Abstract
Objective To report a case of severe supragastric belching and review the literature. Methods A clinical case report and PubMed search of supragastric belching. Results In literature, treatment options have so far not been encouraging. In this report, we can present one patient with severe supragastric belching being cured by therapy of speech and language pathologist. Conclusion To the best of our knowledge, we report the first Swedish severe case of supragastric belching to be cured by a speech and language pathologist.
Introduction
Frequent belching for a long time can be disabling and cause social isolation. If it is the only symptom, the diagnosis is likely to be ‘supragastric belching’, which is a behavioral disorder. Air is either pulled down into the esophagus by a contraction of the diaphragm, or injected by movements in the throat muscles, and then quickly expelled before it reaches the stomach. The diagnosis is primarily clinical, but may be verified by impedance measurements of the oesophagus, which shows a particular pattern.[Citation1] The condition was described in a recent review article,[Citation2] as an acquired behaviour, difficult to treat. No drug has been shown to be effective, but for a short case report on successful treatment with a combination of pregabalin and baclofen.[Citation3]
Case report
A middle-aged healthy male vegetarian from the Middle East suddenly started to suffer from excessive belching in the summer of 2012. As his problems increased, in the fall he was referred from the health centre to the local surgeon for gastroscopy, which was normal. The surgeon also ordered high resolution manometry of the oesophagus, 24-h pH measurement and impedance registration. All surveys were interpreted as normal except for a slight reflux, which was completely acid inhibited after treatment with esomeprazole. The patient was told ‘not to worry’, as his symptoms were considered to be functional. He started to eliminate dairy products, because lactose intolerance was found, but that did not affect his belching problem.
When we met him in February 2013, he had lost 5 kg in weight, because he avoided eating, as he perceived it as he then gulped air. The belching ceased when he went to bed at night. The normally very active man also avoided to run, and to climb the stairs, as problems then were accentuated. His whole social life was affected; he isolated himself, failed to apply for a job and even shunned his family. Our examination with video-laryngoscopy showed normal anatomy and normal swallowing ability, but the oesophagus opened up constantly in involuntary belching.
Encouraged by a pilot study, which showed promising results [Citation4] one of us, the speech and language pathologist, started therapeutic sessions. Speech therapy focused to create awareness of the mechanism of belching, to describe the behaviour causing the injection or suction of air, and to work with contrasting ad- and abduction on the level of glottis including conventional breathing and vocal exercises. Through distraction and shifted focus, attention changed from belching to periods of dense glottal- and oral closure. The aim was to give the patient knowledge that his belching was a learned behaviour, which could be modified and diminished. He was treated for 1 h, on five occasions, 1 week apart. At the first and the last therapy session, audio recordings were made, when he read aloud a standard text of 100 words, and self-assessments were made using a visual analogue scale (VAS) of symptom frequency and intensity, and also of his mental well-being. In the first audio recording, he had 46 belchings, in 26 episodes, which varied in frequency and intensity ( and ). At the last therapy session this had been reduced to two discrete belchings (). On the VAS, he initially estimated belchings to be very frequent, very intense and loud to become isolated, weak and quiet at the last treatment session. Regarding the question about his mental well-being he scored from very bad initially, to become very good in the end. He also described that he came out of his social isolation, started work out at the gym, to powerwalk and was actively job seeking.
Figure 1. The audio spectrogram. The audio spectrogram at the first therapy session, when our patient read a standard text of 100 words.
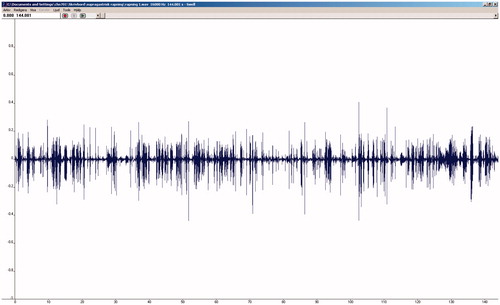
Figure 2. Belching before treatment. Before treatment, 46 separate belchings occured, when our patient read a standard text of 100 words, during 2 min 26 s.
Figure 3. Belching after 4 weeks of treatment. After treatment, he had 2 minor belchings when he read the same text, during 1 min 20 s.

Two years after our initial contact, he came on a follow-up exam. He had no belching problems any more, and was emotionally and physically well. He felt that he still had a tendency to belch, when he was running or climbing the stairs, but he could control this with techniques that he had learned in therapy. Video-laryngoscopy at rest, and during ergometer cycling for 10 min, was completely normal.
Discussion
Supragastric belching is unusual, so symptoms can easily be mistaken for other conditions, and it has attracted attention only in recent years.[Citation2] No drug has been shown to be long-term effective. Blondeau et al. showed in a study with Baclofen that the frequency of belching decreased, but only 2 of the 12 patients in the study had belching as the predominant symptom.[Citation5] More studies need to be done on the effect, and also of the long-term effects of Baclofen, which is known to have many central side effects.[Citation6]
A study of 21 patients with supragastric belching showed impaired social functioning, mental health, vitality, and general health as measured by the SF-36.[Citation7] Although our patient was suffering from the condition, our health care system seemed to treat it as functional and unaddressed. We show that supragastric belching can be diagnosed with video-laryngoscopy during a clinical examination by a team consisting of an ENT physician and a speech and language pathologist. Therapy can be successful. It gave our patient improved quality of life and ability to have a functional everyday life. The results are in line with those reported in a study of 11 patients, who received speech therapy, but only were evaluated by patient VAS scores.[Citation4]
Our objective measurement of the belchings when he read a standard text was also part of the treatment, to show him progress. After treatment, the belchings were much reduced, which made it much easier for him to read, so he could finish the text much quicker.
This case report demonstrates that treatment by a speech and language pathologist can improve mental and physical health of these patients.
Summary
Excessive belching without other symptoms is likely to be supragastric.
The diagnosis can be verified by patient history, and impedance measurement of the oesophagus followed by video-laryngoscopy.
Supragastric belching is a behavioural disorder.
Treatment by a speech and language pathologist can be successful.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
References
- Bredenoord AJ, Weusten BL, Sifrim D, et al. Aerophagia, gastric, and supragastric belching: a study using intraluminal electrical impedance monitoring. Gut. 2004;53:1561–1565.
- Bredenoord AJ. Management of belching, hiccups, and aerophagia. Clin Gastroenterol Hepatol. 2013;11:6–12.
- Kunte H, Kronenberg G, Fink K, et al. Successful treatment of excessive supragastric belching by combination of pregabalin and baclofen. Psychiatry Clin Neurosci. 2015;69:124–125.
- Hemmink GJ, Ten Cate L, Bredenoord AJ, et al. Speech therapy in patients with excessive supragastric belching – a pilot study. Neurogastroenterol Motil. 2010;22:24–28.
- Blondeau K, Boecxstaens V, Rommel N, et al. Baclofen improves symptoms and reduces postprandial flow events in patients with rumination and supragastric belching. Clin Gastroenterol Hepatol. 2012;10:379–384.
- Kessing BF, Bredenoord AJ, Smout AJ. The pathophysiology, diagnosis and treatment of excessive belching symptoms. Am J Gastroenterol. 2014;109:1196–1203; (Quiz) 204.
- Bredenoord AJ, Smout AJ. Impaired health-related quality of life in patients with excessive supragastric belching. Eur J Gastroenterol Hepatol. 2010;22:1420–1423.
