Abstract
A 60-year-old gentleman presented with dyspnoea, hoarse voice and stridor. He had no history suggestive of airway instrumentation or prior laryngeal pathology. Bedside flexible nasopharyngolaryngoscope revealed grossly oedematous bilateral false vocal cord. Computerized tomography scan of the neck with contrast showed rim-enhancing lesions at the paraglottic space and bilateral false vocal cord. A presumptive diagnosis of isolated paraglottic abscess was made. Patient was subjected to tracheostomy, then endoscopic assessment of the larynx. Pus was drained and parenteral antibiotics were commenced. Further assessment revealed improving false vocal cords oedema but right vocal cord palsy was documented. Patient was subsequently discharged well and tracheostomy was successfully decannulated once vocal cords and voice returned to normal.
Although occurrence of isolated abscess in the paraglottic region is rare, this disease entity should be considered as a differential diagnosis in the presentation of upper airway obstruction with no prior laryngeal pathology or airway instrumentation.
Background
Laryngeal abscess occurs typically secondary to systemic illnesses but has changed in recent time due to malignancy or trauma from airway instrumentation. Common aetiology is due to disease process in the larynx per se.[Citation1,Citation2] However, isolated abscess in the paraglottic region is rare.
There are a few case reports of paraglottic lesions secondary to malignancy or infection in aetiology.[Citation2–4] To the best of our knowledge, paraglottic lesions are manifestation of underlying carcinoma of larynx or hypopharynx and extension of cervical abscess.[Citation2,Citation5] Here, we would like to highlight the occurrence of an isolated abscess in the paraglottic space complicated with vocal cord palsy. Current literature on the subject is reviewed and discussed. We seek to characterize the presentation and treatment in hope for better understanding and treatment of this isolated lesion.
Case report
A 60-year-old gentleman presented to the emergency department with history of gradual onset of dyspnoea for four days. This was associated with dysphagia for liquids and solids, hoarse voice and stridor. He denied any history of neck swelling, fever or nasal symptoms. He is a smoker for 45 years and has pre-morbid diabetes mellitus for the past 5 years. Examination revealed a tachypnoeic patient with hoarse voice and audible inspiratory stridor. The neck was soft with no palpable swelling and the laryngeal crepitus was present. Oral cavity and oropharyngeal examinations were unremarkable. Bedside flexible nasopharyngolaryngoscope revealed grossly oedematous bilateral false vocal cord with a small glottic gap seen posteriorly. The true vocal cords were not visualized and there were no other abnormalities noted.
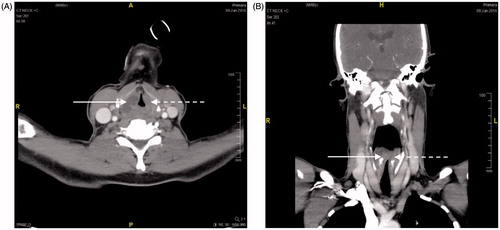
The patient was given intravenous steroid and adrenaline nebulizer, which improved his symptoms transiently. This prompted us for an imaging investigation. A computerized tomography scan of the neck with contrast revealed well-defined hypodense focus with rim enhancement seen at the right false vocal cord and paraglottic space measuring 2.2 (anterior–posterior) × 1.8 (width) × 2.4 (height) cm. A similar lesion was seen at the left false vocal cord at the same level measuring 1.3 (anterior–posterior) × 0.5 (width) × 0.9 (height) cm (Figure ).
Figure 1. Axial and coronal cut sections of bilateral false vocal cords hypodense rim enhancing lesions: right false vocal cord 2.2 (anterior–posterior) × 1.8 (width) × 2.4 (height) cm (in solid arrow) and left false vocal cord 1.3 (anterior–posterior) × 0.5 (width) × 0.9 (height) cm (in broken arrow).
His blood parameters revealed leukocytosis of 18,100 cells/mm3 and the random blood sugar was 12 mmol/L.
After discussion with the anaesthetist colleague, a decision was made for tracheostomy under local anaesthesia in view of upper airway obstruction and anticipated difficult intubation. Once airway was established, we proceeded with a direct laryngoscope and endoscopic evaluation of the larynx. Intra-operative findings revealed severe bilateral false vocal cord oedema with no visible mass. Aspiration from the right false vocal cord yield pus and was subsequently drained. Aspiration from the left side was nil. Nasogastric tube was inserted for feeding.
Our patient was started on parenteral antibiotics of ceftriaxone and metronidazole. Empirical dose of steroid was withheld once airway was established. His diabetic control was monitored in the ward and he begun to show significant improvement within two days of treatment commencement.
Pus aspiration from the right false vocal cord cultured Klebsiella pneumoniae and was sensitive to the administered antibiotics. Infective screening was negative for human immunodeficiency virus (HIV), syphilis, hepatitis B and C. Serial repeat flexible scopes revealed improving false vocal cords fullness and airway patency, however right vocal cord palsy was documented. Nasogastric tube was removed on day seven and the patient was tolerating orally well with no symptoms of aspiration.
Patient was discharged well after 14 days of parenteral antibiotics with a smaller size tracheostomy tube. Flexible scope upon discharge revealed residual right false cord oedema with right vocal cord palsy.
Upon subsequent follow-up, a repeated flexible scope revealed a completely resolved false vocal cords oedema and normal bilateral vocal cord. The tracheostomy tube was successfully decannulated. Patient recovered well and his voice was back to normal.
Discussion
The paraglottic region is a potential space present on either side of glottis. This region of adipose tissue, containing blood vessels and nerves, immediately adjacent to the thyroid lamina, was originally defined by Tucker and Smith (1962).[Citation6] It is bounded by the mucosa covering the lamina of thyroid cartilage laterally, the conus elasticus and quadrangular membranes medially and the anterior reflection of the pyriform fossa mucosa posteriorly.
A precise knowledge of the topography of the paraglottic space can explain typical symptoms of extension and compression of the concerned pathology. Isolated lesion in this laryngeal space is extremely rare and is usually associated with spread of carcinoma of larynx.[Citation3] Involvement of the paraglottic space with an infectious process is also rare and may result as an extension of a supraglottic infection or cervical abscess.[Citation1,Citation4,Citation5]
The present case is an extremely interesting one as the presentation of dyspnea, hoarseness, odynophagia and stridor was due to a pathology in a single space in the larynx, i.e. the paraglottic space. There was no suspicious evidence to suggest the localized paraglottic abscess was secondary from a laryngeal inflammation, laryngeal malignancy or extension of a cervical space infection.
A bedside flexible scope is often sufficient to establish early suspicion of this condition and it also aids to assess the degree of airway compromise.
The ideal imaging modality used to establish the diagnosis is a subject to debate.[Citation7,Citation8] Literature search revealed that an early computerized tomography is not only cost efficient but also time saving to prevent fatal airway compromise. It provides reliable assessment of laryngeal anatomy and neck spaces with image artefacts are unhampered from deglutition and respiration movements. With axial and coronal reconstruction, the site of involvement can be located for early intervention.
Like any infections, the immunocompromised individuals are more susceptible. In our patient, his pre-morbid diabetes mellitus established a higher risk of morbidity for his presentation.
Besides direct laryngoscope and endoscopic evaluation of the larynx prior to drainage, lateral thyrotomy approach of the paraglottic space disease has been described in literature.[Citation9] This provides direct visualization with minimal disruption of the laryngeal architecture. However, the drawback of scar and surgical site infection limits this method. Hence direct visualization with endoscope guidance provides a relatively safe and better option.
Isolation of gram-positive, gram-negative and anaerobes has been reported suggesting a polymicrobial infection.[Citation2–4] Therefore, targeted antimicrobial therapy as per culture and sensitivity provides a good control of infection.
Complications of paraglottic space abscess have a grave prognosis. Case report of extending cervical necrotizing with mediastinitis serves as a reminder to be on the lookout for further airway and complication of infection.[Citation10]
To the best of our knowledge, there is no literature search which revealed vocal cord palsy due to paraglottic space abscess. Therefore, we wish to highlight this rare occurrence, which we attributed to either from localized oedema with mass effect or spasm on the intrinsic muscles of the laryngeal framework of the secondary to paraglottic space infection.
Early diagnosis does not only prevent morbidity, but a good outcome is possible with successful resolution of symptoms.
Conclusion
The occurrence of isolated paraglottic abscess is a learning experience to us. The presentation of paraglottic space pathology invariably compromises the airway due to its topography. Suspicion of malignancy or extension of cervical infection has to be excluded in which an early computerized tomography is sufficient to confirm the diagnosis. Examination under anaesthesia will aid to better understand the causative aetiology and permits any surgical intervention. Vocal paresis which occurred was attributed to localized oedema with mass effect or spasm on the intrinsic muscles of the laryngeal framework of the secondary to paraglottic space infection. Prolonged parenteral antibiotic with serial bedside evaluation is warranted to prevent morbidity and complications.
Acknowledgements
None.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
Funding
None.
References
- Marston AP, Lalich IJ, Dearking AC, et al. Supraglottic laryngeal abscess of idiopathic etiology secondary to community-acquired, methicillin-resistant staphylococcus aureus. Otolaryngol Head Neck Surg. 2013;149:P212.
- Fernández Pérez A, Fernández-Nogueras Jiménez F, Moreno León JA. [Paraglottic laryngeal abscesses]. Acta Otorrinolaringol Esp. 2002;53:435–438.
- Sethi A, Sareen D, Mrig S, et al. Extensive gas-forming infection of the deep neck and laryngeal spaces. Braz J Oral Sci. 2005;4:745–748.
- Healy GB, Hyams VJ, Tucker GF. Paraglottic laryngitis in association with epiglottitis. Ann Otol Rhinol Laryngol. 1985;94:618–621.
- Lam KH, Wong J. The preepiglottic and paraglottic spaces in relation to spread of carcinoma of the larynx. Am J Otolaryngol. 1983;4:81–91.
- Reidenbach MM. The paraglottic space and transglottic cancer: anatomical considerations. Clin Anat. 1996;9:244–251.
- Zinreich SJ. Imaging in laryngeal cancer: computed tomography, magnetic resonance imaging, positron emission tomography. Otolaryngol Clin North Am. 2002;35:971–991.
- Jain SN, Varma R. Imaging in laryngeal tumors. AIJOC Jaypee Journals; 2010.
- Sun X, Wang W. Lateral thyrotomy approach on the paraglottic space disease. Lin Chuang Er Bi Yan Hou Ke Za Zhi. 2003;17:720–721. [Article in Chinese]
- Thomas AJ, Mong S, Golub JS, et al. Klebsiella pneumoniae cervical necrotizing fasciitis originating as an abscess. Am J Otolaryngol. 2012;33:764–766.
