Abstract
Aim: This quasi-experimental study explored application of the self-efficacy theory in improving self-efficacy, communication skills and patient satisfaction among medical interns. Methods: This study was conducted among 70 medical intern students. Being selected by human judgment and homogenous sampling method, participants were assigned into control and intervention groups. Participants in the invention group received an e-book, two one-on-one training sessions and feedback on their shared experiences in group discussions by peers. The Kirkpatrick model was applied to evaluate the intervention. Participants’ knowledge, self-efficacy and communication skills as well as their patients’ satisfaction were assessed. Data from self and observational assessments were compared in and between groups at different time-points. Results: Participants’ knowledge, self-efficacy and communication skills as well as their patients’ satisfaction were improved significantly in the intervention group compared to that of the control group. Correlation coefficient between interns’ self-efficacy and communication skills scores was 0.74 (P = 0.03). Conclusions: Application of self-efficacy theory could improve medical interns’ communication knowledge, self-efficacy and skills leading to patient satisfaction.
PUBLIC INTEREST STATEMENT
Nowadays, despite many invaluable trainings in the field of communication skills, patient dissatisfaction arising from physicians’ poor communication skills is the leading reason for patients’ complaints. So, it seems that something more than communication skills training is necessary to enhance patients’ satisfaction. This article describes the impacts of a one-on-one training based on improving medical interns’ belief in their capacity to successfully communicate with patient and consequently yield their patients’ satisfaction. Based on the data collected over 4 months, both medical students’ communication skills and their patients’ satisfaction were increased. Understanding these impacts, teachers of medical sciences can observe students’ communication with patients and discuss their beliefs in effectively doing this job. Consequently, their students (as the future health care providers) will effectively communicate with patients and their patients’ satisfaction will be increased.
1. Introduction
Over the past decades, effective patient communication has been one of the main priorities in medical education. Despite global efforts to teach and evaluate patient–physician communication skills (Al Odhayani & Ratnapalan, Citation2011; Back, Arnold, Tulsky, Baile, & Fryer-Edwards, Citation2003; Fryer-Edwards et al., Citation2006), patient dissatisfaction stemming from poor communication skills is the leading reason for patients’ complaints (Montini, Noble, & Stelfox, Citation2008).
Theory-driven research and analysis of physicians’ communication skills can discover reasons for failures in learning and teaching patient–physician communication skills (Sharma, Citation2015). Precisely, theory-driven studies identify predictors of doctors’ communication skills (Ghaffarifar, Ghofranipour, et al., Citation2015a). For instance, our previous studies using the PRECEDE PROCEED (Predisposing, Reinforcing and Enabling Constructs in Educational Diagnosis and Evaluation/ Policy, Regulatory, and Organizational Constructs in Educational and Environmental Development) model (Green & Kreuter, Citation2005) and social cognitive theory (Sharma, Citation2016) revealed that communication knowledge and self-efficacy are instrumental predictors of communication skills among medical interns (Ghaffarifar et al., Citation2015b).
Self-efficacy perception is an individual’s belief in her/his capability in successfully performing a task (Sharma, Citation2016). Considering the controversial relationship among self-efficacy, performance, and substantial “within-group heterogeneity of individual correlations”, conducting future theory-driven research is recommended (Honicke & Broadbent, Citation2016). Based on self-efficacy theory, feeling efficacy, one’s belief in one’s capacity in successfully performing a task (Bandura, Citation2006), is affected by the following four factors namely mastery experiences, observational learning, verbal persuasion, as well as physical and emotional states (Bandura, Citation2006).
Research on the effectiveness of theory-based interventions on physicians and medical students’ self-efficacy in communication skills is very limited.
This study is an attempt to fill this gap by assessing the effect of a self-efficacy theory-driven educational intervention on self-efficacy and communication skills among medical interns. This study also assessed patients’ satisfaction with interns’ communication skills as the outcome measure of our intervention.
2. Methods
This quasi-experimental study (field research) was conducted from February 2016 to May 2016 at a teaching and treatment center affiliated with Tehran University of Medical Sciences (TUMS). Tarbiat Modares University ethics review board approved conducting this study, (IRCT2013021812511N1).
2.1. Setting
This study took place at the Shariati teaching and treatment center as a real-practice setting of interns.
2.2. Study population and participants
Each year, about 180 students, graduated from high school, start studying medicine at TUMS. They pass a three-credit course on patient–physician relationship in their third year of study and during their last 18 months of their 7-year education. They spend their internship at different teaching hospitals affiliated with TUMS. Among those 180 interns, those who were practicing at Shariati teaching hospital were invited to participate in this study. Other inclusion criteria were willing to participate, not having any kind of disability to affect their relationship with patients, and not already participating in any self-efficacy focused training course.
Guest and visiting interns who had completed their medical education at other universities and were temporarily transferred to TUMS were excluded. Given that satisfaction assessment of in-patients at pediatrics, neurology, emergency, and surgery wards was not possible because of their special clinical conditions, interns practicing at those wards were excluded as well.
2.3. Sample
Human judgment and homogenous sampling was used to select participants. Human judgment refers to the nonprobability samples, “whom the investigator judges to be typical of individuals possessing a given trait” (Cottrell & McKenzie, Citation2010). Given this point, interns were chosen by homogenous sampling because they had some unique common characteristics, which are described in study population and participants section. Sample size was determined using PS: Power and Sample Size Calculation 3.1.With a standard deviation = 3 and the true difference in the experimental and control means = 5 from a pilot study, as well as considering confidence interval (CI) = 95% and power = 90%, 31 experimental subjects and 31 control subjects were needed. Considering about 15% of the probability of dropping the samples, 35 interns were assigned to each of the control (A) or experimental (B) groups.
2.4. Intervention
The main goal of the intervention in this study was to increase interns’ knowledge and self-efficacy level and consequently improve their communication skills. This goal came from the findings of a previous study, in which “knowledge and self-efficacy were the two most important predictors of interns’ successful patient–physician relationship and together explained about 23% of the changes in interns’ patient–physician communication behavior. Moreover, 53% of the changes in interns’ self-efficacy were attributed to the changes in their knowledge (Ghaffarifar et al., Citation2015b).”
The educational package for interns in the intervention group included an e-book, observational assessment, feedback from observer in two one-on-one training sessions, group discussion, and peer feedback. Details for each part of the intervention are as follows.
First, a 60-page e-book, which was specifically written for participants of the current study by the research team, was delivered to the interns in group B. The e-book focused on patient–physician relationship, communication skills as in CC guide (Amin & Eng, Citation2003), and ways to increase self-efficacy (Sharma, Citation2016). Interns in group B were given two weeks to study the book. Subsequently, their communication with at least three of their patients was observed in two different sessions by an independent researcher, and constructive feedback was provided to them. A group discussion was then organized to the interns in group B by the main researcher (SGH). They were asked to share their learned experiences with their peers and provide supportive and constructive feedback to one another’s experiences. Five different group discussions were facilitated by SGH. Details for each training session are summarized in Table .
Table 1. Details of each of the training sessions to increase the knowledge and self-efficacy of the interns in communicating with their patients (35 interns*)
2.5. Evaluation of the intervention and data analysis
The modified version of the Kirkpatrick model (Cleland & Durning, Citation2015) was applied to evaluate the intervention. Interns’ demographic characteristics, as well as their knowledge, self-efficacy, communication skills, and patients’ satisfaction with their communication skills, were assessed using valid and reliable questionnaires.
The rate for achievement of educational objectives of each one-on-one training session (Table ) was evaluated through an observational assessment by an independent researcher at the end of each session.
Research questionnaires to assess interns’ knowledge and self-efficacy were validated in the previous part of this research. Knowledge and self-efficacy assessment questionnaires (based on a 5-point Likert scale) included 11 and 12 items, respectively (Ghaffarifar et al., Citation2015b).
Assuming that interns with high scores of knowledge and self-efficacy have more effective communication with their patients compared with their peers with low scores, that independent researcher assessed communication skills of interns in both groups using a 37-item checklist based on a 5-point Likert scale. The checklist was designed based on the participatory planning emphasized by the PRECEDE PROCEED model, and its items were 37 out of the total 71 communication skills contained in the CC guide. These items were related to the training purposes in this intervention. The checklist was pilot-tested for both comprehensibility and applicability by interns from another medical university. Interns also assessed their communication skills using that checklist.
The correlation coefficient between observer’s overall communication score and interns’ overall self-assessment score was measured.
The content of interns’ reflection about their communication skills was analyzed as well, and the results will be reported in another paper.
Interns rated the usefulness of group discussions, in terms of every objective of the session, using a 5-point Likert scale. Interns in group B also determined their overall satisfaction with the educational intervention using an 11-item self-assessment checklist, which was based on a 4-point Likert scale. Both questionnaires were prepared by the researchers.
Patients’ satisfaction with interns’ communication skills was assessed using the Persian version of the patient satisfaction questionnaire (PVPSQ). PVPSQ was validated in the previous part of this study, and it had acceptable psychometric properties (BMJ Open, 2017). Its full text will be published in International Journal of Health Care Quality Assurance: 39(2), 2019.
Details of the intervention are summarized in Table .
Table 2. Details on the assessment of educational intervention to increase interns’ knowledge and self-efficacy in communicating with patients
All steps of the educational intervention are summarized in Figure .
Figure 1. All steps of the educational intervention to increase interns’* knowledge and self-efficacy about building effective relationship with patients *, with timing of intervention and assessment
At Shariati Teaching and Treatment Centre, affiliated to Tehran University of Medical Sciences (TUMS), 2015
2.6. Statistical analysis
The mean score of interns’ knowledge (ranging from 11 to 55), self-efficacy (ranging from 12 to 60), and their communication skills (ranging from 37 to 185) were compared in the two groups before and after the intervention during four different time points (before, immediately, and two and four weeks after the intervention) by paired samples t-test and one-way ANOVA using SPSS 21.0(SPSS Inc., Chicago, IL, USA). The significance level of every test was set at 0.05. Independent samples t-test was also used to compare the mean scores in the two groups at specific time intervals.
3. Results
Seventy interns participated in this action research and 33 of them received educational intervention. Interns’ demographic characteristics are revealed in Table . As shown in Table , interns in two groups were matched in terms of their demographic characteristics.
Table 3. Baseline characteristics of interns (n = 67) assigned to intervention or control groups. Values are numbers (percentages) unless stated otherwise
Based on the results of the Greenhouse–Geisser test, the mean scores of interns’ knowledge had a linear pattern over time and the difference in scores was statistically significant in group B (Sig.: 0.000). The trend for interns’ self-efficacy score was the same over time. The mean score of interns’ knowledge, self-efficacy and communication skills are compared between two groups before and after the intervention in 4 different time points in Table .
Table 4. Comparison of the mean score of interns’ knowledge, self-efficacy and communication skills at different times in two groups of intervention and control (n = 67)
Pearson correlation coefficient between observer’s overall score and interns’ overall self-assessment score was 0.39 (P = 0.04).
Immediately after group discussion, 54.5% of interns greatly appreciated the other interns’ experiences in communicating with patients. In total, 36.4 of them were also satisfied with the feedback was provided to their experiences. In all, 69.7% of interns were moderately satisfied with the suggestions made by other interns regarding self-efficacy improvement strategies. Interns’ recommendations for enhancing the effectiveness of their relationship with patients were very useful for 60.6% of interns. In total, 93.9% of interns were highly satisfied with group discussions with their peers.
In all, 54.5% of interns in group B were completely and 42.4% of them were partially satisfied with the educational intervention.
Pearson correlation coefficient between student’s self-efficacy score and their communication skills score was 0.74 (P = 0.03)
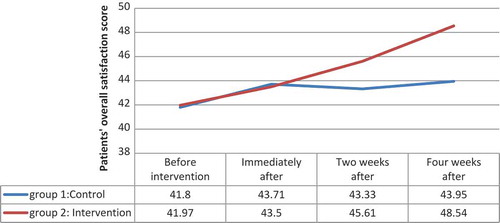
In the pre- intervention stage, 107 patients completed PVPSQ. PVPSQs were completed by 99, 86 and 100 patients immediately, two weeks and 4 weeks after the intervention, respectively. 51.69% of the patients were male and 48.31% of them were female. 64.1% of the patients had not completed their secondary education at school and only 21.7 of them had diploma. The mean of the patients’ satisfaction score in group B, before and 4 weeks after the intervention, was 41.97 ± 15.44 and 48.54 ± 14.22. Pre and post satisfaction scores in group A were 41.8 ± 16.01 and 43.95 ± 14.48.
The changes in the mean score of patients’ satisfaction in both groups are shown in Figure .
4. Discussion
4.1. The educational intervention and its effectiveness
In this field research, a theory-driven educational intervention based on self-efficacy theory was conducted. This intervention, which included written information (e-book), observation, one-on-one training, group discussion, and feedback by the observer and peers, improved interns’ communication with patients. The effectiveness of our educational package was confirmed by an overview of systematic reviews by Berkhof and associates (Berkhof, Van Rijssen, Schellart, Anema, & Van Der Beek, Citation2011).
In our four-week study, providing interns with the opportunity to receive constructive feedback on their practice from both the observer and peers and providing them with the opportunity to reflect on their learning acknowledged the positive role of student-centered programs in achieving enhanced results. According to Gysels et al., the best results are obtained from long-term and learner-centered programs, in which theoretical education is combined with practical training and feedback (Gysels, Richardson, & HigginsonI, Citation2004).
4.2. The impact of the educational intervention on interns’ knowledge and self-efficacy
Interns participating in this study had passed a communication course 3 years before our intervention; however, the mean score of their knowledge in the intervention group significantly increased immediately after the intervention. This finding confirmed that “medical students performed well on examinations and within courses”, but they did not choose to do what they know and what they can do thereafter (Kurtz, Citation2002); thus, continued education should be a requirement in this field.
Immediately after the intervention, subsequent knowledge scores decreased. This downward trend revealed that students were not motivated enough to communicate effectively with patients. Continuous education of students during their studies at medical universities must be arranged because continuity of training and repeated training at reasonable intervals can promote interns’ motivation from the level of reception to the level of response (Gable & Wolf, Citation2012). In line with this inference, the findings of the review by Merckaert, Libert, and Razavi (Citation2005) confirmed that repetition of training at different times is essential for the continuity of communication with patients and maintaining behavioral capabilities. They reported that basic skills related to communication are never learned extemporaneously (Aspegren and LØnberg-Madsen, Citation2005), so the practical training of communication skills and basic communication skills should be the main focus of any future educational program.
Given the above points, our data confirmed two of the research hypotheses. Our findings showed that a theory-driven educational intervention could alter medical interns’ knowledge and self-efficacy about effective communication with their patients. Interns with increased level of knowledge and self-efficacy communicated better with their patients. Similar to our results, participants’ self-efficacy and communication behavior significantly improved after a 7.5 h workshop (Saslaw, Sirota, Jones, Rosenbaum, & Kaplan, Citation2017).
4.3. The causal relationship between interns’ self-efficacy and their communication skills
In this study, interns’ self-efficacy and communication scores were strongly correlated with each other, and the changes in communication skills score were dependent on the changes in their self-efficacy score. Contrary to our findings, in a randomized clinical trial, a 5-day communication teaching course improves physicians and nurses’ self-efficacy, and the changes in self-efficacy are dependent on the changes in communication skills score (Ammentorp et al., Citation2007). Considering these two different causalities, self-efficacy and communication skills are mutually correlated. Doctor Kurtz believes that learning communication skills is related to learners’ self-esteem and self-concept (Kurtz, Citation2002). Our findings revealed that learning communication skills is related to one’s self-efficacy as well. The differences among self-efficacy, self-esteem, and self-concept have been clarified in other studies (Bandura, Citation2006).
4.4. The relationship between self-assessment and observation results
The assessment of interns’ communication skills demonstrated that interns’ self-assessment score and observer’s score were moderately correlated with each other. This moderate correlation indicated that the same framework was used for designing self-assessment and observation tools. The mean of interns’ self-assessment scores was lower than that of the observer’s score at all times. This low self-assessment score indicated that interns did not believe in their capabilities to communicate with patients. Therefore, methods that aim to increase self-efficacy should be regularly taught to medical students. Teaching self-efficacy to medical interns was a good objective for this research.
4.5. The impact of group discussion
The group discussions were highly welcomed by interns in this study. This finding suggests that participatory planning, which is emphasized in theory-driven interventions, such as working with the PRECEDE model (as it was done in this study), increases the chances of success of an intervention. Therefore, group discussion sessions are an integral part of any training program on communication skills training. In addition to enhancing interactions between peers, holding group discussion sessions may enhance the understanding of educational planners of the status quo.
4.6. The impact of the communication-based intervention on patients’ satisfaction
In this study, about 79% of the patients had a diploma, and their satisfaction with interns’ communication skills in group B was average to high (scores ranging from 41 to 49 out of a total of 70) during the various stages of this study. Patients’ high satisfaction scores could be related to their low literacy level. This finding was consistent with the report of a review article, in which the highest degree of satisfaction was reported with patients who had less education than the other patients (Johansson et al., Citation2002).
Immediately and two weeks after the intervention, the mean score of patients’ satisfaction with communication skills of interns in the intervention group increased; however, the difference in patient satisfaction score between groups A and B was not statistically significant. Similarly, in an observational study in 2013, the satisfaction of hospitalized patients was significantly increased 6 months after an 8-h experimental communication skills training. The authors of this study suggested that “longer-term sustainability of such interventions” should be evaluated (Boissy et al., Citation2016).
Communication skills training provided to 80 doctors from 69 cancer centers in England did not have a significant positive effect on patient satisfaction as well (Shilling, Jenkins, & Fallowfield, Citation2003). These findings suggest that increasing patient satisfaction requires long-term interventions.
4.7. Threats to internal validity and steps were taken to control some extraneous variables
To decrease history effect, the interval between pre- and post-assessment was short. During the 4-week period of study, neither major events nor minor disruptive factors occurred.
To lessen maturation threat, participants in the control and intervention groups were recruited from the same department. Thus, the probability of any maturation was almost the same for the participants in both groups.
To decrease instrumentation threat, the assessment tool was the same at all four stages of the study. All stages involved only one observer, and the feedback to all the interns was given only by her.
Selection bias could be a serious threat to internal validity in this study because assignments were not random, and interns voluntarily assigned to both the intervention and control groups. Interns who volunteered to participate in the intervention group might have been more inclined to learn about self-efficacy, and such a high inclination could have intensified the positive outcomes of the intervention. Although the variables in the two groups were not significantly different at the beginning of the study, the difference in participants’ willingness to learn in both groups can be assessed in future studies.
The mere familiarity of the interns with the topic of self-efficacy was likely to sensitize and encourage them to learn about it. For this reason and to lessen testing effect, future studies should measure interns’ sensitivity to learning self-efficacy at the beginning of the study.
5. Limitations
Our study had some limitations. It was conducted in a single center (TUMS) over a 4-month period. We assumed that it is better to assess the impact of self-efficacy training at a medical school, in which medical students had previous formal credit-based education. To the best of our knowledge, until the time of this study, among all Iranian universities, only TUMS had the above criterion and we had to conduct our study in that single center.
Moreover, given the time-consuming data collection technique and limited resources, conducting the present study with a large sample size was not possible.
Although on the basis of the central limit theorem (Heyde, Citation2006), normal distribution of pre-test scores confirmed that our sample size was enough to make a decision about the effectiveness of our training intervention, it is recommended to continue this study over a longer period with multiple cohorts, multiple centers/ institutions, interdisciplinary samples over a prolonged period.
6. Conclusion
In this research, participatory planned theory-driven educational intervention, including an educational e-book, one-on-one training after observational assessments, observers’ feedback, group discussions followed by interns’ reflection, and peers’ constructive feedback, led to a significant increase in interns’ knowledge, self-efficacy, and communication skills and patients’ satisfaction in the intervention group. Considering that the difference in-patients’ satisfaction between the intervention and control groups was not statistically significant, learning, maintaining, and enhancing communication should be a lifelong task.
Competing interests
The authors declare no competing interests.
Acknowledgements
The authors would like to express their gratitude to all medical interns, who participated in this study, for dedication of their invaluable time and experiences.
Additional information
Funding
Notes on contributors
Fazlollah Ghofranipour
Fazlollah Ghofranipour, MScN, PhD. Professor of Health Education. At the time of this study, he was the director of the Health Education department at Tarbiat Modares University.
Saeideh Ghaffarifar
Saeideh Ghaffarifar is an M.D/Ph.D with a master degree on medical education. Her research activities are mainly focused on patient-physician relationship and theory-driven educational interventions. She is also enthusiastic to conduct exploratory studies.
Fazlollah Ahmadi
Fazlollah Ahmadi, MScN, PhD. Professor of Nursing Education. At the time of the present study, he was the education vice at school of Medical Sciences at Tarbiat Modares University.
Hassan Hosseinzadeh
Hassan Hosseinzadeh, PhD of Health Education. At the time of the present study, he was the senior lecturer and academic program director of Health Promotion at School of Health & Society, University of Wollongong NSW, Australia.
Amirhossein Akbarzadeh
Amirhossein Akbarzadeh, Medical student. At the time of this study, he was a master student at medical education department at Tabriz University of Medical Sciences
References
- Al Odhayani, A., & Ratnapalan, S. (2011). Teaching communication skills. Canadian Family Physician Medecin De Famille Canadien, 57, 1216–1218.
- Amin, Z., & Eng, K. H. (2003). Basics in medical education. Singapore: World Scientific.
- Ammentorp, J., Sabroe, S., Kofoed, P., & Mainz, J. (2007). The effect of training in communication skills on medical doctors’ and nurses’ self-efficacy: A randomized controlled trial. Patient Education and Counseling, 66, 270–277. doi:10.1016/j.pec.2006.12.001
- Aspegren, K., & Lonberg- Madsen, P. (2005). Which basic communication skills in medicine are learnt spontaneously and which need to be taught and trained? Medical Teacher, 27, 539–543. doi:10.1080/01421590500136501
- Back, A. L., Arnold, R. M., Tulsky, J. A., Baile, W. F., & Fryer-Edwards, K. A. (2003). Teaching communication skills to medical oncology fellows. Journal of Clinical Oncology, 21, 2433–2436. doi:10.1200/JCO.2003.09.073
- Bandura, A. (2006). Guide for constructing self-efficacy scales. Self-Efficacy Beliefs of Adolescents, 5,307–310.
- Berkhof, M., Van Rijssen, H. J., Schellart, A. J., Anema, J. R., & Van Der Beek, A. J. (2011). Effective training strategies for teaching communication skills to physicians: An overview of systematic reviews. Patient Education and Counseling, 84, 152–162. doi:10.1016/j.pec.2010.06.010
- Boissy, A., Windover, A. K., Bokar, D., Karafa, M., Neuendorf, K., Frankel, R. M., … Rothberg, M. B. (2016). Communication skills training for physicians improves patient satisfaction. Journal of General Internal Medicine, 31(7), 755–761. doi:10.1007/s11606-016-3597-2
- Cleland, J., & Durning, S. J. (2015). Researching medical education. John Wiley & Sons, New Jersy, USA.
- Cottrell, R. R., & McKenzie, J. F. (2010). Health promotion and education research methods: Using the five-chapter thesis/dissertation model (2nd ed.). Jones & Bartlett Publishers, Canada, Mississauga, Ontario.
- Fryer-Edwards, K., Arnold, R. M., Baile, W., Tulsky, J. A., Petracca, F., & Back, A. (2006). Reflective teaching practices: An approach to teaching communication skills in a small-group setting. Academic Medicine : Journal of the Association of American Medical Colleges, 81, 638–644. doi:10.1097/01.ACM.0000232414.43142.45
- Gable, R. K., & Wolf, M. B. (2012). Instrument development in the affective domain: Measuring attitudes and values in corporate and school settings. Springer Science & Business Media, Berlin/ Heidelberg, Germany.
- Ghaffarifar, S, Ghofranipour, F, Ahmadi, F, & Khoshbaten, M. (2015a). Why educators should apply theories and models of health education and health promotion to teach communication skills to nursing and medical students. Nursing Midwifery Studies, 4. doi:10.17795/nms
- Ghaffarifar, S, Ghofranipour, F, Ahmadi, F, Khoshbaten, M, & Sallis, C. (2015b). The causal relationship between interns’ knowledge and self-efficacy and their value in predicting the interns’ communication behavior with patients. International Journal Community Based Nursing Midwifery, 3, 263.
- Green, L. W., & Kreuter, M. W. (2005). Health program planning: An educational and ecological approach. McGraw-Hill Companies, New York, The United States.
- Gysels, M., Richardson, A., & HigginsonI, J. (2004). Communication training for health professionals who care for patients with cancer: A systematic review of effectiveness. Suppor Care Cancer, 12, 692–700. doi:10.1007/s00520-004-0666-6
- Heyde, C. (2006). Central limit theorem. Wiley Stats Ref: Statistics Reference Online. doi:10.1002/9781118445112.stat04559.
- Honicke, T., & Broadbent, J. (2016). The influence of academic self-efficacy on academic performance: A systematic review. Educational Research Review, 17, 63–84. doi:10.1016/j.edurev.2015.11.002
- Johansson, P., Oleni, M., & Fridlund, B. (2002). Patient satisfaction with nursing care in the context of health care: A literature study. Scandinavian Journal of Caring Sciences, 16(4), 337–344. doi:10.1046/j.1471-6712.2002.00094.x
- Kurtz, S. M. (2002). Doctor-patient communication: Principles and practices. The Canadian Journal of Neurological Sciences. Le Journal Canadien Des Sciences Neurologiques, 29, S23–S29.
- Merckaert, I., Libert, Y., & Razavi, D. (2005). Communication skills training in cancer care: Where are we and where are we going? Current Opinion in Oncology, 17, 319–330. doi:10.1097/01.cco.0000167737.72196.f9
- Montini, T., Noble, A. A., & Stelfox, H. T. (2008). Content analysis of patient complaints. International Journal Qualitative Health C, 20, 412–420. doi:10.1093/intqhc/mzn041
- Saslaw, M., Sirota, D. R., Jones, D. P., Rosenbaum, M., & Kaplan, S. (2017). Effects of a hospital-wide physician communication skills training workshop on self-efficacy, attitudes and behavior. Patient Experience Journal, 4, 48–54.
- Sharma, M. (2015). Multi-theory model (MTM) for health behavior change. WebmedCentral Behaviour, 6(9), WMC004982.
- Sharma, M. (2016). Theoretical foundations of health education and health promotion. Jones & Bartlett Publishers, USA.
- Shilling, V., Jenkins, V., & Fallowfield, L. (2003). Factors affecting patient and clinician satisfaction with the clinical consultation: Can communication skills training for clinicians improve satisfaction? Psycho-Oncology, 12, 599–611. doi:10.1002/pon.731