Abstract
Emergence of any pandemic raises serious concerns toward the psychological well-being of an individual and overall society. Although, the magnitude and intensity of the novelwellb coronavirus (COVID-19) pandemic are not precisely known yet, however, this pandemic has predominantly reshaped the global scenario. Scholars have begun to unfold the reality of this traumatic situation, but empirical research that focuses on the identification of key factors that could have a notable impact on mental wellbeing of the general population is limited. To fill this gap, this research endeavors to analyze the impact of fear of getting infected and social isolation on mental well-being during the pandemic. In addition, psychological resilience is used as a moderator between social isolation and mental well-being. A total of 714 responses were received through an online survey from university students across all provinces of Pakistan. The findings demonstrate that people who fear of being infected tend to engage in social isolation, and social isolation brings negative repercussions toward mental well-being. Interestingly, the study findings reveal that psychological resilience could mitigate the negative impact of social isolation on mental well-being. This study calls for creating and promoting awareness concerning psychological resilience in order to cope with the psychological challenges during this COVID-19 pandemic.
PUBLIC INTEREST STATEMENT
The coronavirus pandemic has predominantly influenced every sphere of life and the entire mankind. Due to the abrupt changes in academic, social and personal life students are at higher risk to develop psychological distress that could have a detrimental impact on their mental well-being. Although previously numerous researchers have studied multiple factors concerning students’ mental well-being, this coronavirus pandemic posed unique challenges concerning mental well-being due to fear of getting infected, social disconnectedness and uncertainty. Researchers on psychological implications could play an important role to devise effective coping strategies with empirical evidence. Based on an online survey, this study examined the impact of fear of being infected, and social isolation on university students’ mental well-being. Moreover, the role of psychological resilience as a coping strategy is also examined. This study proposes that in challenging times like the coronavirus pandemic, psychological resilience could promote mental well-being. This study’s findings emphasize on designing and implementing intervention programs for students at various forums.
1. Introduction
Human history corroborates that an outburst of any pandemic results in multiple human causalities, a large number of suspected patients, a wave of uncertainty and deep fear. The typical nature of any pandemic raises multiple challenges entailing various endeavors to find out workable strategies to minimize the negative consequences of such pandemics on human life (e.g; Agüero et al., Citation2011; Djalante et al., Citation2020; Faherty et al., Citation2019; Roy et al., Citation2020). Once, again, the world is passing through tough times as a novel type of coronavirus, named as COVID-19, initially emerged in Wuhan, China in December 2019, and has now spread globally. This sheer speed of the spread of this crisis and the unexpected increment in the quantity of cases has astonished and overpowered public health services (Wu & McGoogan, Citation2020). COVID-19 is caused by a beta coronavirus named SARS-CoV-2 that affects the lower respiratory tract (Sohrabi et al., Citation2020) and is mainly transmitted through respiratory droplets taking equal time for incubation and generation as the SARS coronavirus (Wilson & Chen, Citation2020). On 22 February 2020, WHO declared COVID-19, a public health emergency of international concern and later on, it declared it as a pandemic. By 21 September 2021, globally nearly 228 million confirmed cases and 4.6 million deaths are reported due to COVID-19 (World Health Organization, Citation2021).
Due to the rapid spread of COVID-19 pandemic across the globe, emergency steps are being taken by many countries in adherence to WHO guidelines in terms of ensuring public health measures. The lives of infected people, loved ones and the general public came into question because of the continual potential impacts of the COVID-2019 pandemic (Wilson & Chen, Citation2020). In this situation, detection of the virus at initial stages, prompt isolating and treating cases, contact tracing and social-distancing strategies, in line with the degree of risk, have been considered as the most effective strategies to curb infection spread (World Health Organization, Citation2021). Evasion of swarmed/crowded places is prescribed at each and every level and masks ought to be utilized by an individual to give a physical boundary that may assist with preventing of the spread of the infection. No doubt, social interactions are necessary to individuals’ well-being, but the pandemic characterizes social distancing as a prime preventive measure. Primarily, social isolation implies restricting individuals’ profoundly natural and evolutionarily hard-wired motivations for association (Zandifar & Badrfam, Citation2020). It is a common behaviour that when people feel insecure and upset, their normal requirement for close contact with others becomes more vital and critical. Any constrained isolation can build nervousness due to loneliness and uncertainty, which may cause mental disturbance (Brown et al., Citation2020). Due to social distancing and suspension of major routine activities, an individual’s life has been radically altered. (Singh & Singh, Citation2020). This reflects that “the flare-up of coronavirus illness might be upsetting for individuals, and consequently nervousness, fear and anxiety about a disease can be overpowering” (Centers for Disease (CDC) for Disease Control and Prevention, Citation2020). As development and spread of the virus might prompt psychological trouble, nervousness and fear in the general public may lead to harmful stereotypes (K. Shah et al., Citation2020). Hence, it is important to pay increased attention toward the mental well-being of general public associated with the rising magnitude and intensity of COVID-19 during this unprecedented time of uncertainty (Fan & Lu, Citation2020; Qiu et al., Citation2020; Rajkumar, Citation2020). Moreover, focusing on uplifting an individual’s mental well-being and psychological resilience appeared important to cope during difficult times through disregarding dangers toward adjustment (Masten, Citation2001) and to protect the capacity of an individual to respond (Aiello et al., Citation2011).
Overall, across the globe, the COVID-19 pandemic has posed various challenges concerning countries, societies and individuals. Pakistan is not an exception to this global crisis and has been ranked among the top countries badly hit by this pandemic. The first confirmed case of the corona virus infection in Pakistan was reported on February, 26, 2020 in Karachi and within a week, four more cases were confirmed from other areas of Pakistan. Immediately, after confirmation of the first case of COVID-19, the Government of Pakistan took preventive measures through enforcing partial lockdown and restricting non-essential business activities. However, due to the surge of the number of cases, the Government imposed complete lockdown nationwide on 22 March, 2020. So far, the total number of confirmed COVID-19 cases in Pakistan are 1,257,955 with 28,106 deaths across the country as of 11 October 2011, 2021, Citation2021 (Government of Pakistan (GOP), Citation2021). In Pakistan, this pandemic situation has represented a genuine threat to public well-being due to the suspension of their normal social life, fear of being infected, economic downturn and uncertainty related to the emergence of multiple variants of COVID-19. Moreover, the frequent lockdowns, sudden closure of academic institutions and multiple misinformation spreading regarding the nature and sources of this virus have created an environment of uncertainty and psychological distress. In addition, this health crisis has put immense pressure on Pakistan’s limited health facilities while convincing people to take all preventive measures to stay safe and psychologically strong to avoid any uncontrollable situation. This pandemic imposes a new experience for the general public of Pakistan with multiple psychological concerns. The young population seems to be more distressed due to abrupt changes in their academic, social and personal lives. This scenario poses numerous unanswered queries pertinent to COVID-19 pandemic, and consequently, this situation has immensely caused huge challenges in the lives of individuals across the globe. This issue calls for further research concerning the COVID-19 pandemic that may help create proof driven methodologies to diminish the unfavorable mental health effects on individuals’ well-being (K. Shah et al., Citation2020; C. Wang et al., Citation2020).
The study aims to investigate how fear of being infected and social isolation can affect the mental well-being of an individual. This research also aims to analyze how psychological resilience may moderate the nexus between social isolation and mental well-being of an individual. The contribution of this research toward relevant literature is threefold. First, this study is an original attempt to systematically examine the underlying relationship between fear, social isolation, mental well-being and psychological resilience variables in a single study in the context of the COVID-19 pandemic. Second, majority of the relevant literature are focused on China, Europe, USA and other developed countries; however, fewer studies are focused on the South Asian region and Pakistan in particular. Third, this research is focused on the students of higher educational institutes. Youth form the largest share of the total population in Pakistan, and contrary to other countries, the proportion of young patients of COVID-19 in Pakistan are higher relative to other countries. The remainder of this paper is structured as follows. The literature and hypothesis development are discussed in section 2. Section 3 presents the methodology. The results and key findings are discussed in section 4. Section 5 presents the research discussion. Section 6 finally concludes the study.
2. Background literature and hypotheses development
2.1. Mental well-being during pandemic
Major health crisis such as any pandemic is widely viewed as triggering adverse consequences on mental health of general population (Ravi, Citation2020). The prior literature documents mental well-being as key concern while examining the antecedents and consequences of any pandemic (Lau et al., Citation2008; Marais et al., Citation2014; Wickramage et al., Citation2018). Recent studies conducted across different contexts highlight that various aspects of mental wellbeing could be significantly influenced by the COVID-19 pandemic (Girdhar et al., Citation2020; Greenberg et al., Citation2020; Holmes et al., Citation2020; K. Shah et al., Citation2020). In this context, Lazarus and Folkman (Citation1984) transactional stress and coping theoretical perspective consider stress and coping as key attributes of health education and disease prevention. This is because the fear of developing an illness can provoke stressful reactions, particularly, how individuals cope with stress may promote or inhibit healthy practices (Glanz & Schwartz, Citation2008). Drawing impetus from Lazarus and Folkman (Citation1984) transactional stress and coping theoretical perspective, the present study emphasizes on the capacity of coping up with stressful events (e.g COVID-19 pandemic). When an individual encounters potential threats or uneasiness (social isolation) due to the fear of being infected, his or her ability to alter the situation and manage negative emotional reactions through coping efforts (psychological resilience) helps to boost mental well-being (Folkman & Moskowitz, Citation2000).
2.2. Fear of being infected and social isolation
Fear refers to a feeling of anxiety pertinent to occurrence of something undesired or the safety risk of someone. The development of fear among the general public in a pandemic situation is considered as a common phenomenon, and it has been the issue of investigation from multiple dimensions (Davis et al., Citation2014; Tzeng & Yin, Citation2008; Vance, Citation2011). Generally, during a pandemic, the fear of being infected leads toward social isolation (Anderson et al., Citation2020; Wilder-Smith & Freedman, Citation2020). Social isolation could be defined as the distancing of an individual from his or her circle of desired or needed interactions with other people (Biordi & Nicholson, Citation2013). It is believed that in order to curb the rapid spread of infectious diseases that transfer through respiratory transmission (droplet infection), social isolation acts as a preventive measure that yields better results (WHO 2020). In a similar vein, De Serres et al. (Citation2010) stressed that the call for isolation of H1N1 infection carriers can be comprehended as an expression of fear of the disease because of the expanding and increasing risk of infection. Epstein et al. (Citation2008) suggested self-isolation and spatial flight as just two of numerous potential activities that fear-infected people may take during the disease that can be transmitted from the other person. During the ongoing COVID-19 pandemic, recent studies have offered empirical evidence about promoting social isolation to minimize the magnitude and intensity of virus infected cases (Hellewell, 2020; Sen-Crowe et al., Citation2020). Based on these studies, it is likely that during the period of the pandemic, due to fear of being infected, an individual will lead toward social isolation. Therefore, it is hypothesized that:
H1: During the period of COVID-19 pandemic, there is a positive relationship between fear of being infected and social Isolation.
2.3. Social isolation and mental well-being
Although allowing minimum social interaction among the general public is referred as the main preventive measure to curb the spread of infectious diseases (Lee et al., Citation2010; L. Wang et al., Citation2012) social isolation embedded with fear, uncertainty and helplessness may trigger multifaceted mental issues (Cornwell & Waite, Citation2009; Leigh-Hunt et al., Citation2017; Matthews et al., Citation2015). While an individual’s efforts to maintain minimum social interaction could produce positive outcome in the shape of lessening the spread of contagious disease, however, the feeling of social disconnectedness itself could pose serious threats to an individuals’ mental well-being. Mental well-being could be elucidated in terms of happiness and positive functioning (Ryan & Deci, Citation2001). Whereas social isolation refers to when social networks are disengaged, without order and isolation from relations with others may have a detrimental impact on an individual’s mental well-being (Pinedo et al., Citation2021). Recent research on the pandemic sheds light on the adoption of preventive measures involving social isolation and its negative association with mental well-being (Adhikari et al., Citation2020; Ho et al., Citation2020; Yao et al., Citation2020; Zandifar & Badrfam, Citation2020). Drawn from these studies conducted across different contexts, it is likely that during the period of the pandemic, social isolation could have a negative association with an individual’s mental well-being. Thus, it is hypothesized that:
H2: During the period of COVID-19 pandemic, there is negative relationship between social isolation and mental well-being of an individual.
2.4. Fear of being infected and mental well-being
Extent literature examined different types of fear and its underlying association with the mental well-being of an individual. Mental well-being has been studied in relation to multiple dimensions such as fear of terror (A Shah et al., Citation2018), fear of crime (Cornaglia et al., Citation2014), fear of missing out (Elhai et al., Citation2016), unemployment (Bünnings et al., Citation2017) and personal aging (Kercher et al., Citation1988). Fear in any form could trigger various psychological issues including uneasiness and mental pain/disorder. It has been argued that in most of the incidents, fear could have a notable impact on mental well-being relative to physical wellbeing (Pearson & Breetzke, Citation2014). The type of fear that predominantly determines the causes of the creation of that fear (Dhir et al., Citation2018) and subsequently, preventive measures are identified to mitigate that fear. Prior studies show that fear of getting infected during any pandemic could have a significant impact on the well-being of an individual (Blakey & Abramowitz, Citation2017; Jeong et al., Citation2016). The fear of being infected is generally observed to be higher during a pandemic due to the scale of suspected/confirmed cases, uncertainty, rumors and stigma that collectively contribute negatively toward an individual’s mental well-being. Recent studies indicate that fear of being infected during the COVID-19 pandemic could have a negative association with the mental well-being of an individual (Dong & Bouey, Citation2020; Lin, Citation2020; Mamun & Griffiths, Citation2020). Therefore, it is likely that fear of being infected during the COVID-19 pandemic could negatively influence the mental well-being of an individual. Hence, it is hypothesized that:
H3: During the period of COVID-19 pandemic, there is negative relationship between fear of being infected and mental well-being of an individual.
2.5. Social Isolation as a Mediator
Extant literature corroborates the significant relationship between social isolation and mental well-being (Adhikari et al., Citation2020; Ho et al., Citation2020; Leigh-Hunt et al., Citation2017; Matthews et al., Citation2015; Yao et al., Citation2020; Zandifar & Badrfam, Citation2020). Similarly, relevant literature also documents the significant relationship between fear and social isolation (De Serres et al., Citation2010; Hellewell, 2020; Sen-Crowe et al., Citation2020). However, prior studies have not yet investigated the role of social isolation in mediating the relationship of fear of getting infected and mental well-being. It has been argued that fear can effectively persuade individuals to take prescribed practices and desired behaviors (Gore & Bracken, Citation2005). As Witte (Citation1992) stressed that when an individual has the feeling of personal susceptibility to a big threat and emotionally becomes worried about it (i.e. getting infected by COVID-19), they are more inclined to control the danger conveyed by messages to them and accept the advocated response (Wilder-Smith & Freedman, Citation2020). On one hand, social disconnectedness (social isolation) could result in a significant risk factor that negatively affects the physical and mental well-being of an individual (Cacioppo & Cacioppo, Citation2014). On the other hand, social integration and ties could significantly contribute toward a better state of mental health (Seeman,1996). Turan et al. (Citation2016) used social isolation as a mediator between HIV-related internalized stigma and adherence for women living with HIV. Du Prel et al. (Citation2014) also used social isolation as a mediator between education and depressive symptom. Therefore, it is likely that social isolation mediates the relationship between fear of being infected and mental well-being, and consequently, it is hypothesized that:
H4: During the period of COVID-19 pandemic, social isolation mediates the relationship between fear of being infected and mental well-being of an individual.
2.6. Psychological Resilience as a Moderator
Psychological resilience could be conceptualized as an individuals’ capacity to cope successfully during significant change, threatening circumstances or adversity (Lee & Cranford, Citation2008). It is believed that an individual starts to get mentally disturbed when they do not have positive inputs within inside during challenging events of their life. The present study conceptualizes psychological resilience of the individual as a positive input during difficult times. Recent studies focused on the COVID-19 pandemic give evidence that resilience is a core characteristic to deal with a stressful situation and to bounce back with a higher positive response (Polizzi et al., Citation2020; Shaw, Citation2020). Friborg et al. (Citation2006) in their experimental study used resilience, as a moderator with pain and stress, and reported that although perceived pain and stress significantly increased throughout the experimental session, yet people scored high on the resilience factor, indicating less pain and stress. Resilience moderated miserable symptom intensity in individuals, who experienced childhood abuse or other ordeals—both as a main effect and an interaction with ordeal exposure (Wingo et al., Citation2010). Moreover, resilience might be responsive to external manipulation and could offer a potential focus for treatments and interventions (Arrogante et al., Citation2015; Wingo et al., Citation2010). Hao et al. (Citation2015) moderated resilience with stress and burnout and found that resilience could serve as a buffer to mitigate the adverse effects of work stress and suggested that resilience could be a constructive characteristic for reducing excessive pressure and fighting back in times of adversity. In line with the relevant literature, it is likely that when experiencing a negative emotion of social isolation, the resilient individual can bounce back to a calmer pace (mental well-being) if experiencing positive emotions (psychological resilience). Consequently, it is hypothesized that:
H5: During the period of COVID-19 pandemic, psychological resilience moderates the relationship of social isolation and mental well-being with a buffering effect.
3. Methods
3.1. Procedure
The study is quantitative in nature and a cross-sectional research design was undertaken. The research participants were asked to complete an online survey during the period of 15 March 2020 to 14 April 2020. The online survey included an information section that provided details about the purpose of the research and ethical considerations concerning the confidentiality and privacy pertaining to data collection. The selection of an online survey was informed by two main considerations. Firstly, the degree of Internet connectivity is high among the sample of current participants in the study (Ahmad, Citation2020). Secondly, the data were collected during the lockdown period in the country when physical access to the participants was strictly restricted. Thus, reaching out to study participants via an online survey was the appropriate method in these times (Pinedo et al., Citation2021). Details about the universities were obtained from website of Higher Education Commission of Pakistan. Later on, an e-mail with a survey link was sent to all the concerned administrative authorities of universities with a request to share the survey link with their students.
3.2. Participants
The participants of the present study comprised of students hailing from chartered universities in Pakistan. Students as research participants were sampled based on three key considerations. Firstly, chartered universities have campuses located across all provinces of Pakistan, so it was the most suitable strategy to reach out to a large number of students located across the country. Secondly, after the emergence of initial COVID-19 cases in Pakistan, the Higher Education Commission of Pakistan issued directives to immediately close all educational institutions. This resulted in students facing the sudden suspension of their academic learning and routine life. Students were considered at high risk during pandemic due to abrupt changes in their circumstances (Van et al., Citation2010). Thirdly, despite the growing concern related to the possibility of developing psychological issues amongst the youth, there is a lack of empirical research that focused on the mental wellbeing of students during the COVID-19 pandemic (Shah et al., Citation2021). Therefore, it would be worthy to study those psychological factors that could influence students’ mental well-being. In terms of determining the adequate sample size, G* power 3.1.9.2 approach was used that identified minimum sample size of 134 participants to validate the present study findings (Faul et al., Citation2007). Total 714 students responded to the online survey. The demographic details of the participants are summarized in .
Table 1. Demographic Details
3.3. Measures
3.3.1. Fear of Being Infected
This scale was adapted from Zhang, King, and Chang (2015) and comprised of five items. Respondents were asked to indicate the degree to which they agree with the statement based on the Likert scale ranging from 1 (Strongly disagree) to 5 (Strongly agree): I do not want to leave the house because of the risk of getting infected by COVID- 19 pandemic; I am concerned that I may get sick from COVID-19 pandemic during the next 6 months; I am feeling anxious about COVID-19 pandemic; I am concerned that someone in my immediate family may get sick from COVID-19 pandemic during the next 6 months; I am scared about getting infected by COVID-19 pandemic. This scale was reliable with Cronbach alpha of 0.823.
3.3.2. Social Isolation
This scale was adopted from Hawthorne (Citation2006) and comprised of six items. Respondents were asked to indicate the degree to which each statement fits to them based on Likert scale ranging from 1 (Frequently or always) to 5 (Not at all): It has been easy to relate others; I felt isolated from other people; I have someone to share my feelings with; I found it easy to get in touch with others when I needed others to felt they had to help me; When with other people, I feel separate from them; and I felt alone and friendless. Negatively worded items were reversed in terms of weighting. The scale was reliable with Cronbach alpha of 0.870.
3.3.3. Mental well-being
This scale was adopted from Tennant et al. (Citation2007) and comprised of 14 items. Respondents were asked to indicate the degree to which each statement fits to them based on Likert scale ranging from 1 (Not at all) to 5 (Frequently or always): I have been feeling optimistic about the future; I have been feeling useful; I have been feeling relaxed; I have been feeling interested in other people; I have been dealing with problems well; I have been thinking clearly; I have been feeling good about myself; I have been feeling close to other people; I have been feeling confident; I have been able to make up my own mind about things, I have been feeling loved; I have been interested in new things; I have been feeling cheerful. The scale was reliable with Cronbach alpha of 0.868.
4. Psychological resilience
This scale was adopted from Connor and Davidson (Citation2003) and comprised of 10 items. Respondents were asked to indicate the degree to which each statement fits to them based on Likert scale ranging from 1 (Not true at all) to 5 (True nearly all the time): I am able to adapt when changes occur; I can deal with whatever comes my way; I try to see the humorous side of things when I am faced with problems; Having to cope with stress can make me stronger; I tend to bounce back after illness, injury or other hardships; I believe I can achieve my goals, even if there are obstacles; Under pressure, I stay focused and think clearly; I am not easily discouraged by failure; I think of myself as a strong person when dealing with life’s challenges and difficulties; I am able to handle unpleasant or painful feelings like sadness, fear, and anger. The scale was reliable with Cronbach alpha of 0.847.
4.1. Data analysis
The preliminary data analysis was performed by SPSS 23. In order to further test the validity, reliability, significance and relevance of path coefficients, the partial least square (PLS-SEM) approach was applied by using SMART PLS version 3.0 (Ringle et al., Citation2015). The present study applied PLS-SEM based on the rationale that it facilitates researcher in estimating research models with multiple constructs, indicator variables and structural paths without setting distributional assumptions on the data (Hair et al., Citation2019) and providing causal explanations (Sarstedt et al., Citation2017). In order to avoid the possible destructions in data analysis, the findings from the preliminary analysis reveal that the present study has no missing values as the online survey reduced the occurrence of missing data (Hair et al., Citation2017). Common method bias was not an issue and the findings of multivariate normality test reveal that the data were slightly non-normal as PLS-SEM is a non-parametric statistical method and does not require the data to be normally distributed.
5. Results
represents the key indicators of the measurement model. indicates that the outer loadings are satisfactory and are greater than 0.50. Hence, it establishes the indicator reliability (Hair et al., Citation2017). The values of composite reliability (CR) are higher than the recommended value of 0.7. Hence, it indicates that the establishment of internal consistency is reliable (Hair et al., Citation2006). Average variance extracted (AVE) values are greater than 0.5. Hence, it establishes the convergent validity (Hair et al., Citation2006). Present study follows the suggestion of Henseler et al. (Citation2015) and assesses the discriminant validity in the form of Heterotrait-Monotrait ratio of correlations. In this regard, indicates that all the HTMT values are less than 0.85 as the respondents understood that the five constructs are distinct. The discriminant validity has been ascertained (Henseler et al., Citation2015).
Table 2. Outer loadings, composite reliability & average variance extracted
Table 3. Discriminant validity
Having established reliable and valid results from the measurement model, the next step is to analyze the structural model. The present study has employed the bootstrapping method with 5000 resamples (Hair et al., Citation2017) using Bias-Corrected and Accelerated (BCa) Bootstrap with one-tailed test type where the significance level is 0.05.
specifies that fear is positively and significantly associated with social isolation β =0.215, t-value = 5.258, p < 0.05 (Hair et al., Citation2017) with CI [0.128, 0.285] not overlapping the zero value in between (Preacher & Hayes, Citation2008). Hence, indicating the acceptance of H1, the relationship has small effect size, F2 = 0.083 (Wong, Citation2013).
Table 4. Significance and relevance of path coefficients
Social isolation and fear are negatively and significantly associated to mental well-being β = −0.521, t-value = 10.590, p < 0.05) (β =—0.243, t-value = 5.721, p < 0.05) (Hair et al., Citation2017) with CI [−0.213, −0.088] [−0.204, −0.104] not overlapping the zero value in between (Preacher & Hayes, Citation2008), hence indicating the acceptance of H2 & H3, respectively. The relationship of social isolation and mental well-being has a large effect size (F2 = 0.399) (Wong, Citation2013) while the relationship of fear and mental well-being has a medium effect size F2 = 0.152, (Wong, Citation2013).
The mediating effect of social isolation on the relationship that exists between fear and mental well-being indicate that the indirect effect is significant with β = −0.135, t- value 3.253 and p < 0.05 (Hair et al., Citation2017) with LCI = −0.052 and UCI = −0.018 not overlapping the zero value in between (Preacher & Hayes, Citation2008). This indicates a negative mediating effect of social isolation that is statistically significant to accept and supporting H4.
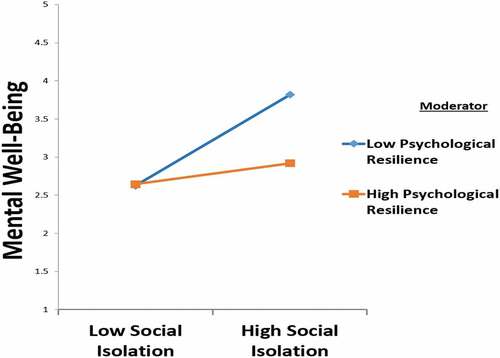
The study corroborates that the psychological resilience moderates the relationship between social isolation and mental well-being β = −0.124, t-value = 3.498 and p < 0.05 (Hair et al., Citation2017). Hence, it accepts and supports H5. As the significance level of the present study pertains to the coefficients is 0.05 (i.e., 95% confidence level) so by employing 95% bias-corrected bootstrap, CI of the interaction term’s effect with psychological resilience is [−0.281, −0.080]. This indicates that the confidence interval has not overlapped the zero value (Preacher & Hayes, Citation2008). Hence, this represents the significant moderating effect of psychological resilience between social isolation and mental well-being. The interaction effect has a small effect size F2 = 0.031, (Wong, Citation2013).
depicts the interaction plot, which holds the buffering effect where psychological resilience reduces the impact of social isolation on mental well-being. Or, in other words, an increase in the moderator would decrease the effect of social isolation on mental well-being. Psychological resilience contributes to adjustment as in the presence of psychological resilience, individuals are less affected by social isolation during COVID-19 pandemic.
The model of the study explains 48.6% of total variance in social isolation while 52.7% in mental well-being. This indicates that social isolation and mental well-being exhibit a moderate level of R2(Chin, Citation1998). The study employed a blindfolding procedure which re-uses the sample by omitting a part of a data matrix with omission distance 7 (Hair et al., Citation2013) that calculates the Stone-Geisser’s Q2 value (Geisser, Citation1975; Stone, Citation1974). This represents an evaluation criterion for the cross-validated predictive relevance of the PLS path model. The result indicates the predictive relevance of the model as the Q2 value of all endogenous variables is above zero, Social Isolation = 0.231, Mental Well-Being = 0.269 (Henseler et al., Citation2009) demonstrating moderate level of predictive relevance (Hair et al., Citation2019).
The present study follows the suggestion of Shmueli et al. (Citation2016. Using the PLS Predict check the model’s out of sample predictive power of mental well-being is 10fold and 10 repetitions. indicates that all the errors of the PLS model of mental well-being indicators (Key Endogenous Construct) were lower than the LM model thus the study model has strong predictive power (Shmueli et al., Citation2019).
Table 5. Key endogenous construct (mental well-being)—indicators predictive relevance
6. Discussion
The COVID-19 pandemic exposes the population at large with unpredictability and uncertainty, so it raises serious challenges concerning deteriorating mental health. In response to the call for taking serious measures toward mental well-being issues (Ravi, Citation2020), a number of recent studies tried to examine various issues concerning mental well-being across a diverse context. (Armitage & Nellums, Citation2020; Greenberg et al., Citation2020; Liew et al., Citation2020; Zheng et al., Citation2020). Within the framework of transactional theory of stress and coping (Lazarus & Folkman, Citation1984), the study focuses on the relationships among stressful conditions related to the fear of getting infected, confinement as a form of social isolation acting as a preventive measure, psychological resilience as a coping strategy, and sustaining mental well-being during the pandemic amongst university students in Pakistan. A major consideration concerning the consequences of encountering negative elements concern mental well-being during the pandemic. This signposts effective coping strategies that examine these negative elements in light of transactional theory of stress and coping perspectives which offer useful insights to identify the most effective coping strategy to mitigate cognitive distress. The study findings validate the relevancy of transactional stress and coping concepts as a theoretical perspective (Lazarus & Folkman, Citation1984).
The findings from the study revealed that the fear of being infected could significantly enhance social isolation amongst university students during the period of the COVID-19 pandemic. This finding is in line with recent studies, which documents empirical evidence toward encouraging social isolation to minimize the magnitude and intensity of number of COVID-19 infected cases (Hellewell, 2020; Sen-Crowe et al., Citation2020). Similarly, in the context of H1N1 pandemic 2009, De Serres et al. (Citation2010) stressed that the call for isolation of H1N1 infection carriers can be comprehended as an expression of fear of the disease because of the expanding and increasing risk of infection. The disease control path is a good mechanism to explain how fear aroused social isolation in the COVID-19 pandemic as it can motivate individuals to take preventative actions that are recommended. The study findings corroborate that students with a higher level of fear of getting infected avoided social interaction.
This study also demonstrates that there is a significant negative relationship between social isolation and mental well-being of students during the period of COVID-19 pandemic. This finding validates the extant literature that sheds light on the adoption of social disconnectedness (social isolation) as preventive measures, but also raises concerns pertinent to potential negative consequences of social isolation on mental health (Adhikari et al., Citation2020; Ho et al., Citation2020; Yao et al., Citation2020; Zandifar & Badrfam, Citation2020). Hence, it can be inferred that social connectivity is an individual’s basic need that is fulfilled through a close social association with others. Whereas social disconnectedness is embedded with fear, uncertainty and helplessness that may trigger a multifaceted of mental issues (Cornwell & Waite, Citation2009; Leigh-Hunt et al., Citation2017; Matthews et al., Citation2015). Primarily, there is higher need of social connection during the pandemic to reduce negative symptomology and facilitate adaptation (Saltzman et al., Citation2020). Otherwise, this results in loneliness due to social distancing that may hamper mental and emotional health significantly (Cecchetto et al., Citation2021. Pinedo et al., Citation2021). Mental well-being embedded in maintaining social ties affords individuals the ability to live, work and appreciate diversion in a network where one has a feeling of belongingness and support, and the capacity to make meaningful contributions.
Moreover, this study highlights that the fear of being infected is significantly reported as a negative relationship with the mental well-being of students during COVID-19 pandemic. This finding is consistent with the previous literature in terms of highlighting that fear could trigger anxiety, insecurity, and vagueness that negatively influence mental well-being of an individuals. (Blakey & Abramowitz, Citation2017; Dhir et al., Citation2018; Jeong et al., Citation2016; L. Wang et al., Citation2012). Recent studies carried out in the context of COVID-19 pandemic highlight that rapidly increasing number of virus infected cases and the emergence of multiple variants of COVID-19 have created an atmosphere of fear that negatively influence the mental well-being of an individual (Dong & Bouey, Citation2020; Mamun & Griffiths, Citation2020; Thangaraj et al., Citation2021; Vassallo et al., Citation2021). In the current pandemic scenario, the fear of getting infected is perceived as posing some immediate harm or loss that could be labeled as a threat or challenge to deal with ((Lazarus & Folkman, Citation1984). Individuals in this worrisome time of the pandemic appear to be afraid, confused and overwhelmed by the constantly changing guidelines, misinformation and fear of emerging multiple variants that could pose serious threats toward the mental well-being of people and society.
Furthermore, the study findings indicate that social isolation negatively mediates the relationship between fear and mental well-being, that is, fear is positively associated with social isolation and in turn social isolation is negatively associated with mental well-being. This finding can also be validated from the work of Turan et al. (Citation2016) where social isolation mediates the relationship between HIV-related internalized stigma and adherence for women living with HIV. Likewise, the outbreak of coronavirus disease is stressful for people as the fear of getting infected and uncertainty about the future can can be overwhelming leading them to self-isolate as a preventive measure for avoiding the risk of infection. Meanwhile, this isolation causes strong negative emotions of anxiety, sadness, loss of interest, frustration, irritability, anger, restlessness, helplessness, social exclusion, fatigue and depression (Cacioppo & Cacioppo, Citation2014). All these factors appear relevant and justifiable during the ongoing pandemic, as there have been wide-scale death causalities, rapid adjustments to way of life (e.g., study, social interaction, work) and unsettled future plans owing to travel restrictions. Moreover, social isolation measures to mitigate the spread of virus transmission ultimately effects the mental well-being of an individual.
In addition, we argue that through enhanced psychological resilience, an individual may reduce the negative impact of social isolation on his/her mental well-being. This finding validates the moderating role of psychological resilience between the relationship of social isolation and mental wellbeing. As the scale of the pandemic and its far-reaching implications continue to unfold globally including Pakistan, it is normal for people to embrace multiple and conflicting thoughts, feelings, assumptions and reactions towards social isolation. However, an increase in psychological resilience may assist individuals in coping with pressure and stress, adjust effectively to any mishaps, bounce back after negative emotional experiences, and reduce negativity through positive reframing of the situation (Burton et al., Citation2010; Graham, Citation2015; Tugade & Fredrickson, Citation2004). During the COVID-19 pandemic, social isolation may make an individual more vulnerable to psychological ill-being, but psychological resilience may help in boosting mental well-being (Osimo et al., Citation2021). Primarily, psychological resilience may act as a buffer against the negative consequences of social isolation on mental well-being and may enable an individual to prosper amidst the challenging times of the pandemic.
7. Conclusion
The study concludes that there is a dire need to address the negative effects of the fear of getting infected and the effects of social isolation during any health crisis on an individual’s mental well-being. Thus, by promoting the effectiveness of psychological resilience, this may help to cope with any uncertain and stressful scenario. It is noteworthy that due to the widespread penetration of the number of cases reported in Pakistan, the fear of getting infected may exhibit through different behaviors—from daily life annoyance to life threatening risks. Although social isolation as a preventive measure is effective in minimizing the rapid transmission of the virus, the negative consequences of this social disconnectedness hinders an individuals’ innate desire to offer and receive social support through maintaining close interactions with social networks. It is worthy to say that amidst this global health crisis, through exercising psychological resilience, students can effectively manage this challenging situation that can enhance their mental well-being.
Despite these valuable insights, the present study is subject to some limitations. First, caution is needed to draw any inferences concerning the causal relationships among the study variables. This is due to the employment of a cross-sectional research design in this study. Future studies may adopt a longitudinal research design to validate underlying causal relationships among study variables. Second, the study solely focuses on university students whilst other segments of the population are ignored but also subject to similar psychological challenges. Therefore, future studies should cover other segments of the population including work employees/businessman, daily wage workers and elderly people to enhance our understanding of the underlying phenomenon. Third, the present study used social isolation as a mediator and psychological resilience as a moderator, but future studies might include other mediating variables (e.g., stress or depression) and moderating variables (e.g., emotional intelligence, family support or perceived knowledge) in the model to offer a wider understanding towards mental wellbeing during a pandemic.
Regardless of these underlying limitations, the study offers important implications concerning theory, practice and policy to academics, practitioners, and policymakers based on empirical evidence. The study validates the relevance and application of Transactional theory of stress and coping during a health crisis. The empirical findings from this study are generalizable across those developing countries that are similar in context related to the effects of the pandemic on similar populations. It is worthy to mention as other researchers have echoed (Pinedo et al., Citation2021; Roy et al., Citation2020) that while social distancing could be necessary during the pandemic, it needs to be dealt with caution. This implies that offering psycho-education and counselling may be an effective counter strategy. This is because social disconnectedness and exclusion could invite psychological distress that hampers mental well-being. Policymakers should plan and implement intervention programs that promote psychological resilience for students and the general public alike, in order to alleviate the negative impact of psychological sufferings on an individuals’ mental well-being during pandemic situations.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
Notes on contributors
Sobia Shafaq Shah
Sobia Shafaq Shah is an Associate Professor at the Institute of Business Administration, University of Sindh, Pakistan. She earned her Ph.D in Business Administration at Anglia Ruskin University, United Kingdom. The psychological distress among university students during pandemic drew her attention to study key aspects concerning students’ mental well-being. One of her recent publications pertinent to the COVID-19 pandemic, and students’ online learning is published in the Journal of Revista de Psicodidactica. She has been involved in numerous research projects and her research interest focuses on management, finance and higher education. Co-authors collaborated with the preparation of this research article in different capacities.
References
- Adhikari, S. P., Meng, S., Wu, Y. J., Mao, Y. P., Ye, R. X., Wang, Q. Z., & Zhou, H. (2020). Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: A scoping review. Infectious Diseases of Poverty, 9(1), 1–20. https://doi.org/10.1186/s40249-020-00646-x
- Agüero, F., Adell, M. N., Giménez, A. P., Medina, M. J. L., & Continente, X. G. (2011). Adoption of preventive measures during and after the 2009 influenza A (H1N1) virus pandemic peak in Spain. Preventive Medicine, 53(3), 203–206. https://doi.org/10.1016/j.ypmed.2011.06.018
- Ahmad, S. (2020). Political behavior in virtual environment: Role of social media intensity, internet connectivity, and political affiliation in online political persuasion among university students. Journal of Human Behavior in the Social Environment, 1–17. https://doi.org/10.1080/10911359.2019.1698485
- Aiello, A., Young‐Eun Khayeri, M., Raja, S., Peladeau, N., Romano, D., Leszcz, M., … Bernard Schulman, R. (2011). Resilience training for hospital workers in anticipation of an influenza pandemic. Journal of Continuing Education in the Health Professions, 31(1), 15–20. https://doi.org/10.1002/chp.20096
- Anderson, R. M., Heesterbeek, H., Klinkenberg, D., & Hollingsworth, T. D. (2020). How will country-based mitigation measures influence the course of the COVID-19 epidemic? The Lancet, 395(10228), 931–934. https://doi.org/10.1016/S0140-6736(20)30567-5
- Armitage, R., & Nellums, L. B. (2020). COVID-19 and the consequences of isolating the elderly. The Lancet. Public Health, 5(5), e256. https://doi.org/10.1016/S2468-2667(20)30061-X
- Arrogante, O., Perez-Garcia, A. M., & Aparicio-Zaldivar, E. G. (2015). Psychological well-being in nursing: Relationships with resilience and coping. Enfermeria Clinica, 25(2), 73–80. https://doi.org/10.1016/j.enfcli.2014.12.009
- Biordi, D. L., & Nicholson, N. R. (2013). Social isolation. Chronic Illness: Impact and Intervention, 85–115. 2014.12.009. https://doi.org/10.1016/j.enfcli
- Blakey, S. M., & Abramowitz, J. S. (2017). Psychological predictors of health anxiety in response to the Zika virus. Journal of Clinical Psychology in Medical Settings, 24(3–4), 270–278. https://doi.org/10.1007/s10880-017-9514-y
- Brown, C., Keene, A. R., Hooper, C. R., & O’Brien, A. (2020). Isolation of patients in psychiatric hospitals in the context of the COVID-19 pandemic: An ethical, legal, and practical challenge. International Journal of Law and Psychiatry, 71, 101572. https://doi.org/10.1016/j.ijlp.2020.101572
- Bünnings, C., Kleibrink, J., & Weßling, J. (2017). Fear of unemployment and its effect on the mental health of spouses. Health Economics, 26(1), 104–117. https://doi.org/10.1002/hec.3279
- Burton, N. W., Pakenham, K. I., & Brown, W. J. (2010). Feasibility and effectiveness of psychosocial resilience training: A pilot study of the READY program. Psychology, Health & Medicine, 15(3), 266–277. https://doi.org/10.1080/13548501003758710
- Cacioppo, J. T., & Cacioppo, S. (2014). Social relationships and health: The toxic effects of perceived social isolation. Social and Personality Psychology Compass, 8(2), 58–72. https://doi.org/10.1111/spc3.12087
- Cecchetto, C., Aiello, M., Gentili, C., Ionta, S., & Osimo, S. A. (2021). Increased emotional eating during COVID-19 associated with lockdown, psychological and social distress. Appetite, 160, 105122. https://doi.org/10.1016/j.appet.2021.105122
- Centers for Disease (CDC) for Disease Control and Prevention (2020) https://www.cdc.gov/mmwr/Novel_Coronavirus_Reports.html
- Chin, W. W. (1998). The partial least squares approach to structural equation modeling. Modern Methods for Business Research, 295(2), 295–336.
- Connor, K. M., & Davidson, J. R. (2003). Development of a new resilience scale: The Connor‐Davidson Resilience Scale (CD‐RISC). Depression and Anxiety, 18(2), 76–82. https://doi.org/10.1002/da.10113
- Cornaglia, F., Feldman, N. E., & Leigh, A. (2014). Crime and mental well-being. Journal of Human Resources, 49(1), 110–140. https://doi.org/10.3368/jhr.49.1.110
- Cornwell, E. Y., & Waite, L. J. (2009). Social disconnectedness, perceived isolation, and health among older adults. Journal of Health and Social Behavior, 50(1), 31–48. https://doi.org/10.1177/002214650905000103
- Davis, M., Lohm, D., Flowers, P., Waller, E., & Stephenson, N. (2014). “We became sceptics”: Fear and media hype in general public narrative on the advent of pandemic influenza. Sociological Inquiry, 84(4), 499–518. https://doi.org/10.1111/soin.12058
- De Serres, G., Rouleau, I., Hamelin, M.-E., Quach, C., Skowronski, D., Flamand, L., Boulianne, N., Li, Y., Carbonneau, J., Bourgault, A.-M., Couillard, M., Charest, H., & Boivin, G. (2010). Contagious period for pandemic (H1N1) 2009. Emerging Infectious Diseases, 16(5), 783. https://doi.org/10.3201/eid1605.091894
- Dhir, A., Yossatorn, Y., Kaur, P., & Chen, S. (2018). Online social media fatigue and psychological wellbeing—A study of compulsive use, fear of missing out, fatigue, anxiety and depression. International Journal of Information Management, 40, 141–152. https://doi.org/10.1016/j.ijinfomgt.2018.01.012
- Djalante, R., Shaw, R., & DeWit, A. (2020). Building resilience against biological hazards and pandemics: COVID-19 and its implications for the Sendai framework. Progress in Disaster Science, 6, 100080. https://doi.org/10.1016/j.pdisas.2020.100080
- Dong, L., & Bouey, J. (2020). Public mental health crisis during COVID-19 pandemic, China. Emerging Infectious Diseases, 26(7), 7. https://doi.org/10.3201/eid2607.200407
- Du Prel, J.-B., Mario Iskenius, RichardPeter, R., & Iskenius, M. (2014). Are effort–reward imbalance and social isolation mediating the association between education and depressiveness? Baseline findings from the lidA § -study. International Journal of Public Health, 59(no. 6), 945–955. https://doi.org/10.1007/s00038-014-0613-3
- Elhai, J. D., Levine, J. C., Dvorak, R. D., & Hall, B. J. (2016). Fear of missing out, need for touch, anxiety and depression are related to problematic smartphone use. Computers in Human Behavior, 63, 509–516. https://doi.org/10.1016/j.chb.2016.05.079
- Epstein, J. M., Parker, J., Cummings, D., Hammond, R. A., & Galvani, A. P. (2008). Coupled contagion dynamics of fear and disease: Mathematical and computational explorations. PLoS One, 3(12), e3955. https://doi.org/10.1371/journal.pone.0003955
- Faherty, L. J., Schwartz, H. L., Ahmed, F., Zheteyeva, Y., Uzicanin, A., & Uscher-Pines, L. (2019). School and preparedness officials‘ perspectives on social distancing practices to reduce influenza transmission during a pandemic: Considerations to guide future work. Preventive Medicine Reports, 14, 100871. https://doi.org/10.1016/j.pmedr.2019.100871
- Fan, X., & Lu, M. (2020). Testing the effect of perceived social support on left-behind children’s mental well-being in mainland China: The mediation role of resilience. Children and Youth Services Review, 109, 104695. https://doi.org/10.1016/j.childyouth.2019.104695
- Faul, F., Erdfelder, E., Lang, A. G., & Buchner, A. (2007). G* Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39(2), 175–191. https://doi.org/10.3758/BF03193146
- Folkman, S., & Moskowitz, J. T. (2000). Positive affect and the other side of coping. American Psychologist, 55(6), 647–654. https://doi.org/10.1037/0003-066X.55.6.647
- Friborg, O., Hjemdal, O., Rosenvinge, J. H., Martinussen, M., Aslaksen, P. M., & Flaten, M. A. (2006). Resilience as a moderator of pain and stress. Journal of Psychosomatic Research, 61(2), 213–219. https://doi.org/10.1016/j.jpsychores.2005.12.007
- Geisser, S. (1975). A new approach to the fundamental problem of applied statistics. Sankhyā. The Indian Journal of Statistics, Series B, 385–397. https://www.jstor.org/stable/25051975
- Girdhar, R., Srivastava, V., & Sethi, S. (2020). Managing mental health issues among elderly during COVID-19 pandemic. Journal of Geriatric Care and Research, 7, 1.
- Glanz, K., & Schwartz, M. D. (2008). Stress, coping, and health behavior. In K. Glanz, B. K. Rimer, & K. Viswanath (Eds.), Health Behavior and Health Education: Theory, Research, and Practice. John Wiley and Sons.
- Gore, T. D., & Bracken, C. C. (2005). Testing the theoretical design of a health risk message: Reexamining the major tenets of the extended parallel process model. Health Education & Behavior, 32(1), 27–41. https://doi.org/10.1177/1090198104266901
- Government of Pakistan (GOP). (2021). //covid.gov.pk/stats/Pakistan.
- Graham, L. J. (2015). Integration of the interaction model of client health behavior and transactional model of stress and coping as a tool for understanding retention in HIV care across the lifespan. Journal of the Association of Nurses in AIDS Care, 26(2), 100–109. https://doi.org/10.1016/j.jana.2014.11.009
- Greenberg, N., Docherty, M., Gnanapragasam, S., & Wessely, S. (2020). Managing mental health challenges faced by healthcare workers during covid-19 pandemic. BMJ, 368. https://doi.org/10.1136/bmj.m1211
- Hair, J. F., Babin, B. J., & Krey, N. (2017). Covariance-based structural equation modeling in the journal of advertising: Review and recommendations. Journal of Advertising, 46(1), 163–177. https://doi.org/10.1080/00913367.2017.1281777
- Hair, J. F., Black, W. C., Babin, B. J., Anderson, R. E., & Tatham, R. L. (2006). Multivariate data analysis. Vol. 6 Pearson Prentice Hall
- Hair, J. F., Ringle, C. M., & Sarstedt, M. (2013). Partial least squares structural equation modeling: Rigorous applications, better results and higher acceptance. Long Range Planning, 46(1–2), 1–12. https://doi.org/10.1016/j.lrp.2013.01.001
- Hair, J. F., Risher, J. J., Sarstedt, M., & Ringle, C. M. (2019). When to use and how to report the results of PLS-SEM. European Business Review, 31(1), 2–24. https://doi.org/10.1108/ebr-11-2018-0203
- Hao, S., Hong, W., Xu, H., Zhou, L., & Xie, Z. (2015). Relationship between resilience, stress and burnout among civil servants in Beijing, China: Mediating and moderating effect analysis. Personality and Individual Differences, 83, 65–71. https://doi.org/10.1016/j.paid.2015.03.048
- Hawthorne, G. (2006). Measuring social isolation in older adults: Development and initial validation of the friendship scale. Social Indicators Research, 77(3), 521–548. https://doi.org/10.1007/s11205-005-7746-y
- Hellewell, J., Abbott, S., Gimma, A., Bosse, N. I., Jarvis, C. I., Russell, T. W., Munday, J. D., Kucharski, A. J., Edmunds, W. J., Funk, S., Eggo, R. M., Sun, F., Flasche, S., Quilty, B. J., Davies, N., Liu, Y., Clifford, S., Klepac, P., Jit, M., Diamond, C., & van Zandvoort, K. (2020). Feasibility of controlling COVID-19 outbreaks by isolation of cases and contacts. The Lancet Global Health, 8(4), e488–e496. https://doi.org/10.1016/S2214-109X(20)30074-7
- Henseler, J., Ringle, C. M., & Sarstedt, M. (2015). A new criterion for assessing discriminant validity in variance-based structural equation modeling. Journal of the Academy of Marketing Science, 43(1), 115–135. https://doi.org/10.1007/s11747-014-0403-8
- Henseler, J., Ringle, C. M., & Sinkovics, R. R. (2009). The use of partial least squares path modeling in international marketing. In New challenges to international marketing: Emerald Group Publishing Limited.
- Ho, C. S., Chee, C. Y., & Ho, R. C. (2020). Mental health strategies to combat the psychological impact of COVID-19 beyond paranoia and panic. Ann Acad Med Singapore, 49(1), 1–3.
- Holmes, E. A., O’Connor, R. C., Perry, V. H., Tracey, I., Wessely, S., Arseneault, L., & Ford, T. (2020). Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. The Lancet Psychiatry, 7(6), 547–560. https://doi.org/10.1016/S2215-0366(20)30168-1
- Jeong, H., Yim, H. W., Song, Y.-J., Ki, M., Min, J.-A., Cho, J., & Chae, J.-H. (2016). Mental health status of people isolated due to Middle East Respiratory Syndrome. Epidemiology and Health, 38. https://doi.org/10.4178/epih.e2016048
- Kercher, K., Kosloski, K. D., & Normoyle, J. B. (1988). Reconsideration of fear of personal aging and subjective well-being in later life. Journal of Gerontology, 43(6), 6. https://doi.org/10.1093/geronj/43.6.P170
- Lau, A. L., Chi, I., Cummins, R. A., Lee, T. M., Chou, K.-L., & Chung, L. W. (2008). The SARS (Severe Acute Respiratory Syndrome) pandemic in Hong Kong: Effects on the subjective wellbeing of elderly and younger people. Aging and Mental Health, 12(6), 746–760. https://doi.org/10.1080/13607860802380607
- Lazarus, R. S., & Folkman, S. (1984). Stress, Appraisal, and Coping. Springer Publishing Company.
- Lee, H. H., & Cranford, J. A. (2008). Does resilience moderate the associations between parental problem drinking and adolescents’ internalizing and externalizing behaviours?A study of Korean Adolescents. Drug and Alcohol Dependence, 96, 213–221. https://doi.org/10.1016/j.drugalcdep.2008.03.007
- Lee, S., Chowell, G., & Castillo-Chávez, C. (2010). Optimal control for pandemic influenza: The role of limited antiviral treatment and isolation. Journal of Theoretical Biology, 265(2), 136–150. https://doi.org/10.1016/j.jtbi.2010.04.003
- Leigh-Hunt, N., Bagguley, D., Bash, K., Turner, V., Turnbull, S., Valtorta, N., & Caan, W. (2017). An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health, 152, 157–171. https://doi.org/10.1016/j.puhe.2017.07.035
- Liew, M. F., Siow, W. T., MacLaren, G., & See, K. C. (2020). Preparing for COVID-19: Early experience from an intensive care unit in Singapore. Critical Care, 24(1), 1–3. https://doi.org/10.1186/s13054-020-2814-x
- Lin, C.-Y. (2020). Social reaction toward the 2019 novel coronavirus (COVID-19). Social Health and Behavior, 3(1), 1–2. https://doi.org/10.4103/SHB.SHB_11_20
- Mamun, M. A., & Griffiths, M. D. (2020). First COVID-19 suicide case in Bangladesh due to fear of COVID-19 and xenophobia: Possible suicide prevention strategies. Asian Journal of Psychiatry, 51, 102073. https://doi.org/10.1016/j.ajp.2020.102073
- Marais, L., Sharp, C., Pappin, M., Rani, K., Skinner, D., Lenka, M., Cloete, J., & Serekoane, J. (2014). Community-based mental health support for orphans and vulnerable children in South Africa: A triangulation study. Vulnerable Children and Youth Studies, 9(2), 151–158. https://doi.org/10.1080/17450128.2013.855345
- Masten, A. S. (2001). Ordinary magic: Resilience processes in development. American Psychologist, 56(3), 227. https://doi.org/10.1037/0003-066X.56.3.227
- Matthews, T., Danese, A., Wertz, J., Ambler, A., Kelly, M., Diver, A., & Arseneault, L. (2015). Social isolation and mental health at primary and secondary school entry: A longitudinal cohort study. Journal of the American Academy of Child & Adolescent Psychiatry, 54(3), 225–232. https://doi.org/10.1016/j.jaac.2014.12.008
- Osimo, S. A., Aiello, M., Gentili, C., Ionta, S., & Cecchetto, C. (2021). The influence of personality, resilience, and alexithymia on mental health during COVID-19 pandemic. Frontiers in Psychology, 12, 341. https://doi.org/10.3389/fpsyg.2021.630751
- Pearson, A. L., & Breetzke, G. D. (2014). The association between the fear of crime, and mental and physical wellbeing in New Zealand. Social Indicators Research, 119(1), 281–294. https://doi.org/10.1007/s11205-013-0489-2
- Pinedo, R., Vicario-Molina, I., González Ortega, E., & Palacios Picos, A. (2021). Factors related to mental health during the COVID-19 lockdown in Spain. Frontiers in Psychology, 3576. https://doi.org/10.3389/fpsyg.2021.715792
- Polizzi, C., Lynn, S. J., & Perry, A. (2020). Stress and coping in the time of COVID-19: Pathways to resilience and recovery. Clinical Neuropsychiatry, 17(2), 59–62.
- Preacher, K. J., & Hayes, A. F. (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40(3), 879–891. https://doi.org/10.3758/brm.40.3.879
- Qiu, Y., Zhou, D., Liu, J., & Yuan, T. (2020). Mental wellness system for COVID-19. Brain, Behavior, and Immunity, 87, 51–52. https://doi.org/10.1016/j.bbi.2020.04.032
- Rajkumar, R. P. (2020). COVID-19 and mental health: A review of the existing literature. Asian Journal of Psychiatry, 52, 102066. https://doi.org/10.1016/j.ajp.2020.102066
- Ravi, R. C. (2020). Lockdown of colleges and universities due to COVID-19: Any impact on the educational system in India? Journal of Education and Health Promotion, 9(1), 209. https://doi.org/10.4103/jehp.jehp_327_20
- Ringle, C. M., Wende, S., & Becker, J. M. (2015). SmartPLS 3. SmartPLS GmbH.
- Roy, D., Tripathy, S., Kar, S. K., Sharma, N., Verma, S. K., & Kaushal, V. (2020). Study of knowledge, attitude, anxiety & perceived mental healthcare need in Indian population during COVID-19 pandemic. Asian Journal of Psychiatry, 51. https://doi.org/10.1016/j.ajp.2020.102083
- Ryan, R. M., & Deci, E. L. (2001). On happiness and human potentials: A review of research on hedonic and eudaimonic well-being. Annual Review of Psychology, 52(1), 141–166. https://doi.org/10.1146/annurev.psych.52.1.141
- Saltzman, L. Y., Hansel, T. C., & Bordnick, P. S. (2020). Loneliness, isolation, and social support factors in Post-COVID-19 mental health. Psychol Trauma, 12(S1), S55–S57. https://doi.org/10.1037/tra0000703
- Sarstedt, M., Ringle, C. M., & Hair, J. F. (2017). Treating unobserved heterogeneity in PLS-SEM: A multi-method approach. In R. Noonan & H. Latan (Eds.), Partial Least Squares Structural Equation Modeling: Basic Concepts, Methodological Issues and Applications (pp. 197–217). Springer International Publishing.
- Sen-Crowe, B., McKenney, M., & Elkbuli, A. (2020). Social distancing during the COVID-19 pandemic: Staying home save lives. The American Journal of Emergency Medicine, 38(7), 1519–1520. https://doi.org/10.1016/j.ajem.2020.03.063
- Shah, A., Yezhuang, T., Shah, A., Durrani, D., & Shah, S. (2018). Fear of terror and psychological well-being: The moderating role of emotional intelligence. International Journal of Environmental Research and Public Health, 15, 11. https://doi.org/10.3390/ijerph15112554
- Shah, K., Kamrai, D., Mekala, H., Mann, B., Desai, K., & Patel, R. S. (2020). Focus on mental health during the Coronavirus (COVID-19) Pandemic: Applying learnings from the past outbreaks. Cureus, 12, 3. https://doi.org/10.7759/cureus.7405
- Shah, S. S., Shah, A. A., Memon, F., Kemal, A. A., & Soomro, A. (2021). Online learning during the COVID-19 pandemic: Applying the self-determination theory in the ‘new normal’. Revista de Psicodidáctica, 26(2), 168–177. https://doi.org/10.1016/j.psicoe.2020.12.003
- Shaw, S. C. (2020). Hopelessness, helplessness and resilience: The importance of safeguarding our trainees‘ mental wellbeing during the COVID-19 pandemic. Nurse Education in Practice, 44. https://doi.org/10.1016/j.nepr.2020.102780
- Shmueli, G., Ray, S., Estrada, J. M. V., & Chatla, S. B. (2016). The elephant in the room: Predictive performance of PLS models. Journal of Business Research, 69(10), 4552–4564. https://doi.org/10.1016/j.jbusres.2016.03.049
- Shmueli, G., Sarstedt, M., Hair, J. F., Cheah, J.-H., Ting, H., Vaithilingam, S., & Ringle, C. M. (2019). Predictive model assessment in PLS-SEM: Guidelines for using PLSpredict. European Journal of Marketing, 53(11), 2322–2347. https://doi.org/10.1108/ejm-02-2019-0189
- Singh, J., & Singh, J. (2020). COVID-19 and its impact on society. Electronic Research Journal of Social Sciences and Humanities, (2).
- Sohrabi, C., Alsafi, Z., O’Neill, N., Khan, M., Kerwan, A., Al-Jabir, A., Iosifidis, C., & Agha, R. (2020). World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19). International Journal of Surgery, 76, 71–76. https://doi.org/10.1016/j.ijsu.2020.02.034
- Stone, M. (1974). Cross‐validatory choice and assessment of statistical predictions. Journal of the Royal Statistical Society: Series B (Methodological), 36(2), 111–133. https://doi.org/10.1111/j.2517-6161.1974.tb00994.x
- Tennant, R., Hiller, L., Fishwick, R., Platt, S., Joseph, S., Weich, S., Parkinson, J., Secker, J., & Stewart-Brown, S. (2007). The Warwick-Edinburgh mental well-being scale (WEMWBS): Development and Uk validation. Health and Quality of Life Outcomes, 5(1), 1. https://doi.org/10.1186/1477-7525-5-63
- Thangaraj, J. W. V., Yadav, P., Kumar, C. G., Shete, A., Nyayanit, D. A., Rani, D. S., Kumar, A., Kumar, M. S., Sabarinathan, R., Saravana Kumar, V., Jagadeesan, M., & Murhekar, M. (2021). Predominance of delta variant among the COVID-19 vaccinated and unvaccinated individuals, India, May 2021. Journal of Infection. https://doi.org/10.1016/j.jinf.2021.08.006
- Tugade, M. M., & Fredrickson, B. L. (2004). Resilient Individuals Use Positive Emotions to Bounce Back From Negative Emotional Experiences. Journal of Personality and Social Psychology, 86(2), 320–333. https://doi.org/10.1037/0022-3514.86.2.320
- Turan, B., Smith, W., Cohen, M. H., Wilson, T. E., & Adimora, A. A. (2016). Depression and Social Isolation Mediate Effect of HIV Stigma on Women’s ART Adherence. Age (Years), 49(8), 59.
- Tzeng, H.-M., & Yin, C.-Y. (2008). A crisis: Fear toward a possible H5N1 pandemic. Journal of Nursing Care Quality, 23(2), 177–183. https://doi.org/10.1097/01.NCQ.0000313768.17514.a3
- Van, D., McLaws, M.-L., Crimmins, J., MacIntyre, C. R., & Seale, H. (2010). University life and pandemic influenza: Attitudes and intended behaviour of staff and students towards pandemic (H1N1) 2009. BMC Public Health, 10(1), 130. https://doi.org/10.1186/1471-2458-10-130
- Vance, M. A. (2011). Disease mongering and the fear of pandemic influenza. International Journal of Health Services, 41(1), 95–115. https://doi.org/10.2190/HS.41.1.g
- Vassallo, M., Manni, S., Klotz, C., Fabre, R., Pini, P., Blanchouin, E., Sindt, A., Lotte, L., Dubertrand, J. M., Liguori, S., Berkane, N., Duval, Y., Rolland, F., & Pradier, C. (2021). Patients Admitted for Variant Alpha COVID-19 Have Poorer Outcomes than Those Infected with the Old Strain. Journal of Clinical Medicine, 10(16), 16. https://doi.org/10.3390/jcm10163550
- Wang, C., Pan, R., Wan, X., Tan, Y., Xu, L., Ho, C. S., & Ho, R. C. (2020). Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. International Journal of Environmental Research and Public Health, 17, 5. https://doi.org/10.3390/ijerph17051729
- Wang, L., Zhang, Y., Huang, T., & Li, X. (2012). Estimating the value of containment strategies in delaying the arrival time of an influenza pandemic: A case study of travel restriction and patient isolation. Physical Review E, 86(3). https://doi.org/10.1103/PhysRevE.86.032901
- WHO- COVID-2019 Situation Reports, (2021) https://www.who.int/publications/m/item/weekly-operational-update-on-covid-19—28-september–2021
- Wickramage, K., Gostin, L. O., Friedman, E., Prakongsai, P., Suphanchaimat, R., Hui, C., Duigan, P., Barragan, E., & Harper, D. R. (2018). Missing: Where are the migrants in pandemic influenza preparedness plans? Health and Human Rights, 20(1), 251–258.
- Wilder-Smith, A., & Freedman, D. O. (2020). Isolation, quarantine, social distancing and community containment: Pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. Journal of Travel Medicine, 27(2), 1–4. https://doi.org/10.1016/j.enfcli.2014.12.009
- Wilson, M. E., & Chen, L. H. (2020). Travelers give wings to novel coronavirus (2019-nCoV). Journal of Travel Medicine, 27, 2. https://doi.org/10.1093/jtm/taaa015
- Wingo, A. P., Fani, N., Bradley, B., & Ressler, K. J. (2010). Psychological resilience and neurocognitive performance in a traumatized community sample. Depression and Anxiety, 27(8), 768–774. https://doi.org/10.1002/da.20675
- Witte, K. (1992). Putting the fear back into fear appeals: The extended parallel process model. Communications Monographs, 59(4), 329–349. https://doi.org/10.1080/03637759209376276
- Wong, K. K. K. (2013). Partial least squares structural equation modeling (PLS-SEM) techniques using Smart PLS. Marketing Bulletin, 24(1), 1–32.
- World Health Organization. (2021). Coronavirus disease (COVID-19) advice for the public.
- Wu, Z., & McGoogan, J. M. (2020). Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. Jama, 323(13), 1239–1242. https://doi.org/10.1001/jama.2020.2648
- Yao, H., Chen, J.-H., & Xu, Y.-F. (2020). Rethinking online mental health services in China during the COVID-19 epidemic. Asian Journal of Psychiatry, 50, 102015. https://doi.org/10.1016/j.ajp.2020.102015
- Zandifar, A., & Badrfam, R. (2020). Iranian mental health during the COVID-19 epidemic. Asian Journal of Psychiatry, 51(51), 101990. https://doi.org/10.1016/j.ajp.2020.101990
- Zheng, Y., Goh, E., & Wen, J. (2020). The effects of misleading media reports about COVID-19 on Chinese tourists’ mental health: A perspective article. Anatolia, 1–4. https://doi.org/10.1080/13032917.2020.1747208