?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Objective: This study evaluated interfacial gap formation in bulk-fill composite restorations using cross-polarization optical coherence tomography (CP-OCT). Materials and methods: Two bulk-fill resin composite materials each with its specific adhesive were used; light-cured Filtek Bulk Fill Posterior Restorative with Scotchbond Universal (3M ESPE) “group A” and dual-cure bulk-fill composite BulkEZ with Prelude One (Danville Materials) “group B.” Proximal cavities (2 × 2 × 4.5 mm; width × length × depth) prepared on extracted human molars (n = 5) were restored with adhesives applied in self-etch mode and the composite placed in bulk. After 24 h storage, the specimens were immersed in ammoniacal silver nitrate solution for 24 h followed by a photo-developing solution for 8 h. Later, CP-OCT (Santec, Japan) at 1310 nm center wavelength was used to scan each specimen. Interfacial gap at the gingival floor was analyzed on cross-sectional OCT images obtained from each specimen at 0.5 mm interval using ImageJ analysis software. Result: Mann–Whitney test showed a significant difference (p < 0.05) between the groups with group A showing higher percentage of gap formation at the gingival floor. Conclusion: Within the limitation of the study, a better sealing of gingival margin was achieved with the dual-cure bulk-fill dental composite compared to the light-cured composite.
PUBLIC INTEREST STATEMENT
Bulk-fill resin composite restorative material has been recently introduced with a claim to have the capacity to be inserted in one increment up to 4 mm. However, the potential for development of discrepancy may exist. Failure of adhesive interface of composite restoration may lead to secondary caries and restoration failure. Optical coherence tomography is an emerging imaging tool that allows objective assessment of biomedical structures and materials without X-ray radiation or magnetic field. This paper evaluated the adaptation of bulk-fill resin composite restorations using optical coherence tomography.
Competing interests
The authors declare no competing interests.
1. Introduction
Direct restoration with resin composite has become the most frequently employed restorative treatment in the daily dental practice (Demarco, Correa, Cenci, Moraes, & Opdam, Citation2012). In addition to the conservative design of the prepared cavities, improved mechanical properties and cost-effective esthetic outcomes have promoted its widespread use. However, gap formation under composite resin is still a clinical problem, as marginal gaps are usually associated with deterioration especially in proximal restorations with a gingival/cervical margin in dentin (Asmussen & Peutzfeldt, Citation2008; Nedeljkovic, Teughels, De Munck, Van Meerbeek, & Van Landuyt, Citation2015).
Interfacial gaps may form due to polymerization shrinkage and weak bonding (Nedeljkovic et al., Citation2015). The shrinkage inherent to the polymeric resin generates internal stresses within the restoration leading to marginal discrepancies, cuspal deflection and interfacial debonding (Ferracane & Hilton, Citation2016; Souza-Junior et al., Citation2011). In an attempt to reduce the polymerization stresses and considering the depth of cure in conventional resin-based composites (RBCs), the incremental placement technique with increments of 2 mm or less has been widely adopted. This technique has shown to reduce the volume and bonded surface area of each increment material and improve light-beam penetration throughout the entire increment, and is thus believed to lower the shrinkage stress and cuspal deflection (Park, Chang, Ferracane, & Lee, Citation2008; Soares, Bicalho, Tantbirojn, & Versluis, Citation2013; Souza-Junior et al., Citation2011). Nevertheless, the inclusion of air bubbles or voids and debonding between successive increments have been associated with this technique. In addition, applying the composite in increments can be a clinically challenging and time-consuming procedure, especially in deep posterior cavities and less cooperative patients.
In an attempt to satisfy dentists demand for composite resin material with a simple and efficient placement technique, bulk-fill composites that can be used to fill more than 4 mm deep-cavities in a single increment have been introduced. Manufacturers state that inclusion of reactive photoinitiator and improvement in translucency by increasing filler size and/or decreasing filler load has increased the light transmission and allowed deeper cure of these materials (Bucuta & Ilie, Citation2014; Li, Pongprueksa, Van Meerbeek, & De Munck, Citation2015). However, in spite of the lower shrinkage stress measured for these composites, data from marginal adaptation studies are not conclusive. Some studies indicated that sealing performance of bulk-fill materials is comparable to that of conventional RBCs (Campos et al., Citation2014; Rengo et al., Citation2015). Meanwhile, others suggested improvement in the marginal seal with bulk-fill RBCs (Al-Harbi et al., Citation2015). Another study showed that some of the bulk-fill RBCs resulted in significantly larger gap formation than that observed with conventional RBCs (Benetti, Havndrup-Pedersen, Honore, Pedersen, & Pallesen, Citation2015). Previous studies have suggested that a slower rate of polymerization, such as in chemically cured composites, may have advantages in terms of stress development in composites, and dual-cured bulk-fill RBCs have been recently introduced (Bolhuis, de Gee, Kleverlaan, El Zohairy, & Feilzer, Citation2006). However, there is very little information available whether these materials have any advantage over the light-cured bulk-fill composites.
Adhesion tests have been routinely used for laboratory evaluation of newly introduced materials. A variety of conventional methods have been utilized for assessing marginal integrity in vitro. This includes microscopic examination of bonded specimen or its replica and dye penetration test (Atoui, Chinelatti, Palma-Dibb, & Corona, Citation2010; Benetti et al., Citation2015; Campos et al., Citation2014). However, such methods are considered semi-quantitative, time-consuming and may be subjective. Nevertheless, sensitivity and specificity of visual and tactile criteria for clinical detection are usually low (Moncada et al., Citation2014). Optical coherence tomography (OCT) has been introduced and employed for two-dimensional and three-dimensional evaluation of dental structures and biomaterials (Bakhsh et al., Citation2018; Bakhsh, Bakry, Mandurah, & Abbassy, Citation2017; Chan et al., Citation2016; Dao Luong et al., Citation2016; Gentile, Maio, Romano, Laino, & Lucchese, Citation2017; Nazari, Sadr, Shimada, Tagami, & Sumi, Citation2013; Sadr et al., Citation2011; Shimada, Sadr, Sumi, & Tagami, Citation2015; Turkistani et al., Citation2018; Turkistani, Nakashima, Shimada, Tagami, & Sadr, Citation2015; Turkistani et al., Citation2014). This promising optical modality allows a high-resolution subsurface detection based on depth-resolved refractive properties of different structures. When the near-infrared laser source is projected over the specimen, backscattered light is collected and transformed into signal intensity from which cross-sectional tomogram is constructed in almost real-time. One of the recent variations of OCT is cross-polarized OCT. Previous reports demonstrated the utility of CP-OCT to assess enamel demineralization and dental biofilms (Bakhsh et al., Citation2017; Chan et al., Citation2016). However, there are few reports on the evaluation of the bulk-fill composite restorations using CP-OCT.
This study aimed to evaluate marginal gap formation in the gingival floor of class-II cavities restored with a light-cured or a dual-cured bulk-fill resin composite using cross-polarization OCT (CP-OCT). The tested null hypothesis of the study was that there was no difference in gingival marginal adaptation between the tested groups.
2. Methods
2.1. Specimens preparation
A schematic drawing of the experiment is shown in Figure . For this in vitro study, human molar teeth with no caries, cracks or previous restorations were collected and stored in normal saline. The use of human teeth in this study was according to the ethical guidelines set by the King Abdulaziz University’s research ethics committee and the Declaration of Helsinki. Standard proximal box cavities were prepared on the proximal surfaces of each tooth using coarse diamond burs in a high-speed hand-piece under air and water spray and finished with fine-grained burs. The cavity measures 4.5 mm in occluso-cervical height (with gingival floor placed 0.5 mm below CEJ), and 2 mm in mesio-distal depth and bucco-lingual width. All measurements were confirmed using 15 UNC periodontal probe. Then, each tooth was secured with a matrix band and tofflemire retainer, and two experimental groups, groups A and B, were randomly assigned according to restorative composite used (n = 5); in group A, Scotchbond Universal (3M ESPE, St. Paul, MN, USA) was applied to cavity surface in self-etch mode and polymerized using an LED light unit with 650–1,200 mW/cm2 output power intensity (Bluephase N, Ivoclar vivadent, Schaan, Liechtenstein). The cavities were then filled with one increment of the light-cured Filtek Bulk Fill Posterior Restorative resin composite (3M ESPE). In group B, cavities were bonded with the single-component Prelude One bonding agent (Danville Materials, Zest Dental, CA, USA) and filled in bulk using dual-cure Bulk EZ resin composite (Danville Materials). All materials were applied according to the manufacturer’s instructions, as described in Table .
Figure 1. Schematic view of used methodology. Class-II cavities were prepared on proximal surfaces of extracted molar teeth. After restoration, the specimens were stored in 100% humidity for 24 h, immersed in ammoniacal silver nitrate followed by developing solution under a fluorescent light for 8 h. Specimens were reduced occlusally to be examined under CP-OCT, and obtained cross-sectional images were analyzed to quantify interfacial gaps
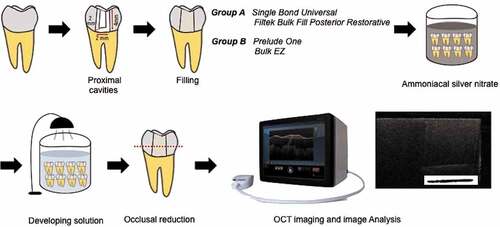
Table 1. Adhesive systems and bulk-fill resin composites used in this study
After restoration, specimens were stored in 100% humidity for 24 h. Later, nail polish (Revlon, New York City, NY, USA) was used to coat specimen surface, excluding 0.5 mm of peripheral area around the restoration margins. Specimens were then stored in dark environment in ammonical silver nitrate solution prepared by dissolving 25 mg of silver nitrate (Sigma Chemical, St. Louis, MO, USA) in distilled water with subsequent ammonium hydroxide titration. After 24 h, specimens were removed from solution, rinsed by distilled water and immersed in a photo-developing solution under fluorescent light for 8 h.
2.2. OCT imaging
To evaluate interfacial debonding, silver nitrate penetration depth along gingival margins of proximal cavity was measured using CP-OCT (CP-OCT; IVS-300, Santec, Komaki, Japan). This system relies on diode laser optical source of 1310 nm center spectral bandwidth and 30 kHz sweep rate. The axial resolution and lateral resolution are ∼12 and 30 μm, respectively. The probe power is within safe ranges defined by the American National Standard Institute.
Given the limitation in depth of OCT light penetration, each specimen was subjected to occlusal reduction by 3 mm leaving 1.5 mm for OCT imaging (Nazari et al., Citation2013). During OCT imaging, each specimen was positioned on micrometer stage and focused light beam was projected at 90◦ onto the cut surface of the specimens. Then, 5 serial 2D cross-sectional images were acquired at 0.5 mm interval. The raw OCT data were then imported to ImageJ software for image analysis. A noise-reducing median filter (2 px radius) was applied and image was rotated to adjust tooth-restoration interface at gingival floor to a zero-degree tilt. Then, cropped images of gingival floor were obtained and subjected to binarization process to measure the interfacial gap (Shimada et al., Citation2015), which was identified by increase in the signal intensity appearing as bright clusters at gingival floor. The extension of bright clusters in a single cross-section was summed up and divided by floor width, resulting in total gap percentage according to the following formula (Sadr et al., Citation2011):
2.3. Statistical analysis
Mann–Whitney and post hoc tests were used to compare gap percentage in experimental groups. The statistical procedure was performed at significance level of α = 0.05 using statistics package (ver. 23 for windows; SPSS, Chicago, IL, USA).
3. Result
Representative OCT images from groups A and B with binary images of gingival floor are shown in Figures and . Some tomographic images in both groups revealed bright reflection of the diffused silver nitrate contrast agent at the gingival floor indicating loss of interfacial seal (Figures ,) and ), while other cross-sections showed the bright area extending throughout the gingival floor (Figure ). Areas with intimate optical sealing with no detectable reflection at the cavity floor were indicated by no bright cluster formation in binary image (Figure )). In addition, voids in the bulk-filled restorations were observed in some cross-sectional images (Figures ) and 3()), which appeared as a slight increase in the brightness within the structure of composite with low signal intensity underneath the defect (Nazari et al., Citation2013).
Figure 2. Representative cross-sectional CP-OCT images of group A after immersion in silver nitrate and developing solution
Figure 3. B-scans of selected specimens from group B
The statistical analysis showed that group B had superior marginal sealing and less gap formation at the gingival floor in comparison to group A. The mean gap percentages (±SD) of groups A and B were 15.95 (±14.06) and 10.06 (±16.99), respectively. The difference was statistically significant (p < 0.05).
4. Discussion
In this study, gap formation along the gingival floor in class-II restorations was investigated. Interfacial sealing of this floor is particularly challenging. Concerns about stress distribution, light cure penetration and adhesion to dentinal margin question the longevity of these restorations (Asmussen & Peutzfeldt, Citation2008). To restore the cavities, a combination of bulk-fill composite and one-step self-etching adhesive was adopted. One-step adhesive systems require less time for the bonding procedure and are less technique-sensitive compared to etch and rinse systems, therefore appear to be a good match for the time-saving bulk-fill technique (Van Meerbeek et al., Citation2011). Each bulk-fill material was used with its specific bonding agent from the same manufacturer to minimize the chance of gap formation at adhesive-composite interface arising from poor copolymerization.
Marginal sealing was evaluated using CP-OCT. OCT is a non-invasive, real-time functional tool that provides images of structures with micron-scale resolution. In dentistry, OCT imaging of hard and soft tissues and dental materials was reported in previous studies (Bakhsh et al., Citation2018, Citation2017; Chan et al., Citation2016; Dao Luong et al., Citation2016; Gentile et al., Citation2017; Nazari et al., Citation2013; Sadr et al., Citation2011; Shimada et al., Citation2015; Turkistani et al., Citation2018, Citation2015, Citation2014). Low-coherence infrared light is utilized to perform in depth imaging for clinical diagnosis of oral diseases and for research studies (Gentile et al., Citation2017; Shimada et al., Citation2015). This modality has been employed in adhesive studies to detect and quantify interfacial gap formation (Bakhsh et al., Citation2018; Turkistani et al., Citation2018, Citation2015, Citation2014). The utilized CP-OCT system has imaging depth limited to less than 3 mm of tissues, while the depth of the prepared cavities was 4.5 mm to provide adequate thickness for assessment of the tested bulk-fill composites. Therefore, occlusal reduction to approximate the gingival floor of restoration to OCT probe was necessary for accurate gap detection.
The concept of gap detection under OCT is based on that media with different compositions and light scattering properties have different refractive indices. When the light travels through different media, a portion of the light is reflected and refracted (Turkistani et al., Citation2014). Loss of seal at the tooth-restorative material interface causes a peak in the signal intensity profile of the backscatter signal due to light refraction at the border of the gap, which appears as a bright cluster in the gray-scale 2D image (Turkistani et al., Citation2015, Citation2014). Additionally, specimens in this study were immersed in silver nitrate to obtain a better contrast from the interfacial gap in the CP-OCT 2D cross-sectional images. Ammoniacal silver nitrate staining is a well-established method in microscopic adhesion studies (Rengo et al., Citation2015). The presence of interfacial gap allows infiltration of silver ions along the debonded interface. Under the effect of fluorescent light, silver ions are reduced into metallic silver grains, which will highly reflect the OCT light.
During OCT image analysis, different bright clusters were visualized at gingival floor-restoration interface. However, group A showed significant increase in microgaps compared to group B. The inclusion of AUDMA, UDMA, and DDMA monomers in Filtek Bulk Fill Posterior Restorative was reported to enable rearrangement of polymerization mixture to accommodate polymerization shrinkage, decreasing generated stresses (Mandava et al., Citation2017). Nevertheless, microgaps detected in certain cross-sections of this group might be attributed to polyalkenoic acid component of Scotchbond Universal, known as Vitrebond copolymer. The competition of this high-molecular weight copolymer with MDP for Ca-binding site in HAp might lead to the prevention of monomer approximation during polymerization (Mitra, Lee, Bui, Tantbirojn, & Rusin, Citation2009; Munoz et al., Citation2013). In addition, light curing at the deepest portion of the 4.5 mm increment of bulk-fill composite might not be adequate (Alrahlah, Silikas, & Watts, Citation2014). In a previous study, Filtek Bulk Fill resin composites have demonstrated significantly higher volumetric shrinkage than the conventional resin composites (Shibasaki et al., Citation2017). This polymerization shrinkage can produce high stresses at the tooth-restoration interface, which could not be compensated by relaxation due to high filler load, resulting in gap formation.
In group B, the low-viscosity bulk-fill composite Bulk EZ could be responsible for the better adaptation. Enhanced flowability and low modulus of elasticity may have counteracted the effect of generated stresses. Recent studies showed that flowable bulk-fill composite restorations had better marginal sealing in comparison with high-viscosity bulk-fill composites (Orłowski, Tarczydło, & Chałas, Citation2015), and lower contraction stresses (Kim, Kim, Choi, & Lee, Citation2015). In addition, patent-pending initiator system designed to control shrinkage is incorporated in dual-cure Bulk EZ composite. The slow chemical curing during the recommended 90 s wait before light-curing of the composite may allow for viscous flow and relaxation of the polymerization stress developed throughout the resin, minimizing contraction stresses at tooth-restoration interface. Also, chemical curing could ensure full depth of polymerization in deep areas, improving interfacial bonding (Bolhuis et al., Citation2006). Further research should focus on the degree of conversion and polymerization kinetics of Bulk EZ composites.
Based on the results of this study, the null hypothesis was rejected. However, it should be emphasized that different outcomes may have been arisen from other adhesive systems. In addition, evaluation of long-term marginal sealing of these bulk-fill type resin composites and their mechanical properties is indispensable.
5. Conclusion
In addition to sealing performance of the bonding system, the attribute of chemical cure in bulk-fill resin composite may ensure optimal marginal adaptation in deep cavities.
Additional information
Funding
Notes on contributors
Alaa Turkistani
Alaa Turkistani received her B.D.S from King Abdulaziz University in 2008. She completed her Ph.D. degree in Cariology and Operative Dentistry at Tokyo Medical and Dental University in 2016. She is currently a faculty member of Operative Dentistry at King Abdulaziz University. Her group’s main research activities involve characterization of dental hard tissues and biomaterials, adhesion of restorative materials, enamel and dentin remineralization, advanced biomedical imaging systems and image analysis.
References
- Al-Harbi, F., Kaisarly, D., Michna, A., ArRejaie, A., Bader, D., & El Gezawi, M. (2015). Cervical interfacial bonding effectiveness of class II bulk versus incremental fill resin composite restorations. Operative Dentistry, 40(6), 622–10. doi:10.2341/14-152-L
- Alrahlah, A., Silikas, N., & Watts, D. C. (2014). Post-cure depth of cure of bulk fill dental resin-composites. Dental Materials, 30(2), 149–154. doi:10.1016/j.dental.2013.10.011
- Asmussen, E., & Peutzfeldt, A. (2008). Class I and Class II restorations of resin composite: An FE analysis of the influence of modulus of elasticity on stresses generated by occlusal loading. Dental Materials, 24(5), 600–605. doi:10.1016/j.dental.2007.06.019
- Atoui, J. A., Chinelatti, M. A., Palma-Dibb, R. G., & Corona, S. A. (2010). Microleakage in conservative cavities varying the preparation method and surface treatment. Journal of Applied Oral Science: Revista FOB, 18(4), 421–425. doi:10.1590/s1678-77572010000400017
- Bakhsh, T. A., Altouki, N. H., Baeesa, L. S., Baamer, R. A., Alshebany, R. M., Natto, Z., … Naguib, G. H. (2018). Effect of self-etch adhesives on the internal adaptation of composite restoration: A CP-OCT Study. Odontology. doi:10.1007/s10266-018-0381-2
- Bakhsh, T. A., Bakry, A. S., Mandurah, M. M., & Abbassy, M. A. (2017). Novel evaluation and treatment techniques for white spot lesions. An in Vitro study. Orthodontics & Craniofacial Research, 20(3), 170–176. doi:10.1111/ocr.12193
- Benetti, A. R., Havndrup-Pedersen, C., Honore, D., Pedersen, M. K., & Pallesen, U. (2015). Bulk-fill resin composites: Polymerization contraction, depth of cure, and gap formation. Operative Dentistry, 40(2), 190–200. doi:10.2341/13-324-L
- Bolhuis, P. B., de Gee, A. J., Kleverlaan, C. J., El Zohairy, A. A., & Feilzer, A. J. (2006). Contraction stress and bond strength to dentinfor compatible and incompatible combinations of bonding systems and chemical and light-cured core build-up resin composites. Dental Materials, 22(3), 223–233. doi:10.1016/j.dental.2005.03.016
- Bucuta, S., & Ilie, N. (2014). Light transmittance and micro-mechanical properties of bulk fill vs conventional resin based composites. Clinical Oral Investigations, 18(8), 1991–2000. doi:10.1007/s00784-013-1177-y
- Campos, E. A., Ardu, S., Lefever, D., Jasse, F. F., Bortolotto, T., & Krejci, I. (2014). Marginal adaptation of class II cavities restored with bulk-fill composites. Journal of Dentistry, 42(5), 575–581. doi:10.1016/j.jdent.2014.02.007
- Chan, K. H., Tom, H., Lee, R. C., Kang, H., Simon, J. C., Staninec, M., … Fried, D. (2016). Clinical monitoring of smooth surface enamel lesions using CP-OCT during nonsurgical intervention. Lasers in Surgery and Medicine, 48(10), 915–923. doi:10.1002/lsm.22500
- Dao Luong, M. N., Shimada, Y., Turkistani, A., Tagami, J., Sumi, Y., & Sadr, A. (2016). Fractography of interface after microtensile bond strength test using swept-source optical coherence tomography. Dental Materials, 32(7), 862–869. doi:10.1016/j.dental.2016.03.019
- Demarco, F. F., Correa, M. B., Cenci, M. S., Moraes, R. R., & Opdam, N. J. (2012). Longevity of posterior composite restorations: Not only a matter of materials. Dental Materials, 28(1), 87–101. doi:10.1016/j.dental.2011.09.003
- Ferracane, J. L., & Hilton, T. J. (2016). Polymerization stress–Is it clinically meaningful? Dental Materials, 32(1), 1–10. doi:10.1016/j.dental.2015.06.020
- Gentile, E., Maio, C., Romano, A., Laino, L., & Lucchese, A. (2017). The potential role of in vivo optical coherence tomography for evaluating oral soft tissue: A systematic review. Journal of Oral Pathology & Medicine, 46(10), 864–876. doi:10.1111/jop.12589
- Kim, R. J., Kim, Y. J., Choi, N. S., & Lee, I. B. (2015). Polymerization shrinkage, modulus, and shrinkage stress related to tooth-restoration interfacial debonding in bulk-fill composites. Journal of Dentistry, 43(4), 430–439. doi:10.1016/j.jdent.2015.02.002
- Li, X., Pongprueksa, P., Van Meerbeek, B., & De Munck, J. (2015). Curing profile of bulk-fill resin-based composites. Journal of Dentistry, 43(6), 664–672. doi:10.1016/j.jdent.2015.01.002
- Mandava, J., Vegesna, D.-P., Ravi, R., Boddeda, M.-R., Uppalapati, L.-V., & Ghazanfaruddin, M. D. (2017). Microtensile bond strength of bulk-fill restorative composites to dentin. Journal of Clinical and Experimental Dentistry, 9(8), e1023–e1028. doi:10.4317/jced.53965
- Mitra, S. B., Lee, C. Y., Bui, H. T., Tantbirojn, D., & Rusin, R. P. (2009). Long-term adhesion and mechanism of bonding of a paste-liquid resin-modified glass-ionomer. Dental Materials, 25(4), 459–466. doi:10.1016/j.dental.2008.09.008
- Moncada, G., Silva, F., Angel, P., Oliveira, O. B., Jr., Fresno, M. C., Cisternas, P., … Martin, J. (2014). Evaluation of dental restorations: A comparative study between clinical and digital photographic assessments. Operative Dentistry, 39(2), E45–56. doi:10.2341/12-339-C
- Munoz, M. A., Luque, I., Hass, V., Reis, A., Loguercio, A. D., & Bombarda, N. H. (2013). Immediate bonding properties of universal adhesives to dentine. Journal of Dentistry, 41(5), 404–411. doi:10.1016/j.jdent.2013.03.001
- Nazari, A., Sadr, A., Shimada, Y., Tagami, J., & Sumi, Y. (2013). 3D assessment of void and gap formation in flowable resin composites using optical coherence tomography. The Journal of Adhesive Dentistry, 15(3), 237–243. doi:10.3290/j.jad.a28623
- Nedeljkovic, I., Teughels, W., De Munck, J., Van Meerbeek, B., & Van Landuyt, K. L. (2015). Is secondary caries with composites a material-based problem? Dental Materials, 31, e247-e277. doi:10.1016/j.dental.2015.09.001
- Orłowski, M., Tarczydło, B., & Chałas, R. (2015). Evaluation of marginal integrity of four bulk-fill dental composite materials: In vitro study. The Scientific World Journal, 2015, 8.
- Park, J., Chang, J., Ferracane, J., & Lee, I. B. (2008). How should composite be layered to reduce shrinkage stress: Incremental or bulk filling? Dental Materials, 24(11), 1501–1505. doi:10.1016/j.dental.2008.03.013
- Rengo, C., Spagnuolo, G., Ametrano, G., Goracci, C., Nappo, A., Rengo, S., & Ferrari, M. (2015). Marginal leakage of bulk fill composites in Class II restorations: A microCT and digital microscope analysis. International Journal of Adhesion and Adhesives, 60, 123–129. doi:10.1016/j.ijadhadh.2015.04.007
- Sadr, A., Shimada, Y., Mayoral, J. R., Hariri, I., Bakhsh, T. A., Sumi, Y., & Tagami, J. (2011). Swept source optical coherence tomography for quantitative and qualitative assessment of dental composite restorations. Proc SPIE. 78840C–78840C.
- Shibasaki, S., Takamizawa, T., Nojiri, K., Imai, A., Tsujimoto, A., Endo, H., … Miyazaki, M. (2017). Polymerization behavior and mechanical properties of high-viscosity bulk fill and low shrinkage resin composites. Operative Dentistry, 42(6), E177–E187. doi:10.2341/16-385-L
- Shimada, Y., Sadr, A., Sumi, Y., & Tagami, J. (2015). Application of Optical Coherence Tomography (OCT) for diagnosis of caries, cracks, and defects of restorations. Current Oral Health Reports, 2(2), 73–80. doi:10.1007/s40496-015-0045-z
- Soares, C. J., Bicalho, A. A., Tantbirojn, D., & Versluis, A. (2013). Polymerization shrinkage stresses in a premolar restored with different composite resins and different incremental techniques. The Journal of Adhesive Dentistry, 15(4), 341–350. doi:10.3290/j.jad.a29012
- Souza-Junior, E. J., de Souza-Regis, M. R., Alonso, R. C., de Freitas, A. P., Sinhoreti, M. A., & Cunha, L. G. (2011). Effect of the curing method and composite volume on marginal and internal adaptation of composite restoratives. Operative Dentistry, 36(2), 231–238. doi:10.2341/10-107-L
- Turkistani, A., Almutairi, M., Banakhar, N., Rubehan, R., Mugharbil, S., Jamleh, A., … Bakhsh, T. (2018). Optical evaluation of enamel microleakage with one-step self-etch adhesives. Photomedicine and Laser Surgery. doi:10.1089/pho.2018.4441
- Turkistani, A., Nakashima, S., Shimada, Y., Tagami, J., & Sadr, A. (2015). Microgaps and demineralization progress around composite restorations. Journal of Dental Research, 94(8), 1070–1077. doi:10.1177/0022034515589713
- Turkistani, A., Sadr, A., Shimada, Y., Nikaido, T., Sumi, Y., & Tagami, J. (2014). Sealing performance of resin cements before and after thermal cycling: Evaluation by optical coherence tomography. Dental Materials, 30(9), 993–1004. doi:10.1016/j.dental.2014.05.010
- Van Meerbeek, B., Yoshihara, K., Yoshida, Y., Mine, A., De Munck, J., & Van Landuyt, K. L. (2011). State of the art of self-etch adhesives. Dental Materials, 27(1), 17–28. doi:10.1016/j.dental.2010.10.023