Abstract
Research has found that discrepancies exist in many health-related behaviors, leading to discrepancies in health outcomes, between men and women. Among these, women tend to have more positive attitudes towards sleep and better sleep hygiene practices despite often having poorer sleep quality and insufficient sleep duration. The present study operationalized sleep hygiene as multi-faceted behaviors rather than a unitary construct. Using the PROCESS macro, we analyzed whether an interaction exists between gender and sleep attitudes to predict sleep hygiene, if sleep hygiene mediated the relationship between sleep attitudes and sleep outcomes, and if this indirect relationship is moderated by gender. Within our sample, gender moderated sleep attitudes predicting environment- and eating-related sleep hygiene behaviors. Sleep quality was indirectly predicted by sleep attitudes via pre-sleep arousal-related sleep hygiene behaviors. Additionally, gender moderated the indirect relationship between sleep attitudes and sleep quality through environment-related sleep hygiene behaviors. These findings reinforce the relevance of studying sleep attitudes in combination with demographic characteristics as predictors of sleep outcomes, and the usefulness of conceptualizing sleep hygiene as separable factors. It may help inform development of potential interventions intended to improve sleep and suggest directions for future studies.
Public Interest Statement
Though a universal behavior, not everybody gets the same quality and duration of sleep. This study looked into potential factors connecting the differences between sleep attitudes, how favorably one views sleep, and the quality of sleep they get. Past research has shown that women often have more opinions that are favorable on health behaviors such as sleep, though often times, these do not result be better health outcomes. By collecting survey data from across America on health data including diet, exercise, stress and sleep, we were able to investigate these gender differences in sleep outcomes. We found that gender does play a role in sleep health, as do other hygiene behaviors, such as when one eats or the activities done before bed.
1. Gender differences in sleep predictors
Most individuals will spend about one-third of their lifetime sleeping, a behavior essential for a variety of health functions including regulating homeostasis across multiple systems of the body and mind (Vyazovskiy, Citation2015). Adequate sleep is important for many immediate benefits to health and behavior, including regulating the immune system, cardiorespiratory health, and preventing fatigue (Tobaldini et al., Citation2017; Vyazovskiy, Citation2015). Additionally, sleep is essential in maintaining long-term health, likely involved in mechanisms for fighting chronic health conditions such as obesity, hypertension, metabolic syndrome, and even cancer (Gaultney, Citation2014; Redline & Berger, Citation2014; Tobaldini et al., Citation2017). Not only is sleep important for health, but it is also essential for many aspects of cognition, such as memory, executive functioning, attention, and emotion regulation, allowing individuals to perform at their best (Goel et al., Citation2009). The costs of poor sleep can be severe; thus it is important to investigate potential factors that can impair one’s ability to receive adequate rest throughout the night.
Among the factors that can contribute to or impair the quality of sleep one receives at night is sleep hygiene. Sleep hygiene is a set of guidelines for behavioral practices and environmental factors that promote optimal sleep duration and quality (Yang et al., Citation2010). Recent work has reported sleep attitudes to successfully predict sleep hygiene, and sleep outcomes indirectly via sleep hygiene (A. Ruggiero et al., Citation2020). Sleep attitudes refer to one’s perception of the value and utility of sleep, as well as their preference for sleeping over engaging in other activities (Peach & Gaultney, Citation2017). Past studies have found some demographic variance in these constructs. For example, sleep hygiene habits related to consuming caffeinated beverages differ across adolescent boys and girls (Galland et al., Citation2017). Galland and colleagues (2017) also found significant gender differences in in arousal behaviors prior to bed, bedtime, time in bed, and delayed onset of sleep. Sleep attitudes also seem to vary across gender, with women placing a higher value on sleep over other activities at night than men do (A. R. Ruggiero et al., Citation2019). These gender differences in sleep hygiene, sleep attitudes and sleep outcomes suggest that gender may alter the associative patterns.
Sleep attitudes can indirectly predict sleep outcomes through sleep hygiene practices (A. Ruggiero et al., Citation2020). Recent findings suggest that demographic variables, such as age, gender, race, and socioeconomic status (SES), likely moderate the relationship between sleep attitudes and sleep hygiene, thus affecting the indirect pathway (A. Ruggiero et al., Citation2020). Many health behaviors, including coping, treatment seeking, smoking and exercise, exhibit gender differences (Gibbons et al., Citation2012; O’Hea et al., Citation2003), leading to the inclusion of gender as a possible mediator. Though research has found that sleep attitudes indirectly predict sleep outcomes via a global measure of sleep hygiene (A. R. Ruggiero et al., Citation2019), research has yet to investigate if individual factors of sleep hygiene, such as environment or eating behaviors, may best explain this relation, and whether the indirect association varies by gender.
2. Sleep hygiene and sleep outcomes
Sleep outcomes include both duration, the number of hours one spends asleep at night, and sleep quality, which includes duration, sleep efficiency (total time asleep out of total time in bed; Buysse et al., Citation1989) sleep latency, sleep disturbances, and subjective restfulness. Measures of sleep quality are often used in examining sleep outcomes, as these allow comparisons to disordered or irregular sleep (Buysse et al., Citation1989). Both of these outcomes are important to measure. Evidence associates duration with many health factors, such as metabolic function, and quality with factors such as cardiorespiratory health and immune health, even for individuals not diagnosed with sleep disorders (Taheri et al., Citation2004; Tobaldini et al., Citation2017). Both duration and quality vary with sleep hygiene, conditions such as a consistent bedtime and a relaxing environment can help improve both (Yang et al., Citation2010).
Disturbances due to environmental conditions like light, noise, or temperature can lead to delayed sleep onset, waking throughout the night, lowering efficiency, duration, and quality. Sleep onset and quality may also be impaired by engaging in presleep arousing behaviors, or consumption of food or other substances, preventing key sleep-specific processes for regulating health from occurring (Galland et al., Citation2017; Vyazovskiy, Citation2015). Furthermore, allowing sufficient time to sleep, and maintaining a consistent sleep schedule contribute to healthy sleep outcomes (Chaput et al., Citation2020).
As a set of behaviors, sleep hygiene can be broken into several components, all of which can affect sleep outcomes of quality and duration. Lin et al. (Citation2007) considered general health practices, optimal environmental conditions, sleep-related behaviors and presleep activities in defining four factors of sleep hygiene: physiological and cognitive arousal, eating and consumption behaviors, environmental factors of the bedroom, and timing factors of the sleep schedule. Optimal sleep occurs when an individual has low arousal, has not eaten recently, is in a quiet, dark, and cool environment, and has a consistent bedtime (Lin et al., Citation2007). Though some components of sleep hygiene are under volitional control, facets such as timing and eating may be harder to maintain for individuals who work varying shifts, leading to poorer sleep outcomes (Ko, Citation2013). Residents halls and apartment complexes may weaken one’s control of the sleep environment.
Often times, attitudes towards behaviors can be an important predictor of those behaviors, and thus must be considered in research or clinical settings. Based on a model of health-related behaviors (Eagly & Chaiken, Citation2007), sleep attitudes reflect values placed sleep over other activities, including socializing, work, or recreational activities (Peach & Gaultney, Citation2017). Individuals who have more positive sleep attitudes tend to also have better sleep hygiene scores, resulting in better sleep quality and appropriate sleep durations (A. R. Ruggiero et al., Citation2019). Research has shown disparities in connections between sleep attitudes, sleep hygiene, and sleep outcomes as a function of demographic characteristics, with women reporting poorer hygiene and sleep quality (A. R. Ruggiero et al., Citation2019). However, women with favorable attitudes about sleep reported better sleep hygiene practices, longer and better quality sleep than men with positive attitudes (A. R. Ruggiero et al., Citation2019).
3. Health-related gender differences
Various differences at the biological and personality domain may contribute to differences in health decision making and attitudes. Literature comparing gender and concern surrounding health found significant differences in trait-based personality outcomes for health-related and health-seeking behaviors (Weller, Ceschi, Hirsch, Satori & Constantini, 2018). Broadly, femlaes tend to have more positive attitudes towards health information seeking and health behaviors compared to males, yet report lower overall health outcomes (Gibbons et al., Citation2012; Gil‐Lacruz & Gil‐Lacruz, Citation2010; O’Hea et al., Citation2003; A. R. Ruggiero et al., Citation2019).
A variety of objective and subjective measures of sleep have investigated gender differences. Polysomnography studies indicate that while males tend to be diagnosed with obstructive sleep apnea at higher rates, females tend to have higher rates of diagnoses for insomnia (Auer et al., Citation2018). When medical students reported whether they were receiving sufficient sleep and sleep quality, females reported higher rates of poor sleep quality and insufficient sleep than males (Vajda et al., Citation2017). Physiological factors related to sleep outcomes and sleep hygiene may exist as well, including different circadian preferences, such as women reporting stronger morning-orientation (Roky et al., Citation2006).
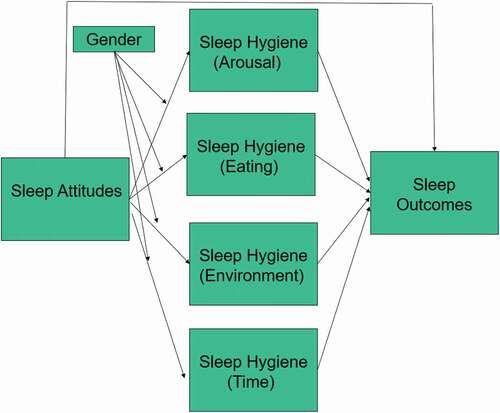
Mixed findings about gender and associations between sleep attitudes, hygiene and outcomes suggest a need to examine sleep hygiene as a multi-faceted construct rather than a global measure. Sleep hygiene includes both personal decisions, such as arousal behaviors and consumption prior to bed, as well as factors that may be beyond an individual’s control, such as environmental conditions and sleep timing. the present study analyzed sleep hygiene as four parallel variables. The four facets were entered simultaneously to examine a finer-grained potential indirect paths from sleep attitudes to sleep outcomes via the four components of sleep hygiene. Presently, no published studies were found that separated sleep hygiene into subcomponents. Gender was used as a moderator of each indirect pathway. We hypothesized that (1) sleep attitudes would interact with gender in predicting the components of sleep hygiene (2) We predicted significant indirect pathways of sleep attitudes with sleep outcomes via each of the four components of sleep hygiene. Additionally, (3) we predicted that the indirect pathways would be moderated by gender, in that indirect paths would be significant for females. This hypothesized relationship is shown in .
4. Methods
4.1. Participants
This study’s sample (N = 173) recruited participants using Amazon’s Mechanical Turk (MTurk) pool. MTurk allows researchers to distribute surveys through their service, with the researchers paying any individuals who participate. The study reported here is a secondary analysis of archived data (A. R. Ruggiero et al., Citation2019). The original study was approved by the IRB at the University of North Carolina Charlotte, study #17-0226. The original study sought to explore the relationship between demographic characteristics (age, race, gender, SES) and sleep attitudes in predicting overall sleep hygiene and sleep outcomes (A. R. Ruggiero et al., Citation2019). Participants had to reside in the United States and be at least 21 years old to be included and were compensated $2.50 for their participation. Demographic data about the sample are shown in . Descriptive and correlational data for the measures are presented in . Gender differences in sleep attitudes, sleep hygiene, and sleep outcomes are shown in . Participants who identified as neither male nor female (N = 1) were excluded from analyses as the study’s focus was on comparing the difference between genders and the sample size for individuals in this category was not sufficient for comparative analyses.
Table 1. Description of Sample demographic statistics
Table 2. Bivariate Correlations for focal variables
Table 3. Descriptive Statistics of focal variables by gender
5. Materials
5.1. Sleep attitudes
The study used the Charlotte Attitudes Towards Sleep Scale (CATS; Peach & Gaultney, Citation2017 to measure sleep attitudes. Items utilized a 7-point Likert scale ranging from strongly disagree (1) to strongly agree (7). Ten items assessed two dimensions of sleep attitudes, the perceived benefits and time commitments of sleep, as well as a global measure of sleep attitude. Higher scores indicated more positive attitudes. Five items were reverse-coded and scores were averaged, with higher scores indicating more positive attitudes towards sleep. Internal consistency between the items showed good reliability in the present data (α = .79), similar to the validation study (α = .76).
5.2. Sleep hygiene
The Sleep Hygiene Practice Scale (SHPS) measured self-reported sleep hygiene (Lin et al., Citation2007; Yang et al., Citation2010). This measure contains 30 items each measuring the frequency of a behavior’s occurrence on a scale of 1–6, with 1 representing the behavior never occurring and 6 representing always. The scale consists of four domains assessing sleep hygiene. Arousal-related behaviors were composed of nine items including engaging in activities before bed or while in bed that could disrupt sleep. Eating/Drinking behaviors were composed of five items such as eating too much or too little, and consumption of caffeine, alcohol, and other possible stimulants close to bedtime. Sleep environment-related behaviors, eight items total, included noise, brightness, ambient temperature and air, and comfort as well as other non-sleep related distractors in the room. Lastly, sleep scheduling and timing behaviors were measured by seven items and included inconsistent bedtimes, wake times, sleeping or staying in bed late, napping excessively, and lack of sunlight and exercise. Higher scores represent poorer sleep hygiene. Internal consistency between items on the scale was high (α = .93) for the present study.
5.3. Sleep outcomes
This study collected data on sleep quantity measured in hours and sleep quality measured via the Pittsburgh Sleep Quality Index (PSQI; Buysse et al., Citation1989). The PSQI is a standardized measure including 19 self-report questions for participants to describe their sleep habits over the past month. After summing individuals scores, a global score can be calculated, ranging from 0–16. Higher scores represent poorer sleep quality, with a five or above indicative of poor sleep quality. The PSQI is considered an acceptable, reliable and validated measure used for subjective sleep quality. A single item from the PSQI estimated sleep duration as hours of sleep obtained at night, differentiating it from hours spent in bed. Higher scores here indicated higher sleep duration. The data produced no significant differences throughout the week (A. R. Ruggiero et al., Citation2019); therefore, sleep duration was operationalized as a single score.
Perceived
5.4. Socioeconomic Status (SES)
This variable was estimated using the MacArthur Scale of Subjective Social Status (Adler et al., Citation2000). Participants are presented with a ladder and are instructed to place themselves upon one of the ladder’s rungs. The highest rung represents individuals of higher incomes, education, and social status, whereas the lowest rung represents those who are worst off in these aspects. Participants were asked to rank themselves on this ladder compared to both the general populations of the United States (reported in this study) and their local communities. Potential scores ranged from 1–10, with higher scores indicating higher perceived social status.
5.5. Procedure
Participants were able to access and register for the present study through MTurk’s website, which redirected them to Qualtrics (www.qualtrics.com) to take the survey. An informed consent screen was presented, and all participants had to acknowledge that they were United States residents and at least 21 years old. This study was approved by the institutional review board at the university which the study was conducted. Participants then proceeded to fill out demographic information, including Socioeconomic Status, gender, race and age. Individuals were also asked to report whether or not they have been diagnosed with any clinical sleep disorders, including insomnia, narcolepsy, sleep apnea or sleepwalking. Participants also responded to surveys describing their stress, exercise and eating habits before filling out the relevant sleep surveys (including sleep attitudes, sleep hygiene, and sleep outcomes).
5.6. Plan of analysis
Demographic data for race was dummy coded and dichotomized by two researchers and checked for accuracy and inter-rater reliability. Race was an open ended prompt, and was coded for 0 to represent racial minorities. Gender was dummy coded with males as 0 and females as 1; one individual identified outside of the gender binary and was excluded from analyses due to insufficient sample size for a separate dummy-coded group. Data for SES and age were left as continuous variables.
Initial descriptive statistics and bivariate correlations were run using SPSS 26.0 (IBM Corporation, Armonk NY, USA). Additionally, differences in focal variables (sleep attitudes, sleep hygiene and facets of it, sleep duration and sleep quality) were compared using independent samples T-Tests using SPSS. The path analyses included race, gender, SES and age as covariates. The test of moderated mediation controlled for race, SES, and age. Hypotheses 1, the interaction between sleep attitudes and gender to predict sleep hygiene, was tested by a simple moderation analysis using the PROCESS macro (Model 1, Hayes, Citation2018). Hypothesis 2 used a parallel path analysis to examine the indirect effects of attitudes on duration or quality via the four subcomponents, entered as simultaneous indirect paths (PROCESS Model 4). The third hypothesis, examining if gender moderated the indirect effects of attitudes onto sleep outcomes via sleep hygiene, was tested using separate analyses for sleep duration and sleep quality (PROCESS Model 8). Nonstandardized coefficients are reported, and indirect effects were supported by bootstrapping.
Due to the large number of individuals reporting sleep disorders, analyses were run in three separate ways. Each analysis was run first including all individuals with sleep disorders without any change to the overall model. The analyses were then re-run excluding any individuals who reported sleep disorders as well as run including individuals reporting sleep disorders but using disorder status as a covariate.
6. Results
Descriptive statistics for demographic characteristics of the sample are provided in . The sample was mostly young-adult, 39% self-reported as members of underrepresented groups, that reported feeling neither high nor low in their subjective socioeconomic status. Most of the sample (81.50%) reported no diagnosed sleep disorders.
Descriptive statistics surrounding sleep are shown in . Participants reported generally good sleep hygiene practices, an average sleep duration of 7.35 hours, and poor average sleep quality PSQI≥5). The four components of sleep hygiene were intercorrelated. Worse sleep hygiene was associated with worse sleep quality, while only the arousal and time components significantly associated with sleep duration. Individuals with more positive attitudes towards sleep reported better sleep hygiene practices, longer sleep duration, and better sleep quality. Additionally, duration and sleep quality had a strong negative correlation; individuals who slept for longer periods reported better quality sleep.
PROCESS Analysis produced initial tests of the main effects of sleep attitudes and gender on each of the four components of sleep hygiene. When controlling for race, SES and age, sleep attitudes remained significantly associated with each component (b ≤ −3.75, p < .001). Gender was a significant moderator of the eating (b = 1.95, p = .02) and environment (b = 3.23, p < .01) components only, thereby partially supporting hypothesis 1, showing an interaction component between gender and attitudes for predicting two facets of sleep hygiene. See for illustration of these interactions. In both instances, males with high sleep attitudes see a greater difference compared to males with lower sleep attitudes than females in each category of sleep attitudes suggesting a moderating effect of gender. While, in both cases, more favorable sleep attitudes associated with better sleep hygiene behaviors, the difference in behaviors was most pronounced among females
Figure 2. Moderating Effects of Gender on Sleep Hygiene Eating sub-score (Hypothesis 1; Higher Scores Indicate Worse Hygiene Behaviors)
Figure 3. Moderating Effects of Gender on Sleep Hygiene Environment sub-score(Hypothesis 1; Higher Scores Indicate Worse Hygiene Behaviors)
Analyses of the second hypothesis, whether sleep attitudes would predict sleep outcomes indirectly via sleep hygiene subcomponents, are shown in . The path analysis explained 9% of the variability in sleep duration, and did not reach significance. The analysis of sleep quality explained a significant 40% of the variability. Sleep attitudes had a significant, direct contribution to each sleep hygiene component (the “a” path) More favorable attitudes towards sleep predicted fewer unhealthy sleep behaviors. Sleep hygiene components did not significantly predict sleep duration (“b” paths), nor were any indirect paths significant. However, analysis using sleep quality as the outcome indicated that hygiene behaviors related to pre-bedtime arousal did significantly predict the outcome. Likewise, the indirect effect of sleep attitudes on sleep quality via arousal behaviors was significant. Thus, the second hypothesis was supported for the arousal subcomponent only.
Table 4. Path Analyses of Direct and Indirect Effects Of Sleep Attitudes On Sleep Outcomes Through Sleep Hygiene (Hypothesis 2)
The final hypothesis, that indirect pathways would be moderated by gender (mediated moderation), was not supported. The indices of moderated mediation generated by the PROCESS analysis all had 95% confidence intervals that included 0, indicating that gender did not moderate indirect pathways (sleep duration indices ≤ .03; sleep quality indices ≤ .27).
Across all three types of analyses (including individuals with sleep disorders, excluding individuals with sleep disorders, and including individuals but marking sleep disorders as a covariate), near identical results were found. All significant findings were conserved across the three studies and effect sizes remained similar and consistent. For the model testing hypothesis three, the moderation of gender effecting the indirect relationship of sleep attitudes onto sleep quality, one additional finding emerged only when sleep disorder status was treated as a covariate. In this analysis, we found that gender did have a non-zero interaction effect on the arousal pathway only, with men seeing a greater effect of sleep attitudes indirectly affecting sleep outcomes through arousal-related behaviors (Men: b = −.74, SE = .26, CI = −1.33—−.30; Women: b = −.54, SE = .22, CI = −1.02.—−.17). Additionally, as these data have been analyzed before, a Bonferoni adjustment was done for all tests but all outcomes remained significant regardless.
7. Discussion
While knowledge of a health behavior plays an important role in making decisions to engage in health behaviors, the broader literature in health psychology has indicated that attitudes towards the behavior may be a better predictor than knowledge (Gil‐Lacruz & Gil‐Lacruz, Citation2010). This has been seen for healthy sleep behaviors, as well (A. R. Ruggiero et al., Citation2019). Furthermore, attitudes about and implementation of healthy behaviors may vary by gender (Gil‐Lacruz & Gil‐Lacruz, Citation2010). This study investigated the relationship between sleep attitudes, sleep hygiene (operationalized as four sub-components), and sleep outcomes, further expanding the literature and nomological network for these constructs. The analyses indicated that gender interacts with sleep attitudes to predict two of four components of sleep hygiene (presleep eating and sleep environment). Sleep attitudes predicted sleep quality but not sleep duration indirectly via presleep arousal behaviors; however, indirect paths were not moderated by gender.
One strength of the present study was to operationalize sleep hygiene as multifaceted rather than as a single construct. This was first investigated by Yang et al. (Citation2010), who found that individuals with insomnia only showed significant correlations between arousal-related behaviors and sleep quality. Additionally, though for good sleepers all four domains of sleep hygiene correlated with sleep quality, eating/drinking-related behaviors did not correlate with insomnia risk (Yang et al., Citation2010). The current study continues to explore upon the differences between these subcomponents to best understand their relationship with both sleep attitudes and sleep outcomes. Sleep outcomes can be investigated more precisely and directly based on the individual’s needs by better understanding individual mechanisms associated with the four subcomponents of sleep hygiene.
Other work has found gender differences in sleep attitudes, sleep hygiene, and sleep practices (Chang & Choi, Citation2016; Dimakos et al., Citation2019; Joshi et al., Citation2015; A. R. Ruggiero et al., Citation2019), raising the possibility that gender must be taken into consideration to understand the mechanisms by which sleep attitude predict sleep practices and outcomes. Our first hypothesis, whether gender would interact with sleep attitudes to predict components of sleep hygiene, was shown to be true for the eating and environment subscales, but not for other subscales. Sleep hygiene problems were more frequent among those with negative sleep attitudes; however, attitude seemed to play a more significant role in presleep eating behaviors and providing an environment conducive to sleep among males. The findings are similar to those of many previous researchers who have found that women tend to have more favorable attitudes towards sleep (Cha & Eun, Citation2018; A. R. Ruggiero et al., Citation2019; Venn et al., Citation2013) but that sleep-behaviors and sleep-outcomes differed across gender and other demographic characteristics (Hantsoo et al., Citation2013; A. R. Ruggiero et al., Citation2019).
Males with less regard for sleep appear to invest less in sleep-related behaviors relative to other groups, possibly due to personality or societal differences as seen in other studies (Gil‐Lacruz & Gil‐Lacruz, Citation2010; O’Hea et al., Citation2003). Among personality and physiological differences, various outcomes associated with sleep have been observed across gender. Personality traits, such as assertiveness, are often lower in women as well as individuals reporting greater symptoms of clinical insomnia and other sleep disruptors (Cerolini et al., Citation2017; Leaper & Robnett, Citation2011). These differences in personality across gender may explain differences in sleep attitudes, sleep hygiene behaviors and sleep outcomes experienced separately by men and women given the similarities observed to those with other sleep disorders. Though not specific to sleep research, concern surrounding health-behaviors may be related to higher neuroticism and humility, observed more often among women than among men (Weller et al., Citation2018). Higher neuroticism and lower conscientiousness have been shown to be associated with poorer sleep outcomes (Duggan et al., Citation2014). Personality and physiological differences may be related as well; morning-oriented circadian rhythms, a preference found more strongly in females (Roky et al., Citation2006) is possibly related to conscientiousness (Rahafar et al., Citation2017; Randler, Citation2008).
Sleep attitudes indirectly predicted sleep quality via presleep arousal behaviors. Individuals may have more control over arousal-related sleep hygiene behaviors than other aspects (such as a supportive environment, and timing) which may vary due to work schedule and interaction with others interfering with optimal sleep conditions (Shriane et al., Citation2020). No indirect path was seen for sleep duration. Though sleep quality is not necessarily under one’s control, sleep duration may involve greater volitional control, leading to possible differences in outcomes. Individuals may choose to sleep for longer durations of time in order to attempt to compensate for a night of poor sleep quality, leading to longer duration, though sleep quality remains sensitive to sleep hygiene related deficits.
Lastly, we were able to find a significant moderation effect of gender when looking at the indirect pathway of sleep attitudes to sleep quality via environmental behaviors. Other pathways through sleep hygiene to sleep quality did not show any moderated mediation effects, nor did any pathways to sleep duration. This may suggest the moderating effect of gender on establishing a conducive sleep environment reported above. Those with more positive attitudes about sleep may be more motivated to arrange their environment to facilitate sleep quality, as research has shown those with more positive health attitudes tend to make greater efforts to adjust their health behaviors (O’Hea et al., Citation2003).
This study had several strengths. The use of MTurk for distributing the surveys and recruiting participants allowed for a more diverse sample by including a variety of ages, races, and socioeconomic statuses. Notably, a larger percentage of participants were male, relative to many samples of college students (e.g., Peach & Gaultney, Citation2017). Although no claim is made here of an ethnically representative sample of adults in the United States, the percentage of participants who identified as members of an under-represented population was somewhat higher than the general population of Americans (31% vs. 24%; United States Census Bureau, Citation2020). The findings are also useful in that they apply to non-clinical populations, as most studies investigating differences in sleep across gender tend to look at those with diagnosed sleep conditions (Auer et al., Citation2018). Additionally, though the CATS scale was originally validated for college students (Peach & Gaultney, Citation2017), it maintained high internal consistency in this study, suggesting its scope has broader applications in future studies. Use of the PROCESS macro for SPSS allowed exploration of whether indirect pathways were moderated by gender. This study expands upon previous work (A. R. Ruggiero et al., Citation2019) which primarily looked at dichotomized interactions. Additionally, this study is novel in looking at the four components of sleep hygiene as separate components, rather than grouping them as a single variable. It may be useful to further explore volitional and nonvolitional elements of sleep hygiene.
Several limitations must be taken into consideration. Notably, no objective data were collected on the sample, as all information was self-report. For some variables, such as subjective SES, this could be especially problematic due to individuals having little reference for assessment, however, research shows that subjective and objective SES are highly correlated and related for predicting health outcomes (Kim et al., Citation2018). Due to the nature of self-report and biases, participants may have not answered some of the survey items honestly, including aspects of the SHPS regarding consumption of alcohol, caffeine, and stimulants. Some items from the SHPS can be vague about what behaviors to report and the measure does not specify a timeframe. Additionally, participants were not asked about any shift work, which may confound sleep hygiene and sleep outcome measures (Schwartz & Roth, Citation2006). Though MTurk is a useful tool for acquiring data from a diverse sample across the country, the nature of it being unmonitored through an online survey may have led individuals to rush through it or become distracted and our survey did not include any attention checks, a large potential limitation.
Though some data were collected on mental health (Depression and Stress), we chose to leave this out of the analyses. Previous studies have shown that mental health issues including depression and anxiety are strongly correlated with poorer sleep outcomes (Gregory et al., Citation2011), though the relationship appears bidirectional. Because data for this study was collected at a single time point and did not go in-depth into facets of mental health, these variables were left out of analyses. This limitation should be further explored in future studies to address the role that depression, anxiety, stress, and similar facets of mental health may have in predicting different sleep behaviors and outcomes, as well as the role that better sleep behaviors may have in predicting them.
Due to only one individual reporting their gender as nonbinary, this was insufficient for analyses exploring the role that other gender identities (transgender, nonbinary, etc.) play in sleep attitudes, sleep hygiene and sleep outcomes, leading to possible future research topics to explore. Although gender differences are present in these data, we have no basis to speculate on what aspect of gender (such as biological sex, gender identity) may underlie the differences. The finding that gender did not interact with controllable behaviors such as arousal may reflect differences in concern about health behaviors in general (Weller et al., Citation2018). Additionally, many of the items related to sleep hygiene factors in the environment such as external light, noise, or temperature may be less within the control of individuals if have a shared sleeping environment or they can’t choose factors such as light and noise. Other aspects of sleep such as chronicity, timing, and consistency, were not included. It is also worth noting that because participants on MTurk can choose which studies to participate in, there could likely be a self-selection bias for those who are interested in sleep (thus having more favorable and healthier sleep attitudes and behaviors, respectively) or those concerned with their sleep (having poorer sleep outcomes), likely contributing to the large number of individuals diagnosed with sleep disorders. However, approximately 20% of the United States population is diagnosed with a sleep disorder, suggesting good external validity and generalizability (American Sleep Association, Citation2021).
This study serves as an exploration between gender differences as they relate to sleep attitudes and outcomes. The findings of this study support further research into demographic difference in sleep related attitudes and behaviors to improve overall sleep. Sleep interventions, which often feature increasing knowledge about sleep (e.g., reducing engaging activity and eating before bed, having consistent bed and wake times and a calm sleep environment) may be improved by considering the role of attitudes among various demographic groupings. Intervention strategies that successfully improve sleep may contribute to improvements in mental and physical health. It appears useful to view both sleep and sleep hygiene as multi-faceted constructs rather than unitary ones.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, PZ, upon reasonable request https://doi.org/10.15139/S3/QZUBHT.
Additional information
Funding
Notes on contributors
Philip Zendels
Research in Dr. Gaultney’s Sleep for Life lab focuses on using health psychology to better understand discrepancies individuals may have in sleep outcomes from a variety of factors. The lab has investigated multiple projects that look into how demographic information, including age, gender, race, and socioeconomic status may play a role into health as it relates to sleep. Aria Ruggiero’s research has investigated differences in sleep and health behaviors across underserved populations and looked at behavioral and educational methodology to overcome this to ensure better sleep in clinical patients. Philip Zendels’s research has investigated differing aspects of sleep hygiene to better understand their effects on sleep outcomes and health. Examples of these include the timing of sleep and the sleep environment, that certain populations may have less control over.
References
- Adler, N. E., Epel, E. S., Castellazzo, G., & Ickovics, J. R. (2000). Relationship of subjective and objective social status with psychological and physiological functioning: Preliminary data in healthy, White women. Health Psychology, 19(6), 586–14. https://doi.org/10.1155/2013/314295
- American Sleep Association (2021). Sleep Statistics: Data About Sleep Disorders. American Sleep Association. https://www.sleepassociation.org/about-sleep/sleep-statistics/
- Auer, M., Frauscher, B., Hochleitner, M., & Högl, B. (2018). Gender-Specific Differences in Access to Polysomnography and Prevalence of Sleep Disorders. Journal of Women’s Health, 27(4), 525–530. https://doi.org/10.1089/jwh.2017.6482
- Buysse, D. J., Reynolds, C. F., Monk, T. H., Berman, S. R., & Kupfer, D. J. (1989). The Pittsburgh Sleep Quality Index . A New Instrument Psychiatric Practice and Research.
- Cerolini, S., Devoto, A., Ballesio, A., & Lombardo, C. (2017). Assertiveness, insomnia and depression: Which relationship? Sleep Medicine, 40(Supp.1), e49–e49. https://doi.org/10.1016/j.sleep.2017.11.137
- Cha, S.-E., & Eun, K.-S. (2018). Convergence in Sleep Time Accomplished? Gender Gap in Sleep Time for Middle-Aged Adults in Korea. International Journal of Environmental Research and Public Health, 15(4), 803. https://doi.org/10.3390/ijerph15040803
- Chang, A., & Choi, J. (2016). Predictors of Sleep Quality Among Young Adults in Korea: Gender Differences. Issues in Mental Health Nursing, 37(12), 918–928. https://doi.org/10.1080/01612840.2016.1235636
- Chaput, J., Dutil, C., Featherstone, R., Ross, R., Giangregorio, L., Saunders, T., Janssen, I., Poitras, V., Kho, M., Ross-White, A., Zankar, S., & Carrier, J. (2020). Sleep timing, sleep consistency, and health in adults: A systematic review. Applied Physiology, Nutrition, and Metabolism, 45(10), S232–S247. https://doi.org/10.1139/apnm-2020-0032
- Dimakos, J., Somerville, G., Finn, C., Boursier, J., Keskinel, D., & Gruber, R. (2019). Gender differences in sleep hygiene associated with poor sleep in adolescents with adhd symptoms. Sleep Medicine, 64(supp. 1), S137–S138. https://doi.org/10.1016/j.sleep.2019.11.376
- Duggan, K., Friedman, H., McDevitt, E., & Mednick, S. (2014). Personality and Healthy Sleep: The Importance of Conscientiousness and Neuroticism. PloS One, 9(3), e90628–e90628. https://doi.org/10.1371/journal.pone.0090628
- Eagly, A. H., & Chaiken, S. (2007). The advantages of an inclusive definition of attitude. Social Cognition, 25(5), 582–602.
- Galland, B., Gray, A., Penno, J., Smith, C., Lobb, C., & Taylor, R. (2017). Gender differences in sleep hygiene practices and sleep quality in New Zealand adolescents aged 15 to 17 years. Sleep Health: Journal of the National Sleep Foundation, 3(2), 77–83. https://doi.org/10.1016/j.sleh.2017.02.001
- Gaultney, J. (2014). Weekend-weeknight shifts in sleep duration predict risk for metabolic syndrome. Journal of Behavioral Health, 3(3), 1. https://doi.org/10.5455/jbh.20140704094111
- Gibbons, S., Barnett, S., Hickling, E., Herbig‐Wall, P., & Watts, D. (2012). Stress, coping, and mental health‐seeking behaviors: Gender differences in OEF/OIF health care providers. Journal of Traumatic Stress, 25(1), 115–119. https://doi.org/10.1002/jts.21661
- Gil‐Lacruz, M., & Gil‐Lacruz, A. (2010). Health Perception and Health Care Access: Sex Differences in Behaviors and Attitudes. American Journal of Economics and Sociology, 69(2), 783–801. https://doi.org/10.1111/j.1536-7150.2010.00723.x
- Goel, N., Rao, H., Durmer, J., & Dinges, D. (2009). Neurocognitive Consequences of Sleep Deprivation. Seminars in neurology, 29, 320–339. https://doi.org/10.1055/s-0029-1237117.
- Gregory, A. M., Buysse, D. J., Willis, T. A., Rijsdijk, F. V., Maughan, B., Rowe, R., Cartwright, S., Barclay, N. L., & Eley, T. C. (2011). Associations between sleep quality and anxiety and depression symptoms in a sample of young adult twins and siblings. Journal of Psychosomatic Research, 71(4), 250–255. https://doi.org/10.1016/j.jpsychores.2011.03.011
- Hantsoo, L., Khou, C. S., White, C. N., & Ong, J. C. (2013). Gender and cognitive–emotional factors as predictors of pre-sleep arousal and trait hyperarousal in insomnia. Journal of Psychosomatic Research, 74(4), 283–289. https://doi.org/10.1016/j.jpsychores.2013.01.014
- Hayes, A. (2018). Introduction to mediation, moderation, and conditional process analysis (3rd ed. ed.). Guilford Press.
- Joshi, K., Mishra, D., Dubey, H., & Gupta, R. (2015). Sleep pattern and insomnia among medical students: Effect of gender and dysfunctional beliefs and attitudes about sleep. Somnologie : Schlafforschung Und Schlafmedizin = Somnology : Sleep Research and Sleep Medicine, 19(3), 205–211. https://doi.org/10.1007/s11818-015-0012-x
- Kim, K. W., Wallander, J. L., Peskin, M., Cuccaro, P., Elliott, M. N., & Schuster, M. A. (2018). Associations Between Parental SES and Children’s Health-Related Quality of Life: The Role of Objective and Subjective Social Status. Journal of Pediatric Psychology, 43(5), 534–542. https://doi.org/10.1093/jpepsy/jsx139
- Ko, S. (2013). Night Shift Work, Sleep Quality, and Obesity. Journal of Lifestyle Medicine, 3(2), 110–116.
- Leaper, C., & Robnett, R. (2011). Women Are More Likely Than Men to Use Tentative Language, Aren’t They? A Meta-Analysis Testing for Gender Differences and Moderators. Psychology of Women Quarterly, 35(1), 129–142. https://doi.org/10.1177/0361684310392728
- Lin, S. C., Cheng, C. P., Yang, C. M., & Hsu, S. C. (2007). Psychometric properties of the Sleep Hygiene Practice Scale. Sleep, 30, A262.
- O’Hea, E., Wood, K., & Brantley, P. (2003). The Transtheoretical Model: Gender Differences Across 3 Health Behaviors. American Journal of Health Behavior, 27(6), 645–656. https://doi.org/10.5993/AJHB.27.6.7
- Peach, H., & Gaultney, J. (2017). Charlotte Attitudes Towards Sleep (CATS) Scale: A validated measurement tool for college students. Journal of American College Health, 65(1), 22–31. https://doi.org/10.1080/07448481.2016.1231688
- Rahafar, A., Castellana, I., Randler, C., & Antúnez, J. (2017). Conscientiousness but not agreeableness mediates females’ tendency toward being a morning person. Scandinavian Journal of Psychology, 58(3), 249–253. https://doi.org/10.1111/sjop.12362
- Randler, C. (2008). Morningness–eveningness, sleep–wake variables and big five personality factors. Personality and Individual Differences, 45(2), 191–196. https://doi.org/10.1016/j.paid.2008.03.007
- Redline, S., & Berger, N. (2014). Impact of Sleep and Sleep Disturbances on Obesity and Cancer. Springer New York. https://doi.org/10.1007/978-1-4614-9527-7
- Roky, R., Benaji, B., & Benchekroun, M. (2006). Gender differences in sleep, sleepiness and chronotype. Gender Medicine, 3(suppl 1), S63–S64. https://doi.org/10.1016/S1550-8579(06)80149-X
- Ruggiero, A., Peach, H., Zendels, P., & Gaultney, J. (2020). Sleep Attitudes As A Predictor Of Sleep Outcomes: A Secondary Data Analysis. Health Psychology and Behavioral Medicine, 8(1), 623–635. https://doi.org/10.1080/21642850.2020.1852939
- Ruggiero, A. R., Peach, H. D., & Gaultney, J. F. (2019). Association of sleep attitudes with sleep hygiene, duration, and quality: A survey exploration of the moderating effect of age, gender, race, and perceived socioeconomic status. Health Psychology and Behavioral Medicine, 7(1), 19–44. https://doi.org/10.1080/21642850.2019.1567343
- Schwartz, J. R., & Roth, T. (2006). Shift work sleep disorder. Drugs, 66(18), 2357–2370. https://doi.org/10.2165/00003495-200666180-00007
- Shriane, A., Ferguson, S., Jay, S., & Vincent, G. (2020). Sleep hygiene in shift workers: A systematic literature review. Sleep Medicine Reviews, 53, 101336. https://doi.org/10.1016/j.smrv.2020.101336
- Taheri, S., Lin, L., Austin, D., Young, T., & Mignot, E. (2004). Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Medicine, 1(3), 210–217. https://doi.org/10.1371/journal.pmed.0010062
- Tobaldini, E., Costantino, G., Solbiati, M., Cogliati, C., Kara, T., Nobili, L., & Montano, N. (2017). Sleep, sleep deprivation, autonomic nervous system and cardiovascular diseases. Neuroscience and Biobehavioral Reviews, 74(Pt B), 321–329. https://doi.org/10.1016/j.neubiorev.2016.07.004
- United States Census Bureau. (2020, July 1). U.S. census bureau QUICKFACTS: United States. https://www.census.gov/quickfacts/fact/table/US/IPE120219
- Vajda, C., Czernin, M., Matzer, F., Schenkeli, E., Lorenzoni, N., & Fazekas, C. (2017). The European Journal of Public Health. Gender Related Difference in Sleep Quality and Tiredness in Austrian Medical Students, 27(3), 491–492. https://doi.org/10.1093/eurpub/ckx186.258
- Venn, S., Meadows, R., & Arber, S. (2013). Gender differences in approaches to self-management of poor sleep in later life. Social Science & Medicine (1982), 79, 117–123. https://doi.org/10.1016/j.socscimed.2012.09.037
- Vyazovskiy, V. (2015). Sleep, recovery, and metaregulation: Explaining the benefits of sleep. Nature and Science of Sleep, 7, 171–184. https://doi.org/10.2147/NSS.S54036
- Weller, J., Ceschi, A., Hirsch, L., Sartori, R., & Constantini, A. (2018). Accounting for Individual Differences in Decision-Making Competence: Personality and Gender Differences. Frontiers in Psychology, 9, 2258. https://doi.org/10.3389/fpsyg.2018.02258
- Yang, C., Lin, S., Hsu, S., & Cheng, C. (2010). Maladaptive Sleep Hygiene Practices in Good Sleepers and Patients with Insomnia. Journal of Health Psychology, 15(1), 147–155. https://doi.org/10.1177/1359105309346342