Abstract
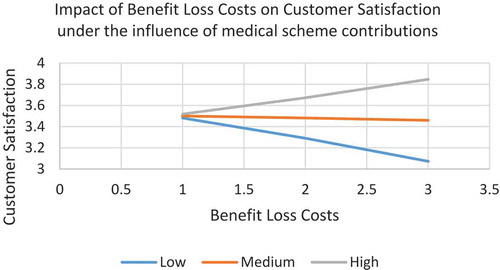
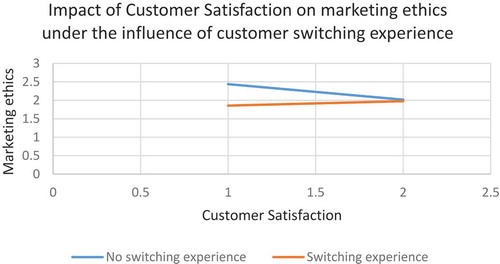
The issue regarding the transition of members from their current medical schemes to the National Health Insurance (NHI) in South Africa has erupted in much debate. This study, modelled on enlightened marketing philosophy concepts, measures the effects of the perceived costs classified by type (procedural, financial, and relational) and direction (positive and negative) of this switch in terms of Customer Satisfaction. It also measures the impact on the perceived marketing ethics of current medical schemes in South Africa. Data were collected using a face-to-face survey from 250 consumers of medical schemes in South Africa. An 83.2% response rate was entered into SPSS Version 26, and AMOS Version 26 to test a two-step modelling approach (SEM). The results reveal positive significant effects of personal relational loss costs and benefit loss costs on Customer Satisfaction, which in turn, negatively affects currently perceived marketing ethics of medical schemes. For customers paying high and medium medical scheme contributions, and those who have prior switching experience, the results show that the costs of increasing benefit loss enhance Customer Satisfaction. Increasing satisfaction then enhances perceptions of marketing ethics for customers who do not have switching experience. The practical implications and recommendations explain marketing strategies to medical scheme practitioners to enable the enhancement of personal relationships with customers and increase the service benefits, which in turn, removes the current negatively perceived marketing ethics. This paper, therefore, links articulation of the disconfirmation Expectation Theory and the General Theory of Marketing Ethics in the context of medical schemes in South Africa. Limitations and relevant future research avenues conclude the discussion of the research study.
PUBLIC INTEREST STATEMENT
The policy on National Health Insurance (NHI) promotes the principle of social solidarity. It will eradicate imbalances in South African healthcare by enabling private-public health sector interactions. Owing to high switching costs, both the satisfied consumers (who like to try new products) and dissatisfied customers often feel “locked-in”. Looking ahead, it seems the enlightened marketing philosophy needs to be embraced to enhance the long-term performance of the marketing system of the medical schemes. However, more knowledge is required on how switching costs will affect the continuously changing expectations of customers and the consequent outcome on the currently perceived marketing ethics of medical schemes. Results show significant positive effects of Personal Relational Loss costs and Benefit Loss Costs on Customer Satisfaction, which negatively affects their perceptions of marketing ethics. Increasing Benefit Loss Costs enhance the satisfaction of members contributing large and medium monthly fees, and those with switching experience. Satisfaction affects perceptions of marketing ethics for customers who do not have switching experience.
1. Introduction
The enlightened marketing philosophy involves using the five broader principles of ▪customer-value marketing; ▪ consumer-oriented marketing; ▪ innovative marketing; ▪ societal marketing; and ▪ sense-of-mission-marketing to support the long-term performance of the marketing system (Kotler & Armstrong, Citation2010). The relevant topic of societal issues was introduced by Kotler and Levy (Citation1971) based on social responsibility, ethics, marketing, ecology, consumerism, the desired political advertising appeal, and the growing demand for public goods with a focus on the marketing problems of non-profit entities (i.e. non-profit, micro, normative). The Normative Ethical Theory sets the guidelines for ethical behaviour and integrates Positive Ethical Theory and outcomes, while Distributive Justice is an ethics precept embracing enlightened marketing ethics (Ferrell & Ferrell, Citation2008). Distributive Justice, a central concept in the Catholic social tradition introduced by Laczniak (Citation1999), is another foundation of marketing ethics involving human rights, dignity and stewardship, and the common good and fair treatment of vulnerable markets.
A recent World Health Organisation (WHO) report acknowledges the “flexibility and enabling role” of public health law in accomplishing the right to health (A. Gray & Vawda, Citation2017). In appreciation of the work by South African activists, Section 27 of the post-apartheid Constitution (Republic of South Africa, Citation1996) also endorses the right to health as a human right when it states, “(1) everyone has the right to have access to (a) healthcare services, and reproductive healthcare” (Annas, Citation2003). Consequently, as a fundamental human right, access to healthcare is viewed as value (Cosma et al., Citation2020). Groenewoud et al. (Citation2019) have further argued that introducing a business ethics concept into healthcare seems to erode the essential healthcare values. In other words, a single-minded focus on Value-Based HealthcareVBHC) may infringe on the four medical ethics principles; firstly, by neglecting patients’ personal values; secondly, by ignoring the intrinsic value of the caring act; thirdly, by completely ruining patients’ trust of accountable professionals; and lastly, by waiving the social solidarity principle. The premise in this paper includes the argument related to the latter principle in the South Africa’s new National Health Insurance (NHI) system, whereby all taxpayers will contribute to the benefits to be shared across the entire population. Enlightened marketing; ▪customer-value marketing; holds that when an organization builds long-term customer loyalty and relational exchanges by continuously increasing the value customers acquire from its market offering, it can capture value from consumers in exchange (Kotler & Armstrong, Citation2010).
This study uses an enlightened marketing philosophy to revive the long-term performance of the marketing system of the medical aid (Kotler & Armstrong, Citation2008) scheme industry in South Africa (Council for Medical Schemes Annual Report, Citation2017–2018). The norms of professional ethics are usually to consider healthcare as a moral obligation in a decent society that embraces a sense of needs for belonging and caring for the community (Rowe & Moodley, Citation2013). Holcombe (Citation2015) recommends the importance to follow the guidelines of ethical marketing set by the American Marketing Association (Citation2005), and to conduct health-related marketing campaigns that promote the core principles of fairness, honesty, citizenship, respect, and transparency. Care ethics also holds that the existing layers must be uncovered below the surface of outcome measurement to acquire healthcare quality. These layers are:
Firstly, the quality of accomplishing a health need (caring about);
Secondly, the quality to care for (hold responsibility for the specified need and responsiveness, both on physician’s technical care delivery and emotional engagement);
Thirdly, the quality of caregiving (the direct action involved in facilitating the actual physical work of the caring responsiveness);
Lastly, the quality of care receiving (the reactions of the object of care towards the care given (Groenewoud et al., Citation2019)).
Clearly, complex ethical implications affect the daily requirements of healthcare services (Rowe & Moodley, Citation2013). Latham (Citation2004) examines the complexities faced in marketing the medical services ethically in the United States. In this context, from the early 1990s, the health insurance market developed rapidly with products by using above-the-line marketing (i.e. mail adverts and radio media) to gain popularity in the local market (Erasmus et al., Citation2016). In another study that examined the ethics of advertising for healthcare services in the United States, Schenker et al. (Citation2014) have argued that clinical advertising by healthcare organizations constitutes a fiduciary responsibility to patients (both healthcare providers and health organizations are obligated to patients). They insist that the ethics of clinical advertising by healthcare organizations are investigated in isolation from those that do not impose these obligations. In addition, from a legal and ethical perspective, such fiduciary exchange relies on patient trust (British Medical Association, Citation2017).
The healthcare industry probably remains one of the most interrogated industries globally. The marketing ethics of medical services involving hospitals, physicians, medical groups, and other mainstream medical caregivers in the United States have been examined by Latham (Citation2004), while the relevance of the specific “social marketing” element in the development of medical marketing strategies is commended by Cătoiu et al. (Citation2013) in the international context. Unfortunately, the growing business of medical schemes in South Africa makes it a pivotal research area due to its vulnerability to increasing opportunities of unethical marketing. However, issues from unscrupulous parties in this sector (which is a primary area of ethical concern) are rarely explicit. The South African Lancet National Commission Report shows the gaps in management, ethical leadership, and governance as determinants of poor healthcare quality, leading to vast consequences (i.e. overuse of inappropriate care, underuse of evidence-based care, poor patient-driven care, collusion, financial insecurity, patient safety hazards, delay, inefficiency, inequity and corruption), all of which cause unnecessary loss of lives (A. Gray & Vawda, Citation2019). Clearly, such corruption contributes to its high costs and the artificially inflated prices in the South African healthcare sector (Dambisya et al., Citation2008).
The use of private hospitals and related health services closely attached to a medical scheme insurance (A. Gray & Vawda, Citation2017) coverage; since it secures household members from incurring unexpected healthcare costs (Dambisya et al., Citation2008). However, a very high minimum cost of the medical-aid schemes invites criticism about their lack of affordability to many South Africans (Erasmus et al., Citation2016). This then contradicts the notion of managed healthcare as defined in the Medical Schemes Act (No. 131 of 1998) as:
Managed healthcare refers to clinical and financial risk assessment and healthcare management with a vision to facilitate appropriateness and cost-effectiveness of relevant health services within the framework of affordability, using rules-based and clinical management based programmes (Kaplan & Ranchod, Citation2014–2015).
To further cite Erasmus et al. (Citation2016), the Medical Schemes Act (No. 131 of 1998) defines the business of a medical scheme as:
Undertaking liability in return for a premium or contribution
to make provision for the obtaining of any relevant health service;
to grant assistance in defraying expenditure incurred in connection with the rendering of any relevant health service; and
where applicable, to render a relevant health service, either by the medical scheme itself, or by any supplier or group of suppliers of a relevant health service or by any person, in association with or in terms of an agreement with a medical scheme.
According to the Competition Commission of South Africa, the country’s current medical schemes fall into two market categories, namely, the open medical schemes and the restricted medical schemes (which target specific members of the defined group, employer, industry, or union) (Competition Commission, South Africa. H, Citation2018). Many large open schemes have high marketing budgets (i.e. costs embedded into administration fees) and implement tactical and complex strategies and marketing activities (Erasmus et al., Citation2016). While these medical schemes finance the costs of each healthcare benefit package offered to members for a monthly fee, the major concern includes the increasing high hospital and related costs, where members with a benefit package from one scheme perceive the switching costs as high (Competition Commission, South Africa. H, Citation2018). Conversely, perceived high switching costs are the prohibitive factor for dissatisfied customers to divert their loyalty from an organization (Ul Hadi et al., Citation2019). Hence, together with brand and customer loyalty, high switching costs remain the barrier for consumers to change from this product or service that they regularly use (Competition Commission, South Africa. H, Citation2018).
The purpose of this study is to develop and test the conceptual model of the effects of perceived switching costs classified by type (procedural, financial, and relational) and direction (positive and negative), on Customer Satisfaction as well as their effect on perceived marketing ethics of medical-aid schemes in South Africa. This study, therefore, tests the moderating effects of medical scheme contributions and customers’ switching experience on the effects of such costs in terms of Customer Satisfaction. It also examines the satisfaction effects on the perceived marketing ethics of medical schemes. In the literature, Customer Satisfaction is the primary objective of all organizations (Gaski, Citation1999), but its related antecedents for medical scheme customers have not been investigated in the context of medical schemes, especially in emerging markets such as South Africa.
In sum, this paper argues that the inability of satisfied and dissatisfied customers to switch their medical schemes due to higher costs could have a detrimental effect on the perceived marketing ethics of the medical schemes. The next section discusses the scope of the medical scheme market in South Africa.
1.1. Market environment of medical schemes in South Africa
To fulfil the main obligation relating to the constitutional right of provision of access to healthcare, the South African government has enacted a legislative framework in the National Health Act (No. 61 of 2003) (NHA). The purpose is:
to grow a framework for structured uniformity of health system within the Republic, particularly consider liability for the responsibility of the obligations imposed by the Constitution and other regulations guiding health services at the local, provincial and national government spheres (Competition Commission, South Africa. H, Citation2018).
Following the National Health Act (No. 61 of 2003) which authorises medical schemes to hold the legal powers to finance healthcare (Competition Commission, South Africa. H, Citation2018), the promulgation of the Consumer Protection Act (No. 68 of 2008) has introduced amendments to the Act (No. 61 of 2003) (Rowe & Moodley, Citation2013). Medical schemes, therefore, operate under the jurisdiction of the Consumer Protection Act (No. 68 of 2008), which affects the benefit packages in numerous ways:
all representations made to the clients must be in the preferred language that is clearly understood by an ordinary person possessing average literacy skills and understanding;
discriminatory marketing activities are forbidden, i.e. exclusion of persons from any goods or services or target particular communities for exclusive supply of goods or services (Kaplan & Ranchod, Citation2014–2015).
In South Africa, as stipulated in the Medical Schemes Act (No. 131 of 1998), the medical schemes are the primary private health-financing mechanism and similarly managed for the nonprofit trust funds (Erasmus et al., Citation2016; Kaplan & Ranchod, Citation2014–2015). They are regulated by a separate and independent regulatory authority − the Council for Medical Schemes (CMS) − which aims to increase access to good quality medical scheme cover and protect the consumer’s best interests (Kaplan & Ranchod, Citation2014–2015). The marketing literature also recommends organizations to perform ethical practices to secure their customers’ best interests (Hunt, Citation2010). That is, the marketing decision-making process of enlightened organization; ▪societal marketing concept considers consumers’ interests and wants, the organization’s requirement, and society’s interest in the long term (Kotler & Armstrong, Citation2008).
Before the promulgation of the Medical Scheme Act (No. 131 of 1998) in 2000, not all the medical schemes abided by the responsibility to report to a central body. This increased the possibility that data and figures reported prior this enactment could have understated the financial irregularities incurred by the schemes and the number of people who could access medical schemes (Dambisya et al., Citation2008). Today, all the medical schemes are obliged to comply with the requirements of the Medical Schemes Act (No. 131 of 1998), unless the Council for Medical Schemes (CMS) exempts the medical schemes from certain provisions of the Act (Erasmus et al., Citation2016).
Introducing the Medical Schemes Act (No. 131 of 1998) in 2000 brought together the principles of social solidarity in the medical scheme market, i.e. open enrolment, community rating and it also mandated all the medical schemes to offer the Prescribed Minimum Benefits (PMBs) (Erasmus et al., Citation2016; A. Gray & Vawda, Citation2017; Kaplan & Ranchod, Citation2014–2015). Each medical scheme markets a variety of product portfolios to customers (known as benefit options or benefit packages) which differ in design, and each medical scheme (approved and registered with the Council for Medical Schemes (CMS)) has to ascertain if the design meets the prescribed standard set in the Medical Schemes Act (No. 131 of 1998). The Low-Income Medical Schemes (LIMS) report shows that the scope of these PMBs requires revision, as they constitute high-base cost; thereby driving medical scheme cover prices higher (Kaplan & Ranchod, Citation2014–2015).
According to the World Health Organisation (WHO), “health monitoring must extend beyond the health sector and realise the economic, social, and environmental factors, including inter-sectoral initiatives” (A. Gray & Vawda, Citation2017). In 1992/93 an estimated cost of R30 billion (8.5% of GDP) was spent on healthcare in South Africa. This varied between the private sector (60.8%) and the public sector (38.7%) (A. Gray & Vawda, Citation2017). By 1998/99, up to 59% of the total South African health sector resources (i.e. financial and human) were consumed in private healthcare, covering less than 20% of the population (i.e. people who access and use health services via the medical schemes) (Dambisya et al., Citation2008). In 2002, the medical schemes dominated the pre-funded health finance market in South Africa with the top three administrators holding 49.3% of market share, driven by industry alliance (e.g., Momentum and Metropolitan formed the union entity of MMI Holdings) (Erasmus et al., Citation2016). This rose to 80% in 2014 and as a result, the total medical scheme expenditure increased (in nominal terms) from R127.2 billion in 2014 to R138.6 billion in 2015, or R15 822.76 per average beneficiary per year. This accounted for hospital care (37.1%); medical dispensaries in pharmacies; and health service providers beyond the hospitals (16.1%); supplementary and allied health professionals (7.2%); medical specialists (6.6%); and general practitioners (GPs) (6.2%) (A. Gray & Vawda, Citation2017). The 2015 General Household Survey revealed that 9 458 000 (17.5%) South Africans had medical scheme cover, while 23.5% of households had at least one member who was covered (A. Gray & Vawda, Citation2017). In 2016, the medical scheme's expenditure accounted for 41.8% of the total healthcare expenditure − considered high according to international standards. However, it should be noted that medical scheme members volunteer for cover, and the medical scheme contribution is a service condition imposed by employers (Erasmus et al., Citation2016).
Consequently, the 2017 increase of Value Added Tax (VAT) from 14% to 15% was a challenge for medical schemes in South Africa and this slowed the growth in the general numbers of medical scheme membership. As rising membership is a driver of medical scheme business growth, the fall in membership was attributed to weak economic growth (i.e. low GDP, negative credit ratings, etc.). In 2018, members benefited from the lower average monthly contribution of 7.2%, compared to 11.3% proposed in 2017 (Council for Medical Schemes Annual Report, Citation2017–2018). Despite this, the cost of pre-funded healthcare in South Africa has since increased to a rate above the Consumer Price Index (CPI), which has pressurized the medical scheme costs for a while, and more recently, the cost of health insurance products. Thus, a growth in the usage of medical services among customers is the key driver of costs (Erasmus et al., Citation2016).
Presently, the South African population is estimated at 55.5 million (National Department of Health, Citation2016), yet over 50% of the total healthcare expenditure serves only 16% of the population (8.8 million people) covered by the medical schemes in the private sector (Erasmus et al., Citation2016; A. Gray & Vawda, Citation2017; Maphumulo & Bhengu, Citation2019; National Department of Health, Citation2014). Clearly, this raises concerns when the affordability of medical schemes is examined: the relatively high proportion of the state’s healthcare expenditure flows into medical schemes which only serve the minority of the population (16%) (Erasmus et al., Citation2016). Currently, over R200 billion is spent on 16% of the population who currently have a medical scheme cover (A. Gray & Vawda, Citation2019). Consequently, in the private sector, an estimated 80% of medical specialists in South Africa serve the same population (16%) (Maphumulo & Bhengu, Citation2019; National Department of Health, Citation2016), while 84% of the South Africans rely heavily on the government’s under-resourced public health sector for their health needs (Maphumulo & Bhengu, Citation2019). The obvious difference, however, is that the public facilities render free care for most medical conditions while private facilities charge a service fee (Jacobsen & Hasumi, Citation2014). Thus, consumers covered by medical schemes are likely to have a high socio-economic status and their preference is to visit the private facilities that they perceive offer a higher standard care. Therefore, socio-economic status has been shown to predict Customer Satisfaction with private healthcare in South Africa (Ayo-Yusuf et al., Citation2016; Dambisya et al., Citation2008).
The Medical Schemes Act (No. 131 of 1998) aims at reducing the discriminatory clauses by matching the schemes’ operations in accordance with the Constitutional vision of the provision of more equitable medical care (Dambisya et al., Citation2008). However, social inequalities in access to medical scheme cover still persist (e.g., the number of “Africans” on medical schemes has reduced from 10% in 1996 to 8% in 2003, while coverage for “white” members reflected at over 60%) (Dambisya et al., Citation2008). The problems identified by McIntyre (Citation1995), for example, the overall maldistribution between the private and public sectors (relative to the populations served); the overall under-resourcing of the public sector; maldistribution of funds between geographical areas with relatively affluent (urban) areas acquiring a greater proportion than underdeveloped areas (rural, ex-homeland); and maldistribution between levels of care, still persist in 2017. The National Health Insurance (NHI) policy, however, aims to eradicate these imbalances (A. Gray & Vawda, Citation2017) between the current co-existing private and public health sector systems. This is the premise of “social solidarity”.
1.2. National health insurance (NHI)
The National Health Act (No. 61 of 2003) together with other laws and policies, e.g., the National Development Plan (NDP) and the National Health Insurance (NHI) form the regulatory framework governing the provision of health service in South Africa (Competition Commission, South Africa. H, Citation2018). The NHI refers to a series of major health system reforms that aim to promote the social solidarity principle, as well as to address issues of greater quality and equity in the South African healthcare sector (Erasmus et al., Citation2016; Rowe & Moodley, Citation2013) that is not achieved to date.
As endorsed by the National Health Plan, the provision of Universal Health Coverage (UHC) aims to enable a conducive environment for public-private health sector interactions (African National Congress, Citation1994). The World Health Organisation (WHO) insists that:
Accelerating the progress in provision of Universal Health Coverage (UHC) depends on three broad principles to guide health financing reforms. First, [a] shift towards a predominant reliance on compulsory (i.e. public) funding sources. Second, [to] reduce fragmentation in pooling to enhance the re-distributional capacity of these prepaid funds. Lastly, [a] shift towards strategic purchasing, which intends to align funding and incentives with promised health services (A. Gray & Vawda, Citation2019).
One key element of the NHI reforms, therefore, is the design of a split between purchaser-to-provider through the provision of a “single-buyer” services body. This aims to strategically purchase health services despite affiliation with the private or public sector. Such a classic feature is provided in health services markets in the developing countries (Wagstaff et al., Citation2016), but is still absent in the context of South Africa (Competition Commission, South Africa. H, Citation2018).
The crux of the NHI healthcare system is that the health risk will be cross-subsidised to all the citizens of South Africa (Erasmus et al., Citation2016; Rowe & Moodley, Citation2013). Consequently, all taxpayers or income earners will make mandatory contributions so that the benefits are shared across the entire population, including people who are unable to make a direct monetary contribution to the NHI fund (French, Citation2012; A. Gray & Vawda, Citation2018; Rowe & Moodley, Citation2013).
The potential for NHI to generate additional funds for the healthcare sector and to enhance equity and efficiency relies largely on the implementation of finance, pools, purchase, and provision of reforms (A. Gray & Vawda, Citation2017). Areas of interest for NHI funding include establishing the interim NHI fund and developing health techno-assessment capacity (A. Gray & Vawda, Citation2018). The overall tax subsidy of R15.9 billion in 2014 which equates to 12% of gross contributions has indicated an improved equity between the medical scheme tax subsidy and the cost per capita in the public sector. Consequently, this has sparked discussions on the possible removal of this tax subsidy and redirecting it towards the NHI funds (Erasmus et al., Citation2016). A major adjustment to the 2017 Medium Term Budget Policy Statement was the allocation of R4.2 billion to the NHI fund via the adjustments of medical credits on personal income tax at a margin below inflation for a three-year period, i.e., R700 million (year one), R1.4 billion (year two) and R2.1 billion (year three) (A. Gray & Vawda, Citation2018). Thus, the White Paper estimates a funding deficit of R72 billion for NHI by 2025/26 due to an expected 3.5% annual economic growth rate (A. Gray & Vawda, Citation2019).
Predictably, the NHI is envisioned to erode many of the health service sector’s challenges (Erasmus et al., Citation2016); since the private medical scheme sector can expect vast disputes subsequent to the introduction of NHI, such as the separation between health insurance and medical scheme cover, and the constantly evolving regulatory environment (French, Citation2012). However, looking further ahead, if these NHI reforms are implemented successfully, the current high demand for private over the public healthcare will disappear naturally, with medical schemes expected to play a substantially reduced role by providing only supplementary healthcare cover (Erasmus et al., Citation2016). The NHI services benefit package and the Prescribed Minimum Benefits (PMBs) will be merged to assist members to transit swiftly from medical schemes to NHI (French, Citation2012). In addition, a capitation payment system (i.e. the doctor paid a specific amount per enrolled person for a set period of time) will be adopted to incentivise underprovision of services by doctors. Thus, extensive consultations with the medical professional groups in South Africa are critical, as many health workers could migrate to the developed countries (A. Gray & Vawda, Citation2019). The rationale for this is that the more services they actually provide, the more a patient is costing them (Rowe & Moodley, Citation2013). Capitation payments will complement the performance-based payments to limit unnecessary referrals and reach targets for preventive services (Competition Commission, South Africa. H, Citation2018; A. Gray & Vawda, Citation2019).
1.3. Objectives of the study
Switching costs in competitive health insurance markets were examined by Lamiraud (Citation2013); however, a critical area of the ethical marketing is for medical schemes to meet consumers’ expectations. This study, therefore, offers a novel architecture to bridge the gap of limited research on the effects of perceived switching costs on Customer Satisfaction, and the consequent outcome on perceived marketing ethics of medical schemes. The objectives developed to measure the identified marketing research problem include:
an examination of the effects of perceived switching costs on Customer Satisfaction;
a proposal to test a conceptual model on the effects perceived switching costs on Customer Satisfaction, and the resultant effect on perceived marketing ethics.
an investigation on the moderating effects of the medical scheme contributions and customer switching experience and the threefold impact of the perceived switching costs on satisfaction, satisfaction effects, and marketing ethics in the South African healthcare sector.
To achieve these objectives requires a rigorous study that answers the following questions:
What is the role of perceived switching costs on customers’ satisfaction?
How does satisfaction affect perceived marketing ethics?
Do the medical scheme contributions and consumers’ switching experience moderate the effects of perceived switching costs on Customer Satisfaction, and the satisfaction effects on marketing ethics?
In general, this paper has described the background information critical to develop an understanding of the problem investigated in this study and to develop the research objectives and the research questions. The next section discusses the literature review on the switching costs, Customer Satisfaction, and marketing ethics, including multiple theories fundamental to the development of the conceptual model shown in Figure . The research methodology applied in the systematic design, collection, analysis, and interpretation of the findings will be discussed, including the practical implications and recommendations, and limitations of this study and future research ideas.
2. Literature review
The issues of ethical principles and social responsibility are guided by two philosophies. The first philosophy does not oblige organizations and their managers to inherit the responsibility for making moral decisions, but ethical issues follow and are decided by both the free market and legal system. The second philosophy rests the responsibility in the hands of the organizations and their managers, and not on the system, which is an enlightened philosophy that embraces “social conscience” (reflecting beyond the legal systems and allowed) and which adheres to the standards of corporate conscience, personal integrity, and long-term customer welfare (Kotler & Armstrong, 2008).
Thus, organizations follow corporate marketing ethics as broad guidelines affecting its product development, pricing, distribution relations, advertising standards, customer services, and the general ethical standards (Kotler & Armstrong, Citation2010). From the perspective of Marketing 101, Latham (Citation2004) has examined ethics in the marketing of medical services and has argued that each of the four P’s (i.e. product, price, place, promotion) have a component of ethical questions. He insists on the importance of an attempt to determine the selling price at which the product or service will generate more profit to the seller and still be attractive to the target consumer (e.g., should the product or service cost less, be a “loss-leader,” or a high markup cost, such as luxury goods?).
In the healthcare sector, the medical schemes use a price-rationing method. That is, goods and services are sold to consumers who are able and willing to pay the price. The “price” in this view constitutes the contribution rate and the degree of out-of-pocket payments incurred from levies, co-payments, tariff shortfalls, and other deductibles (A. Gray & Vawda, Citation2019; Kaplan & Ranchod, Citation2014–2015). The 2010 results of the South African General Household Survey (GHS) show that 93.4% of patients who visited a private facility paid for their services via a medical scheme or from out-of-pocket, while only 6.6% visited a public healthcare facility (Jacobsen & Hasumi, Citation2014). This shows that many South Africans use medical schemes to access private hospital care, while those without medical scheme cover pay out-of-pocket to gain these benefits (Erasmus et al., Citation2016).
Paradoxically, the research shows the price elasticity of demand for medical schemes as relatively low (Erasmus et al., Citation2016). The challenge with price competition in the healthcare sector is that it reluctantly relies on the private (in terms of quality and expense) rather than public (government) health insurance to fairly ensure that patients and their doctors determine prices, and choose the healthcare service they want to purchase (Competition Commission, South Africa. H, Citation2018). As the “buyer beware” concept is not acceptable, today’s business laws (anti-trust law, consumer protection law, etc.) have been promulgated to help consumers to make well-informed market choices, and enable specialised protection to novice customers (Axtell-Thompson, Citation2005; Sirgy & Lee, Citation2008). The Economic Theory holds consumers to be as well informed as possible about the key features of goods or services they purchase (Bhattacharya, Citation2013). Furthermore, Economic Theory argues that healthcare markets are destined for failure in ways that have a detrimental effect on the patients’ interests. For example, the General Practitioners (GPs) are responsible for a vast number of patient referrals, and have control over the commissioning budget, thereby generating cost savings. If patients could choose their healthcare providers, and if those providers are paid a fixed sum for each service episode of care they render, then, from the market logic perspective, those providers would compete on the basis of service quality and experience, thus, giving patients more choice (British Medical Association, Citation2017).
From a legal perspective, all patients are considered “consumers”, which enables them to enjoy the rights of the consumer, such as the right to choose; the right to privacy; the right to disclosure of information; the right to fair, just and reasonable terms and conditions; the right to fair and honest dealing; the right to fair value, good quality and safety; the right to fair and responsible marketing; the right to equality in marketing; and the right to hold their suppliers accountable (Rowe & Moodley, Citation2013). For over 30 years, the NHS in England, a developed country, has been subjected to growing market-oriented supply-side reforms driven by the goal of efficiency savings and the aim to allow patient choice and enhance healthcare satisfaction (British Medical Association, Citation2017). Researchers probing into the ethical limits of choice and responsibility in healthcare (Axtell-Thompson, Citation2005, p. 212) have echoed the importance of a well-informed market choice and asks “can consumers switch to another supplier?”. From a holistic view, the appropriateness of choice relies on the “switching costs”, intensity of rivalry, and the firm’s market share in the industry.
Further, understanding consumer behaviour has become complex due to the variety of competitive products and services, and the satisfied customers’ willingness to try new products and those of rivals, which enhance the temptation to switch (Willys, Citation2018). Consequently, many firms increase switching costs to reduce the customers’ desire to switch to competitors (M.A. Jones et al., Citation2000). Obviously, switching intentions rarely occur if the incumbent firm satisfies customers (Zeithaml et al., Citation1996). Balabanis et al. (Citation2006) have revealed that switching costs are more influential when Customer Satisfaction is low. Hence, the two primary strategies for retaining customers are by increasing switching costs and enhancing Customer Satisfaction through a balanced management process. Ethics and practice applications show that organizations can increase switching costs by adding customer value (e.g., teach customers to identify the unique product benefits, use the product better, and gain the valuable rewards and bonus), and by building long-term customer relationships (Burnham et al., Citation2003). The consumer values health service provider whose activities engage with and treat customers as partners in an overall approach to their care, who is honest, listens and acknowledges their varied conditions, and treats them equally (Hassmiller & Bilazarian, Citation2018) will satisfy consumers, as they are generally cared for. This situation further leads them to perceive this provider as either ethical or unethical (Javed et al., Citation2019).
When purchasers “buy” the best possible care at the lowest possible cost (Groenewoud et al., Citation2019), consumers behave as critical healthcare customers and tend to evaluate the switching costs and develop various satisfaction responses to these costs (Klemperer, Citation1995). If switching costs are higher, Customer Satisfaction is negatively impacted (Nagengast et al., Citation2014; Willys, Citation2018; Yen, Citation2010). This indicates that, in the firm’s short-term defensive marketing strategy, the positive relationship between switching cost and satisfaction is mixed (Fornell, Citation1992); however, in the long term, the organization’s ability to retain the patronage of dissatisfied customers through switching cost costs is limited. In other words, switching costs and satisfaction may interact negatively in driving customer intentions (M.A. Jones et al., Citation2000).
In the literature, Bolton (Citation1998) has identified the significance of Customer Satisfaction for the cellular communication industry in relation to switching. Biedenbach et al. (Citation2015) found the positive effect of switching costs on Customer Satisfaction in the B2B setting. Sanjeepan (Citation2017) has confirmed a moderate positive interaction of switching costs and Customer Satisfaction for Internet banking services at commercial banks in Batticaloa, Sri Lanka, which is a developing country. Moliner (Citation2009) found the effect of functional value consisted of monetary costs and non-monetary costs on consumer satisfaction in the public and private healthcare sector in Valencia (Spain). Thus, the question of how switching costs and Customer Satisfaction relate is under-researched in the medical scheme industry, especially in the context of emerging markets such as South Africa. Given the scant research on switching costs management, the marketing effort to increase Customer Satisfaction waives the relevance of switching costs, or worse, the marketing field has “blacklisted” switching costs as very painful to customers and unworthy to study (Burnham et al., Citation2003).
A SERVQUAL model developed by Parasuraman, Zeithaml and Berry (Citation1992) is a widely used instrument measuring customers’ perceptions of service quality in a service industry. It has been adopted in previous studies that measure patients’ satisfaction about healthcare service quality as a fundamental factor of the overall performance system evaluation of healthcare (Cosma et al., Citation2020; Dambisya et al., Citation2008; Maphumulo & Bhengu, Citation2019; Nwobodo-Anyadiegwu et al., Citation2018). However, a gap exists in the literature on the impact of switching costs on consumer satisfaction linked to the medical schemes industry. There is also little insight on the impact of switching costs on consumer behaviour in the context of medical schemes in South Africa. Consumers’ perception of marketing ethics of medical schemes in the post-purchase evaluation stage is unknown. This study, therefore, closes this gap by focusing the enlightened marketing view on the conceptualisation and testing of the switching costs on Customer Satisfaction, and their effect on the marketing ethics of medical schemes in South Africa. Enlightened marketing; ▪ Consumer-oriented marketing; means sensing, serving, and satisfying the consumer needs (Kotler & Armstrong, 2008). A. Gray and Vawda (Citation2017) report that, in South Africa, 88% of the patients were “very satisfied” or “somewhat satisfied” with their medical schemes compared to 83% of patients without medical scheme cover. It was expected that the anticipations of medical scheme members would be high given their higher-income status and payment for health cover. Their satisfaction could also be potentially affected by shorter waiting times and better amenities in the private sector. Ayo-Yusuf et al. (Citation2016) confirm that medical scheme membership has an indirect impact on satisfaction (i.e. if the patient could have used a private facility rather than a public facility) for the following reasons:
it reduced the financial burden of out-of-pocket payment for care visit;
lowered the perceived expensive of the treatment; and
ultimately, limited customers’ dissatisfaction.
Customer dissatisfaction occurs when a customer has expectations more than the organization’s level of performance (e.g., perceived quality is lower than Customer Satisfaction) (Nwobodo-Anyadiegwu et al., Citation2018). In South Africa, Jacobsen and Hasumi (Citation2014) have reported no variance in customers’ satisfaction with medical scheme cover (e.g., health insurance plan).
In a study on patients as consumers of healthcare in South Africa, Rowe and Moodley (Citation2013) highlight the ethical and legal implications for healthcare systems, healthcare providers and the doctor and patient relations. Gundlach and Murphy (Citation1993) show customer trust, equity, responsibility, and commitment as the necessary ethical and legal foundation for fair and open relational marketing exchange. An ethical brand is characterised by features of respect, diversity, quality, honesty, integrity, responsibility, and accountability, and such ethical brands promote themselves without ruining their consumer’s morale (Javed et al., Citation2019). Consequently, firms complying with high standards of organization ethics (social responsibility to act ethically and provide benefits to society) create a competitive advantage and generate profit by:
lowering the business transactional cost;
establishing customer trust;
building the internal services scope (i.e. teamwork success); and
acquiring social capital gains endorsed by a positive image in the public eye (McMurrian & Matulich, Citation2016; Mohammed & Rashid, Citation2018).
2.1. Theoretical foundation, conceptual framework and hypotheses development
Cognitive Dissonance Theory and Self-perception Theory posit that consumers who feel “locked-in” will be defensive about it and think of themselves as satisfied, while dissatisfied customers attribute “being locked-in” to actions of a firm and will certainly feel highly dissatisfied (Burnham et al., Citation2003, p. 20). They have related to a question investigated in this current study, by asking: “can switching costs independently impact dissatisfaction”? They contend that studies which could answer such question would be capable of managing the dynamic and contextual effects of perceived switching costs. In consideration of this view, this current study develops and tests a conceptual model (see Figure below) of switching costs as a multi-dimensional construct using a typology of switching cost categories developed by Burnham et al. (Citation2003). These are the three switching cost types classified into eight distinct facets:
Procedural switching costs (i.e. facets of economic risk, evaluation, learning, and setup costs) measure the loss of time and effort;
Financial switching costs (i.e. facets of benefit loss, monetary loss) measure the loss of financially quantifiable resources; and
Relational switching costs (i.e. facets of personal relational loss, brand relational loss costs) measure the emotional discomfort from the identity loss and ending bonds.
The multi-dimensional view of the switching costs construct will:
clarify the theoretical explanatory power of the construct (Whitten & Wakefield, Citation2006);
clarify the relevant theoretical and managerial implications across types of switching costs (M.A. Jones et al., Citation2007); and
properly interrogate the interactions of switching costs and other related constructs (Barroso & Picón, Citation2012) measured in this study.
Switching costs are not mutually exclusive. As time cost is a key element of setup and learning costs, switchers often reduce these costs via monetary costs or setup costs (i.e. purchase learning materials, instructor services or installation services) (Parry & Sarma, Citation2019).
Further, switching costs fall into two distinct types, i.e. positive switching costs and negative switching costs (M.A. Jones et al., Citation2002). Ngo and Pavelková (Citation2017) believe that this classification is useful for practitioners as it provides detailed guidance for applying switching costs in enhancing customer loyalty. However, in the light of Attribution Theory, Bhattacharya (Citation2013) argues that customers should perceive switching costs that reflect high customer value positively. Empirical evidence shows that positive switching costs positively affect Customer Satisfaction while negative switching costs negatively affect satisfaction (Julander & Söderlund, Citation2003). As positive switching costs are benefits beyond the core service, they may give rise to substantially different emotional and behavioral responses than do negative switching costs (Marcos, Citation2018). Nagengast et al. (Citation2014) have merged the two types of positive switching costs (i.e. financial and relational switching costs) into a single factor, despite other studies (Blut et al., Citation2015; Burnham et al., Citation2003; M.A. Jones et al., Citation2007) that have measured financial and relational switching costs as separate constructs. Surprisingly, however, there are no such research studies in the health services industry that separate positive and negative switching costs, as recommended in the literature (Burnham et al., Citation2003; M.A. Jones et al., Citation2002, Citation2007). This raises the question of the need to understand the varied mechanisms or routes through which various switching costs influence Customer Satisfaction and how this satisfaction impacts the perceived marketing ethics of medical schemes.
The Disconfirmation Expectation Theory developed by R.L. Oliver (Citation1999) is a dominant theory of consumer behaviour cited widely in the literature that links the satisfaction outcomes to the differences in expected and actual product performance. It posits that customers evaluate their satisfaction from an overall evaluation of their perceived services experience in terms of whether the services consumption meets or exceeds their prior expectations. Any discrepancy between expectations and actual performances creates a positive disconfirmation (performance exceeds expectations) or a negative disconfirmation (expectations exceed performance). Confirmation and positive disconfirmation lead to satisfaction, whereas negative disconfirmation leads to dissatisfaction.
Consequently, consumer dissatisfaction has a negative impact on the perceptions of the marketing ethics of an organisation (Chonko et al., Citation1996; Thomas et al., Citation2002). Hunt and Vitell (Citation1986) introduced the General Theory of Marketing Ethics as a unified framework that measures ethical judgements within specific sales situations by depicting a “perceived ethical problem” as a catalyst of the ethical decision-making process of marketers. The ethical decisions rely on deontological norms and judgments and on teleological norms and judgements. The deontological norms rely on hypernorms and local norms of the Integrative Social Contracts Theory (Ferrell & Ferrell, Citation2008). By its nature, the definition of marketing is a precept grounded in the utilitarian approach to ethics as marketers set a deontological approach to marketing (Nantel & Weeks, Citation1996). In general, the multiple theoretical approach guides the theoretical explanatory power of constructs and their interactions as shown in the conceptual model (see Figure ).
2.2. Switching costs
From his seminal work of strategic management literature of “Competitive Strategy”, Porter (Citation1980, p. 10) defined switching costs as “onetime” costs, rather than the ongoing costs in the repeat purchase with an organization. This definition guides the formation of switching costs typology by Burnham et al. (Citation2003). The switching cost definition measures the monetary cost, psychological and emotional costs incurred in facing the uncertainty of dealing with another firm (Dick & Basu, Citation1994).
The management, economics, and marketing literature view considers switching costs as industry-specific and consumer-specific (Fornell, Citation1992; Klemperer, Citation1995). In the service industry, switching costs refer to consumers’ subjective evaluation of perceived costs incurred in changing a service firm (Burnham et al., Citation2003). In the medical scheme industry, switching costs refer to the subjective evaluation of perceived costs that the customer incurs in leaving a medical scheme services provider.
2.2.1. Procedural switching costs
Procedural switching costs are viewed by Burnham et al. (Citation2003) as the traditional view of what switching costs that involve the following:
the consumers’ perceived complexity of effort in the search for information prior switching a firm (pre-switching costs),
evaluation of the relevant steps (uncertainty costs); and
learning the procedures and routines of a new firm (setup costs).
Higher perception of procedural switching costs affects the switching barrier (M.A. Jones et al., Citation2000). The literature has emphasized that the procedural switching costs often making it difficult for customers to switch a firm (e.g., the time and effort in the search for a new firm, and challenges incurred in terminating a contract) derive from the negative sources of constraint, hence, falling in the domain of negative switching costs (M.A. Jones et al., Citation2007; Ngo & Pavelková, Citation2017). While Burnham et al. (Citation2003) have measured procedural switching costs consisting of the economic risk costs, evaluation costs, set up costs, and learning costs, this study examines economic risk costs (i.e. perceived alternatives’ risk or uncertainty) and evaluation costs (i.e. time and effort costs to find new medical scheme and the challenges incurred in terminating a contact) due to the nature of the business of medical schemes. Nagengast et al. (Citation2014) have found that customers perceive even small procedural switching costs as painful and do not switch even when they are dissatisfied. Burnham et al. (Citation2003) and M.A. Jones et al. (Citation2007) refer to this condition as “being locked-in” and it completely forces customers to stay in the relationship, thus forming perceived calculative commitment.
2.2.1.1. Economic risk costs
Economic risk costs refer to perceived psychological costs faced with the “perceived alternatives’ risk or uncertainty of the potential negative consequences that may occur when adopting a new firm whom a customer has less information” (Burnham et al., Citation2003, p. 111), as unused brands may not meet his or her expectations due to uncertainty. This study, therefore, hypothesises that:
H1: Economic risk costs have a significant direct negative effect on Customer Satisfaction.
2.2.1.2. Evaluation costs
Evaluation costs refer to “the time and effort costs in the search and analysis required to make a switching decision” (Aydin & Özer, Citation2005), and require the mental effort to analyse and restructure information to arrive at a meaningful decision (Burnham et al., Citation2003, p. 111). This study, therefore, hypothesises that:
H2: Evaluation costs have a significant direct negative effect on Customer Satisfaction.
2.2.2. Financial switching costs
Financial switching costs are financially quantifiable costs that customers incur in transitioning from an incumbent firm (Aydin et al., Citation2005). These switching costs involve structural bonds imposed by the incumbent firm, capturing costs stemming from the specific benefits lost when switching (costs of lost performance), and loss of investments (sunk costs) (Burnham et al., Citation2003). Burnham et al. (Citation2003) have also classified financial switching costs as the benefits loss and monetary loss costs. The benefits loss costs and monetary loss costs are viewed as positive switching costs (foregone gains) that derive from the positive sources of constraint and reflect the positive value and behaviours that customers sacrifice when leaving a firm (Burnham et al., Citation2003; M.A. Jones et al., Citation2002).
2.2.2.1. Benefit loss costs
Benefit loss costs refer to “the costs incurred in the contractual bonds that establish economic benefits for staying with a firm” (Burnham et al., Citation2003, p. 111). The net effect of switching efforts relies on the perceived strength of switching costs against the corresponding benefits (Yang & Peterson, Citation2004). Benefits involving membership programs and frequent flier discounts, for example, show an increment’s core service relationship (Aydin & Özer, Citation2005). Hence, a customer who switches the firm loses these benefits and prerequisites accrued from past services patronage (M.A. Jones et al., Citation2002). Positive switching costs (social and lost benefits) impact Customer Satisfaction (Julander & Söderlund, Citation2003; Meng & Elliott, Citation2009). This study, therefore, hypothesises that:
H3: Lost benefits costs have a significant direct positive effect on Customer Satisfaction.
2.2.2.2. Monetary loss costs
Monetary loss costs or “the onetime financial outlays [that] incur when switching a firm instead of costs spent in purchasing a new product itself” (Burnham et al., Citation2003:111; Klemperer, Citation1995). Monetary switching costs include penalties for switchers to lose the monetary benefits acquired from long-term membership and the costs required by a new firm (Kim et al., Citation2019). In the medical scheme market, for example, monetary loss costs include not only the costs of purchasing a new benefit package but also the sunk cost of a switched benefit package (Porter, Citation1980). Hence, switchers will incur onetime costs such as a deposit or initiation fee from a new firm (Burnham et al., Citation2003). In the health sector, Moliner (Citation2009) reports that monetary costs and service quality are critical determinants of Customer Satisfaction in private sector, while in a public sector, in terms of Customer Satisfaction, all the factors of perceived value are equally relevant, though the non-monetary costs stand. This study, therefore, hypothesises that:
H4: Monetary loss costs have a significant direct positive effect on Customer Satisfaction.
2.2.3. Relational switching costs
Relational switching costs represent “the onetime costs that customers incur for switching a firm and the subsequent costs need to re-establish a new relationship” (Burnham et al., Citation2003, p. 111). The literature suggests that switching costs are the customers’ perceived magnitude of additional costs incurred to break the bond with the firm and expenditures incurred to secure a place in a new firm (Ram & Wu, Citation2016; Willys, Citation2018). Relational switching costs occur if comfort, faith, understanding, and affection in the firm create a switching barrier for customers (M.A. Jones et al., Citation2007), since they reflect relationship-specific assets (e.g., learnt procedure, proprietary system, brand preference, etc.) valued by exchange parties (Bhattacharya, Citation2013; Tuu, Citation2015). Value refers to customer’s perceived variances between the personal revenue generated (results and process quality) and the personal cost (price and acquisition cost) (McMurrian & Matulich, Citation2016). Hence, instances of leaving a firm’s brand (brand relations costs) or contact staff (personal relations loss costs) may cause emotional discomfort for that customer (Burnham et al., Citation2003). In retail banking, Ngo and Pavelková (Citation2017) report that customers treat positive switching costs as good initiatives from their banks and that they enhance the emotional relationship to their banks. Burnham et al. (Citation2003) measured relational switching costs consisting of the brand relations costs or contact personnel (personal relations loss costs). The nature of the business of medical schemes makes it relevant to examine personal relational loss costs incurred in breaking the bond.
2.2.3.1. Personal relationship loss costs
Personal relationship loss costs are “the affective losses involving psychological or emotional discomfort due to identity loss or breaking the relationship and acquaintance with the firm and its staff” (M.A. Jones et al., Citation2000, p. 262). Blut et al. (Citation2014) found a positive effect of relational switching costs on customers’ cross-buying behaviour across the firm’s product categories, and its share of the wallet. Relational benefits focus on the relationships rather than on performance and positively increase Customer Satisfaction (Hennig-Thurau et al., Citation2002). Higher levels of Customer Satisfaction are a significant antecedent of relational switching costs, as customers avoid breaking bonds that meet their expectations and satisfy them (Gounaris & Boukis, Citation2013; Tuu, Citation2015; Yoon & Suh, Citation2003). This study, therefore, hypothesises that:
H5: Personal relationship loss costs have a significant direct positive effect on Customer Satisfaction.
2.3. Customer satisfaction
Satisfaction is defined as “a state of pleasurable fulfilment response from a judgment that a product or a service provides a pleasurable consumption-related fulfilment, including under- or over-fulfilment” (R.L. Oliver, Citation1997, p. 27). The consumer’s response is an outcome of a cognitive evaluation process of whether a service meets a pleasurable level, thereby fulfilling a need and want after single or multiple contacts (R.L. Oliver, Citation1993). The consumer senses that the medical scheme is fulfilling a need, goal, desire, or so forth and that this forms a state of pleasurable fulfilment. Thus, satisfaction is the customer’s sense that the medical scheme services offer outcomes forming a standard of pleasure as opposed to displeasure state.
The philosophy of “marketing concept” views Customer Satisfaction as the key factor in achieving organisational goals (Gaski, Citation1999). Customer Satisfaction is a critical determinant of keeping long-term patient loyalty and achieving a competitive advantage (Chang, Chen & Lan, Citation2013; Moliner, Citation2009; Nwobodo-Anyadiegwu et al., Citation2018; Shan et al., Citation2016; Tang, Citation2011). The most commonly selected criteria for measuring Customer Satisfaction with health services include the hospital servicescape, service type (public or private), health condition, politeness of the service contact staff, core service (i.e. the policy), and insurance provider, among others (Cosma et al., Citation2020; Crosby & Stephens, Citation1987; Singh, Citation1991). This study examines satisfaction in the medical scheme context to enhance the knowledge on how customers evaluate overall healthcare and make judgements.
Customer Satisfaction is defined as “positive affective responses resulting from the post-purchase evaluation of all relationship aspects with a firm” (Geyskens et al., Citation1998, p. 224). This study examines satisfaction as the consumers’ evaluation of the overall core services of medical schemes, as each service contact may positively or negatively affect satisfaction. Thus, even if consumers evaluate overall in a summary, or judge its separate features, either way, satisfaction with healthcare experience is a multi-dimensional construct, derived from the judgment of varied features (Crow, Gage, Hampson, Hart, Kimber, Storey & Thomas et al., Citation2002). Moliner (Citation2009) has applied Agency Theory in healthcare to examine the theoretical base and concepts of post-purchase perceived value and relationship quality among hospital users. Patient satisfaction was regarded as evaluation between the outcomes of cumulative service transactions; both consumed and prior to expectations. A cumulative satisfaction cumulates customers’ satisfaction in a long-term, sequential series of episodes forming overall satisfaction, and it is a key fundamental factor in the firm’s past, current and future performance (Lam et al., Citation2004). Thus, a transaction-specific satisfaction defines a consumer’s emotional response into a single pleasant transaction experience (R.L. Oliver, Citation1993), which shows that satisfaction is achieved by cultivating long-term customer relationships with the objective to retain valuable customers rather than pursuing single transactions (Tuu, Citation2015). Hence, for a customer’s satisfaction to affect loyalty, a cumulative satisfaction is needed for satisfaction episodes to be blended (R.L. Oliver, Citation1999).
2.4. Marketing ethics
Marketing ethics refer to “the systematic inquiry into the nature and grounds of standards, moral judgments, and rules of conduct focusing on marketing decisions, behaviours and institutions” (Eastman et al., Citation1996, p. 952). Ethics is an Aristotelian moral philosophical tradition for judging the rightness not of an action per se, but of an action of one person relative to others, based on the evaluation of the personal interactions (Gaski, Citation1999; Román, Citation2003; Thomas et al., Citation2002). Marketers must be subjective on every policy and strategy to test for fairness, and ask not only “is it legal?”, but also “is it right?” (Berry, Citation1995). Instead of measuring what is right or wrong, the research has examined the ethical issues and concerns that occur in marketing and how customers and firms behave when they encounter such issues (Diacon & Ennew, Citation1996).
Bartels (Citation1967) developed the first conceptualisation of the factors affecting marketing ethical decisions. Since then, the research has evolved by reflecting on the increased public concern on unethical marketing activities (i.e. dangerous products, misleading pricing, and deceptive advertising). Ferrell and Gresham (Citation1985) have since incorporated ethical issues such as price, collusions, bid rigging, bribes, falsifying information, and deceptive advertising into a contingency framework for understanding ethical marketing decision-making. The traditional marketing concept uses the 4Ps (e.g., product, price, place, and promotion) to manipulate the mass market (Ferrell & Ferrell, Citation2008). Relative to this, Eastman et al. (Citation1996) have identified the following as areas of ethical concern:
the product (i.e. sell products that lack customer benefits),
price (i.e. charge higher prices to claim superiority over rivals selling similar service),
fairness (i.e. bribery, honesty, misrepresent service benefits), and
confidentiality.
Holcombe (Citation2015) uses the argument that the ethics of marketing cancer by the cancer centres and hospitals aims at the “emotions more than facts” of consumers and it could be misleading and imply a perception that new equipment or new services will improve the outcomes without substantial evidence on such a claim. Latham (Citation2004) believes that the pitfalls in medical marketing ethics (e.g., the nature of the medical product and price, fairness and quality problems, deception, problems with placement, lack of information, and conflicting interests in promotion, agency and access) can be resolved by professionalism as the fifth P in the medical marketing mix. Thus, marketing ethics applied in the medical services must encompass all the extended services in the marketing mix elements (Murphy, Citation2002). Marketing ethics assumes more relevance and complexity in the services marketing context where the ethical behaviour of marketers is essential to the realization of marketing effectiveness and satisfaction (Singhapakdi et al., Citation1996).
Given the increased frequency of their boundary spanning contacts (Nantel & Weeks, Citation1996), the contact staff is a suitable example for ethical abuse linked to the activities of the marketing department (Ferrell & Gresham, Citation1985). These activities often include products and customer situations without a proper set of guidelines (Donoho et al., Citation2013). Examples would include when they exaggerate or lie about the benefits, or communicate misleading information, use manipulative tactics, and high-pressure selling techniques (Román, Citation2003). Previous studies (Chonko et al., Citation1996; Thomas et al., Citation2002) indicate that the perceived high ethics of salespeople has declined, and consumers have a negative perception of salespeople as they perceive them to have low ethical standards (i.e. false promises or coercion into a purchase).
Unethical sales behaviour, as perceived by consumers, is defined as the short-term salesperson’s conduct to generate a sale at the expense of customers and has a profound impact on the public image about the firm (Pezhman et al., Citation2013). Consumers’ have subjective beliefs and their source of unethical behaviour may distort their buying behaviour (Brunk, Citation2010). The perceived vicarious or personal, unethical marketing behaviours that relate negatively to the customers’ expectations (Creyer & Ross, Citation1997) are:
attitude (Babin et al., Citation1999);
satisfaction (Alexander, Citation2002); and
Behavioural Intention (Creyer & Ross, Citation1997).
Thus, the ethical behaviour of salespeople positively affects Customer Satisfaction (Mulki & Jaramillo, Citation2011; Pezhman et al., Citation2013; Thomas et al., Citation2002). Consequently, when the overall Customer Satisfaction is negative, the perceived marketing ethics of a firm will be affected negatively by the overall dissatisfaction (Chonko et al., Citation1996; Thomas et al., Citation2002). “In a real world, consciously dissatisfying customers contradicts with the definition of marketing” (Gaski, Citation1999, p. 319). This study, therefore, hypothesises that:
H6: Low Customer Satisfaction has a negative impact on perceived marketing ethics.
3. Research methodology
3.1. Measures
A quantitative research study (Malhotra, Citation2007), was conducted by using structured self-administered questionnaires used to measure Economic Risk Cost (six-items), Evaluation Cost (four-items), Benefit Loss Cost (three-items), Monetary Loss Cost (three-items), Personal Relationship Loss Costs (four-items), and Customer Satisfaction (four-items). Section A captured the demographic data involving age, gender, medical scheme affiliations, monthly contribution, number of covered households, customer switching experience, and the length of membership. Section B comprised validated scale-items sourced from the typology of switching costs developed by Burnham et al. (Citation2003), to the Ethical Marketing Issues (nine-items) scale (sourced from Murphy et al., Citation1992) to measure the marketing ethics in this study.
All the 33 scale-items formed statements suitable for collecting primary data needed to answer the research questions and achieve the objectives of this study. Responses were measured using a five-point Likert-scale varied from strongly disagree (1) to strongly agree (5). The questionnaire was pre-tested on a sample (n = 50) with similar traits to the initial sample to eliminate survey and measurement errors, thus, improving the overall quality of the survey.
3.2. Sampling and data collection
A cross-sectional study (Malhotra, Citation2007), collected data only once from a targeted population of medical scheme clients ranging between 18 to 60 years of age, who resided in South Africa, Gauteng Province. In 2016, the population of South Africa was estimated at 55.91 million, with the highest proportion (24%) or 13.5 million people residing in Gauteng Province (A. Gray & Vawda, Citation2017) and therefore, the largest proportion of medical scheme beneficiaries reside in Gauteng province (40%). While the proportion of medical scheme membership has declined in other provinces, Gauteng has recorded an increase of 1.4% (Council for Medical Schemes Annual Report, Citation2017–2018).
A non-probability judgment sampling method (Hair et al., Citation2017) ensured the inclusion of (n = 250) beneficiaries directly paying monthly contributions, whose medical scheme memberships exceeded 6 months. This sample size corresponds with prior similar studies (Edward & Sahadev, Citation2011; Li, Citation2015; Ngo & Pavelková, Citation2017).
In May 2019, primary data were collected using a face-to-face survey over a period of a month, in the public locations near the public and private healthcare facilities by a team of skilled fieldworkers. Each respondent self-administered a structured questionnaire written in English language, which captured objective responses about perceived switching costs, satisfaction and perceived marketing ethics of medical schemes. The ethical conduct of the researcher and ethical treatment of the participants in the study, (i.e. consent, debrief the respondents about the study purpose, rights to refuse or to withdraw from participation, assure them about disclosed data privacy, data storage safety and thank them for their participation) were addressed.
The University of Johannesburg, College of Business and Economics (CBE) Ethical Committee issued the Ethical Clearance Certificate.
4. Analysis and findings
4.1. Descriptive statistics
A total of 208 completed questionnaires were returned, yielding 83.2% response rate, which was processed (i.e. coded, edited, tabulated) into SPSS Version 26 for multivariate statistical analysis, and AMOS Version 26 tested the latent variables with their causal structure using a structural equation modelling (SEM). The descriptive statistics of the sample profiles shown in Table indicate that most respondents (24.0%) had 25–29 years of age. Many subjects were females (53.4%) and 40.4% of respondents contribute up to R3 000 per month. Many subjects (41.8%) have been members of their medical schemes for more than a period of 5 years, and most respondents (65.9%) indicated that they have not switched before. The majority of the respondents are members of the Discovery Health Medical Scheme (55.3%), followed by BankMed (20.2%), Momentum (11.1%), and Bonitas (4.8%). Table presented below is useful for understanding the economic and socio-demographics of the target sample in this study.
Table 1. Descriptive profiles of sample
4.2. Exploratory factor analysis (EFA)
In EFA, the Bartlett’s Test of Sphericity (Bartlett, Citation1954) and the Kaiser-Meyer-Olkin (KMO) measure of sampling adequacy (Kaiser, Citation1960), determine the number of variables capturing the underlying relationships of the factors (Pallant, Citation2010). Table below shows that the model with Kaiser-Meyer-Olkin Measure of Sampling Adequacy =.815; Bartlett’s Test of Sphericity, approximately Chi-Square = 3914.174; df = 528, is significant p < .000, and explained 72.39% of the total variance.
Table 2. Item loading and factor analysis
The varimax rotation, as the traditional orthogonal approach, was used to minimise the number of variables with high loadings on each factor (Pallant, Citation2010), and determine the suitability of all 33-item scale in the context of medical schemes in South Africa. Ethical Marketing Issues had one item (EMI1 = .531) that cross-load with two items (ERC1 = .828; ERC2 = .688) of Economics Risk Costs. Ethical Marketing Issues also had two items (EMI5 = −.698 and EMI9 = .497) that cross-load with one item (SAT2 = .578) of Customer Satisfaction. These cross-loading items were deleted. The remaining items loaded above 0.50 on their expected factors, showing good reliability (Hair et al., Citation1998). The eight iterations rotation procedure for refinement of the measurement scale explored the 27 scale-items that tested the split-half reliability of the factors using Cronbach alpha (Cronbach, Citation1951), with coefficients recommended above 0.7 (Malhotra, Citation2007), and closer to 1 representing a greater internal consistency reliability (Pallant, Citation2010).
A check for assumptions shows that multicollinearity (r = .9 and above) does not exist in this study as the independent factors are not highly correlated, and Tolerance Value is greater than .10 and Variance inflation factor (VIF) value is less than 10, indicating no sign of multicollinearity (Pallant, Citation2010). Table below shows descriptive statistics of the constructs. Six-items of Ethical Marketing Issues had alpha of .872 (M = 2.0507; St. Dev = .72563). Four items of Personal Relation Loss Costs had alpha of .921 (M = 2.6454; St. Dev = 1.16830). Four-items of Evaluation Costs had alpha of .8663 (M = 3.5120; St. Dev = 1.06910). Four-items of Economic Risk Costs had alpha of .830 (M = 3.2917; St. Dev = .94473). Three-items of Benefit Loss Costs had alpha of .912 (M = 3.5449; St. Dev = 1.29291). Three-items of Monetary Loss Costs had alpha of .857 (M = 3.2821; St. Dev = 1.05792), and three-items of Customer Satisfaction had alpha of .792 (M = 3.3471; St. Dev = .72181). The negative skewness values ranging from Economic Risk Costs (−.323), Monetary Loss Costs (−.437), Customer Satisfaction (−.514), Benefit Loss Costs (−.588), and Evaluation Costs (−.608) show that the values cluster at the upper right-hand side of the standard normal distribution. The positive kurtosis values for Marketing Ethics (1.381) and Customer Satisfaction (.899) show the peaked distribution (i.e. clustered in the centre), and kurtosis value for Customer Satisfaction (.899), below zero shows a distribution curve that is relatively flat with many extreme cases in the data. This can be corrected by increasing “sample size to exceed 200+ cases” (Pallant, Citation2010, p. 57).
Table 3. Descriptive statistics of the constructs
4.3. Confirmatory factor analysis (CFA)
A CFA (Anderson & Gerbing, Citation1988), tested the reliability of the measurement model using Cronbach alpha (Cronbach, Citation1951), Composite reliability (Fornell & Larcker, Citation1981), and Average Variance Extracted (Fornell & Larcker, Citation1981) to confirm the discriminant validity (Fornell & Larcker, Citation1981) of the interactions between the seven factors extracted in EFA.
A maximum likelihood estimation tested the covariance matrix in AMOS Version 26 to identify the estimates of various parameters (Jöreskog et al., Citation1999). Data had no missing values. The factor loading of the items in the constructs verified the convergent validity (see Figure below), with values above 0.5 showing a positive correlation among the scale-items of each factor (Pallant, Citation2010). The size of the correlation coefficients for EMI7 = .64 below (>.70) was deleted (Low λ). Subsequently, EMI8 = .69 below (>.70) was also deleted (Low λ). Satisfaction had only three items, therefore, SAT1 = .69 below (>.70) was not deleted. The smaller correlations may be accepted, but as a general rule of thumb, the size of the correlation coefficient must be .70 and above (Hair et al., Citation2017). The measurement model with one covariance added between PRLC3 <-> PRLC4, which improved the measurement model with .38 (see Figure ), showed good fit indices as recommended by Schreiber et al. (Citation2006). With Chi-square = 373.019; degrees of freedom (df) = 230, the measurement model is significant at p < .000, with satisfactory (CMIN/DF = 373.019/230 = 1.622, Goodness-of-fit index (GFI) = .877, Adjusted GFI (AGFI) = .840, Comparative Fit Index (CFI) = .950, Tucker–Lewis index (TLI) = .940, Incremental Fit Index (IFI) = .951, Normed Fit Index (NFI) = .881, Standardized Root Mean Square Residual (RMR) = .084, and Root Mean Square Error of Approximation (RMSEA) = .055.
Figure 2. Measurement model.
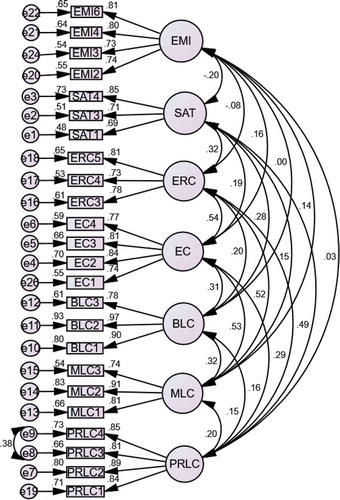
The Measurement Model tested the possibility existence of outliers or negative error variances (also known as Heywood cases) and the standardised factor loadings above 1.0 or below −1.0 (Hair et al., Citation1998). The residual covariance of −2.779 between BLC1 and ERC4 represents standard error, and all the other standardised residuals had values less than two, showing appropriateness of the measurement model (Jöreskog et al., Citation1999). Table below shows the standardised regression weights of CFA.
Table 4. Standardised regression weights (CFA)
Table below shows that the AVE is greater than shared variance with other variables as recommended by Fornell and Larcker (Citation1981). All the AVE values were above (>0.50), supporting convergent reliability (Fornell & Larcker, Citation1981), and composite reliability (CR) values were all above (>0.70) verifying discriminant validity of the measurement model (Fornell & Larcker, Citation1981). The values of the square root of the AVE (bold values on Table ) are greater than the correlation coefficients, which allow for continuation of the structural model testing.
Table 5. Discriminant validity of the constructs
4.4. Structural model
The structural model in Figure , tested the path estimates and overall model fit, wherein it was hypothesised that Economic Risk Costs (H1) and Evaluation Costs (H2) have direct negative significant effects on Satisfaction, while Benefit Loss Costs (H3), Monetary Loss Costs (H4), and Personal Relational Loss Costs (H5) have direct positive significant effects on Satisfaction. Lower Satisfaction levels (H6) will negatively affect perceived Marketing Ethics of medical schemes.
Figure 3. Structural equation modelling (SEM).
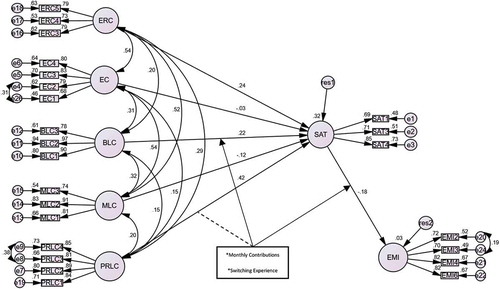
The structural model in Figure with one covariance added between PRLC3 <-> PRLC4 (to enhance the structural model with .38); another one added between EC1 <-> EC2 (to improve the structural model with .31); and the last one added between EMI2 <-> EMI3 (to improve the structural model with .19); showed good fit indices as recommended by Schreiber et al. (Citation2006). With Chi-square = 370.934; degrees of freedom (df) = 233, the structural model is significant at p < .000, with satisfactory CMIN/DF = 370.934/233 = 1.592, Goodness-of-fit index (GFI) = .877, Adjusted GFI (AGFI) = .841, Comparative Fit Index (CFI) = .952, Tucker–Lewis index (TLI) = .943, Incremental Fit Index (IFI) = .953, Normed Fit Index (NFI) = .882, Standardised Root Mean Square Residual (RMR) = .098), and Root Mean Square Error of Approximation (RMSEA) = .053.
Table shows that Economic Risk Costs had positive significant effect on Customer Satisfaction (.236; p < .025), and Evaluation Costs had negative insignificant effect on Customer Satisfaction (−.034; p < .736). Benefit Loss Costs had positive significant effect on Customer Satisfaction (.221; p < .004) and Monetary Loss Costs had negative insignificant effect on Customer Satisfaction (−.117; p < .232). H1, H2, and H4 were rejected. Personal Relational Loss Costs had positive significant effect on Customer Satisfaction (.416; p < .001). Lastly, lower Satisfaction levels had negative significant impact on perceived Ethical Marketing Issues of medical schemes (−.184; p < .028). Therefore, H3, H5 and H6 were accepted.
Table 6. Structural path results
Figure above, also shows the squared multiple correlation (SMC) coefficients. Satisfaction had 0.32, which suggests that 32% of the variance in Customer Satisfaction is explained by customers’ perceptions of personal relationship loss costs and benefit loss costs. Marketing ethics had 0.3, which suggests that 3% of the variance in customers’ perception of ethical marketing is explained by overall satisfaction of customers with the medical scheme services.
4.5. Moderation
The study tested moderation effects of medical scheme contributions and customer switching experience on the effects of personal relational loss costs and benefit loss costs on Customer Satisfaction, and on satisfaction effects on the perceived marketing ethics, using the Johnson Neyman’s regression technique.
4.5.1. Medical scheme contributions
When the South African government delivers the NHI fund through tax funding, rather than via health insurance contributions, the entitlement to use health services will not be directly tied to contributions (A. Gray & Vawda, Citation2017, Citation2019). Currently, many income taxpayers belong to medical scheme and face the contributions that account for a large percentage of their income (A. Gray & Vawda, Citation2019). Many South Africans earn below R6 000 per month per household, and those with income levels above R15 000 per month are subsidised for the medical scheme cover. This means people earning above the threshold (Erasmus et al., Citation2016). Recently, estimates show that medical scheme contributions in South Africa are regressive across the members from different socio-economic groups. Monthly contributions range from 15.8% of income before tax credits (and 9.2% after tax credits) for the lowest income medical scheme members to 5.5% before and 4.7% after tax credits for the highest income scheme members (A. Gray & Vawda, Citation2019). As the medical scheme contribution is still a service condition imposed by employers (Erasmus et al., Citation2016), this, therefore, necessitates the investigation of the following hypotheses:
H7: Medical scheme contributions moderate the relationship between personal relational loss costs and Customer Satisfaction.
H8: Medical scheme contributions moderate the relationship between benefit loss costs and Customer Satisfaction.
H9: Medical scheme contributions moderate the relationship between Customer Satisfaction and marketing ethics.
Table below shows that the results of the interaction effect (γ = .1354; t-value = 2.1686) of medical scheme contributions on the relationship between Benefit Loss Costs and Customer Satisfaction (LLCI = .0123; ULCI = .2585), is significant at p < .0313. H8 is accepted while H7 and H9 were rejected. Knowledge is required on the conditions under which this moderation effect is significant (i.e. is it when medical scheme contributions are either low, medium, or high?). Table shows that the moderation effect under the condition of low contributions (LLCI = −.1246; ULCI = .1535), is not significant, p < 0.8382. The moderation effect under the condition of medium contributions (LLCI = .0488; ULCI = .2469), is significant at p < .0036. The moderation effect under the condition of high contributions (LLCI = .1131; ULCI = .4854), is highly significant at p < .0018.
Table 7. Conditional effect of benefit loss costs on satisfaction at values of the moderator(s)
Figure below shows that the development of satisfaction is important for customers paying medium monthly contributions and it is even important for those paying high monthly contributions. The difference is that an increase in benefit loss costs does not increase Customer Satisfaction of customers who pay low contributions, but increasing benefit loss costs enhance satisfaction of customers who make medium contributions, and increasing benefits loss costs strongly enhance the satisfaction of customers who make high contributions per month.
4.5.2. Customer switching experience
Enhancing consumers’ perceived switching costs contribute to the entry barriers, especially if the firm’s products and quality lack transparency to consumers do not provide meaningful and comparative information (Competition Commission, South Africa. H, Citation2018). While consumers who perceive low switching costs, and do not perceive additional value on the service they receive from a medical scheme will switch to competing brokerages; however, many of them are reluctant to switch despite the limited switch barriers imposed by medical schemes on consumers (Competition Commission, South Africa. H, Citation2018). The market complexity is that many consumers have a considerable apathy (i.e. emotions) and consider it serious to switch medical schemes as those who switch lose credit points and are, therefore disincentivised from switching (Competition Commission, South Africa. H, Citation2018). Furthermore, some health professionals have violated the Constitution and other related laws, disregarded their professional code of ethics, and thus have demonstrated disrespect for patients’ rights including their families (A. Gray & Vawda, Citation2018). Such unethical behaviour has a profound effect on the public image about the firm (Pezhman et al., Citation2013). Negative ethical image and socially irresponsible behaviour will repel customers from an organisation and its products (Mulki & Jaramillo, Citation2011), which therefore necessitates the investigation of the following hypotheses:
H10: Customer switching experience moderate the relationship between personal relational loss costs and Customer Satisfaction.
H11: Customer switching experience moderate the relationship between benefit loss costs and Customer Satisfaction.
H12: Customer switching experience moderate the relationship between Customer Satisfaction and perceived marketing ethics.
Table below shows that the results of the interaction effect (γ = .2246; t-value = 2.1197) of customer switching experience on the relationship between benefit loss costs and Customer Satisfaction (LLCI = .0157; ULCI = .4334), is significant at p < .0352. H10 is rejected while H11 and H12 were accepted. Knowledge is required on the conditions under which this moderation effect is significant (i.e. is it when customers have switching experience or do not have switching experience?). Table shows that under the condition where customers do not have switching experience, the moderation effect (LLCI = −.1465; ULCI = .1719) is not significant, p < .8756, but under the condition where customers have switching experience, the moderation effect (LLCI = .1020; ULCI = .3724) is significant at p < .0034.
Table 8. Conditional effect of benefit loss costs on satisfaction at values of the moderator(s)
Figure below shows that the development of Customer Satisfaction is important for customers who have switching experience. The difference is that increasing benefit loss costs does not increase the satisfaction of customers who do not have switching experience, but increased Benefit Loss Costs enhance the satisfaction of customers with prior switching experience.
Figure 5. The moderating effect of customer switching experience on the link between benefit loss costs and Customer Satisfaction.
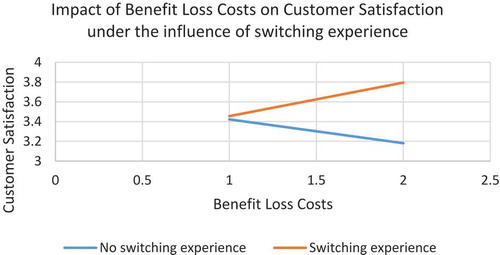
Table below shows that the results of the interaction effect (γ = .2900; t-value = 2.6278) of customer switching experience on the influence of Customer Satisfaction on perceived marketing ethics (LLCI = .0724; ULCI = .5075) is significant at p < .0092. Therefore, H11 is accepted. Knowledge is required on the conditions under which this moderation effect is significant (i.e. is it when customers have switching experience or do not have switching experience?). Table shows that under the condition where customers do not have switching experience, the moderation effect (LLCI = −.4732; ULCI = .1505), is significant, p < .0002, but under the condition where customers have switching experience, the moderation effect (LLCI = −.1679; ULCI = .1241), is not significant at p < .7679.
Table 9. Conditional effect of satisfaction on marketing ethics at values of the moderator(s)
Figure below shows that the development of perceived ethical marketing is important for customers who do not have switching experience. The difference is that an increase in Customer Satisfaction enhances perceptions of marketing ethics for customers who do not have switching experience; however, increased satisfaction for customers who have switching experience does not enhance their perceived marketing ethics of medical schemes.
5. Discussion and conclusion
This study provides insights regarding the management of perceived switching costs on Customer Satisfaction, and the effect on perceived marketing ethics of medical schemes in the South African healthcare sector. The study has profiled a large segment (24.0%) of consumers ranging between the ages of 25 to 29 years old, the majority of whom are female consumers (53.4%). Many customers (55.3%) identify with the Discovery Health Medical Scheme, and about 40.4% contribute over R3 000 per month. The large membership (41.8%) exceeds a period of 5 years, and 65.9% of the consumers report having no switching experience.
This study finds that economic risk costs positively impact Customer Satisfaction, which was an unintended outcome. This result, therefore, supports the findings by Blut et al. (Citation2014) who reported that procedural switching costs positively relate with important relationship outcome of satisfaction.
It appears, therefore, that customers do not view themselves as “being locked-in” to the medical scheme. Instead, customers perceive switching costs may attribute the view of “being locked-in” to their own inability state to switch, as indicated by Burnham et al. (Citation2003). This study, therefore, does not find evidence supporting the direct negative impact of economic risk costs and evaluation costs on Customer Satisfaction, therefore, support the findings by Burnham et al. (Citation2003) who also did not find this evidence. By contrast, M.A. Jones et al. (Citation2000) used a holistic measure of switching costs and observed supportive evidence showing the negative interaction effect.
The findings, therefore, show that Benefit Loss Costs have a positive significant effect on Customer Satisfaction. This result supports the findings by M.A. Jones et al. (Citation2007). Monetary loss costs do not have significant effect on Customer Satisfaction in this study, and as Moliner (Citation2009) reports, monetary costs and service quality are fundamental factors for a private healthcare satisfaction. Moreover, personal relation loss costs have a positive significant impact on Customer Satisfaction. This result corroborates with the literature, (Julander & Söderlund, Citation2003; Meng & Elliott, Citation2009), showing the impact of positive switching costs (social and lost benefits) on Customer Satisfaction. Lower satisfaction levels were found to affect perceived marketing ethics of medical schemes negatively, which confirms the results by Chonko et al. (Citation1996) and Thomas et al. (Citation2002).
The moderation effects of both medical scheme contributions and customer switching experience, as control variables on the interaction of personal relational loss costs and Customer Satisfaction were not supported. However, evidence shows that these control variables moderate interaction of Benefit Loss Costs and Customer Satisfaction. Results also show that increasing Benefit Loss Costs enhance satisfaction of customers who contribute high and medium monthly fees and for consumers with switching experience. The moderation of medical scheme contributions, as control variables on the negative interaction of Customer Satisfaction and perceived marketing ethics, was not supported. The findings support the moderation effect of consumers switching experience on the negative interaction of Customer Satisfaction and perceived marketing ethics. Increasing satisfaction of customers who have no switching experience enhances their perceived marketing ethics of medical schemes.
5.1. Theoretical contribution
This paper contributes insights to the body of knowledge embracing the enlightened marketing philosophy intended to enhance the long-term performance of the marketing system of the medical schemes. This study also contributes to the literature on services marketing in various ways. It has tested the structural model that uncovered insights on:
the effectiveness of switching cost typology developed by Burnham et al. (Citation2003) which classified switching costs by type (procedural, financial, and relational) and direction (positive and negative);
Customer Satisfaction (R.L. Oliver, Citation1997); and on
the resultant impact on perceived marketing ethics (Murphy et al., Citation1992) of medical schemes.
This approach is useful for various reasons. Firstly, Burnham et al. (Citation2003) recommend the research on the relationship between switching costs and satisfaction to examine whether, or when, switching costs lead to customer dissatisfaction. Secondly, it clears the empirical evidence shown in the literature regarding the overall effects of perceived switching costs on Customer Satisfaction (Biedenbach et al., Citation2015; Chang & Chen, Citation2008; Sanjeepan, Citation2017). Thirdly, results confirm the direct positive impact of switching costs (Personal Relationship Loss Costs and Benefit Loss Costs) on Customer Satisfaction (Julander & Söderlund, Citation2003; Meng & Elliott, Citation2009). Lastly, the study confirms that lower satisfaction contributes negatively to perceived ethical marketing activities, which supports the results by Thomas et al. (Citation2002).
This study has uncovered knowledge regarding the moderation effects of the medical scheme contributions and customer switching experience on Benefit Loss Costs and Customer Satisfaction. Increasing Benefits Loss Costs impact satisfaction under conditions where members contribute high and medium monthly fees and when customers have switching experience. Clearly, consumers who do not have switching experience perceive a negative interaction of satisfaction and marketing ethics. In general, this research study recommends the service firms to view switching costs as an ethical problem instead of one of the economic costs incurred in switching a firm. This view, therefore, embraces Distributive Justice as an ethics precept necessary to understand enlightened marketing ethics (Ferrell & Ferrell, Citation2008).
5.2. Managerial implications
The medical scheme industry in Southern Africa should constantly monitor and evaluate strategies and adapt swiftly to the rapidly changing needs of the emerging market. As a practical recommendation in this study, it is advisable for managers of the medical schemes in South Africa to coordinate a strategy of increasing Customer Satisfaction and switching costs. To improve Customer Satisfaction, managers must also closely monitor and increase Personal Relations Loss costs and Benefit Loss Costs by increasing additional services, rewards, discounts, special deals, or savings, among others. By increasing the Benefits Loss Costs, managers will satisfy members who contribute high and medium monthly fees and those with switching experience. Increasing service benefits lead to lower perceived costs, and managers can improve service benefits and raise costs with an ethical approach (i.e. assume the responsibility to improve customer value).
Julien Le Grand, LSE economist, states that in the choice and competition model, customers choose between services offered by competing providers, whereas in the voice model, customers express satisfaction (or dissatisfaction) through complaints directly to a service provider, or a higher manager or an elected representative (Groenewoud et al., Citation2019). Resolving customers’ complaints is considered the proper means to avoid customer dissatisfaction, which in the normative paradigm of the marketing concept, is a strategy that resonates strongly with the marketers’ self-interests (Gaski, Citation1999). Managers should monitor the evolution of satisfaction among customers and avoid situations that could lead to dissatisfaction.
From enlightened marketing perspective, realizing marketing ethics, societal marketing, customer value, and suchlike factors can enhance Customer Satisfaction. Lower satisfaction levels predict perceived unethical marketing practices by medical schemes; hence, managers must set a higher standard of professionalism and ethical behaviour, and control inappropriate selling through an intensive training of their salesforce and via newly appointed salesmen. The recruitment of qualified salesmen and their subsequent training is crucial.
Enlightened marketing; ▪ innovative marketing; requires organizations to continuously seek new and better ways of improving its products and services to avoid losing customers (Kotler & Armstrong, 2008). The medical scheme practitioners in South Africa should develop marketing strategies linked to the National Patients’ Rights Charter developed by the Department of Health, which promotes the entitlement of members to information about their medical scheme and to challenge, where necessary, the decisions of such a medical scheme (Health Professions Council of South Africa, Citation2016).
Contact staff should do more to help customers make wise and informed decisions, and provide relevant information in a range of languages, instead of coercing them to purchase. Clearly, the medical schemes can position themselves as ethical brands in the market by endorsing features of quality, integrity respect, honesty, diversity responsibility, and accountability. Enlightened marketing; ▪ sense-of-mission marketing; advocates for an organization to define its mission in broad social terms to serve best interests of both the consumers and the brand in the long-run (Kotler & Armstrong, 2008).
Marketing practitioners in healthcare must ensure fair and balanced promotion of health services, and avoid exaggerating claims in the context of reputable marketing. Oh and Yoon (Citation2014) recommend that ethical businesses adopt new marketing tactics reflecting ethical principles to reinforce the consumers’ belief in ethical consumerism (e.g., using promotions to demonstrate ethical obligations). Thus, in healthcare, a Consumerist Model may view patients as consumers, whereas in the Socialist Model of the NHI, patients are viewed as beneficiaries or as entitled “users”—the term used in the National Health Act (No 61 of 2003) (Rowe & Moodley, Citation2013). This study highlights the potential introduction of the NHI in South Africa to directly improve satisfaction with health service and not only reduce the role of medical schemes but also to propel them to promote the prevention of unethical marketing practices. The NHI will make a provision for the measurement of patient satisfaction, the results of which (according to the NHI White Paper, as amended), will help the Office of Health Standards Compliance (OHSC) to identify gaps and put corrective measures necessary to sustain patient satisfaction (Competition Commission, South Africa. H, Citation2018). In developed nations like the UK, the beneficiaries to private medical schemes were found to be less satisfied with the NHS than non-beneficiaries, and most had enrolled as a condition of employer (Crow et al., Citation2002).
A clarity is required on the misunderstanding of the natural features of the proposed NHI reforms. In particular, the misconception regarding expansion of medical scheme coverage to all South Africans (A. Gray & Vawda, Citation2019). It is important for health practitioners in South Africa to realize that even with a fully operational NHI, the supplementary health insurance products will still have to be regulated (French, Citation2012), because “if the burden of cost containment is incurred by consumers who already have limited healthcare access, then the quality of healthcare will erode” (Furrow, Citation1988, p. 188). Consequently, what is likely to be an area of contestation is the idea of consumers duplicating cover (i.e. by contributions to NHI and ongoing purchase of private cover) (Erasmus et al., Citation2016).
The NHI fund faces hurdles before it can fulfil the role of private healthcare funding in South Africa. As a potential solution, the Government must accept the critical role of and collaborate with the private healthcare sector in facilitating NHI. This requires the private sector to be prepared and willing to render health services beyond the boundaries of medical scheme target market; to assist the government in serving higher volumes of patients from the public sector, and people who cannot afford monthly contributions; and to charge more affordable prices (A. Gray & Vawda, Citation2019). Thus, through regular meetings and follow-up, involvement, and extensive consultations will be necessary via the Quality Standards (QS) development process to ensure commitment and buy-in at appropriate levels (A. Gray & Vawda, Citation2019). Clearly, the first step in the implementation of the NHI reforms will necessitate the amendments to the Medical Schemes Act (131 of 1998) (A. Gray & Vawda, Citation2017).
6. Limitations and future research directions
The limitations of external validity (e.g., generalising the findings to the broader population) can be corrected by including the medical scheme beneficiaries in other provinces of the country. The measurement error and scale improvements can include the eight facets of switching costs proposed in the literature. Qualitative method can be adopted to gain more insights on the daily personal and sensitive ethical issues facing members of medical schemes in South Africa.
A further point of investigation includes the consumers’ perceived value and concerns in relation to higher hospital and related increasing costs that make the medical scheme membership to be viewed as highly expensive and less accessible. Investigations should expand on the issue of marketing ethics in the various services contexts with strong competition, high, and low switching costs (e.g., telecommunication, banking, insurance, etc.). Research views the effect of switching costs as a “lock-in” strategy (Nie et al., Citation2018). Increasing switching costs by the affective dimension can avoid negative word-of-mouth by customers generated in a “lock-in” situation. Future research can examine the possibility of increasing switching costs via anti-lock mechanisms to increase satisfaction. Interestingly, the nature of satisfaction–loyalty interaction moderated by switching costs in the medical scheme sector can be examined, as satisfaction alone is insufficient to create loyal customers. In health services, Customer Satisfaction rates alone cannot be considered as evidence of high-quality care (Jacobsen & Hasumi, Citation2014).
Additional information
Funding
Notes on contributors
Thabang Excellent Mofokeng
Thabang Excellent Mofokeng completed Baccalaureus Technologiae Degree in Marketing Management, and Master’s Degree in Marketing Management, both from Vaal University of Technology, and his PhD in Marketing Management from North West University, South Africa. He completed the Post-graduate Diploma in Higher Education from the University of Johannesburg, South Africa. He has been working in academia for the last 10 years. Moreover, he has been teaching at Undergraduate and Graduate programs at the University of Johannesburg for the last 3 years. He has also been working as a BCom Marketing Program coordinator and as lecturer in Marketing Management at the Department of Marketing, School of Consumer Intelligence and Information Systems, College of Business and Economics, University of Johannesburg, South Africa. His research interests include services marketing, e-commerce marketing, retail marketing, and consumer behaviour. He is an emerging researcher aiming to publish research articles in both national and international journals.
References
- African National Congress. (1994). The national health plan for South Africa. ANC. www.anc.org.za/ancdocs/policy/health.htm
- Alexander, E. C. (2002). Consumer reactions to unethical service recovery. Journal of Business Ethics, 36(3), 223–35. https://doi.org/10.1023/A:1014086327876
- American Marketing Association. (2005). Statement of ethics. Spring, 2005. https://archiveama.org/archive/aboutAMA/pages/statement%20of%20Ethics.aspx
- Anderson, J. C., & Gerbing, D. W. (1988). Structural equation modeling in practice: A review and recommended two-step approach. Psychological Bulletin, 103(3), 411–423. https://doi.org/10.1037/0033-2909.103.3.411
- Annas, G. J. (2003, February). The right to health and the Nevirapine case in South Africa. The New England Journal of Medicine, 348(8), 750–754. https://doi.org/10.1056/NEJMlim022737
- Axtell-Thompson, L. M. (2005). Consumer directed health care: Ethical limits to choice and responsibility. Journal of Medicine and Philosophy, 30(2), 207–226. https://doi.org/10.1080/03605310590926867
- Aydin, S., & Özer, G. (2005). The analysis of antecedents of customer loyalty in the Turkish mobile telecommunication market. European Journal of Marketing, 39(7/8), 910–925. https://doi.org/10.1108/03090560510601833
- Aydin, S., Ozer, G., & Arasil, O. (2005). Customer loyalty and the effect of switching costs as a moderator variable: A case in the Turkish mobile phone market. Marketing Intelligence & Planning, 23(1), 89–103. https://doi.org/10.1108/02634500510577492
- Ayo-Yusuf, I. O., Ayo-Yusuf, I. J., & Matjila, S. A. (2016). The role of socio-economic position on satisfaction with oral health services among South African adults: A structural equation model. SADJ, 10(71), 442–446.
- Babin, B. J., Boles, J. S., & Griffin, M. (1999, 10). Buyer-seller interactions: The role of ethical perceptions on customer attitudes and intentions. American Marketing Association. Conference Proceedings, suppl. 1999 AMA Winter Educators’ Conference: Marketing Theory: Chicago, 270.
- Balabanis, G., Reynolds, N., & Simintiras, A. (2006). Bases of e-store loyalty: Perceived switching barriers and satisfaction. Journal of Business Research, 59(2), 214–224. https://doi.org/10.1016/j.jbusres.2005.06.001
- Barroso, C., & Picón, A. (2012). Multi-dimensional analysis of perceived switching costs. Industrial Marketing Management, 41(3), 531–543. https://doi.org/10.1016/j.indmarman.2011.06.020
- Bartels, R. (1967). A model for ethics in marketing. Journal of Marketing, 20-26(January), 1967.
- Bartlett, M. S. (1954). Significance test for sphericity of a normal n-variate distribution. Journal of the Royal Statistical Society, 16, 296–298.
- Berry, L. L. (1995). Relationship marketing of services – Growing interests, emerging perspectives. Journal of the Academy of Marketing Science, 23(4), 236–245. https://doi.org/10.1177/009207039502300402
- Bhattacharya, A. (2013, September). Switching costs and sustained competitive advantage. International Journal of Business and Management Invention, 2(9), 101–111.
- Biedenbach, G., Bengtsson, M., & Marell, A. (2015). Brand equity, satisfaction, and switching costs: An examination of effects in the business-to-business setting. Marketing Intelligence & Planning, 33(2), 164–178. https://doi.org/10.1108/MIP-03-2014-0059
- Blut, M., Beatty, S. E., Evanschitzky, H., & Brock, C. (2014). The impact of service characteristics on the switching costs-customer loyalty link. Journal of Retailing, 90(2), 275–290. https://doi.org/10.1016/j.jretai.2014.04.003
- Blut, M., Frennea, C. M., Mittal, V., & Mothersbaugh, D. L. (2015). How procedural, financial and relational switching costs affect customer satisfaction, repurchase intentions, and repurchase behavior: A meta-analysis. International Journal of Research in Marketing, 32(2), 226–229. https://doi.org/10.1016/j.ijresmar.2015.01.001
- Bolton, R. N. (1998). A dynamic model of the duration of the customer’s relationship with a continuous service provider: The role of satisfaction. Marketing Science, 17(1), 45–65. https://doi.org/10.1287/mksc.17.1.45
- British Medical Association. (2017). The ethical implications of the use of market-type mechanisms in the delivery of NHS care. A discussion paper from the BMA’s Medical Ethics Committee. B MA 20170240.
- Brunk, K. H. (2010). Exploring origins of ethical company/brand perceptions: A consumer perspective of corporate ethics. Journal of Business Research, 63(3), 255–26. https://doi.org/10.1016/j.jbusres.2009.03.011
- Burnham, T. A., Frels, J. K., & Mahajan, V. (2003). Consumer switching costs: A typology, antecedents, and consequences. Journal of the Academy of Marketing Science, 31(2), 109–126. https://doi.org/10.1177/0092070302250897
- Cătoiu, I., Geangu, I. P., & Gârdan, D. A. (2013). Applying marketing principles in the field of medical services an ethical challenge? International Economic Conference of Sibiu 2013 Post Crisis Economy: Challenges and Opportunities, IECS 2013. Procedia Economics and Finance, 6, 449–456. https://doi.org/10.1016/S2212-5671(13)00162-7
- Chang, C., Chen, S. & Lang, Y. (2013). Service quality, trust, and patient satisfaction in interpersonal-based medical service encounters. BMC Health Services Research, 13(22), 1–11 doi:10.1186/1472-6963-13-22
- Chang, H. H., & Chen, S. W. (2008). The impact of customer interface quality, satisfaction and switching costs on e-loyalty: Internet experience as a moderator. Computers in Human Behavior, 24(6), 2927–2944. https://doi.org/10.1016/j.chb.2008.04.014
- Chonko, L. B., Tanner, J. F., Jr., & Weeks, W. A. (1996). Ethics in salesperson decision making: A synthesis of research approaches and an extension of the scenario method. Journal of Personal Selling & Sales Management, 16(1), 35–52. https://search.proquest.com/docview/216748956?acountid=13425
- Competition Commission, South Africa. H. (2018). Health Market Inquiry Provisional funding and recommendations report.
- Cosma, S. A., Bota, M., Fleseriu, C., Morgovan, C., Valeanu, M., & Cosma, D. (2020). Measuring patients’ perception and satisfaction with the Romanian healthcare system. Sustainability, 12(1 612), 1–16. https://doi.org/10.3390/su12041612
- Council for Medical Schemes Annual Report. (2017 – 2018) . Annual report council for medicals schemes. A healthy industry for all.
- Creyer, E. H., & Ross, W. T., Jr. (1997). The influence of firm behavior on purchase intention: Do consumers really care about business ethics? Journal of Consumer Marketing, 14(6), 421–432. https://doi.org/10.1108/07363769710185999
- Cronbach, L. J. (1951). Coefficient alpha and the internal structure of tests. Psychometrika, 16(3), 297–335. https://doi.org/10.1007/BF02310555
- Crosby, L. A., & Stephens, N. (1987). Effects of relationship marketing on satisfaction, retention, and prices in the life insurance industry. Journal of Marketing Research, 24(4), 404–411. https://doi.org/10.1177/002224378702400408
- Crow, R., Gage, H., Hampson, S., Hart, J., Kimber, A., Storey, L., & Thomas, H. The measurement of satisfaction with healthcare: Implications for practice from a systematic review of the literature. (2002). Health Technology Assessment, 6(32), 1366–5278. https://doi.org/10.3310/hta6320
- Dambisya, Y. M., & Modipa, S. I. & Health Systems Research Group, Department of Pharmacy, University of Limpopo (2008). Capital flows in the health sector in South Africa: Implications for equity and access to health care. EQUINET Discussion Paper Series 76. Rhodes University. York University, TARSC, SEATINI; EQUINET: Harare.
- Diacon, S. R., & Ennew, C. T. (1996). Ethical issues in insurance marketing in the UK. European Journal of Marketing, 30(5), 67–80. https://doi.org/10.1108/03090569610118786
- Dick, A. S., & Basu, K. Customer loyalty: Toward an integrated conceptual framework. (1994). Journal of the Academy of Marketing Science, 22(2), 99–113. Spring, 1994. https://doi.org/10.1177/0092070394222001
- Donoho, C., Herche, J., & Heinze, T. (2013). The personal selling ethics scale: Revised and shortened for time-sensitive professionals. Innovative Marketing, 9(1), 46–56.
- Eastman, K. L., Eastman, J. K., & Eastman, A. D. (1996). The ethics of insurance professionals: Comparison of personal versus professional ethics. Journal of Business Ethics, 15(9), 951–962. https://doi.org/10.1007/BF00705575
- Edward, M., & Sahadev, S. (2011). Role of switching costs in the service quality, perceived value, customer satisfaction and customer retention linkage. Asia Pacific. Journal of Marketing and Logistics, 23(3), 327–345. https://doi.org/10.1108/13555851111143240
- Erasmus, D., Ranchod, S., Abraham, M., Carvounes, A., & Dreyer, K. (2016). Challenges and opportunities for health finance in South Africa: A supply and regulatory perspective. Prepared for FinMark Trust by Insight Actuaries and Consultants, 1-76(April), 2016.
- Ferrell, O. C., & Ferrell, L. (2008, March). A macromarketing ethics framework: Stakeholder orientation and distributive justice. Journal of Macromarketing, 28(1), 24–32. https://doi.org/10.1177/0276146707311290
- Ferrell, O. C., & Gresham, L. G. (1985, Summer). A contingency framework for understanding ethical decision making in marketing. Journal of Marketing, 49(3), 87–96. https://doi.org/10.1177/002224298504900308.
- Fornell, C., & Larcker, D. F. (1981). Evaluating structural equation models with unobservable variables and measurement error. Journal of Marketing Research, 18(1), 39–50. https://doi.org/10.1177/002224378101800104
- Fornell, O. C. (1992, January). A national customer satisfaction barometer: The Swedish experience. Journal of Marketing, 56(1), 6–21. https://doi.org/10.1177/002224299205600103
- French, I. (2012, July). Designing a healthy future. Strategic and emerging issues in the medical scheme industry. First Southern African edition, PricewaterhouseCoopers.
- Furrow, B. R. (1988). The Ethics of cost-containment: Bureaucratic medicine and the doctor as patient-advocate. Notre Dame Journal of Law, Ethics & Public Policy, 3(2), 187–225. http://scholarship.law.nd.edu/ndjlepp/vol3/iss2/3
- Gaski, J. F. (1999). Does marketing ethics really have anything to say? – A critical inventory of the literature. Journal of Business Ethics, 18, 315–334.
- Geyskens, I., Steenkamp, J. E. M., & Kumar, N. (1998). Generalizations about trust in marketing channel relationships using meta-analysis. International Journal of Research in Marketing, 15(3), 223–248. https://doi.org/10.1016/S0167-8116(98)00002-0
- Gounaris, S., & Boukis, A. (2013). The role of employee job satisfaction in strengthening customer repurchase intentions. Journal of Services Marketing, 27/4(4), 322–333. https://doi.org/10.1108/08876041311330799
- Gray, A., & Vawda, Y. (2017). Health policy and legislation. In A. Padarath & P. Barron. (Eds.), South African Health Review 2007 (pp. 1 - 348). Health Systems Trust. http://www.hst.org.za/publications/south-african-health-review-2017
- Gray, A., & Vawda, Y. (2018, November). Health legislation and policy. In L. C. Rispel & A. Padarath (Eds.), South African Health Review 2018 (pp. 1 - 256). Health Systems Trust.
- Gray, A., & Vawda, Y. (2019). Health legislation and policy. In T. Moeti & A. Padarath. (Eds.), South African Health Review 2019 (pp. 1 - 313). Health Systems Trust. http://www.hst.org.za/publications/Pages/SAHR2019
- Groenewoud, A. S., Westert, G. P., & Kremer, J. M. A. (2019). Value based competition in health care’s ethical drawbacks and the need for a values-driven approach. BMC Health Services Research, 19(256), 1–6. https://doi.org/10.1186/s12913-019-4081-6
- Gundlach, G. T., & Murphy, P. E. (1993, October). Ethical and legal foundations of relational marketing exchanges. Journal of Marketing, 57(4), 35–46. https://doi.org/10.1177/002224299305700403
- Hair, J. F., Jr., Celsi, M. W., Otinau, D. J., & Bush, R. P. (2017). Essentials of Marketing Research (4th ed.). McGraw-Hill Irwin.
- Hair, J. F., Tatham, R. L., Anderson, R. E., & Black, W. (1998). Multivariate data analysis with readings (5th ed.). Prentice-Hall.
- Hassmiller, S., & Bilazarian, A. (2018, April). The business, ethics, and quality cases for consumer engagement in nursing. JONA, 48(4), 184–190. https://doi.org/10.1097/NNA.0000000000000597
- Health Professions Council of South Africa. (2016, September). Ethical guidelines for good practice in the health care professions. Protecting the public and guiding the professions. Guidelines for good practice in the health care professions. General ethical guidelines for the health care professions. Booklet 2.
- Hennig-Thurau, T., Gwinner, K. P., & Gremler, D. D. (2002, February). Understanding relationship marketing outcomes: An integration of relational benefits and relationship quality. Journal of Service Research, 4(3), 230–247. https://doi.org/10.1177/1094670502004003006
- Holcombe, R. F. (2015). The ethics of marketing cancer. Journal of Cancer Policy, 3, 1–2. https://doi.org/10.1016/j.jcpo.2014.11.001
- Hunt, S. D. (2010). Marketing theory: Foundations, controversy, strategy, resource-advantage theory. Taylor & Francis. Routledge.
- Hunt, S. D., & Vitell, S. (1986, Spring). A general theory of marketing ethics. Journal of Macromarketing, 5-16, 1986. http://dx.doi.org/10.1177/027614678600600103
- Jacobsen, K. H., & Hasumi, T. (2014). Satisfaction with healthcare services in South Africa: Results of the national 2010 General Household Survey. The Pan African Medical Journal, 18(172), 1–11. https://doi.org/10.11604/pamj.2014.18.172.4084
- Javed, M. K., Degong, M., & Qadeer, T. (2019). Relation between Chinese consumers’ ethical perceptions and purchase intentions: A perspective on ethical company/brand management strategies. Asia Pacific Journal of Marketing and Logistics, 31(3), 670–690. https://doi.org/10.1108/APJML-10-2017-0254
- Jones, M. A., Mothersbaugh, D. L., & Beatty, S. E. (2000). Switching barriers and repurchase intentions in services. Journal of Retailing, 76(2), 259–274. https://doi.org/10.1016/S0022-4359(00)00024-5
- Jones, M. A., Mothersbaugh, D. L., & Beatty, S. E. (2002). Why customers stay: Measuring the underlying dimensions of services switching costs and managing their differential outcomes. Journal of Business Research, 55(6), 441–450. https://doi.org/10.1016/S0148-2963(00)00168-5
- Jones, M. A., Reynolds, K. E., Mothersbaugh, D. L., & Beatty, S. E. (2007). The positive and negative effects of switching costs on relational outcomes. Journal of Service Research, 9(4), 35–44. https://doi.org/10.1177/1094670507299382
- Jöreskog, K. G., Sorbon, D., Du Toit, S., & Du Toit, M. (1999). LISREL 8: New Statistical Features. Scientific Software International.
- Julander, C. R., & Söderlund, M. (2003). Effects of switching barriers on satisfaction, repurchase intentions and attitudinal loyalty. SSE/EFI Working Paper Series in Business Administration.
- Kaiser, H. (1960). The application of electronic computers to factor analysis. Educational and Psychological Measurement, 20(1), 141–151. https://doi.org/10.1177/001316446002000116
- Kaplan, J., & Ranchod, S. (2014-2015). South African Health Review. Analysing the structure and nature of medical scheme benefit design in South Africa. Department of Actuarial Science, School of Management Studies, University of Cape Town.
- Kim, M., Park, M., Lee, D. H., & Park, J. (2019). Determinants of subscriptions to communications service bundles and their effects on customer retention in Korea. Telecommunications Policy, 43(9), 101792. https://doi.org/10.1016/j.telpol.2018.10.005
- Klemperer, P. (1995). Competition when consumers have switching costs: An overview with applications to industrial organization, macroeconomics, and international trade. Review of Economic Studies, 62(4), 515–539. https://doi.org/10.2307/2298075
- Kotler, P., & Armstrong, G. (2008). Principles of marketing. 12th edition. Upper Saddle River, NJ: Pearson Prentice Hall. ISBN-13: 9780132390026
- Kotler, P., & Armstrong, G. (2010). Principles of marketing. Global and Southern African Perspectives. Cape Town. Pearson Education.
- Kotler, P., & Levy, S. L. (1971). Demarketing, yes, demarketing. Harvard Business Review, 49, 71–80.
- Laczniak, G. R. (1999). Distributive justice, Catholic social teaching, and the moral responsibility of marketing. Journal of Public Policy & Marketing, 18(1), 125–129. https://doi.org/10.1177/074391569901800114
- Lam, S. Y., Venkatesh, S., Krishna, E., & Bvsan, M. (2004). Customer value, satisfaction, loyalty, and switching costs: An illustration from a business-to-business service context. Journal of the Academy of Marketing Science, 32(3), 293–311. https://doi.org/10.1177/0092070304263330
- Lamiraud, K. (2013). Switching costs in competitive health insurance markets. ESSEC Working paper. Document de Recherche ESSEC/Centre de recherche de l’ESSEC. 1291-9616. WP 1305. 2013. <hal-00808420>
- Latham, S. R. (2004, September). Ethics in the marketing of medical services. The Mount Senai Journal of Medicine, 71(4), 243–250.
- Li, C. (2015). Switching barriers and customer retention: Why customers dissatisfied with online service recovery remain loyal. Journal of Service Theory and Practice, 25(4), 370–393. https://doi.org/10.1108/JSTP-10-2013-0220
- Malhotra, N. K. (2007). Marketing research: An applied orientation (5th ed.). Pearson Prentice Hall.
- Maphumulo, W. T., & Bhengu, B. R. (2019). Challenges of quality improvement in the healthcare of South Africa post-apartheid: A critical review. Curationis, 42(1), a1901. https://doi.org/10.4102/curationis.v42i1.1901
- Marcos, A. (2018). The role of the positive switching costs in the insurance industry. International Journal of Marketing, Communication and New Media, 6(10), 7–31.
- McIntyre, D. (1995). Financing and expenditure. In D. Harrison & M. Neilson (Eds.), South African Health Review 1995. Health Systems Trust.
- McMurrian, R. C., & Matulich, E. (2016). Building customer value and profitability with business ethics. Journal of Business & Economics Research, 14(3), 83–90. Third Quarter, 2016. http//doi.org/10.19030/jber.v14i3.9748
- Meng, J., & Elliott, K. M. (2009). Investigating structural relationships between service quality, switching costs, and customer satisfaction. Journal of Applied Business and Economics, 9(2), 54–66.
- Mohammed, A., & Rashid, B. (2018). A conceptual model of corporate social responsibility dimensions, brand image, and customer satisfaction in Malaysian hotel industry. Kasetsart Journal of Social Sciences, 39(2), 358–364. https://doi.org/10.1016/j.kjss.2018.04.001
- Moliner, M. A. (2009). Loyalty, perceived value and relationship quality in healthcare services. Journal of Service Management, 20(1), 76–97. https://doi.org/10.1108/09564230910936869
- Mulki, J. P., & Jaramillo, F. (2011). Ethical reputation and value received: Customer perceptions. International Journal of Bank Marketing, 29(5), 358–372. https://doi.org/10.1108/02652321111152891
- Murphy, P. (2002). Marketing ethics at the millennium: Review, reflections, and recommendations. In N. E. Bowie (Ed.), The Blackwell guide to business ethics. Blackwell.
- Murphy, P., Smith, J., & Daley, J. (1992). Executive attitudes, organizational size and ethical issues: Perspectives on a service industry. Journal of Business Ethics, 11(1), 11–19. https://doi.org/10.1007/BF00871987
- Nagengast, L., Evanschitzky, H., Blut, M., & Rudolph, T. (2014). New insights in the moderating effect of switching costs on the satisfaction–repurchase behavior link. Journal of Retailing, 90(3), 408–427. https://doi.org/10.1016/j.jretai.2014.04.001
- Nantel, J., & Weeks, W. A. (1996). Marketing ethics: Is there more to it than the utilitarian approach? European Journal of Marketing, 30(5), 9–19. https://doi.org/10.1108/03090569610118713
- National Department of Health. (2014). Department of Health Strategic Plan 2014/15–2018/19, Health e-News, Pretoria. Accessed March 31 2017, from. https://www.healthe.org.za/2014/09/25/report-department-health-strategic-plan-201415-2 0189/
- National Department of Health (2016). Statistics South Africa. Mid-year population estimates, Pretoria. Accessed May 8 2017, from. https://www.statssa.gov.za/publications/P0302/P03022016.pdf.
- Ngo, V., & Pavelková, D. (2017). Moderating and mediating effects of switching costs on the relationship between service value, customer satisfaction and customer loyalty: Investigation of retail banking in Vietnam. Journal of International Studies, 10(1), 9–33. https://doi.org/10.14254/2071-8330.2017/10-1/1
- Nie, P., Wang, C., Chang, Y., & Yang, Y. (2018). Effects of switching costs on innovative investment. Technological and Economic Development of Economy, 24(3), 933–949. https://doi.org/10.3846/tede.2018.1430
- Nwobodo-Anyadiegwu, E., Ibrahimu, K., & Mbohwa, C. (2018, December). Service quality evaluation: Patients from a South African university clinic. Journal of Industrial and Intelligent Information, 6(2), 50–56. https://doi.org/10.18178/jiii.6.2.50-56
- Oh, J. C., & Yoon, S. J. (2014). Theory-based approach to factors affecting ethical consumption. International Journal of Consumer Studies, 38(3), 278–288. https://doi.org/10.1111/ijcs.12092
- Oliver, R. L. (1993). Cognitive, affective and attribute bases of the satisfaction response. Journal of Consumer Research, 20(3), 418–430. https://doi.org/10.1086/209358
- Oliver, R. L. (1997). Satisfaction: A behavioral perspective on the consumer. McGraw- Hill.
- Oliver, R. L. (1999). Whence consumer loyalty. Journal of Marketing, 63(4_suppl1), 33–44. https://doi.org/10.1177/00222429990634s105
- Pallant, J. (2010). SPSS survival manual. A step by step guide to data analysis using SPSS (4th ed.). [S.l.]: McGraw Hill Education.
- Parasuraman, A., Zeithalm, V. A. & Berry, L. L. (1992). Perceived service quality as customer-based performance measure: an empirical examination of organizational barriers using an extended service quality model. Human Resource Management, 30(3), 335–364. Fall 1991
- Parry, M., & Sarma, E. S. (2019). The impact of pioneer adopter characteristics and perceptions on the perceived costs of switching to a follower product. Asia Pacific Journal of Marketing and Logistics, 31(4), 875–897. https://doi.org/10.1108/APJML-03-2018-0113
- Pezhman, R., Javadi, M. H. M., & Shahin, A. (2013, September). Analyzing the influence of ethical sales behavior on customers loyalty through customer satisfaction and trust in insurance company. International Journal of Academic Research in Business and Social Sciences, 3(9), 754–763. https://doi.org/10.6007/IJARBSS/v3-i9/266
- Porter, M. E. (1980). Competitive Strategy: Techniques for analyzing industries and competitors. The Free Press.
- Ram, J., & Wu, M. (2016). A fresh look at the role of switching cost in influencing customer loyalty: Empirical investigation using structural equation modelling analysis. Asia Pacific Journal of Marketing and Logistics, 28(4), 616–633. https://doi.org/10.1108/APJML-11-2015-0172
- Republic of South Africa. (1996). Constitution of the Republic of South Africa. Government Gazette, 2014 edn., Pretoria, South Africa, viewed n.d., from. https://www.gov.za/documents/constitution/constitution-republic-southafrica-1996-1.
- Román, S. (2003). The impact of ethical sales behavior on customer satisfaction, trust and loyalty to the company: An empirical study in the financial services industry. Journal of Marketing Management, 19(9–10), 915–935. https://doi.org/10.1080/0267257X.2003.9728245
- Rowe, K., & Moodley, K. (2013). Patients as consumers of health care in South Africa: The ethical and legal implications. BMC Medical Ethics, 14(15), 1–9. https://doi.org/10.1186/1472-6939-14-15
- Sanjeepan, N. (2017). A study on impact of switching cost on customer satisfaction for internet banking services at commercial banks in Batticaloa. International Journal of Economics & Management Sciences, 6(2), 402. https://doi.org/10.4172/2162-6359.1000402
- Schenker, Y., Arnold, R. M., & London, A. J. (2014). The ethics of advertising for health care services. The American Journal of Bioethics, 14(3), 34–43. https://doi.org/10.1080/15265161.2013.879943
- Schreiber, J. B., Nora, A., Stage, F. K., Barlow, E. A., & King, J. (2006). Reporting structural equation modeling and confirmatory factor analysis results: A review. The Journal of Educational Research, 99(6), 323–338. https://doi.org/10.3200/JOER.99.6.323-338
- Shan, L., Li, Y., Ding, D., Wu, Q., Liu, C., Jiao, M., Hao, Y., Han, Y., Gao, L., Hao, J., Wang, L., Xu, W., & Ren, J. (2016, October). Patient satisfaction with hospital in patient care: Effects of trust, medical insurance and perceived quality of care. PLoS ONE, 11(10), 1–18. https://doi.org/10.1371/journal.pone.0164366
- Singh, J. (1991). Understanding the structure of consumers’ satisfaction evaluations of service delivery. Journal of the Academy of Marketing Science, 19(3), 223–244. https://doi.org/10.1007/BF02726498
- Singhapakdi, A., Rao, C. P., & Vitell, S. J. (1996). Ethical decision making: An investigation of services marketing professionals. Journal of Business Ethics, 15(6), 635–644. https://doi.org/10.1007/BF00411798
- Sirgy, M. J., & Lee, D. (2008). Well-being marketing: An ethical business philosophy for consumer goods firms. Journal of Business Ethics, 77(4), 377–403. https://doi.org/10.1007/s10551-007-9363-y
- Tang, L. (2011). The influences of patient’s trust in medical service and attitude towards health policy on patient’s overall satisfaction with medical service and sub satisfaction in China. BMC Public Health, 11(472), 1–8. https://doi.org/10.1186/1471-2458-11-472
- Thomas, J. L., Vitell, S. J., Gilbert, F. Y., & Rose, G. M. (2002). The impact of ethical cues on customer satisfaction with service. Journal of Retailing, 78(3), 167–173. https://doi.org/10.1016/S0022-4359(02)00062-3
- Tuu, H. H. (2015, August). The moderator effects of switching costs and customer expertise in the satisfaction-repurchase intention relationship for mobile telecommunication services. Journal of Economics and Development, 17(2), 83–103.
- Ul Hadi, N., Aslam, N., & Gulzar, A. (2019). Sustainable service quality and customer loyalty: The r ole of customer satisfaction and switching costs in the Pakistan cellphone industry. Sustainability, 11(2408), 1–17. doi: 10.3390/su11082408
- Wagstaff, A., Cotlear, D., Eozenou, P. H.-V., & Buisman, L. R. (2016). Measuring progress towards universal health coverage: With an application to 24 developing countries. Oxford Review of Economic Policy, 32(1), 147–189. https://doi.org/10.1093/oxrep/grv019
- Whitten, D., & Wakefield, R. L. (2006). Measuring switching costs in IT outsourcing services. Journal of Strategic Information Systems, 15(3), 219–248. https://doi.org/10.1016/j.jsis.2005.11.002
- Willys, N. (2018). Customer satisfaction, switching costs and customer loyalty: An empirical study on the mobile telecommunication service. American Journal of Industrial and Business Management, 8(4), 1022–1037. https://doi.org/10.4236/ajibm.2018.84070
- Yang, Z., & Peterson, R. T. (2004, October). Customer perceived value, satisfaction, and loyalty: The role of switching costs. Psychology & Marketing, 21(10), 799–822. https://doi.org/10.1002/mar.20030
- Yen, Y. (2010). Can perceived risks affect the relationship of switching costs and customer loyalty in e-commerce? Internet Research, 20(2), 210–224. https://doi.org/10.1108/10662241011032254
- Yoon, M. H., & Suh, J. (2003). Organizational citizenship behaviors and service quality as external effectiveness of contact employees. Journal of Business Research, 56(8), 597–611. https://doi.org/10.1016/S0148-2963(01)00290-9
- Zeithaml, V. A., Berry, L. L., & Parasuraman, A. (1996). The behavioral consequences of service quality. Journal of Marketing, 60(2), 31–46. https://doi.org/10.2307/1251929