ABSTRACT
In our society, people’s health behaviors are considered a dilemma that can intensify the probability of developing a disease in the future. This study aimed to investigate the association between health risk behaviors and depression among a sample of university students, Karachi, Pakistan. A self-reported health behavior questionnaire was distributed to 813 consented students. The Center for Epidemiological Studies-Depression (CES-D-10) questionnaire was used, a short, self-report scale that measures the recent level of depressive symptomatology, primarily focusing on depressed mood. Their results were further compared with some important health behaviors and social activities. At the univariate stage, the chi-square test was executed to compare the characteristics of categorical variables with depression status. The effect size was measured in terms of the odds ratio (OR) using logistic regression models. According to the adopted classification of CES-D, one out of eight students were found to be depressed. Among students’, females were found to be 70% more depressed than males (OR: 1.7, 95% CI: 0.9–3.0). Depression was higher among students who were not satisfied with their lives, were socially isolated, had trouble sleeping, little control over things, and the future depends on others. The chances of depression were 90% higher among students who did not share private concerns with others (P = 0.01). Overall, depression prevalence was 12.5%, and it was associated with dissatisfaction with life, social isolation, insomnia, and others. Female students were found to be more depressed compared to males.
PUBLIC INTEREST STATEMENT
Health behavior refers to a group of activities required to maintain or regain good health. ‘Health risk behaviors’ are factors like sedentary lifestyle, eating disorders, alcohol/drug abuse, early onset of sexual activity or unsafe sexual practices and antisocial behaviors which have a negative impact on health and contribute to social and psychological problems like depression. We observed that depression (12.5% prevalence) was associated with dissatisfaction with life, social isolation and insomnia. It was less existent amongst the students who were socially interactive, satisfied with their lives, involved in essential activities, planned for their future happenings and enjoyed a sound sleep. We therefore encourage all students to manage stress by a positive attitude, healthy diet, physical activity, social interaction, and good sound sleep. We recommend to have a culture with support systems, recreational and effective counselling services for all students to avoid stress, depression and resultant psychological problems emerging into mental health disorders.
1. Introduction
Health behavior is the activity undertaken by people to uphold or improve their health, avoid health problems, or achieve a positive body image (Cockerham, Citation2014. Globally, we are facing various types of health risks behaviors, like lack of physical activity, diet-related issues, obesity, stress, sleep disturbance, unsafe sexual practices, smoking, and increased alcohol consumption. The health behaviors may be divided into “health-enhancing” and “health impairing.” Here the health-enhancing category activities include exercise, maintaining a diet plan, avoiding drugs like alcohol, and using protection in sexual contacts to prevent sexually transmitted diseases (STDs). While health-impairing activities are those, which bring harm to health like smoking, alcohol consumption, avoid exercising, improper diet, and unprotected sexual engagement (Conner, Citation2002; Fragelli & Günther, Citation2012). The positive health behaviors and healthy lifestyle like regular exercise, consumption of more fruit and vegetables, proper dental care, use of good fat, involvement in healthy social activities, avoid the use of tobacco and alcohol can help us to prevent physical and mental ailments (Peltzer et al., Citation2016). In this modern era, life expectancy can be increased by promoting public awareness about health issues and providing a better quality of health facilities. The endeavor of edification regarding health can help us to reduce morbidity and mortality.
Depression has been declared one of the highest-burden illnesses for individuals, families, and society (Organization, Citation2002), affecting about 322 million people globally. According to a report, depression would become a leading cause of morbidity along with HIV/AIDS and coronary heart disease by the year 2030 (Mathers, C.D.; Loncar, D., 2006). Depression is a mental state or a psychiatric mood disorder that affects multiple aspects of an individual’s life, including his/her cognition, emotions, feelings, sleep, appetite, weight loss or gain, and lack of interest in carrying out daily life activities, and suicidal thoughts.
Several studies have reported the prevalence of depression and health behaviors, but there is a lack of data about this important topic in our country. Therefore, the current study aimed to investigate the association between health behaviors and depression among university students of Karachi, Pakistan, and fill up the research gap in our population.
2. Literature review
Behavioral risk factors including tobacco smoking, alcohol consumption, sedentary lifestyle, obesity, unhealthy diet are the most important determinants of many diseases like hypertension, coronary heart disease, diabetes mellitus, stroke, etc. which are the leading cause of morbidity and mortality (Mokdad et al., Citation2004; Nisar et al., Citation2009, Citation2007; Yusuf et al., Citation2004). Kasl and Cobb (Citation1966) defined three types of health-related behavior. First is the health behavior that is aimed at preventing disease (for example, eating a healthy diet), second is the illness behavior that is aimed at seeking remedy (for example, visiting the doctor) and third is the sick role behavior that is aimed at getting well (for example, taking prescribed medicine or rest). However, on the other hand, health risk behaviors lead to unhealthy outcomes. Matarazzo and Herman (Citation1984) described the health behaviors by using two terms; “behavioral pathogens,” which means health impairing habits, such as smoking or eating a high-fat diet. The other term is “behavioral immunogens,” which means health-protective behaviors, such as attending a health checkup. Depression is typically presented with a combination of low mood, loss of interest in daily activities, feelings of guilt, low self-esteem and loss of appetite, concentration, and sleep (Ryder et al., Citation2002). In spite of a number of culture-related differences in its presentation, the association with cognitive symptoms as well as the disturbance in the social development of an individual leading to alcohol and drug abuse have been observed with depression (Kessler et al., Citation1997). A WHO report indicated that by the year 2030, depression would be the second-most common cause of disability globally (Reddy, Citation2010).
Depression is more prevalent in university students than in the general population (Ibrahim et al., Citation2013). Several studies indicated that depressive symptoms are common among students ranging from 5% to 40% (Othieno et al., Citation2014; Youssef, 2016; Azim & Baig, Citation2019). Numerous factors have been reported to be associated with depression among university students like, sleeping problems, and lack of social support (Peltzer et al., Citation2013), increased age or academic year of study (Othieno et al., Citation2014; Youssef, 2016), female gender (Adewuya et al., Citation2006), smoking, lower socioeconomic status (Ibrahim et al., Citation2013), poor academic performance (Othieno et al., Citation2014;Yusoff, 2013), lack of physical activity (Taliaferro et al., Citation2009), excessive weight or obesity (Reeves et al., Citation2008). The association of depression is also significant among university students from different cities/countries with different backgrounds and cultures. They feel homesickness and social disconnectedness as they are away from their home. They need special attention to keep up their mental health and overcome the challenges they face while living in a new environment (Nguyen & Le, 2019). In a bid to investigate factors that influence an individual’s overall health, research studies have demonstrated that health risk behaviors play an extremely important role (Peltzer et al., Citation2013 &, Citation2016).
Research studies revealed that in Pakistan, the prevalence of anxiety and depressive disorders is about 34% (range for females 29-66% and males 10-33%). Depression is more associated with the female gender, middle age, housewives, low level of education, financial difficulty, and relationship problems (Mirza & Jenkins, 2004). In Pakistan, during the last few decades, due to urbanization and western influence, a rapid increase has been observed in health risk behaviors like fast food consumption, smoking, and physical inactivity. About 9.6% of the young population live a sedentary lifestyle, and 29.5% eat fast food (Mushtaq et al., 2011), 29.4% consume soft drinks regularly (Ishaque et al., 2012), 6.3% smoke cigarettes, and 9.8% use tobacco (Organization, Citation2002). Mental health issues and physical abuse are also significantly prevalent in our society (Mirza & Jenkins, 2004; Sabir & Zaman, Citation2013). There is a lack of health awareness in Pakistan that leads to an unhealthy lifestyle, which is the root cause of many serious illnesses. This study investigates the health risk issues in our sample population and relates them to a significant problem of our society that is depression.
3. Experimental procedure and summary statistics methods
3.1. Sample
The present study was accomplished in 2013-14 in Karachi. An anonymous, self-reported questionnaire was distributed to 813 students after taking their consent.
Researchers invited 813 students from different education fields to participate in this study. Questionnaires were distributed to them; however, only 463 students returned the filled questionnaire. The students were selected by convenient sampling technique.
All students were assured about the confidentiality and anonymity of their identification. Ethical Committee of Bahria University Medical and Dental College approved this study (Approval No. ERC01/13). The health questionnaire was adopted from already published studies (Radloff, Citation1977; Steptoe & Wardle, Citation1996).
3.2. Procedure
The questionnaire used for data collection had two parts. Part one was related to demographic information like age, gender, year of study, residence, marital status, studying in a public or private institute, and others. Part two was related to the depression measurement by the Center for Epidemiological Studies-Depression (CES-D) scale. It was comprised of ten questions, and Laurie Radloff designed it in 1977 (Radloff, Citation1977), and it was revised in 2004. It is a short, self-report scale used to measure the recent level of depressive symptomatology, primarily focusing on depressed mood. The items of the scale are designed to rate according to the symptoms associated with depression and identify the individuals at risk for clinical depression or in need of treatment.
4. Statistical methods
Data were analyzed using IBM Statistical Package for Social Sciences (SPSS v. 22. Cronbach’s alpha was computed to check the reliability of the scales. The CES-D scores were measured while adding responses of 10 items in the scale. Students’ acquired a score of 11 or more were classified as depressed (http://scireproject.com). At the univariate stage, the chi-square test was executed to compare the characteristics of categorical variables with depression status. Continuous variables were found skewed using Shapiro-Wilk’s test; hence, the Mann–Whitney U test was run to compare age and metabolic equivalent (MET) score of depressed and non-depressed students. The effect size was measured in terms of the OR using logistic regression models. Variables with a p-value less than 0.1 at the univariate stage were processed for univariable logistic regression, and crude ORs were obtained. Variables that showed a p-value less than 0.25 from the univariable logistic regression model were further included in the multivariable model to obtain an adjusted OR.
5. Results and findings
Among 813 approached students, 463 students returned the completed questionnaires making a response rate of 57.2%. The average age of the students was 20.2±1.6 years. The male-to-female ratio was 1:1.1.
6. Personal information
The value of Cronbach’s alpha for the CES-D scale was 70.2%, showing good consistency in the responses of the students. According to the adopted classification of CES-D, one out of eight students was found to be depressed. There was no significant difference found in the age of the depressed and non-depressed students (P = 0.40). Females were found to be 70% more depressed than males (OR: 1.7, 95% CI: 0.9-3.0). The year of study and MET score also did not significantly affect the depression status of the students (). When students were asked whether they are satisfied with their lives as a whole, 81 (19.6%) were not satisfied, and among them, the proportion of depression was 20.9%. The univariable analysis revealed that depression was 2.2 folds higher among students who were not satisfied with their life.
Table 1. Personal characteristics and status of depression among students
UOR = unadjusted odds ratio, AOR = unadjusted odds ratio
7. The reaction of any upsetting life events
One hundred and seventy-two students divulged that they kept isolating and upsetting while reminding any upsetting events (). The likelihood of being depressed was 2.5 folds higher among such students (OR: 2.5, 95% CI: 1.4-4.3). Nevertheless, involving enjoyable activities was not significantly associated with the depression status of students (P=0.08). A similar finding was observed for the association, feeling of affection for others, and the presence of depression (P=0.16). More than one-sixth (n=178) felt isolated in their life, and such students had a significantly elevated level of depression (OR: 2.6, 95% CI: 1.4-4.6). Ninety-one students thought there was no point in planning for the future, and 20% of them were depressed and had 2.3 times higher chances of being depressed as compared to those who did not refuse planning for the future. Trouble in sleeping was reported by 27.4% (n = 127) students, and one-quarter of them (n=32) were depressed. Trouble sleep caused a 4.1 times higher likelihood to cause depression among students (OR: 4.1, 95% CI: 2.3-7.4). Nearly one-quarter (n = 28) of students were found to get jumpy over ordinary noises, and movements and the likelihood of depression were 3.2 times higher among such students (OR: 3.2, 95% CI: 1.8-5.6).
Table 2. Reaction towards life events and status of depression among students
UOR = unadjusted odds ratio, AOR = unadjusted odds ratio
8. Attitude towards life decisions
Around 40% (n = 183) of students were not much involved in things in their lives, which they considered important. The odds of depression were 2.1 times higher in such students than those involved in important things in life (P = 0.009). The proportion of feeling helpless was significantly higher in our setup (n = 143), and about 19% of them were depressed (P = 0.006). The univariable analysis revealed that the likelihood of depression among such students was 2.2 times higher (OR: 2.2, 95% CI: 1.2-3.8). The odds of depression were 70% and 60% higher among students who had little control over things and had the future depends on others. After adjustment, the item “future only depends on me” occurred as the only significant predictor among attitude towards life decision ().
Table 3. Attitude towards life decisions and status of depression among students
9. Practices in casualties
Ninety students reported that they remained alone during sickness, and only 16% of them were found depressed (P = 0.33). One hundred and thirty-eight did not share private concerns with others, and chances of depression among such students were 90% higher (P = 0.01). Nearly half of the students did not attend religious meetings, and depression was found in 10.4% of such students. Spending time on religious activities was also found insignificantly associated with depression status ().
Table 4. Practices in casualties and status of depression among students
UOR = unadjusted odds ratio
10. Discussion
Mental health is expressed and conceptualized culturally, community, and society-wise. Mental well-being challenges in university students are both short term and long term in terms of career and academic success.
In a set of university students, the frequency of depression was 25% (Zaman, Citation1996). Depression prevalence related to academic stress was 53.43% in a study conducted in 2003 (Ghayas et al., Citation2014), which escalated to 60-70 % in the subsequent years (Inam et al., Citation2003; Khan et al., Citation2006; Rehmani et al., Citation2018).
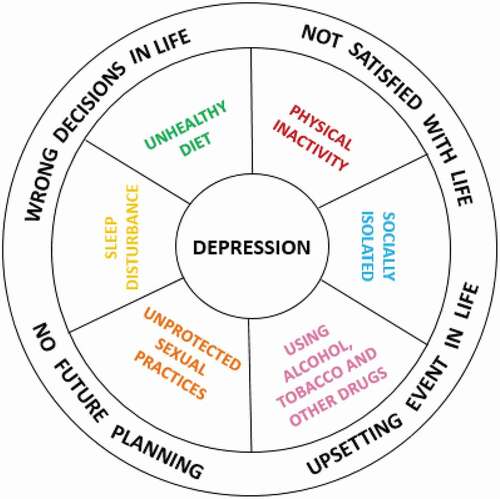
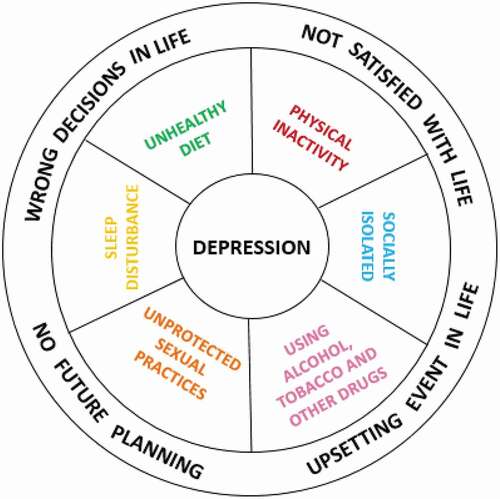
Recent studies reported the prevalence of depression 72% in Karachi’s medical students (Azim & Baig, Citation2019) and 75% in university students at Sialkot, Pakistan (Asif et al., Citation2020). Academic stress, a cut-throat competition to get honors, scholarship competition for board exams, tight schedule without leaves and lack of recreational facilities play a pivotal role in the upsurge of depression and mental health disorders (Rehmani et al., Citation2018). The association between depression and health risk behaviors and its relationship with our study outcomes are shown in . Collectively, we found that peoples’ wrong decisions in life, upsetting events in life, no future planning, and unsatisfied life can lead to developing health risk behaviors, which eventually, sooner or later, can cause depression. Educational institutions may lead to harmful consequences like decreased life satisfaction, depressive moods, poor academic performance, diminished empathy, and reduced competency skills (Haldorsen et al., Citation2014; Rehman, Habib et al., Citation2014). In this cross-sectional study, we observed that one out of eight students were found to be depressed with its preponderance in female students. Depression is likely to impact aspects of cognition, behavior, and attitude of students that affect their daily life activities and society (Gazzaz et al., Citation2018; Schwenk et al., Citation2010). We observed that depression was higher among students’ who were not satisfied with their lives, were socially isolated, had trouble sleeping, little control over things and future depends on others. Studies have identified the prevalence of depression in association with lifestyle habits, sleeping hours, physical activities, recent trauma, and coping mechanisms in Pakistan’s medical students (Alvi et al., Citation2010; Jadoon et al., Citation2010; Kumari et al., Citation2019).
Depression, as declared to be one of the illnesses, was having the highest burden for individuals, families, and society (Organization, Citation2002). The condition is associated with many socio-demographic factors, including age, gender, education, socioeconomic and marital status. We observed higher reporting of depression in females, comparable to another study among the first-year medical students (Basnet et al., Citation2012). Dahlin et al. (Citation2005) reported higher stress levels and advanced depression rates among women than men and the general population.
It is a known fact that human beings are social animals’, and their lives are dependent upon the social network of relationships. Socially isolated people are more prone to poor health conditions due to lack of social connectivity, which contributes to an individual’s overall health state by suggestions from peers (Rehman, Habib et al., Citation2014). It is cited in the literature that social isolation is associated with a lower level of an individual’s physical as well as mental health problems (Chou et al., Citation2011). The chances of depression among students who did not share private concerns with others were 90% higher. The association of social isolation with depression in our study is similar to a study in which a significant prevalence of burnout and depressive symptoms was observed (Youssef, Citation2016). Other health risks associated with social isolation besides depression (Heikkinen & Kauppinen, Citation2004) are infections (Cohen et al., Citation1997) and cognitive decline (Barnes et al., Citation2004). The lack of social contacts can raise the risk of death by at least 50% and, in certain cases, by more than 90% (Holt-Lunstad et al., Citation2010). A study reported that “in campus living” caused depression in medical students (Al-Dubai et al., Citation2011).
Our results demonstrated that depressed students had sleep disorders, which have also been explained in the literature (Luca et al., Citation2013). The finding is supported by a study in which nursing home residents’ mood and quality were improved by their involvement in enjoyable activities (Travers, Citation2017). Studies report that the students use many active coping strategies like positive reframing, planning, and acceptance to withstand stress for psychological problems (Al-Dubai et al., Citation2011; Haldorsen et al., Citation2014; IsHak et al., Citation2013). Social interdependence and social networking helped Karachi’s medical students improve their emotional well-being, overcome stress and emotional outbursts (Katpar et al., Citation2017). These coping strategies enhance life satisfaction that improves subjective well-being (Koivumaa-Honkanen et al., Citation2004). Students who were involved in enjoyable activities were less depressed. We also observed higher depression among students who were not satisfied with their lives that call for the use of coping abilities that can enhance performance and strength to survive episodes of mental stress, depression, and anxiety (Rehman et al., Citation2015).
The absence of prospective planning is a potential susceptibility marker for depression and anxiety in older adults (Vilhauer, Citation2014). The odds of depression in our study were higher among students who had little control over things and had the future depends on others. This demonstrates that learning to build a more optimistic vision about the future, subjects with major depression do better than dwelling on pessimistic feelings regarding their previous experiences. Future studies could investigate the care planning’s impacts on subsequent moods (Sörensen et al., Citation2012).
11. Conclusion
Overall, depression prevalence was 12.5%, and it was associated with dissatisfaction with life, social isolation, insomnia, and others. Moreover, it was less existent amongst the students who were socially interactive, satisfied with their lives, involved in essential activities, planned for their future happenings, and enjoyed a sound sleep. Female students were more depressed as compared to their counterparts. Policies are required to focus on high levels of anxiety in university students. In order to address stress, with healthier eating and sleeping habits, aerobic practices such as athletics and yoga should be encouraged. Students should further be educated with coping strategies and the concept of wellness and spiritual well-being. Teachers can play an inspirational role by enhancing students’ ability to cope with academic problems. These findings suggest an imperative need for preventive measures and interventions to enhance the students’ mental health.
12. Limitations
This study’s findings are based on a self-reported questionnaire with a chance of some reporting bias from students. The authors did not consider students’ place of residence, either they were residing in hostel or day scholar. The study is conducted in a private university, and so the results cannot be generalized. The study is confined to a single university student only, and the prospective study could be carried out with a cohort of various university students to look at the different levels of stress.
13. Recommendations
Culture shapes psychological processes, and this outspreads to depression and psychopathology. We recommend having a culture with support systems for all students plus effective counselling services and mentorship as an integral part of the academic curriculum. Curriculum innovation with break times for exercise, rehabilitation, social activities, event celebration, and music concerts should also be considered. Institutes should plan intervention programs and workshops on stress management, time management, study techniques and coping skills for the identified targeted groups. The policies of financial support through scholarships and remunerations can be proposed and monitored for effective implementation. The recommendations mentioned above can alleviate unnecessary stress and mental health disorders effectively.
Compliance with Ethical Standards Conflict of interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the Ethical Review Committee of Bahria University Medical and Dental College. Permission to carry out the study was granted by Bahria University Medical and Dental College, Karachi (Approval no. ERC01/13)
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Acknowledgements
We are grateful to University of Limpopo, Medunsa Campus, for funding this study and providing financial support for Health Survey in middle-income countries. These funders are not involved in any aspect of the study nor the preparation of this write-up. We are also thankful to Bahria University Medical & Dental College for facilitating in conducting this research.
Data Availability statement
Data are available with the corresponding author upon reasonable request.
Additional information
Funding
Notes on contributors

Rehana Rehman
Dr Rehana Rehman MBBS, MPhil, PhD, FHEA is working as an Associate Professor in the Department of Biological and Biomedical Sciences, Aga Khan University, Karachi, Pakistan. She is involved in teaching of Physiology for the last 20 years in different medical colleges. The interest in medical education has inspired her to develop a synergy between teaching and research and take part in research on teaching and learning methodologies. She leads group of imminent researchers who have worked on better understanding, relevance and application of computer ergonomics, lifestyle trends and complementary alternative medicine. She has also participated in “Health Survey in middle-income countries “organized by University of Limpopo, Medunsa Campus. Dr Rehman has researched all aspects of wellness wheel; physical, mental, social, spiritual, financial, occupational, environmental wellness. Her book “Five minutes to Wellness” is based on holistic review of all dimensions of wellness of medical students.
References
- Adewuya, A. O., Ola, B. A., Aloba, O. O., Mapayi, B. M., & Oginni, O. O. (2006). Depression amongst Nigerian university students. Social Ssychiatry and Psychiatric Epidemiology, 41(8), 674–13. https://doi.org/10.1007/s00127-006-0068-9
- Al-Dubai, S. R., Al-Naggar, R. A., AlShagga, M. A., & Rampal, K. G. (2011). Stress and coping strategies of students in a medical faculty in Malaysia. The Malaysian Journal of Medical Sciences, 18(3), 57–64. https://www.ncbi.nlm.nih.gov/pubmed/22135602
- Alvi, T., Assad, F., Ramzan, M., & Khan, F. A. (2010). Depression, anxiety and their associated factors among medical students. Journal of the College of Physicians and Surgeons--Pakistan : JCPSP, 20(2), 122–126. https://doi.org/10.2010/JCPSP.122126
- Asif, S., Mudassar, A., Shahzad, T. Z., Raouf, M., & Pervaiz, T. (2020). Frequency of depression, anxiety and stress among university students. Pakistan Journal of Medical Sciences, 36(5), 971–976. https://doi.org/10.12669/pjms.36.5.1873
- Azim, S. R., & Baig, M. (2019). Frequency and perceived causes of depression, anxiety and stress among medical students of a private medical institute in Karachi: A mixed method study. JPMA. The Journal of the Pakistan Medical Association, 69(6), 840–845. PMID: 31189292.
- Barnes, L. L., De Leon, C. M., Wilson, R. S., Bienias, J. L., & Evans, D. A. (2004). Social resources and cognitive decline in a population of older African Americans and whites. Neurology, 63(12), 2322–2326. https://doi.org/10.1212/01.WNL.0000147473.04043.B3
- Basnet, B., Jaiswal, M., Adhikari, B., & Shyangwa, P. (2012). Depression among undergraduate medical students. Kathmandu University Medical Journal, 10(3), 56–59. https://doi.org/10.3126/kumj.v10i3.8021
- Chou, K. L., Liang, K., & Sareen, J. (2011). The association between social isolation and DSM-IV mood, anxiety, and substance use disorders. The Journal of Clinical Psychiatry, 72(11), 1468–1476. http://doi.org/10.4088/JCP.10m06019gry
- Cockerham, W. C. (2014). the Wiley Blackwell encyclopedia of health, illness, behavior and society (pp. 764–766). Wiley Online Library.
- Cohen, S., Doyle, W. J., Skoner, D. P., Rabin, B. S., & Gwaltney, J. M. (1997). Socialties and susceptibility to the common cold. Journal of American Medical Association, 277(24), 1940–1944. https://doi.org/10.1001/jama.1997.03540480040036
- Conner, M. 2002. Health behaviors. http://userpage.fu-berlin.de/~schuez/folien/conner [Accessed on 12 July, 2018].
- Dahlin, M., Joneborg, N., & Runeson, B. (2005). Stress and depression among medical students: A cross‐sectional study. Medical Education, 39(6), 594–604. https://doi.org/10.1111/j.1365-2929.2005.02176.x
- Fragelli, T. B. O., & Günther, I. D. A. (2012). Ecological approach to evaluate of preventive behavior: Proposal of an inventory applied to musicians. Per Musi, 25(25), 73–84. https://doi.org/10.1590/S1517-75992012000100007
- Gazzaz, Z. J., Baig, M., BSM, A. A., MMO, A. S., Al Alhendi, A. S., Al-Grad, R. M. S. H., & Qurayshah, M. A. A. (2018). Perceived stress, reasons for and sources of stress among medical students at rabigh medical college, king abdulaziz university, jeddah, Saudi Arabia. BMC Medical Education, 18(1), 29. https://doi.org/10.1186/s12909-018-1133-2
- Ghayas, S., Shamim, S., Anjum, F., & Hussain, M. (2014). Prevalence and severity of depression among undergraduate students in Karachi, Pakistan: A cross sectional study. Tropical Journal of Pharmaceutical Research, 13(10), 1733–1738. https://doi.org/10.4314/tjpr.v13i10.24
- Haldorsen, H., Bak, N. H., Dissing, A., & Petersson, B. (2014). Stress and symptoms of depression among medical students at the University of Copenhagen. Scandinavian Journal of Public Health, 42(1), 89–95. https://doi.org/10.1177/1403494813503055
- Heikkinen, R. L., & Kauppinen, M. (2004). Depressive symptoms in late life: A 10-year follow-up. Archives of Gerontology and Geriatrics, 38(3), 239–250. https://doi.org/10.1016/j.archger.2003.10.004
- Holt-Lunstad, J., Smith, T. B., & Layton, J. B. (2010). Social relationships and mortality risk: A meta-analytic review. PLOS Medicine, 7(7), e1000316. https://doi.org/10.1371/journal.pmed.1000316
- Ibrahim, A. K., Kelly, S. J., & Glazebrook, C. (2013). Socioeconomic status and the risk of depression among UK higher education students. Social Psychiatry and Psychiatric Epidemiology, 48(9), 1491–1501. https://doi.org/10.1007/s00127-013-0663-5
- Inam, S. N. B., Saqib, A., & Alam, E. (2003). Prevalence of anxiety and depression among medical students of private university. Journal of Pakistan Medical Association, 53(2), 44–46. PMID: 12705482
- IsHak, W., Nikravesh, R., Lederer, S., Perry, R., Ogunyemi, D., & Bernstein, C. (2013). Burnout in medical students: A systematic review. The Clinical Teacher, 10(4), 242–245. https://doi.org/10.1111/tct.12014
- Jadoon, N. A., Yaqoob, R., Raza, A., Shehzad, M. A., & Zeshan, S. C. (2010). Anxiety and depression among medical students: A cross-sectional study. JPMA. Journal of Pakistan Medical Association, 60(8) 699–702. PMID: 20726214.
- Kasl, S. V., & Cobb, S. (1966). Health behavior, illness behavior and sick role behavior. Archives of Environmental Health: An International Journal, 12(2), 246–266. https://doi.org/10.1080/00039896.1966.10664365
- Katpar, S., Rana, Z., Hussain, M., Khan, R., & Rehman, R. (2017). Impact of social interdependence on emotional well-being of medical students. Journal of Pakistan Medical Association, 67(7), 992–997. https://ecommons.aku.edu/pakistan_fhs_mc_surg_surg/783
- Kessler, R. C., Crum, R. M., Warner, L. A., Nelson, C. B., Schulenberg, J., & Anthony, J. C. (1997). Lifetime co-occurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in the National Comorbidity Survey. Archives of General Psychiatry, 54(4), 313–321. https://doi.org/10.1001/archpsyc.1997.01830160031005
- Khan, M. S., Mahmood, S., Badshah, A., Ali, S. U., & Jamal, Y. (2006). Prevalence of depression, anxiety and their associated factors among medical students in Karachi, Pakistan. Journal-Pakistan Medical Association, 56(12), 583–588.
- Koivumaa-Honkanen, H., Kaprio, J., Honkanen, R., Viinamäki, H., & Koskenvuo, M. (2004). Life satisfaction and depression in a 15-year follow-up of healthy adults. Social Psychiatry and Psychiatric Epidemiology, 39(12), 994–999. https://doi.org/10.1007/s00127-004-0833-6
- Kumari, U., Dawani, N., Devnani, J., Qureshi, M. F. H., Soleja, F. K., Mohammad, D., & Sadiq, S. (2019). Depression among medical students of Karachi a cross sectional study. MedEdPublish, 8(3), 1-10. https://doi.org/10.15694/mep.2019.000181.1
- Luca, A., Luca, M., & Calandra, C. (2013). Sleep disorders and depression: Brief review of the literature, case report, and nonpharmacologic interventions for depression. Clinical Interventions in Aging, 8, 1033–1039. https://doi.org/10.2147/CIA.S47230
- Matarazzo, J. D., & Herman, D. O. (1984). Relation of education and IQ in the WAIS-R standardization sample. Journal of Consulting and Clinical Psychology, 52(4), 631–634. https://doi.org/10.1037/0022-006X.52.4.631
- Mokdad, A. H., Marks, J. S., Stroup, D. F., & Gerberding, J. L. (2004). Actual causes of death in the United States, 2000. Journal of American Medical Association, 291(10), 1238–1245. https://doi.org/10.1001/jama.291.10.1238
- Nisar, N., Qadri, M. H., Fatima, K., & Perveen, S. (2007). A community based study about knowledge and practices regarding tobacco consumption and passive smoking in Gadap Town, Karachi. Journal of Pakistan Medical Association, 57(4), 186–188. PMID: 17489526.
- Nisar, N., Qadri, M. H., Fatima, K., & Perveen, S. (2009). Dietary habits and life style among the students of a private medical university, karachi. Journal of Pakistan Medical Association, 59(2) 98–101. PMID:19260574.
- Organization, W. H. (2002). The World Health Report 2002: reducing risks, promoting healthy life. World health report. http://www.who.int/whr/2002/en/. [Accessed on 18 June 2018]
- Othieno, C. J., Okoth, R. O., Peltzer, K., Pengpid, S., & Malla, L. O. (2014). Depression among university students in Kenya: Prevalence and sociodemographic correlates. Journal of Affective Disorders, 165, 120–125. https://doi.org/10.1016/j.jad.2014.04.070
- Peltzer, K., Pengpid, S., Olowu, S., & Olasupo, M. (2013). Depression and associated factors among university students in Western Nigeria. Journal of Psychology in Africa, 23(3), 459–465. https://doi.org/10.1080/14330237.2013.10820652
- Peltzer, K., Pengpid, S., Yung, T. K., Aounallah‐Skhiri, H., & Rehman, R. (2016). Comparison of health risk behavior, awareness, and health benefit beliefs of health science and non‐health science students: An international study. Nursing & Health Sciences, 18(2), 180–187. https://doi.org/10.1111/nhs.12242
- Radloff, L. S. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement 1, 1(3), 385–401. https://doi.org/10.1177/014662167700100306
- Reddy, M. (2010). Depression: The disorder and the burden. Indian Journal of Psychological Medicine, 32(1), 1. https://doi.org/10.4103/0253-7176.70510
- Reeves, G. M., Postolache, T. T., & Snitker, S. (2008). Childhood obesity and depression: Connection between these growing problems in growing children. International Journal of Child Health and Human Development, 1(2), 103–114. PMID:18941545.
- Rehman, R., Habib, M., & Fatima, S. S. (2014). A take on social wellbeing attributes by first year medical students. Journal of Pakistan Medical Association, 64(6), 679. PMID:25252489.
- Rehman, R., Nadeem, S., Hussain, M., Khan, R., & Katpar, S. (2015). Exploring emotional wellness: The art of being cheerful about life at medical campus. European Journal of Psychology and Educational Studies, 2(2), 57–64. https://doi.org/10.4103/2395-2555.170723
- Rehman, R., Usmani, A., Omaeer, Q., & Gul, H. (2014). Mentorship” a stride towards maintenance of medical student’s wellbeing. Journal of Pakistan Medical Association, 64(12), 1352–1357. PMID:25842576
- Rehmani, N., Khan, Q. A., & Fatima, S. S. (2018). Stress, Anxiety and Depression in students of a private medical school in Karachi, Pakistan. Pakistan Journal of Medical Sciences, 34(3), 696–701. https://doi.org/10.12669/pjms.343.14664
- Ryder, A. G., Yang, J., & Heine, S. J. (2002). Somatization vs. psychologization of emotional distress: A paradigmatic example for cultural psychopathology. Online Readings in Psychology and Culture, 10(2), 3. https://doi.org/10.9707/2307-0919.1080
- Sabir I, Zaman M. (2013). Youth Violence in Pakistan: The Social Structure and Culture of Violence. Profilaktyka Społeczna i Resocjalizacja, 21, 7–24.
- Schwenk, T. L., Davis, L., & Wimsatt, L. A. (2010). Depression, stigma, and suicidal ideation in medical students. Journal of American Medical Association, 304(11), 1181–1190. https://doi.org/10.1001/jama.2010.1300
- Sörensen, S., Mak, W., Chapman, B., Duberstein, P. R., & Lyness, J. M. (2012). The relationship of preparation for future care to depression and anxiety in older primary care patients at 2-year follow-up. The American Journal of Geriatric Psychiatry, 20(10), 887–894. https://doi.org/10.1097/JGP.0b013e31822ccd8c
- Steptoe, A., & Wardle, J. (1996). The European health and behaviour survey the development of an international study in health psychology. Psychology & Health, 11(1), 49–73. https://doi.org/10.1080/08870449608401976
- Taliaferro, L. A., Rienzo, B. A., Pigg, R. M., Miller, M. D., & Dodd, V. J. (2009). Associations between physical activity and reduced rates of hopelessness, depression, and suicidal behavior among college students. Journal of American College Health, 57(4), 427–436. https://doi.org/10.3200/JACH.57.4.427-436
- Travers, C. (2017). Increasing enjoyable activities to treat depression in nursing home residents with dementia: A pilot study. Dementia, 16(2), 204–218. https://doi.org/10.1177/1471301215586069
- Vilhauer, J. (2014). Think forward to thrive: How to use the mind’s power of anticipation to transcend your past and transform your life. New World Library.
- Youssef, FF. (2016). Medical student stress, burnout and depression in Trinidad and Tobago. Academic Psychiatry, 40:69–75
- Yusuf, S., Hawken, S., Ounpuu, S., Dans, T., Avezum, A., Lanas, F., McQueen, M., Budaj, A., Pais, P., Varigos, J., & Lisheng, L. (2004). Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): Case-control study. Lancet, 364(9438), 937–952. https://doi.org/10.1016/S0140-6736(04)17018-9
- Zaman, R. M. (1996). Psychological problems of medical students in Pakistan: data from the aga khan university, karachi. Teaching and Learning in Medicine: An International Journal, 8(1), 19–27. https://doi.org/10.1080/10401339609539758