Abstract
Trichilemmal cysts mainly occur in areas of dense hair follicle concentration. Locations include face, trunk, extremities and genitalia are less common. Prevalence and description of cases in the literature are rare in pediatric age. We report a pilar cyst removal from the upper lip with intraoral approach in an adolescent.
Introduction
There is a myriad of cutaneous and subcutaneous lumps and cysts therefore sometimes the clinical nomenclature is deceptive and the initial diagnosis may not be the same as the histological finding. Even the first describer of pilar cysts called them sebaceous cysts [Citation1]. Today they are distinct entities, but usually they cannot be distinguished from each other clinically [Citation2]. Trichilemmal (pilar) cysts are intradermal cysts and 90% are found on the scalp where hair follicles are abundant [Citation3]. Less common locations are face, trunk, extremities and rarely genitalia, groin, palms and fingertips [Citation4]. Cysts arising from deep hair follicles in the lip area can grow toward the mouth presenting oral lesions rather than skin lesions. The rarity of intraoral hairs accounts for the lack of reported cases of trichilemmal cysts in oral or perioral locations where its formation can be explained by the presence of ectopic hair follicles in some oral sites, especially the lips [Citation5–7].
Case
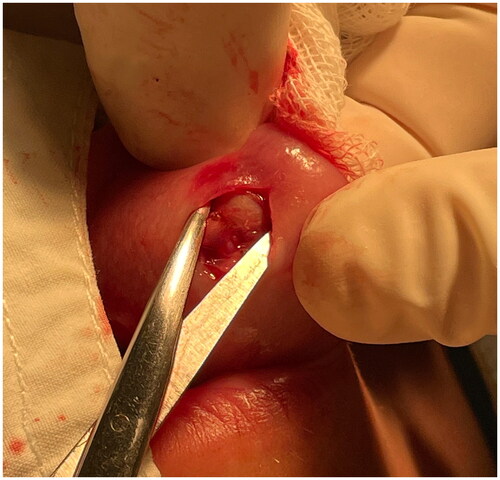
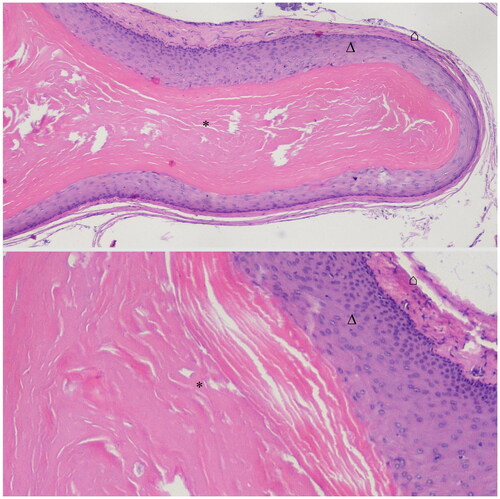
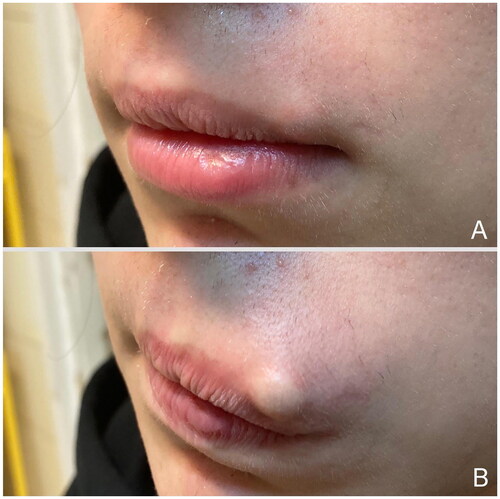
A healthy seventeen-year-old boy presented with a four-month-old history of a painless slow-growing subcutaneous mass on the left side of his upper lip close to the vermillion border () at the pediatric plastic surgery outpatient clinic. There were no injury, piercing, inflammation or any notable condition in the patient’s medical history and no similar nodules were detected on other parts of the body. By physical examination a mobile, moderately hard and round lump was found with no functional deficit. First impression was epidermoid cyst but there was no visible punctum and the localization was unusual as well. After consultation with the adolescent patient and his parent surgical removal was decided. For esthetic reasons the removal of the lesion was planned from intraoral approach. The operation was performed under regional and local anesthesia. On the left side infraorbital (Lidocaine 1% 1 ml) nerve block was given with additional local infiltration (Lidocaine-epinephrine 2% 2 ml) of the mucosal side of the upper lip. After vertical incision on the labial mucosa with blunt preparation a well-defined, round and light colored cyst was found (). It was removed as a whole with intact cyst wall. During preparation care was taken to preserve the integrity of the orbicular muscle and the superior labial artery. Wound closure was made with 4.0 absorbable sutures. Specimen was sent to histopathological examination. The histological finding was trichilemmal cyst. On the inner surface of the cyst wall trichilemmal keratinization was observed without granular layer. This keratinization pattern distinguishes epidermal cyst from trichilemmal cyst. The content of the cyst was keratin (). During the follow-ups - one week, two weeks, one month and three months after surgery – the recovery was uneventful. The esthetic result meets our expectations and the orbicular muscle function was also preserved ().
Figure 1. Preoperative pictures show a subcutaneous mass on the left side of the upper lip. (A) Appearance of the swelling at rest, and when the patient pushes it out with his tongue (B).
Discussion
Skin cysts can be classified based on cellular origin into the following major types: cysts with epithelial cells from outer root sheath of the hair follicle, cysts with epithelial cells from the sebaceous duct, cysts with epithelial cells from infundibulum or interfollicular epidermis, cysts with epithelial cells from sweat gland, cysts with epithelial cells from hair matrix and hamartomatous cysts [Citation8]. By definition, cyst is a closed sac that has two main features: a lining and contents that are liquid or semi-solid. In the differential diagnosis of facial cysts, and cyst-like nodular lesions the following are found: epidermoid cyst, dermoid cyst, pilomatrixoma, sebaceous cyst, neurofibroma, branchial cleft cyst, trichilemmal cyst, proliferating trichilemmal tumor, lipoma, abscess, nodulocystic acne, xanthogranuloma, mucocele, vellus hair cyst, steatocystoma, milia, comedo, apocrine hidrocystoma, histiocytoma and nodulocystic basal cell carcinoma. Although other rare tumors, metastases and vascular malformations can also show a clinical presentation suggestive of a skin cyst.
Trichilemmal cysts account for 20% of epithelial cysts and 80% are epidermal. Compared to epidermal cysts, the lesions of pilar cyst do not have an overlying punctum and tend to be more mobile. Pilar cysts are benign and tumor form is very rare, which is called proliferating trichilemmal cyst, and occurs in 3% of cases [Citation9, Citation10]. Trichilemmal cysts occur in less than 10% of the population. These lesions are usually seen in adults and are solitary in only 30% of patients. Usually, they are slow-growing nodules but sometimes they increase in size rapidly and might cause pain. Inflammation, cosmetic disfigurements, infection and calcification may also occur. They have no known racial predilection and are more often present in women than men [Citation11]. They contain keratin and its breakdown products and are lined by walls resembling the external root sheath of the hair. Earlier an autosomal dominant pattern of inheritance was proposed [Citation12]. The definitive treatment is surgical excision including the wall of the cysts to avoid the recurrence although when the cyst is inflamed surgical removal is not recommended [Citation13]. Histopathological examination is indispensable to make a definite diagnosis [Citation14]. In conclusion, cystic lesions of the skin often call for surgical intervention, regardless of precisely known etiology whether for cosmetic reasons or for evaluation of a neoplastic process. Different cellular origins contribute to diverse skin cysts formation. The exact origin of the lesion may not be clear based on the physical examination in many cases. It is worth keeping in mind the possibility of pilar cyst even in pediatric age and in unusual location. After an operation the subsequent appearance of the resulting scar is definitely important, especially if we also take into account that children are still growing and the psychosocial effects on them in the community is also significant. These are also worth considering when planning surgeries. As far as we know, pilar cyst removal from the lip with this technique in pediatric age group has not been reported before. The special features of our case are the adolescent patient and the removal method of the pilar cyst.
Ethical approval
Our work has an institutional (IRB/IEC) approval (KUT-12/2023). A copy of the approval form is available for review by the Editor of this journal.
Consent form
Written informed consent for publication of the clinical details and clinical images was obtained from the patient and the parent of the patient. A copy of the consent form is available for review by the Editor of this journal.
Author contributions
Drafting of the manuscript: Márió Mikóczi MD
ICMJE contribution form and authorship statement are attached as separate documents during submission.
Prior presentation information: We hereby state that the article has not been published and is not under consideration for publication elsewhere.
Acknowledgments
We thank Dr. Viktória Vass (Department of Pathology, Heim Pál National Pediatric Institute, Budapest, Hungary) for providing histological photographs.
Disclosure statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Additional information
Funding
References
- Pinkus H. “Sebaceous cysts” are trichilemmal cysts. Arch Dermatol. 1969;99(5):1–4. doi: 10.1001/archderm.1969.01610230036008.
- Requena L, Yus ES. Follicular hybrid cysts. Am J Dermatopathol. 1991;13(3):228–233. doi: 10.1097/00000372-199106000-00003.
- Liu M, Han H, Zheng Y, et al. Pilar cyst on the dorsum of hand: a case report and review of literature. Medicine. 2020;99(31):e21519. doi: 10.1097/MD.0000000000021519.
- Melikoglu C, Eren F, Keklik B, et al. Trichilemmal cyst of the third fingertip: a case report. Hand Surg. 2014;19(1):131–133. doi: 10.1142/S0218810414720113.
- Karaman E, Duman C, Yagiz C. Giant trichilemmal cyst at the neck region. J Craniofac Surg. 2009;20(3):961–962. doi: 10.1097/SCS.0b013e3181a2d85d.
- Abrahao AC, Daltoé PFP, Santos MVA, et al. A rare case of intraoral trichilemmal cyst. J Oral Diag. 2016;1(1):1–3.
- Perez LM, Bruce JW, Murrah VA. Trichilemmal cyst of the upper lip. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;84(1):58–60. doi: 10.1016/s1079-2104(97)90296-1.
- Qiu W, Gu PR, Chuong CM, et al. Skin cyst: a pathological dead-end with a new twist of morphogenetic potentials in organoid cultures. Front Cell Dev Biol. 2020;8:628114. doi: 10.3389/fcell.2020.628114.
- Maheshwari K, Hindocha S, Yousif A. Rare presentation of pilar cyst of the thumb. World J Plast Surg. 2019;8(2):259–261. doi: 10.29252/wjps.8.2.259.
- Al Aboud DM, Yarrarapu SNS, Patel BC. Pilar cyst. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; [cited 2022 Jan]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK534209/
- Varghese R, Yabit F, Alrifai A, et al. Pilar cysts of the head and neck: a case report. Cureus. 2022;14(4):e23932. doi: 10.7759/cureus.23932.
- Leppard BJ, Sanderson KV, Wells RS. Hereditary trichilemmal cysts. Hereditary pilar cysts. Clin Exp Dermatol. 1977;2(1):23–32. doi: 10.1111/j.1365-2230.1977.tb01533.x.
- Weir CB, St.Hilaire NJ. Epidermal inclusion cyst. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; [cited 2022 Jan]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532310/
- Chandrasekaran V, Parkash S, Raghuveer CV. Epidermal cysts–a clinicopathological and biochemical study. Postgrad Med J. 1980;56(662):823–827. doi: 10.1136/pgmj.56.662.823.