, and Narsaq, Greenland, for their helpful participation.
Disclosure statement
The authors declare that they have no competing interests.
Additional information
Funding
References
- Soriano RP,Depression, Dementia, and Delirium. In: Fundamentals of geriatric medicine. A case based approach. New York, NY: Springer; 2007.
- Burns A, Iliffe S. Dementia. BMJ. 2009;338:b75.
- Statistikbanken. Befolkningen pr 1. januar 1977-2020 (National Statistics for the Population of Greenland). January 2021]; Available from: https://bank.stat.gl/pxweb/da/Greenland/Greenland__BE__BE01__BE0120/BEXST1.PX/table/tableViewLayout1.
- Departementet_for_Sundhed. Demensredegørelse (The challenge of dementia in Greenland). 2012. Dec 2020]; Available from: https://www.peqqik.gl/Footerpages/Publikationer/Rapporter.
- Departementet_for_Sundhed_og_Infrastruktur. Forslag til demensplan (Proposal for improved dementia care in Greenland). 2013 Dec 2020]; Available from: https://naalakkersuisut.gl/da/Publikationer/2013.
- Government_of_Greenland. Facts about Greenland Jan 2021]; Available from: https://naalakkersuisut.gl/en/About-government-of-greenland/About-Greenland/Facts-about-Greenland.
- Tvermosegaard M, Rønn PF, Pedersen ML, et al. Validation of cardiovascular diagnoses in the Greenlandic hospital discharge register for epidemiological use. Int J Circumpolar Health. 2018;77(1):1422668.
- Borson S, Scanlan J, Brush M, et al. The mini-cog: a cognitive ‘vital signs’ measure for dementia screening in multi-lingual elderly. Int J Geriatr Psychiatry. 2000;15(11):1021–8.
- Scanlan J, Borson S. The Mini-Cog: receiver operating characteristics with expert and naïve raters. Int J Geriatr Psychiatry. 2001;16(2):216–222.
- Standardized Mini-Cog© Instrument. January 2021. https://mini-cog.com/mini-cog-instrument/standardized-mini-cog-instrument.
- Storey JE, Rowland JTJ, Conforti DA, et al. The Rowland Universal Dementia Assessment Scale (RUDAS): a multicultural cognitive assessment scale. Int Psychogeriatr. 2004;16(1):13–31.
- Rowland JT, Basic D, Storey JE, et al. The Rowland Universal Dementia Assessment Scale (RUDAS) and the Folstein MMSE in a multicultural cohort of elderly persons. Int Psychogeriatr. 2006;18(1):111–120.
- Nielsen TR, Andersen BB, Gottrup H, et al. Validation of the Rowland Universal Dementia Assessment Scale for multicultural screening in Danish memory clinics. Dement Geriatr Cogn Disord. 2013;36(5–6):354–362.
- Hosmer DW, Lemeshow S. Applied logistic regression. Second ed. A Wiley-Interscience Publication, New York; 2000. p. 156–164.
- Iype T, Ajitha BK, Antony P, et al. Usefulness of the Rowland Universal Dementia Assessment scale in South India. J Neurol Neurosurg Psychiatry. 2006;77(4):513–514.
- Limpawattana P, Tiamkao S, Sawanyawisuth K. The performance of the Rowland Universal Dementia Assessment Scale (RUDAS) for cognitive screening in a geriatric outpatient setting. Aging Clin Exp Res. 2012;24(5):495–500.
- Nielsen TR, VOGEL A, GADE A, et al. Cognitive testing in non-demented Turkish immigrants--comparison of the RUDAS and the MMSE. Scand J Psychol. 2012;53(6):455–460.
- Chaaya M, Phung TKT, El Asmar K, et al. Validation of the Arabic Rowland Universal Dementia Assessment Scale (A-RUDAS) in elderly with mild and moderate dementia. Aging Ment Health. 2016;20(8):880–887.
- Nielsen TR, Segers K, Vanderaspoilden V, et al. Validation of the Rowland Universal Dementia Assessment Scale (RUDAS) in a multicultural sample across five Western European countries: diagnostic accuracy and normative data. Int Psychogeriatr. 2019;31(2):287–296.
- Nielsen TR, Jørgensen K. Cross-cultural dementia screening using the Rowland Universal Dementia Assessment Scale: a systematic review and meta-analysis. Int Psychogeriatr. 2020;32(9):1031–1044.
- Brislin RW. Back-translation for cross-cultural research. J Cross-Cult Psychol. 1970;1(3):185–216.
- Brislin RW. The wording and translation of research instruments. In field methods in Cross-Cultural research. Vol. 8. Lonner WJ, Berry JW, ed.. Sage Publications, California, USA; 1986.
- Jones PS, Lee JW, Phillips LR, et al. An adaptation of Brislin’s translation model for cross-cultural research. Nurs Res. 2001;50(5):300–304.
- Cha ES, Kim KH, Erlen JA. Translation of scales in cross-cultural research: issues and techniques. J Adv Nurs. 2007;58(4):386–395.
- Sousa VD, Rojjanasrirat W. Translation, adaptation and validation of instruments or scales for use in cross-cultural health care research: a clear and user-friendly guideline. J Eval Clin Pract. 2011;17(2):268–274.
- Maneesriwongul W, Dixon JK. Instrument translation process: a methods review. J Adv Nurs. 2004;48(2):175–186.
- Bacchetti P. Current sample size conventions: flaws, harms, and alternatives. BMC Med. 2010;8(1):17.