?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
The outbreak of COVID-19 severely affected the achievement of the sustainable development goals. The American Hospital Association estimated an average loss of US$50.7 billion per month for US hospitals during the COVID-19 pandemic. In the less developed economies, it costs about US$52 billion per month to effectively manage COVID-19. This current study, therefore, sought to assess how risk management practices could moderate the relationship between supply chain risk and healthcare delivery, during the COVID-19 pandemic. A survey research design was adopted, with a quantitative research approach. The study adopted purposive sampling technique to select 216 respondents (senior/management members from procurement, stores/inventory, pharmacy, and administration) of the selected public hospitals. Structural Equation Modelling (SEM) was run in Amos (v.23), to estimate the path coefficients. The study concludes that supply chain risk had a significant negative effect on healthcare delivery among public hospitals in Ghana. Also, supply chain risk management had a significant positive effect on healthcare delivery among public hospitals in Ghana. Finally, it was concluded that risk management practices positively moderated the negative effect on supply chain risk on healthcare delivery.
1. Introduction
Effective supply chain is essential for the success of businesses (Amoako et al., Citation2022, Citation2022). Three key aspects of supply chain (cost-effectiveness, timely delivery, and quality), when achieved, contribute to the success and competitive advantage of firms (Haleem et al., Citation2018; Wiengarten et al., Citation2016). However, the turbulent and dynamic business environment affect the effectiveness and efficiency of supply chain. This turbulent and dynamic business environment, results in unexpected disruptions, affecting supply chain performance (Ahmed & Huma, Citation2021; Borah et al., Citation2023; Kauppi et al., Citation2016). These disruptions within the supply chain expose firms to what is termed supply chain risk. The outbreak of COVID-19 for example is a classic example of supply chain risk, where production of some goods halted, national borders closed (affecting the shipment of goods), diversification of resources into essential COVID-19 medical supplies, etc. (Haque et al., Citation2022; Hebbar et al., Citation2020; Ngoc et al., Citation2021). Jiang et al. (Citation2021) identified that, during the pandemic, sustainable development goals severely affected. The American Hospital Association estimated an average loss of US$50.7 billion per month for US hospitals during the COVID-19 pandemic (Kaye et al., Citation2021). In the less developed economies, it costs about US$52 billion per month to effectively manage COVID-19 (Kaye et al., Citation2021). The present study therefore sought to assess the effect of supply chain risks on healthcare delivery, and how effective risk management, could help mitigate the effects of supply chain risks.
Effective healthcare system and delivery is important for the economic stability of any nation (Ngoc et al., Citation2021; Rasheed et al., Citation2021). This was evident during the COVID-19 outbreak, where nations with a more robust healthcare system were able to manage the virus, and quickly bounced back its economy (Kaftan et al., Citation2023). Supply chain risk however undermines the effectiveness of healthcare systems, it causes disruptions which negatively affects healthcare delivery. Attention on health supply chain risk in literature and specific attention on its impact on healthcare delivery in less developed countries is very limited. For example, Singh and Parida (Citation2022) looked at the “Decision-making models for healthcare supply chain disruptions: review and insights for post-pandemic era”, while in Italy, Aldrighetti et al. (Citation2019) also assessed “healthcare supply chain simulation with disruption considerations”. These notwithstanding, the economy of less developed countries suffered the most, during the outbreak of the pandemic, with some countries still struggling to bounce back their economies (Anyanwu & Salami, Citation2021; Ataguba, Citation2020). The weak healthcare system in developing countries was further hampered by the outbreak of the pandemic (Okereke et al., Citation2021). This therefore calls for specific attention on the effect of health supply chain risk on healthcare delivery in Africa, specifically Ghana, and the role of risk management.
Supply chain risk management is the process of finding good managerial ways to reduce risk in supply chain process (Abdel-Basset & Mohamed, Citation2020; Duong et al., Citation2021), which are essential for mitigating the devastating effects of the inherent risks in supply chain, arising from the turbulent business environment. A number of strategies have been identified to reduce the negative effects of supply chain risks, such as procrastination, dual sourcing and redundancy (Bastas & Liyanage, Citation2018; Gupta & Ivanov, Citation2020; Kamalahmadi et al., Citation2021). Despite the importance of risk management, not much is done on risk management practices within the health sector. Senna et al. (Citation2020) for example, conducted “A systematic literature review on supply chain risk management: is healthcare management a forsaken research field?”. The current study thus extends knowledge by looking at the role of risk management, in mitigating the effect of supply chain risk on healthcare delivery in Ghana.
The measures taken globally (travel restrictions, social distancing, and lockdowns), to reduce the spread of COVID-19 came at a cost. The Social Accounting Matrix multiplier model estimated that Ghana’s 3 weeks urban lockdown caused 27.9% drop in GDP, and making extra 3.8 million Ghanaians to become temporarily poor (Amewu et al., Citation2020). Aduhene and Osei-Assibey (Citation2021) revealed that, during the peak of the COVID-19 pandemic, Ghana’s healthcare system was overwhelmed, so the country had to resort to temporary structures as isolation and treatment centers. Dzigbede and Pathak (Citation2020) further added that, the outbreak of COVID-19 pushed more Ghanaians into poverty zone, and also led to an increase in government spending. A study by Yu et al. (Citation2021) also focused on the disruptions in global supply chain and socio-economic shocks during the COVID-19 pandemic. With the devastating effects of COVID-19, it is essential to ascertain how the healthcare supply chain was also affected.
The remaining sections of the study were organized as follows. Section 2 considers the literature review, where consideration was given to the relationships between supply chain risks and healthcare delivery, supply chain risk management and healthcare delivery, and the moderating role of healthcare supply chain risk management. Section 3 presents the methods of the study, where attention was placed on population, sample, sampling technique, data collection instruments, validity and reliability analyses. Section 4 presents the path analysis, while Section 5 presents the discussion of results and theoretical contributions. Managerial implications followed, and finally, conclusions, limitations and future research suggestions were presented. Figure presents the conceptual framework of the study.
2. Literature review
2.1. Supply chain risks and healthcare delivery
Supply chain risk is anything that affects the in-flow and out-flow of material or information from a supplier to the end customer (Richardson et al., Citation2021). Any form of risk being physical or non-physical can interrupt the free flow of organization operations (Tang & Musa, Citation2011). The challenges in supply chains have exposed firms to several risks from both internal and external (Asafo-Adjei et al., Citation2023; Panova & Hilletofth, Citation2018). Supply chain risks can be grouped into four viz., physical, financial, informational, and relational (Ho et al., Citation2015). Physical supply chain focuses on how to transport goods from the manufacturer to a place where the consumer can get access. Financial supply chain is the flow of money in the supply chain, while informational supply chain focuses on both the material and monetary chains that are used to create electronic system for service operation. Relational supply chain focuses on the connections between producers, transporters and consumers.
Supply chain risks in healthcare originate from various sources, inadequate medical supply, unpredictable demand from customer, pharmaceutical counterfeits, low technology, strikes from medical practitioners, irregular power supply, infrastructure deficit, longer supply chain processes, unpredictable fuel and transportation prices (Shenoi et al., Citation2021). Health facilities do not just focus on reducing healthcare supply chain risks and its effect of healthcare delivery, they also focus on reducing and managing future risks (Fathollahi-Fard et al., Citation2022). Like other organizations, the hospital is not immune to the shocks in supply chain, and this was evident during the COVID-19 pandemic (Goodarzian et al., Citation2021). The COVID-19 pandemic led to a reduction in production capacity, national stockpiling and ban on exports, which affected the pharmaceutical supply chain (Jifar et al., Citation2022). That notwithstanding, effective supply chain systems are needed to move essential pharmaceuticals from the manufacturer to end users at service delivery point (Goodarzian et al., Citation2021). Shortages were therefore recorded for some essential medicines, which affected the effectiveness of healthcare delivery during the COVID-19 pandemic. Sibevei et al. (Citation2022) identified that supply chain risk negatively affected health systems in Iran. In the pharmaceutical sector, Breen (Citation2008) identified that supply chain risk, negatively affected the performance of national health service. We therefore hypothesize based on the discussions that;
H1:
Supply chain risk has a significant negative effect on healthcare delivery among public hospitals in Ghana.
2.2. Supply chain risk management and healthcare delivery
Ho et al. (Citation2015, p. 5036) defined supply chain risk management as “an inter-organisational collaborative endeavour utilising quantitative and qualitative risk management methodologies to identify, evaluate, mitigate and monitor unexpected macro and micro level events or conditions, which might adversely impact any part of a supply chain”. Chapman et al. (Citation2002, p. 3) also defined supply chain risk management as “the identification and management of risks within the supply chain and risks external to it, through a co-ordinated approach amongst supply-chain members, to reduce supply-chain vulnerability as a whole”. The aim of supply chain risk management is to make assessment of the potential sources of risk and to adopt strategies that will help mitigate the effects of the risks (Duong et al., Citation2021). Some supply chain risks are exogenous, thereby exerting serious shocks to the supply chain, leading to possible collapse and disruptions in the entire network (Dolgui & Ivanov, Citation2021; Sodhi & Tang, Citation2021). The ripple effects realized from these shocks could cause a change in the supply chain structure (Goodarzian et al., Citation2022). COVID-19 was an external shock which caused destruction in the global health supply chain system, causing shortages in medical supplies, affecting the effectiveness to deliver health service. Effective supply chain management could thus enhance health service delivery (Behera & Kannan, 2018).
Health providers’ ability to effectively manage these disruptions is essential for effective health service delivery (Fathollahi-Fard et al., Citation2021, Citation2022). Risk management system adds value and increases organizational performance (Pilbeam et al., Citation2012). Hospitals need to implement risk management system as part of the organizational culture to provide clear road map for risk management activities to better the organizational performance (Abdel-Basset & Mohamed, Citation2020). Organizations that give more attention to risk management culture are able to withstand the dangers that will hit the organization in future and also respond and recover quickly from supply chain disruptions (Anton & Nucu, Citation2020). Managing risk in healthcare sector is very crucial because it provides the opportunity to identify the possible sources of risks in supply chain activities (Iqbal et al., Citation2017; Nazam et al., Citation2020). In a systematic literature review by Senna et al. (Citation2020), they found that supply chain risk management positively affected healthcare management. In Malawi, Kanyoma et al. (Citation2013) identified that supply chain risk management positively influenced public healthcare delivery. In a similar study by Senna et al. (Citation2022), healthcare supply chain risk management positively affected healthcare delivery. We therefore hypothesize based on the discussions that;
H2:
Supply chain risk management will have a significant positive effect on healthcare delivery among public hospitals in Ghana.
2.3. Moderating role of healthcare supply chain risk management
Supply chain risk management has become a major consideration for organisations in recent times, especially with the advent of COVID-19 (Abdel-Basset & Mohamed, Citation2020; Mawonde et al., Citation2023). Organisations, including health service providers, are expected to build quality relationship with their suppliers and clients, for a superior service delivery (Hashemi et al., Citation2022; Khorasani et al., Citation2020). Sodhi et al. (Citation2012) identified that risk management can improve decision-making processes. Risk management within a hospital is significant to protect cost and loss in the present and the future (Sodhi et al., Citation2012). Supply chain risk management gives more knowledge and understanding on how to implement measures to reduce dangers and problems that hinders the free flow of supply chain (Abdel-Basset & Mohamed, Citation2020).
Risk management is important to healthcare supply chain because it helps to make clear decisions that optimally provides strategic processes in reducing risks (Iqbal et al., Citation2017). Risk management contributes to adopting good strategies by bestowing hospitals with a set of principles concerning how to properly response to unpredicted danger (Vishnu et al., Citation2019). It suggests that supply chain risk management will help hospitals to successfully initiate strategies, especially when it comes to healthcare delivery. Adoption of risk management strategies by health providers will help mitigate the effects of supply chain risks caused by the advent of the COVID-19 pandemic. Effective risk management strategy will therefore help to ensure effective healthcare delivery, despite the available risks in the health supply chain. That is, although the COVID-19 pandemic caused significant risks in the health supply chain (Fathollahi-Fard et al., Citation2022; Jifar et al., Citation2022), healthcare providers with effective supply chain risk management strategies, were able delivery effective health service to patients. We therefore hypothesize that;
H3:
Supply chain risk management will significantly moderate the direct impact of supply chain risk and healthcare delivery among public hospitals in Ghana.
3. Methods
3.1. Population, sample and sampling technique
There are two groups of public hospital, which are Government and Christian Health Association of Ghana (CHAG). Although there are some other health facilities such as Clinics, Health Centres, Maternity Homes, and CHPS, this present study only focused on health facilities classified as main stream hospital by Ministry of Health. These hospitals were selected because they provided a comprehensive health service and served a larger community. Local authorities were also not included in the study, because the study focused specifically on healthcare delivery, and hospital staff were the best category of respondents to offer the required information. The unit of analysis was the healthcare sector, as the study focused on healthcare delivery. Multiple respondents were selected from one hospital because different units of the hospital might have different view on the effectiveness of healthcare delivery. Having multiple respondents therefore provides an avenue for a wholistic assessment of the healthcare delivery of the hospitals, as was also done in a study by Iddris et al. (Citation2022) in the insurance sector. Purposive sampling technique was used in selecting senior staff from the supply chain, procurement, stores, pharmacy and administrative units of the selected public hospitals in Ashanti region of Ghana. Out of the 38 public hospitals in the region, 27 agreed to participate in the study, which was considered adequate enough for the study. In each of the hospitals, two procurement staff, two stores/inventory staff, two pharmacy staff, and two administrative staff were selected. This gave a total of 6 respondents from each hospital, giving a total of 216 responses. The analysis was therefore based on 216 responses. The respondents were senior/management members of the selected hospitals.
3.2. Data collection instruments
Structure questionnaire was used as data collection instrument for the study. Self-administered questionnaire was adopted since respondents could read and write. However, when clarification was sought, the researcher is available to clarify. The questionnaire had four parts. Part I contained respondents’ information, and Part II assessed healthcare supply chain risks. Part III determined the healthcare supply chain risks management practices engaged by the hospitals; and Part IV ascertained the healthcare deliver at the various hospitals. Items from Part II to IV were answered on a Likert scale of 1-Strongly Disagree, 2-Disagree, 3-Indifferent, 4-Agree, and 5-Strongly Agree. The measurement items under healthcare supply chain risk were adapted from Sreedevi and Saranga (Citation2017) and Macdonald et al. (Citation2018); while those of healthcare supply chain risk management were adapted from Fan and Stevenson (Citation2018) and Manhart et al. (Citation2020); and those of healthcare performance were also adapted from Hebbar et al. (Citation2020) and Gordon et al. (Citation2020).
3.3. Data validity and reliability analysis
The study conducted a Structural Equation Modelling (SEM) which was run in Amos (v.23). As a methodological approach, running any estimation models such as SEM requires the data to be tested as valid and reliable. Else the estimated results will be misleading. For this reason, a number of approaches were taken to ensure the data used in the model estimation were valid and reliable. As part of SEM, it is expected that the Exploratory Factor Analysis (EFA) and Confirmatory Factor Analysis (CFA) are presented to ensure the soundness of the path estimates. Discriminant validity was also checked.
An Exploratory Factor Analysis (EFA) was run in SPSS (v.23). There were three main constructs for the study, which were supply chain risk, supply chain risk management, and healthcare delivery. Supply chain risk however was a higher/second-order dimension with six first-order variables which were demand risk, delay risk, inventory risk, supply risk, system risk, and transportation risk. This therefore gave a total of 8 variables, including supply chain risk management and delivery. The questionnaire 3 measurement items for demand risk, 4 measurement items for delay risk, 4 measurement items for inventory risk, 6 measurement items for supply risk, 3 measurement items for systems risk, 5 measurement items for transportation risk, 6 measurement items as supply chain risk management practices, and 10 items were used in measuring healthcare delivery. The EFA helped to determine if these measurement items correctly loaded under the respective observed variables. A minimum factor loading of 0.5 was expected, and measurement items were also expected to load under their respective latent variables. Measurement items which failed to meet these criteria were deleted. After the EFA process, two measurement items from healthcare deliver were deleted, and 1 item each were deleted from transportation risk and supply chain management practices.
The extraction method was the Principal Component Analysis, while the rotation method was Varimax with Kaiser Normalization. The rotation converged in five iterations, with the Eigenvalues for each of the extracted factors being greater than 1. The total variance extracted (TVE) was expected to be at least 50%, and from Table , we realize the TVE for this study was 79.54%, which was very high. The Kaiser–Meyer–Olkin (KMO) Measure of Sampling Adequacy, and a minimum of 0.6 is expected. This study however scored 0.87.9. The Bartlett’s Test of Sphericity is expected to be statistically significant, to indicate there exist adequate relationships between the variables to warrant EFA. Results for this were statistically significant (x2 = 5373.422; Sig. = 0.000), indicating EFA was appropriately conducted. The correlation Determinant is expected to be not equal to zero (0), which signifies positive assurance. The Determinant for this EFA was 0.03 (greater than 0), indicating there was great assurance in the data used for the estimation.
Table 1. Exploratory Factor Analysis (EFA)
After the EFA met the individual thresholds, CFA was further run using the data, as presented in Table . Just like the EFA, the standardized factor loadings for each measurement variables are expected to be at least 0.5. From the CFA results, the least factor loading was 0.634 (HCD3), which indicated that all the measurement items had factor loading of greater than the minimum expected value of 0.5. This was accomplished for all the retained measurement items, showing the measurement items positively affect the proposed latent variables. The Cronbach’s Alpha (CA) for all the variables were larger than the minimum expected value of 0.7, indicating there was high internal consistency (reliability) among the measurement variables.
Table 2. Confirmatory Factor Analysis (CFA)
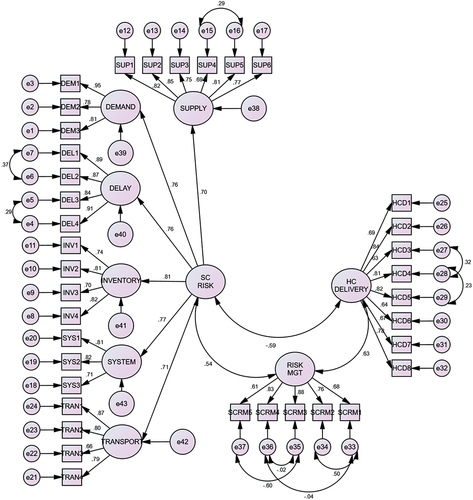
As per model fit indices, CMIN/DF is expected to be less than 3, GFI should be at least 0.8, TLI and CFI are all expected to be greater than 0.9, whiles RMSEA and SRMR are also expected to be less than 0.08 (Hair et al., Citation2010). From Table , it is shown that the outcome met these thresholds, and so it was concluded that the data appropriately fit the construct model. To attain common validity, Average Variance Extracted (AVE) should be greater than 0.5, with Composite Reliability (CR) and Cronbach’s alpha (CA) also being at least 0.7 (Fornell & Larcker, Citation1981), and these were also achieved as presented in Table . Figure presents the output of CFA.
The study assessed discriminant validity by comparing the square-root of Average Variance Extracted (√AVE) to the respective inter-correlation coefficients. To claim discriminant validity, the √AVE should be higher than the respective inter-correlation coefficients (Bamfo et al., Citation2018). As was the case in Table , the least √AVE was 0.740, which was more than the highest correlation score of 0.631. Another area in model estimation is multicollinearity, that is, high correlation among two predicting variables. Coefficients of 0.8 are usually considered as high, which may cause confounding effect in the model estimation. The highest coefficient score of 0.631 however indicates multicollinearity was not a challenge to the reliability of the model estimated. It was therefore concluded from the CFA analysis, that the data was valid for model estimation.
Table 3. Discriminant validity
4. Path analysis
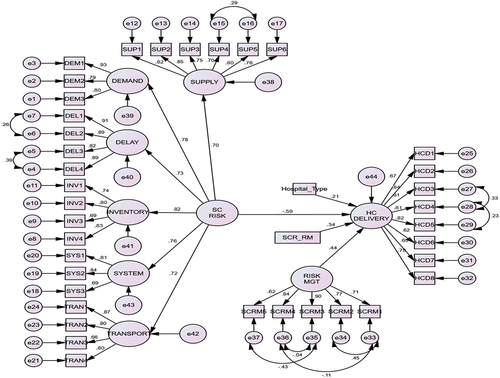
Structural Equation Modelling (SEM) was run in estimating the path coefficient using Amos (v.23) after checking data reliability and validity. The results were presented in Table and Figure . The study controlled for one variable, which was the type of hospital (be it CHAG or Government). The type of hospital was controlled for because this could influence the outcome of the study, and its effects must therefore be considered. From the analysis, hospital type had a positive and significant effect on healthcare delivery (HC_DELIVERY). The type of hospital was categorical data and was coded 0=CHAG and 1=Government. A positive coefficient therefore indicates government hospitals performance significantly better than CHAG.
Table 4. Path Estimates
First, the study sought to assess the effect of supply chain risks on healthcare delivery among public hospitals in Ghana. From the results presented, it was realized that supply chain risk (SC_RISK) had negative influence on healthcare delivery (). This implies that supply chain risks were detrimental to the healthcare delivery (performance) of public hospitals. Based on these results, H1 (supply chain risk has a direct negative effect on healthcare delivery among public hospitals in Ghana) was therefore accepted. It is therefore understood that supply chain risks such as demand, delay, inventory, supply, systems, and transportation, had a negative toll on the effectiveness of healthcare delivery among public hospitals in Ghana. Secondly, the study sought to assess the effect of supply chain risks management practices on healthcare delivery among public hospitals in Ghana. From the results presented, it was realized that supply chain risk management (RISK_MGT) was positively associated with healthcare delivery (
). This implies that, risk management practices such as, prioritizing risk events based on severity of impact to hospital; involving clients in identifying and reducing future supply chain risks; understanding stakeholders to deal with any problems relating to cost in material supplying and realizing how to plan and manage risks, had a positive influence on healthcare delivery. Based on these results, H2 (supply chain risk management has a direct positive effect on healthcare delivery among public hospitals in Ghana) was therefore accepted.
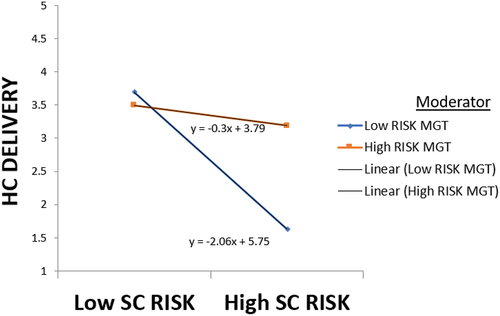
The study also assessed the moderating role of supply chain risk management practices, in the relationship between supply chain risks and healthcare delivery among public hospitals in Ghana. From the results presented, the interaction term (SCR_RM) is positively associated with healthcare delivery (). SCR_RM as a variable represents the multiplication of the residuals of supply chain risks and risks management practices. This implies that, risk management practices positively moderated the negative effect on supply chain risk on healthcare delivery. That is, although supply chain risk has a negative effect on healthcare delivery, hospitals with effective risk management practices are able to counter this negative effect. Figure presents the interaction diagram, the highest score for healthcare delivery was when there was both low supply chain risks and risk management practices (blue line). This is so because when there is no or less risk, there will be no or less need for risk management practices. Risk management practices are to counter risk, so where there is no risk, there is no need for investment in risk management practices. Hospitals could therefore channel risk management investments into other areas of business operations for an enhanced health service delivery. In a similar manner, Figure shows that when supply chain risk is high, but there is low-risk management efficiency, healthcare delivery was at its lowest (blue line). Healthcare delivery was however much higher when there was high-risk management practice (orange line) to counter the negative effect of high supply chain risks. Based on these results, H3 (supply chain risk management will moderate the relationship between supply chain risk and healthcare delivery among public hospitals in Ghana) was therefore accepted.
5. Discussion of results and theoretical contributions
Supply chain risk was identified to have a significant negative effect on healthcare delivery among public hospitals in Ghana. Supply chain risks emanating from inventory, delay, supply/procurement, transportation, demand and system, negatively affected the effectiveness of healthcare delivery. A study by Jifar et al. (Citation2022) to assess the impact of COVID-19 on pharmaceutical shortages and supply disruptions for non-communicable diseases among public hospitals in Ethiopia also came to similar findings. Fathollahi-Fard et al. (Citation2022) proposed a sustainable and robust home healthcare logistics, as a response to the COVID-19 pandemic. In the Iranian health sector, Sibevei et al. (Citation2022) identified that supply chain risk negatively affected health systems. Similarly, Breen (Citation2008) found that, supply chain risk had a negative effect on the performance of national health service.
Moreover, supply chain risk management was found to have a significant positive influence on healthcare delivery among public hospitals in Ghana. Managing risk is vital to know the future sources and causes of the in supply chain process. This implies that, risk management practices such as, prioritizing risk events based on severity of impact to hospital; involving clients in identifying and reducing future supply chain risks; understanding stakeholders to deal with any problems relating to cost in material supplying and realizing how to plan and manage risks, had a positive influence on healthcare delivery. This finding of the study further contributes to contingency theory, which place emphasis on making decision based on the situation at hand because there is no one best way to make decision (Burns & Stalker, Citation1961). Gordon et al. (Citation2020) also stated the need to set official procedures for managing risk in and among organizations. Senna et al. (Citation2020) conducted a systematic literature review on supply chain risk management within the healthcare sector. They concluded supply chain risk management entails an understanding that supply chain represents a set of processes with potential risks, and these risks could be managed through identification, assessment, mitigation and monitoring. Prior studies (Senna et al., Citation2020, Citation2022), concluded that supply chain risk management positively affected healthcare management. Similarly, in Malawi, Kanyoma et al. (Citation2013) concluded that supply chain risk management positively influenced public healthcare delivery.
Lastly, the study found that risk management practices positively moderated the negative effect on supply chain risk on healthcare delivery. That is, although supply chain risk has a negative effect on healthcare delivery, hospitals with effective risk management practices are able to counter this negative effect. This was in line with past studies such as McShane et al. (Citation2011) and Haque and Islam (Citation2013) who identified risk management as a critical tool to nullify inevitable supply chain risks. It was realized that, the highest score for healthcare delivery was when there were both low supply chain risks and risk management practices (Figure ). This was so because when there is no or less risk, there will be no or less need for risk management practices. Risk management practices are to counter risk, so where there is no risk, there is no need for investment in risk management practices. Hospitals could therefore channel risk management investments into other areas of business operations for an enhanced health service delivery. In a similar manner, healthcare delivery was at its lowest when risk in supply chain is high, but there is poor-risk management. Healthcare delivery was however much higher when there was high-risk management practice to counter the negative effect of high supply chain risks (Fathollahi-Fard et al., Citation2022; Goodarzian et al., Citation2021, Citation2021). Govindan et al. (Citation2020) assessed the decision support system for demand management in healthcare supply chains during the COVID-19 pandemic.
6. Managerial implications
It must be realized that some supply chain risks are inevitable. As such, the only option left is to hedge around it by adopting appropriate risk management practices. For example, the COVID-19 pandemic has had a significant effect on healthcare supply chain, and this risk was inevitable. Firms or health facilities with proactive risk management practices will however be able to cope with the disruptions in supply chain. The findings of the study provide some important implications to management of health facilities.
First, management of hospitals should involve their suppliers in the supply chain process to be able to identify future risks. By this, both parties could brainstorm on the potential risks’ occurrences, and how to best solve them together. Since every supply chain is made up of many actors, it is expedient to involve them all in the identification and mitigation of potential risk which will affect the supply chain.
Second, management must share cost which emanates from supply chain disruptions, with supply chain members like suppliers. This agreement must be contractual, that is well-documented to make them binding on all parties. By doing so in case of any eventuality, cost could be shared to reduce the burden of the hospitals. For example, there could be a contractual agreement between hospitals and pharmaceutical drug suppliers that expired goods/medicine (which is associated with inventory risk) could be returned and cost of goods/medicines shared based on predefined percentage term. Whenever problem arise during material supply, management (hospitals) and suppliers must mutually bear the responsibility.
Finally, hospitals should follow the laid down procedures for managing risk in their operations. Management must invest in the process/technology of risk identification, engage experts on risk analysis, must develop plan on how to counter the risks, and subsequently establish the control measures.
7. Conclusions and future Research suggestions
The study assessed the moderating effect of risk management practices in the relationship between supply chain risk and healthcare delivery among public hospitals in Ghana. It was concluded that supply chain risk negatively affected healthcare delivery during the COVID-19 pandemic. Risk management practices, however, had significant positive effect on healthcare delivery. Finally, it was concluded that risk management practices positively moderated the negative effect of supply chain risk on healthcare delivery. That is, although supply chain risk has a negative effect on healthcare delivery, hospitals with effective risk management practices are able to counter this negative effect.
The present study used demand risk, delay risk, inventory risk, supply risk, system risk, and transportation risk, as the first-order variable for the second-order variable (supply chain risk). The influence of COVID-19 on these supply chain risks may not be the same across board. As such, it is essential to consider the individual effects of supply chain risk dimensions, on health service delivery. Future studies could therefore pay attention to this. This may offer new insights into the effect of supply chain risk on healthcare delivery.
Disclosure statement
No potential conflict of interest.
Data availability statement
Data shall be made available upon request.
References
- Abdel-Basset, M., & Mohamed, R. (2020). A novel plithogenic TOPSIS-CRITIC model for sustainable supply chain risk management. Journal of Cleaner Production, 247, 119586. https://doi.org/10.1016/j.jclepro.2019.119586
- Aduhene, D. T., & Osei-Assibey, E. (2021). Socio-economic impact of COVID-19 on Ghana’s economy: Challenges and prospects. International Journal of Social Economics, 48(4), 543–17. https://doi.org/10.1108/IJSE-08-2020-0582
- Ahmed, W., & Huma, S. (2021). Impact of lean and agile strategies on supply chain risk management. Total Quality Management & Business Excellence, 32(1–2), 33–56. https://doi.org/10.1080/14783363.2018.1529558
- Aldrighetti, R., Zennaro, I., Finco, S., & Battini, D. (2019). Healthcare supply chain simulation with disruption considerations: A case study from Northern Italy. Global Journal of Flexible Systems Management, 20(Suppl 1), 81–102. https://doi.org/10.1007/s40171-019-00223-8
- Amewu, S., Asante, S., Pauw, K., & Thurlow, J. (2020). The economic costs of COVID-19 in sub-saharan Africa: Insights from a simulation exercise for Ghana. European Journal of Development Research, 32(5), 1353–1378. https://doi.org/10.1057/s41287-020-00332-6
- Amoako, T., Huai Sheng, Z., Dogbe, C. S. K., & Pomegbe, W. W. K. (2022). Effect of internal integration on SMEs’ performance: The role of external integration and ICT. International Journal of Productivity and Performance Management, 71(2), 643–665. https://doi.org/10.1108/IJPPM-03-2020-0120
- Amoako, T., Sheng, Z. H., Dogbe, C. S. K., & Pomegbe, W. W. K. (2022). Assessing the moderation role of ICT in the relationship between supply chain integration and SME performance. Journal of Industrial Integration and Management, 7(2), 203–233. https://doi.org/10.1142/S2424862221500160
- Anton, S. G., & Nucu, A. E. A. (2020). Enterprise risk management: A literature review and agenda for future research. Journal of Risk and Financial Management, 13(11), 281. https://doi.org/10.3390/jrfm13110281
- Anyanwu, J. C., & Salami, A. O. (2021). The impact of COVID‐19 on African economies: An introduction. African Development Review, 33(Suppl 1), S1. https://doi.org/10.1111/1467-8268.12531
- Asafo-Adjei, E., Hamidu, Z., Issau, K., Seidu, B. A., & Adam, A. M. (2023). The dark and bright side of network complexity: Novel insights from an asymmetric supply chain recovery and disruption approach. Cogent Business & Management, 10(2), 2225808. https://doi.org/10.1080/23311975.2023.2225808
- Ataguba, J. E. (2020). COVID-19 pandemic, a war to be won: Understanding its economic implications for Africa. Applied Health Economics and Health Policy, 18(3), 325–328. https://doi.org/10.1007/s40258-020-00580-x
- Bamfo, B. A., Dogbe, C. S. K., Mingle, H., & Wright, L. T. (2018). Abusive customer behaviour and frontline employee turnover intentions in the banking industry: The mediating role of employee satisfaction. Cogent Business & Management, 5(1), 1522753. https://doi.org/10.1080/23311975.2018.1522753
- Bastas, A., & Liyanage, K. (2018). Sustainable supply chain quality management: A systematic review. Journal of Cleaner Production, 181, 726–744. https://doi.org/10.1016/j.jclepro.2018.01.110
- Borah, P. S., Dogbe, C. S. K., Dzandu, M. D., & Pomegbe, W. W. K. (2023). Forging organizational resilience through green value co‐creation: The role of green technology, green operations, and green transaction capabilities. Business Strategy and the Environment. https://doi.org/10.1002/bse.3446
- Breen, L. (2008). A preliminary examination of risk in the Pharmaceutical Supply Chain (PSC) in the National Health Service (NHS). http://bradscholars.brad.ac.uk/handle/10454/7206
- Burns, T., & Stalker, G. M. (1961). The management of Innovation. Tavistock Publishing.
- Chapman, P., Christopher, M., Jüttner, U., Peck, H., & Wilding, R. (2002). Identifying and managing supply chain vulnerability. Logistics and Transport Focus, 4(4), 1–6.
- Dolgui, A., & Ivanov, D. (2021). Ripple effect and supply chain disruption management: New trends and research directions. International Journal of Production Research, 59(1), 102–109. https://doi.org/10.1080/00207543.2021.1840148
- Duong, N. H., Ha, Q. A., & Tan, A. W. K. (2021). The links between supply chain risk management practices, supply chain integration and supply chain performance in Southern Vietnam: A moderation effect of supply chain social sustainability. Cogent Business & Management, 8(1), 1999556. https://doi.org/10.1080/23311975.2021
- Dzigbede, K. D., & Pathak, R. (2020). COVID-19 economic shocks and fiscal policy options for Ghana. Journal of Public Budgeting, Accounting & Financial Management, 32(5), 903–917. https://doi.org/10.1108/JPBAFM-07-2020-0127
- Fan, Y., & Stevenson, M. (2018). A review of supply chain risk management: Definition, theory, and research agenda. International Journal of Physical Distribution & Logistics Management, 48(3), 205–230. https://doi.org/10.1108/IJPDLM-01-2017-0043
- Fathollahi-Fard, A. M., Ahmadi, A., & Karimi, B. (2021). Multi-objective optimization of home healthcare with working-time balancing and care continuity. Sustainability, 13(22), 12431. https://doi.org/10.3390/su132212431
- Fathollahi-Fard, A. M., Ahmadi, A., & Karimi, B. (2022). Sustainable and robust home healthcare logistics: A response to the COVID-19 pandemic. Symmetry, 14(2), 193. https://doi.org/10.3390/sym14020193
- Fornell, C., & Larcker, D. F. (1981). Evaluating structural equation models with unobservable variables and measurement error. Journal of Marketing Research, 18(1), 39–50. https://doi.org/10.1177/002224378101800104
- Goodarzian, F., Ghasemi, P., Gunasekaren, A., Taleizadeh, A. A., & Abraham, A. (2021). A sustainable-resilience healthcare network for handling COVID-19 pandemic. Annals of Operations Research, 312(2), 1–65. https://doi.org/10.1007/s10479-021-04238-2
- Goodarzian, F., Navaei, A., Ehsani, B., Ghasemi, P., & Muñuzuri, J. (2022). Designing an integrated responsive-green-cold vaccine supply chain network using internet-of-things: Artificial intelligence-based solutions. Annals of Operations Research, 328(1), 1–45. https://doi.org/10.1007/s10479-022-04713-4
- Goodarzian, F., Taleizadeh, A. A., Ghasemi, P., & Abraham, A. (2021). An integrated sustainable medical supply chain network during COVID-19. Engineering Applications of Artificial Intelligence, 100, 104188. https://doi.org/10.1016/j.engappai.2021.104188
- Gordon, A. L., Goodman, C., Achterberg, W., Barker, R. O., Burns, E., Hanratty, B., & Spilsbury, K. (2020). Commentary: COVID in care homes—challenges and dilemmas in healthcare delivery. Age and Ageing, 49(5), 701–705. https://doi.org/10.1093/ageing/afaa113
- Govindan, K., Mina, H., & Alavi, B. (2020). A decision support system for demand management in healthcare supply chains considering the epidemic outbreaks: A case study of coronavirus disease 2019 (COVID-19). Transportation Research Part E: Logistics & Transportation Review, 138, 101967. https://doi.org/10.1016/j.tre.2020.101967
- Gupta, V., & Ivanov, D. (2020). Dual sourcing under supply disruption with risk-averse suppliers in the sharing economy. International Journal of Production Research, 58(1), 291–307. https://doi.org/10.1080/00207543.2019.1686189
- Hair, J. F., Black, W. C., Babin, B. J., & Anderson, R. E. (2010). Multivariate data analysis: A global perspective (7th ed.). Pearson Education, Inc.
- Haleem, F., Farooq, S., Wæhrens, B. V., & Boer, H. (2018). Offshoring experience and performance: The role of realized drivers and risk management. Supply Chain Management: An International Journal, 23(6), 531–544. https://doi.org/10.1108/SCM-02-2018-0074
- Haque, M., & Islam, R. (2013). Effects of supply chain management practices on customer satisfaction: Evidence from pharmaceutical industry of Bangladesh. Global Business & Management Research, 5(2/3), 120.
- Haque, M. Z., Islam, M. S., Deb, S. K., & Islam, M. R. (2022). Strategic value of Online Social Networks (OSNs) in supply chain networks during COVID-19. Cogent Business & Management, 9(1), 2148336. https://doi.org/10.1080/23311975.2022.2148336
- Hashemi, S. M., Handayanto, E., Masudin, I., Zulfikarijah, F., & Jihadi, M. (2022). The effect of supply chain integration, management commitment and supply chain challenges on non-profit organizations performance: Empirical evidence from Afghanistan. Cogent Business & Management, 9(1), 2143008. https://doi.org/10.1080/23311975.2022.2143008
- Hebbar, P. B., Sudha, A., Dsouza, V., Chilgod, L., & Amin, A. (2020). Healthcare delivery in India amid the COVID-19 pandemic: Challenges and opportunities. Indian Journal of Medical Ethics, 5(3), 215–218. https://doi.org/10.20529/IJME.2020.064
- Ho, W., Zheng, T., Yildiz, H., & Talluri, S. (2015). Supply chain risk management: a literature review. International Journal of Production Research, 53(16), 5031–5069. https://doi.org/10.1080/00207543.2015.1030467
- Iddris, F., Dogbe, C. S. K., & Kparl, E. M. (2022). Transformational leadership, employee self-efficacy, employee innovativeness, customer-centricity, and organizational competitiveness among insurance firms. International Journal of Innovation Science. https://doi.org/10.1108/IJIS-05-2022-0092
- Iqbal, M. J., Geer, M. I., & Dar, P. A. (2017). Medicines management in hospitals: A supply chain perspective. Systematic Reviews in Pharmacy, 8(1), 80. https://doi.org/10.5530/srp.2017.1.14
- Jiang, P., Klemeš, J. J., Fan, Y. V., Fu, X., & Bee, Y. M. (2021). More is not enough: A deeper understanding of the COVID-19 impacts on healthcare, energy and environment is crucial. International Journal of Environmental Research and Public Health, 18(2), 684. https://doi.org/10.3390/ijerph18020684
- Jifar, W. W., Geneti, G. B., & Dinssa, S. D. (2022). The impact of COVID-19 on pharmaceutical shortages and supply disruptions for non-communicable diseases among public hospitals of South West, Oromia, Ethiopia. Journal of Multidisciplinary Healthcare, 15, 1933–1943. https://doi.org/10.2147/JMDH.S377319
- Kaftan, V., Kandalov, W., Molodtsov, I., Sherstobitova, A., & Strielkowski, W. (2023). Socio-economic stability and sustainable development in the post-COVID era: Lessons for the business and economic leaders. Sustainability, 15(4), 2876. https://doi.org/10.3390/su15042876
- Kamalahmadi, M., Shekarian, M., & Mellat Parast, M. (2021). The impact of flexibility and redundancy on improving supply chain resilience to disruptions. International Journal of Production Research, 60(6), 1–29. https://doi.org/10.1080/00207543.2021.1883759
- Kanyoma, K. E., Khomba, J. K., Sankhulani, E. J., & Hanif, R. (2013). Sourcing strategy and supply chain risk management in the healthcare sector: A case study of malawi’s public healthcare delivery supply chain. Journal of Management & Strategy, 4(3), 16. https://doi.org/10.5430/jms.v4n3p16
- Kauppi, K., Longoni, A., Caniato, F., & Kuula, M. (2016). Managing country disruption risks and improving operational performance: Risk management along integrated supply chains. International Journal of Production Economics, 182, 484–495. https://doi.org/10.1016/j.ijpe.2016.10.006
- Kaye, A. D., Okeagu, C. N., Pham, A. D., Silva, R. A., Hurley, J. J., Arron, B. L., Sarfraz, N., Lee, H. N., Ghali, G. E., Gamble, J. W., Liu, H., Urman, R. D., & Cornett, E. M. (2021). Economic impact of COVID-19 pandemic on healthcare facilities and systems: International perspectives. Best Practice & Research Clinical Anaesthesiology, 35(3), 293–306. https://doi.org/10.1016/j.bpa.2020.11.009
- Khorasani, S. T., Cross, J., & Maghazei, O. (2020). Lean supply chain management in healthcare: A systematic review and meta-study. International Journal of Lean Six Sigma, 11(1), 1–34. https://doi.org/10.1108/IJLSS-07-2018-0069
- Macdonald, J. R., Zobel, C. W., Melnyk, S. A., & Griffis, S. E. (2018). Supply chain risk and resilience: Theory building through structured experiments and simulation. International Journal of Production Research, 56(12), 4337–4355. https://doi.org/10.1080/00207543.2017.1421787
- Manhart, P., Summers, J. K., & Blackhurst, J. (2020). A meta‐analytic review of supply chain risk management: Assessing buffering and bridging strategies and firm performance. The Journal of Supply Chain Management, 56(3), 66–87. https://doi.org/10.1111/jscm.12219
- Mawonde, D., Samuel, B., Nyoni, J., & Muzenda, A. C. (2023). The effect of supply chain resilient strategies on operational performance of humanitarian organisations in Zimbabwe during the coronavirus period. Cogent Business & Management, 10(2), 2246741. https://doi.org/10.1080/23311975.2023.2246741
- McShane, M. K., Nair, A., & Rustambekov, E. (2011). Does enterprise risk management increase firm value? Journal of Accounting, Auditing & Finance, 26(4), 641–658. https://doi.org/10.1177/0148558X11409160
- Nazam, M., Hashim, M., Ahmad Baig, S., Abrar, M., Ur Rehman, H., Nazim, M., Raza, A., & Tan, A. W. K. (2020). Categorizing the barriers in adopting sustainable supply chain initiatives: A way-forward towards business excellence. Cogent Business & Management, 7(1), 1825042. https://doi.org/10.1080/23311975.2020.1825042
- Ngoc, P. T. B., Huya, D. T. N., & Nhung, P. T. H. (2021). Healthcare policy for patients with chronic heart failures at Nam Dinh General hospital in Vietnam. Journal of Pharmaceutical Research International, 33(40B), 292–299. https://doi.org/10.9734/jpri/2021/v33i40B32290
- Ngoc, P. T. B., Huy, D. T. N., Binh, V. T., Nhung, P. T. H., & Hoang, N. H. (2021). Extra analysis of health care policy for patients with corona virus during COVID-19 and with chronic heart failures and roles of nurses at hospitals in Vietnam. Journal of Pharmaceutical Research International, 33(47), 358–368. https://doi.org/10.9734/jpri/2021/v33i47A33021
- Okereke, M., Ukor, N. A., Adebisi, Y. A., Ogunkola, I. O., Favour Iyagbaye, E., Adiela Owhor, G., & Lucero‐Prisno, D. E., III. (2021). Impact of COVID‐19 on access to healthcare in low‐and middle‐income countries: Current evidence and future recommendations. The International Journal of Health Planning and Management, 36(1), 13–17. https://doi.org/10.1002/hpm.3067
- Panova, Y., & Hilletofth, P. (2018). Managing supply chain risks and delays in construction project. Industrial Management & Data Systems, 118(7), 1413–1431. https://doi.org/10.1108/IMDS-09-2017-0422
- Pilbeam, C., Wilding, R., Wagner, B., Alvarez, G., & Wilson, H. (2012). The governance of supply networks: A systematic literature review. Supply Chain Management: An International Journal, 17(4), 358–376. https://doi.org/10.1108/13598541211246512
- Rasheed, R., Rizwan, A., Javed, H., Sharif, F., & Zaidi, A. (2021). Socio-economic and environmental impacts of COVID-19 pandemic in Pakistan—an integrated analysis. Environmental Science and Pollution Research, 28(16), 19926–19943. https://doi.org/10.1007/s11356-020-12070-7
- Richardson, R., Quinet, G., & Kitajima, U. (2021). Supply chain risk as a barrier to trade: A concise exploration. International Management Review, 17(2), 48–146.
- Senna, P., Reis, A. D. C., Leão Santos, I., & Dias, A. C. (2022). Healthcare supply chain risk management in Rio de Janeiro, Brazil: What is the current situation? Work, 72(2), 511–527. https://doi.org/10.3233/WOR-205216
- Senna, P., Reis, A., Santos, I. L., Dias, A. C., & Coelho, O. (2020). A systematic literature review on supply chain risk management: Is healthcare management a forsaken research field? Benchmarking: An International Journal, 28(3), 926–956. https://doi.org/10.1108/BIJ-05-2020-0266
- Shenoi, V. V., Dath, T. S. & Rajendran, C.(2021). Supply chain risk management in Indian manufacturing industries: an empirical study and a fuzzy approach. Supply Chain Management in Manufacturing and Service Systems: Advanced Analytics for Smarter Decisions. In S. Srinivas. (Ed.), Supply Chain Management in Manufacturing and Service Systems, International Series in Operations Research & Management Science (Vol. 304, pp. 107–145). Springer. https://doi.org/10.1007/978-3-030-69265-0_4
- Sibevei, A., Azar, A., Zandieh, M., Khalili, S. M., & Yazdani, M. (2022). Developing a risk reduction support system for health system in Iran: A case study in blood supply chain management. International Journal of Environmental Research and Public Health, 19(4), 2139. https://doi.org/10.3390/ijerph19042139
- Singh, A., & Parida, R. (2022). Decision-making models for healthcare supply chain disruptions: Review and insights for post-pandemic era. International Journal of Global Business and Competitiveness, 17(2), 130–141. https://doi.org/10.1007/s42943-021-00045-5
- Sodhi, M. S., Son, B. G., & Tang, C. S. (2012). Researchers’ perspectives on supply chain risk management. Production and Operations Management, 21(1), 1–13. https://doi.org/10.1111/j.1937-5956.2011.01251.x
- Sodhi, M. S., & Tang, C. S. (2021). Supply chain management for extreme conditions: Research opportunities. The Journal of Supply Chain Management, 57(1), 7–16. https://doi.org/10.1111/jscm.12255
- Sreedevi, R., & Saranga, H. (2017). Uncertainty and supply chain risk: The moderating role of supply chain flexibility in risk mitigation. International Journal of Production Economics, 193, 332–342. https://doi.org/10.1016/j.ijpe.2017.07.024
- Tang, O., & Musa, S. N. (2011). Identifying risk issues and research advancements in supply chain risk management. International Journal of Production Economics, 133(1), 25–34. https://doi.org/10.1016/j.ijpe.2010.06.013
- Vishnu, C. R., Sridharan, R., & Kumar, P. R. (2019). Supply chain risk management: Models and methodss. International Journal of Management & Decision Making, 18(1), 31–75. https://doi.org/10.1504/IJMDM.2019.096689
- Wiengarten, F., Humphreys, P., Gimenez, C., & McIvor, R. (2016). Risk, risk management practices, and the success of supply chain integration. International Journal of Production Economics, 171, 361–370. https://doi.org/10.1016/j.ijpe.2015.03.020
- Yu, Z., Razzaq, A., Rehman, A., Shah, A., Jameel, K., & Mor, R. S. (2021). Disruption in global supply chain and socio-economic shocks: A lesson from COVID-19 for sustainable production and consumption. Operations Management Research, 15(1–2), 1–16. https://doi.org/10.1007/s12063-021-00179-y