Abstract
Intravascular papillary endothelial hyperplasia is an uncommon benign vascular lesion characterized by a reactive proliferation of endothelial cells. The lesion of the finger often presents diagnostic challenges to surgeons because of its rarity. We report a case of intravascular papillary endothelial hyperplasia to facilitate the recognition of this uncommon lesion.
Introduction
Intravascular papillary endothelial hyperplasia (IPEH), also known as Masson’s tumor, is an uncommon benign vascular lesion characterized by a reactive proliferation of endothelial cells. The lesion arising from an ulcerated hemorrhoidal vein was first described by Masson [Citation1] as a ‘vegetant intravascular hemangioendothelioma’. Thereafter, it has been reported with diverse descriptions such as intravascular angiomatosis, intravenous vascular proliferation, Masson’s pseudoangiosarcoma, and Masson’s tumor. Masson believed that it was a specific type of hemangioma. However, Henschen [Citation2] proposed that the endothelial proliferation is reactive rather than neoplastic. The descriptive term ‘intravascular papillary endothelial hyperplasia’ was first proposed by Clerkin and Enzinger [Citation3].
IPEH usually presents as a well-defined, superficial papule or a deep nodule in the skin or subcutaneous tissue. It commonly occurs in the head, neck, and upper extremities in the third and fourth decades of life. Less frequently, it also occurs in the adrenal gland, heart, intestine, kidney, liver, lungs, popliteal artery, and superior vena cava. IPEH of the finger often poses a diagnostic challenge for hand surgeons because of its rarity and absence of characteristic clinical features. Herein, we report a case of IPEH manifesting as a cystic nodule in the finger to facilitate the recognition of this uncommon lesion. We also present other conditions to be included in the differential diagnosis of finger nodules through a comprehensive review of the relevant literature.
Case report
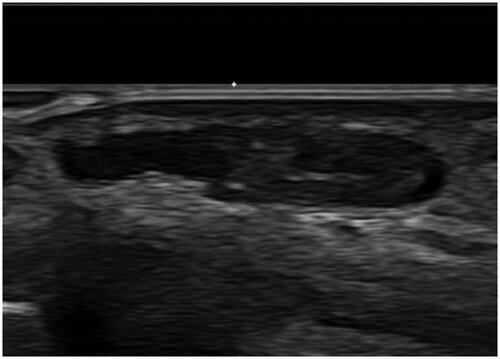
A 53-year-old woman presented with a small, asymptomatic, protruding mass on the volar surface of the proximal phalanx of the left index finger. She noticed the lesion 3 months prior to her visit to our clinic. She had no remarkable medical or trauma history. On clinical examination, the lesion revealed a subcutaneous cystic nodule with no discoloration of the overlying skin. It was non-tender and movable. Preoperative ultrasonography revealed a cystic lesion approximately 0.7 × 0.3 × 1.2 cm in size, with no remarkable increase in the vascularity. Ultrasonography was ultimately suggestive of a probable ganglion cyst ().
Figure 1. Preoperative ultrasonography reveals about 0.7 × 0.3 × 1.2 cm sized cystic lesion with no remarkable increased vascularity.
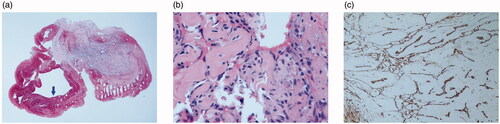
The lesion was excised under digital nerve block. It was located in the subcutaneous plane and easily dissected from the surrounding tissues. Intraoperatively, gross examination of the tumor showed a soft, red purple, and well-circumscribed cystic mass, which looked like a hemangioma (); however, remarkable feeding vessels were not observed while dissecting the lesion. Histologic examination revealed intravascular arborizing endothelial tissue with an organizing thrombus (). The vascular tissue showed intravascular endothelial cell proliferation with characteristic papillary hyaline cores (). On immunohistochemical analysis, the endothelial cells were positive for the endothelial markers CD31 and CD34 (). Based on these histopathological findings, the patient was diagnosed as having IPEH.
Figure 2. Intraoperative photograph shows a soft, red purple, and well-circumscribed cystic mass looking like a hemangioma at the volar surface of left 2nd proximal phalanx.

Figure 3. Histopathologic appearance of the lesion. (a) The specimen showed intravascular proliferative lesion with organizing thrombus (arrow) (H&E, ×15). (b) High magnification of papillary proliferations revealed fibrinous and hyaline stalks lined by endothelial cells (H&E, ×400). (c) These lining cells were positive for anti-CD31 (immunohistochemical stain, clone JC70, Cell Marque, ×100).
Discussion
IPEH is known to be a non-neoplastic reactive endothelial proliferation. These lesions account for approximately 2% of the vascular tumors of skin and soft tissue [Citation4]. Some of them present with tenderness or discoloration of the overlying skin. The lesions are usually solitary, but multiple lesions have occasionally been reported.
The pathogenesis of IPEH is poorly understood. Most evidence suggests that it is a reactive process that occurs in the setting of unusual thrombus organization. However, the order of disease progression remains controversial. Either endothelial proliferation is the primary process with secondary thrombus formation [Citation1] or the thrombus serves as a matrix for papillary proliferation [Citation5]. Several investigators have described that this reactive process could be related to an antecedent trauma history and the consecutively formed thrombus [Citation3]. Levere et al. proposed that IPEH could be initially triggered by the release of basic fibroblast growth factor (bFGF) from macrophages recruited to the area by minor trauma or irritation. This release of bFGF could stimulate the proliferation of endothelial cells, which in turn would secrete more bFGF, which would then set up a positive feedback loop causing a cascade of endothelial proliferation [Citation6].
Three types of IPEH are recognized [Citation7]. The primary, pure, or intravascular type (56%) occurs in dilated vascular spaces. The mass is usually a small subcutaneous lesion and occurs most commonly in the finger. The secondary or mixed type (40%) occurs in pre-existing vascular lesions such as hemangiomas, pyogenic granulomas, or vascular malformations. About half of the mixed type lesions were intramuscular. The extravascular type (4%) arises from a hematoma. The extravascular type lesions tend to be larger than the other types.
The characteristic histological feature of IPEH is the presence of papillary structures covered with hyperplastic endothelial cells within the vascular lumen. Besides the intra-luminal location of the lesion, other useful diagnostic features include an intimate association with the organizing thrombus, and the absence of necrosis, cellular pleomorphism, and mitotic activity. IPEH needs to be differentiated from angiosarcoma as the lesion may clinically and histologically be mistaken for a low grade angiosarcoma [Citation8]. A critical distinction between angiosarcoma and IPEH is that angiosarcomas are typically not present inside the lumen of blood vessels [Citation9]. Moreover, unlike angiosarcoma, the endothelial cells of IPEH lack necrosis, marked pleomorphism, significant mitotic activity, and solid sheet formation.
Apart from angiosarcoma, other conditions that can be included in the differential diagnosis of finger nodules are: giant cell tumor of the tendon sheath, digital mucous cyst/digital ganglion cyst/digital myxoid pseudocyst, glomus tumor, neurogenic tumor, dermatofibroma, rheumatoid nodules, subcutaneous sarcoidosis, vascular malformations, angioleiomyoma, Dabska tumor, Heberden Node, Bouchard node, and gouty tophus (). Ultrasonography, computed tomography and magnetic resonance imaging are often helpful in differentiating these subcutaneous nodules. However, confirmative diagnosis is usually made after microscopic examination.
Table 1. Differential diagnosis for subcutaneous finger nodules.
The preferred treatment of IPEH is marginal excision. Additional tissue removal is usually not required to prevent recurrence. Its prognosis is good because it does not transform to a malignant neoplasm and does not recur after proper management. However, a thorough understanding of this lesion is needed to differentiate it from angiosarcomas as well as other tumors causing finger nodules and to ensure proper management.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Masson P. Hemangioendothelioma vegetant intravasculaire. Bull Soc Anat. 1923;93:517–523.
- Henschen F. L'endovasculite proliferante thrombopoietique dans la lesion vasculaire locale. Ann Anat Patho. 1932;9:113–121.
- Clearkin K, Enzinger F. Intravascular papillary endothelial hyperplasia. Arch Pathol Lab Med. 1976;100:441–444.
- Tedla M, Bežová M, Biró C, et al. Intravascular papillary endothelial hyperplasia of larynx: case report and literature review of all head and neck cases. Otolaryngol Pol. 2014;68:200–203.
- Requena L, Sangueza OP. Cutaneous vascular proliferation. Part II. Hyperplasias and benign neoplasms. J Am Acad Dermatol. 1997;37:887–919.
- Levere SM, Barsky SH, Meals RA. Intravascular papillary endothelial hyperplasia:a neoplastic ‘actor’ representing an exaggerated attempt at recanalization mediated by basic fibroblast growth factor. J Hand Surg Am. 1994;19:559–564.
- Hashimto H, Daimaru Y, Enjoji M. Intravascular papillary endothelial hyperplasia a clinicopathologic study of 91 cases. Am J Dermatopathol. 1983;5:539–546.
- Barr RJ, Graham JH, Sherwin LA. Intravascular papillary endothelial hyperplasia. A Benign lesion mimicking angiosarcoma. Arch Dermatol. 1978;114:723–726.
- Kim DS, Ryu DJ, Oh SH, et al. Intravascular papillary endothelial hyperplasia simulating malignant melanoma. Acta Derm Venereol. 2010;90:220–221.
