Abstract
Digital papillary adenocarcinoma (DPAca) is an aggressive lesion with high metastatic potential, which is easily misdiagnosed. We present a 55-year-old male with a cystic lesion on his right thumb. Above all else, lesions of the digits should be sent for histopathology routinely, regardless of their history or appearance.
A 55-year-old old male right-hand dominant truck driver was referred by his general practitioner for removal of a ‘cyst’ on the tip of his right thumb. It had been present for several years with no history of trauma or foreign body.
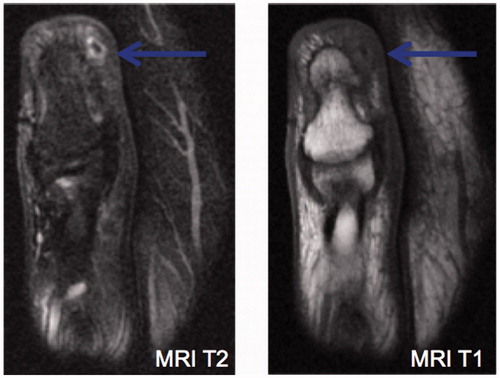
Plain radiographs did not have any worrying features. Given there was no history suggestive of a foreign body and location was atypical for a ganglion, an MRI with gadolinium was arranged for local staging of a suspected tumour. Ultrasonography was not used, as its reliability is operator dependent, it is less likely to delineate the nature of the lesion and does not demonstrate the tumour’s relationship with the surrounding anatomy. On MRI a 1 × 2 × 3 mm lesion with surrounding oedema and enhancement () was identified with no evidence of erosion of the terminal tuft. The MRI was reported as a “small retained foreign body and surrounding inflammatory change”. No clinical photos were taken prior to surgery reflecting the benign appearance of the lesion. An excisional biopsy was performed and intra-operatively the lesion was not dissimilar to a retained foreign body containing a thorn as per the MRI report. Despite its benign appearance it was sent for histopathology.
Figure 1. A subsequent MRI was reported as most likely a small foreign body with no evidence of erosion.
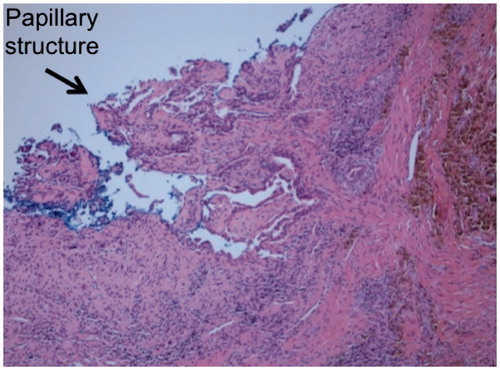
The histopathology unexpectedly demonstrated a Digital Papillary Adenocarcinoma (DPAca). The specimen showed tubular and papillary architecture with a peripheral zone of dense fibrosis (). It was focal S100 positive, CEA and HBME-1 negative. The tumour extended beyond the margins of the specimen.
With the benefit of hindsight and the knowledge of the unexpected pathology finding of DPAca, the senior author’s opinion is that this was never a foreign body, and was just mislabelled at the time of the MRI report. Although we acknowledge that foreign body-induced carcinogenesis is another potential pathway for cancer development and progression, accelerated by reactive oxygen species derived from inflammatory cells.
CT of the chest was unremarkable and no lymph nodes were palpable. A thumb amputation was performed at the level of the interphalangeal joint, to ensure a macroscopic margin of 10 mm. At 5 years post-amputation he has no evidence of local or regional reoccurrence nor distant metastatic disease.
DPAca is an extremely rare tumour of the sweat glands usually involving the distal end of the digits. It is most common in middle-aged men in their 5th or 6th decade of life with a 9:1 male to female ratio. It rarely if ever is diagnosed clinically and often misdiagnosed as a benign entity, thus highlighting how essential routine biopsy and histological examination is of lesions involving the digits.[Citation1] Initially these tumours were subcategorized into adenomas and aggressive adenocarcinomas based on their histological morphology (i.e. mitotic rate, atypical, local invasion, etc.) but this morphology did not reflect their biological behaviour and the distinction was abandoned in favour of Digital Papillary Adenocarcinoma.[Citation1]
On histopathological examination these lesions demonstrate multinodular solid and/or cystic architectural pattern, with papillary projections, tubular and ductal structures. Approximately half of lesions are well circumscribed.[Citation1,Citation2]
If left untreated without amputation or wide excision, the tumour has a rate of recurrence/distal spread approaching 50%. Metastasis is most common to lung and regional lymph nodes, respectively, and occurs in 14–20% of the patients.[Citation2,Citation3] Sentinel lymph node (SLN) biopsy for staging has been reported in 11 patients with two findings of positive nodes.[Citation2,Citation4] The benefit of SLN staging is not clear, given both the limited numbers and short-term follow-up of the cases which have been published, however, seems promising on a first principle basis. Mortality of DPAca is approximately 5% [Citation1,Citation3] allowing for wide variance in length of follow-up. Distant metastases have been poorly responsive to chemotherapy, but lymph node clearance and/or local lung resection appears to have some benefit again with limited numbers reported.[Citation2,Citation3]
DPAca is an aggressive lesion with high metastatic potential, which is easily misdiagnosed. Digit amputation is the gold standard of surgical management or at the very least wide local excision.[Citation1,Citation2] Clinical and radiological evaluation for regional lymph node and lung metastases needs to be carried out, possibly with the addition of a SLN biopsy at the time of excision.[Citation4] The patient should be followed-up for a minimum of 10 years. Above all else, lesions of the digits should be sent for histopathology routinely, regardless of their clinical or intraoperative appearance, to allow for the correct diagnosis of these rare tumours.
Disclosure statement
The authors alone are responsible for the content and writing of the paper. No funding was received for the present work. The authors have no financial or other conflicts of interest to disclose.
References
- Scolyer RA, Karim RZ, Thompson JF, et al. Digital papillary adenocarcinoma. Pathology. 2013;45:55–61.
- Suchak R, Wang W-L, Prieto VG, et al. Cutaneous digital papillary adenocarcinoma: a clinicopathologic study of 31 cases of a rare neoplasm with new observations. Am J Surg Pathol. 2012;36:1883–1891.
- Duke WH, Sherrod TT, Lupton GP. Aggressive digital papillary adenocarcinoma: aggressive digital papillary adenoma and adenocarcinoma revisited. Am J Surg Pathol. 2000;24:775.
- Kempton SJ, Navarrete AD, Salyapongse AN. Aggressive digital papillary adenocarcinoma: case report of a positive sentinel lymph node and discussion of utility of sentinel lymph node biopsy. Ann Plast Surg. 2015;75:34–36.