Abstract
With less than 40 cases in the English literature, liposarcomas of the upper aerodigestive tract are extremely rare. We present the first Scandinavian case: a 72-year-old male with progressive dysphagia and dysphonia. Tumour was located in the left aryepiglottic fold, 4–5 mm with normal epithelium. Tumour was excised macroscopically radical and histology showed myxoid liposarcoma, grade I. The patient received adjuvant radiotherapy. The gold standard is core needle or excisional biopsy. Main treatment remains surgery and the use of adjuvant radiotherapy is debatable. Liposarcomas have a high rate of recurrence and a tendency of de-differentiation over time; therefore, long-term follow-up is recommended. The diagnosis can only be made histologically and preferably with FISH probes.
Background
Liposarcomas are classified by their histopathological appearance with 5 subtypes; well-differentiated, myxoid, round-cell, dedifferentiated and pleomorphic.[Citation1] The well-differentiated and myxoid subtypes are the most common.[Citation2–4]
Liposarcomas accounts for less than 1% of all malignant tumours. The primary locations are extremities and retroperitoneum and 5% of the tumours are located in the head and neck region.[Citation1] Liposarcomas of the upper aerodigestive tract are extremely rare with less than 40 cases reported to date in the English literature.[Citation2,Citation3]
These tumours show male predominance 7:1,[Citation3] 24:3.[Citation4] The mean age at the time of diagnosis is 55 years and about half of the cases have recurrences.[Citation3,Citation4]
As with other tumours of the upper aerodigestive tract the most common symptoms are dysphonia and dysphagia.[Citation4,Citation5] Some tumours have been reported asymptomatic, and therefore, may result in tumours of substantial size at the time of diagnosis. The neoplasm demonstrates de-differentiation, from one subtype to another, over time. The 5-year survival rate is relatively high, although varying between subtypes: well-differentiated 85–100%, myxoid 77–95%, pleomorphic 21–45% and around 30% for de-differentiated.[Citation3]
The pathogenesis is believed to be associated with either translocation t(12;16)(q13;p11.2) or abnormalities of 1q and 12q13, which encodes the DDIT3 gene (formerly CHOP) which is necessary for adipocyte differentiation.[Citation6,Citation7]
Although a rare neoplasm with a relative high 5-year survival rate, the size (resulting in post-operative morbidity), recurrence rate and de-differentiation over time makes this a relevant subject.
Case presentation
We present the case of a 72-year-old male who was referred to gastroscopy due to progressive dysphagia and dysphonia over six months. Gastroscopy revealed inflammation of the ventricle and duodenum. Also, a tumour with normal epithelium was found in the supraglottic larynx and the patient was referred to the Department of Otolaryngology, Copenhagen University Hospital, Køge. The patient had been seen in 2003 due to a cyst-like lesion in the left aryepiglottic fold. The lesion was left intact and the patient was asymptomatic for 12 years.
The patient smoked 30 pipes and drank 4 units of alcohol per day at the time of diagnosis.
The lesion was seen during flexible rhino-laryngoscopy and was located in the left aryepiglottic fold, 4–5 mm in diameter, normal epithelium. The true vocal cords were mobile and the rest of the examination was normal. Excisional biopsy was performed during general anaesthesia. The epithelium was opened and a soft, cystic tumour with gelatinous material was excised. The tumour was fragmented and removed macroscopically radical.
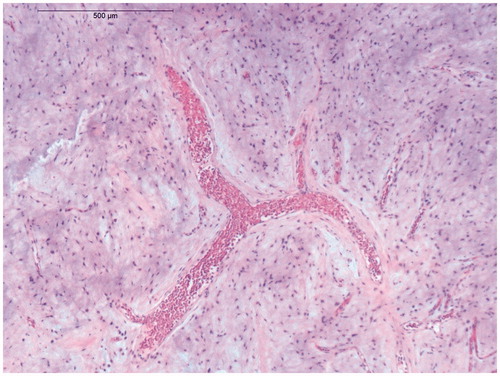
The histology showed a myxoid tumour of low cellularity and spindle-shaped stromal cells without significant pleomorphism (Figure ). There were scattered lipocytes, sometimes in small clusters, but no multivacuolated lipoblasts. There was an arborizing capillary network. The morphology was considered to be compatible with a myxoid liposarcoma, grade I. This was supported by the finding of rearrangement of the DDIT3 gene, by fluorescence in situ hybridization, in 22% of the tumour cells.
Figure 1. Micrograph demonstrating the delicate branching capillary network which is characteristic of myxoid liposarcoma (hematoxylin-eosin stain).
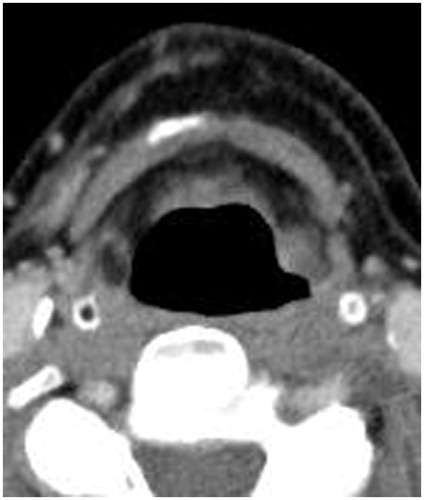
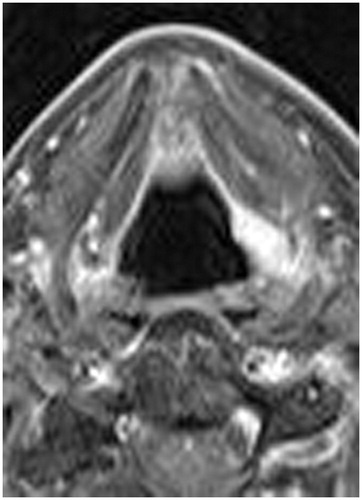
Post-operative CT and MRI scans (Figures and ) with intravenous contrast showed a 10 × 7 × 5 mm lesion in left aryepiglottic fold, representing previous tumour location, no residual tumour or signs of metastasis.
The patient was referred to the Department of Otolaryngology, Copenhagen University Hospital, Copenhagen for further treatment. Histology could not confirm microscopically radical excision, this uncertainty and knowing the subtype contributed to deciding on adjuvant radiotherapy, which was initiated two months post-operative. 2 Gy ×32.
Discussion
The diagnosis is difficult and often delayed due to the slow and sometimes asymptomatic course of this neoplasm. The gold standard when diagnosing remains core needle or excisional biopsy. The diagnosis is often not suspected until histological examination for example from an excisional biopsy. Surgical excision is considered the main treatment for liposarcomas. The per-operative aim is tumour-free margins, no consensus has been reached regarding margins; some recommend up to 2 cm.[Citation7,Citation8]
There is no consensus whether to use adjuvant radiotherapy. It has shown higher survival rates and local control rates. In a review by Spiro et al. highest control rate was achieved with dose >64 Gy and when using an intraoperative electron beam.[Citation8] The myxoid subtype may be more susceptible to radiotherapy.[Citation3,Citation4]
In this case, no adjuvant chemotherapy was given, as most previous authors on the subject agree is not beneficial for survival or rate of recurrence.
In a review by Mandell et al.,[Citation4] 50% of patients had recurrences. Average time after primary surgery was 3.9 years. It is also noted that in 18 (94.7%) of 19 recurrences, the primary surgery had been an excisional biopsy, either endoscopically or by external approach. To our knowledge, no occurrence of cervical metastasis has been reported, but a few distant metastases, to the lung, bone and skin.[Citation4] There is, therefore, no indication of neck dissection.
Post-operative morbidity depends on the use of adjuvant radiotherapy and size of the tumour. Larger tumours result in a greater per-operative risk of complications and larger post-operative craters and hence higher morbidity.
Conclusions
Although a very rare neoplasm of the upper aerodigestive tract, liposarcomas must be differentiated from other mesenchymal tumours and lipomas of the upper aerodigestive tract. This is important because these neoplasms have a high rate of recurrence and few observed cases of distant metastasis. We recommend a long-term follow-up due to the risk of recurrence, which has been observed up to 23 years after primary surgery.[Citation9]
Surgery is the primary treatment modality and there is a relatively high 5-year survival rate, with or without adjuvant radiotherapy. Diagnosis can only be made histologically and preferably supported by the use of FISH probes.
Consent
Written informed consent was obtained from the patient for publication of this Case Report and any accompanying images.
Notes on contributors
Alexander Nygren, MD, 1st year resident at Copenhagen University Hospital.
Frans Rømeling, physician, associate professor at Copenhagen University Hospital.
Acknowledgements
Bo Hainau, Department of Pathology, Copenhagen University Hospital, Køge, Denmark.
Disclosure statement
We have no conflict of interest.
References
- Enzinger FM, Weiss SW. Soft tissue tumors. In: DeFransesco K, editor. Philadelphia (PA): Elsevier; 1995. p. 1176.
- Han Y, Yang LH, Liu TT, et al. Liposarcoma of the larynx: report of a case and review of literature. Int J Clin Exp Pathol. 2015;8:1068–1072.
- Powitzky R, Powitzky ES, Garcia R. Liposarcoma of the larynx. Ann Otol Rhinol Laryngol. 2007;116:418–424.
- Mandell DL, Brandwein MS, Woo P, et al. Upper aerodigestive tract liposarcoma: report on four cases and literature review. Laryngoscope. 1999;109:1245–1252.
- Wenig BM, Heffner DK. Liposarcomas of the larynx and hypopharynx: a clinicopathologic study of eight new cases and a review of the literature. Laryngoscope. 1995;105:747–756.
- Muddaiah A, Zaffarullah W, Tewary A. Recurrent well-differentiated liposarcoma of the larynx: a case report and review of literature. Eur Arch Otorhinolaryngol. 2010;267:1163–1165.
- Gleinser DM, Font JP, Clement CG, et al. Primary myxoid liposarcoma of the supraglottic larynx. Rare Tumors. 2010;2:e41.
- Spiro IJ, Gebhardt MC, Jennings LC, et al. Prognostic factors for local control of sarcomas of the soft tissues managed by radiation and surgery. Semin Oncol. 1997;24:540–546.
- McCormick D, Mentzel T, Beham A, et al. Dedifferentiated liposarcoma. Clinicopathologic analysis of 32 cases suggesting a better prognostic subgroup among pleomorphic sarcomas. Am J Surg Pathol. 1994;18:1213–1223.