Abstract
Benign lymphoepithelial cysts (LECs) are rare lesions that can be found in the lateral neck or in the parotid glands. A 52-year-old woman presented to our clinic with a slowly growing mass of the left malar region. MRI was obtained showing a cystic lesion lying between the mandibular ramus medially, the masseter muscle laterally and the parotid gland posteriorly. The lesion was surgically removed. Complete resection of the cystic lesion was done with preservation of the facial nerve. Histopathology study confirmed the diagnosis of lymphoepithelial cyst. No recurrence was found at 6 months follow up. To our knowledge, it is the first reported case of an intra-masseteric lymphoepithelial cyst. Surgical removal of deep facial lesions can be very delicate and tedious especially when preservation of facial nerve is a priority.
Introduction
Benign lymphoepithelial cysts (LECs) are rare, benign, slowly growing uniloculated or multiloculated lesions that commonly occur in the head and neck region.[Citation1] These dysontogenetic lesions are usually found in the lateral neck but can also be located in the salivary glands, mostly in the parotids. Depending on their location, LECs are thought to originate either from remnants of branchial cleft epithelium in the lateral neck or from epithelial remnants within the retained lymphoid tissue of the parotid gland.[Citation2,Citation3]
Case report
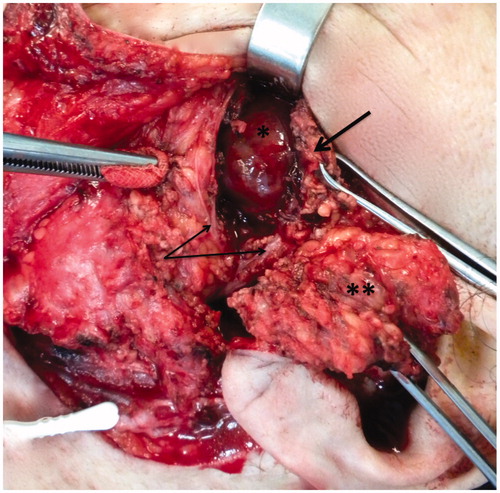
A 52-year-old Caucasian woman presented to our clinic with a 2-year history of recurrent swelling of the left cheek causing significant discomfort and cosmetic impairment. The patient’s past medical history was inconsistent. She was an occasional smoker and denied ethanol abuse. Her family history was negative for head and neck tumors and other disorders. Physical exam showed a 2 × 2 cm, firm, non-tender, mobile mass arising in the cheek area and right underneath the zygomatic arch. No inflammation, fluctuance or drainage was noted and the facial nerve was intact. No palpable cervical lymph nodes were noted and the rest of the head and neck as well as the general exam were unremarkable. Fine needle aspiration cytology of the lesion was inconclusive yet showed no signs of malignancy. In order to further characterize the lesion, a contrast-enhanced MRI of the parotid glands was obtained (Figures , and ). The MRI showed a well-circumscribed uniloculated cystic lesion of 21 × 20 × 17 mm located in the deep aspect of the left masseter muscle in its posterior–superior part, hypointense on T1-weighted images (WI), with thin rim enhancement after gadolinium injection (Figure ) and hyperintense on T2-WI (Figures and ). The lesion was lying between the mandibular ramus medially, at the level of the mandibular notch, the masseter muscle laterally and the parotid gland posteriorly, with no signs of infiltration. No similar findings were noted on the contralateral side. The patient underwent surgery through a superficial parotidectomy approach with facial nerve dissection and preservation, which allowed delivery of the cystic lesion between the zygomatic and buccal branches of the facial nerve and through the masseter muscle (Figure ). Pathology revealed a cystic lining consistent with squamous epithelium along with abundant lymphoid tissue containing clusters of cholesterol crystals, thus confirming the diagnosis of benign LEC. Interestingly, the cyst was surrounded by salivary glandular tissue.
Figure 1. Axial T1-WI with fat saturation showing a well-circumscribed hypointense lesion located in the posterior part of the left masseter muscle, anterior to the parotid gland, with thin rim enhancement after contrast injection.
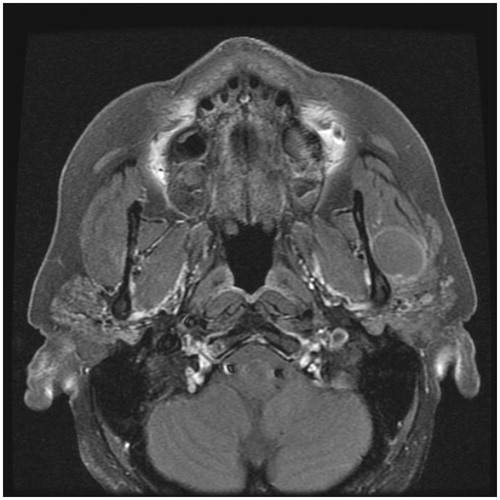
Figure 2. Axial T2-WI showing a well-circumscribed hyperintense lesion lying between the masseter muscle and the mandibular ramus, with a thin layer of masseter separating it from the parotid gland.
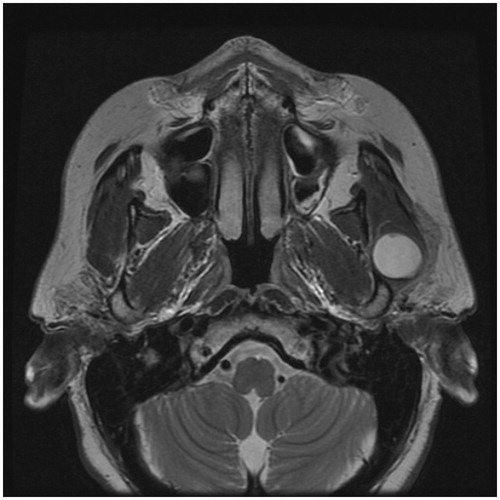
Figure 3. Coronal T2-WI showing a well-circumscribed hyperintense lesion lying deep to the masseter muscle, at the level of the mandibular notch.
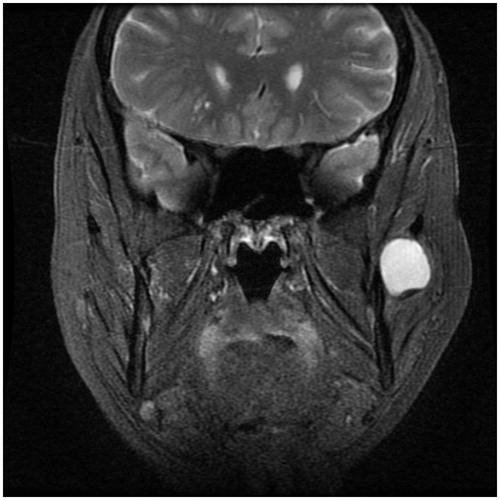
Figure 4. Per-operative image showing the cystic lesion (*) lying deep to the masseter muscle (divided and reclined, thick black arrow), between the buccal and zygomatic branches of the facial nerve (preserved and reclined, thin black arrows), after dissecting and reclining the superficial lobe of the left parotid gland (**).
Discussion
LECs account for less than 3% of benign parotid lesions and typically present as unilateral painless masses.[Citation4] Higher parotid LECs incidence rates have been reported in HIV-positive patients in whom cysts can often present bilaterally.[Citation5] Occasionally, benign parotid LECs were associated to Sjögren’s syndrome in immunocompetent individuals.[Citation6] In view of these findings and despite the unilateral presentation of the lesion, our patient underwent HIV serology in the post-operative course and tested negative. Furthermore, she denied any sicca symptoms suggestive of Sjögren’s.
The differential diagnosis of parotid LEC includes Warthin’s tumor, intramuscular benign hemangioma (IMH), branchial cleft cyst and lymphoma. MRI is the imaging modality of choice and helps characterizing the lesion. IMH are typically multiloculated and resemble a ‘bunch of grapes’. They are isointense on T1-WI and hyperintense on T2-WI and show a heterogeneous peripheral enhancement after contrast administration.[Citation7] Warthin’s tumors show similarly low signal on T1-WI and moderate to high signal on T2-WI, with however, no rim enhancement after contrast injection.[Citation8]
The characteristic histopathologic pattern is that of a glandular or squamous epithelium-lined cleft surrounded by abundant lymphoid tissue with prominent germinal centers, with some specimens even containing cholesterol crystals.[Citation3] In the reported case, pathology revealed that the cyst was surrounded by a thin layer of parotid salivary tissue, which led us to evoke two potential hypotheses; either the cyst originated in an ectopic intra-masseteric salivary gland or it developed in the most anterior part of the gland thus explaining its exclusive outward growth deep to the masseter muscle, even though we could not find a stalk attaching it to the gland.
HIV patients with salivary gland LECs are at higher risk of developing lymphomas and thus require close monitoring and follow up.[Citation1] However, this risk has not been reported in the immunocompetent population. Treatment options include watchful waiting, fine-needle aspiration and drainage, sclerotherapy, radiation therapy and surgical excision; the latter being considered the optimal attitude given the very low-recurrence rates of LECs in immunocompetent individuals.[Citation9,Citation10]
To our best knowledge, this is the first reported case of a benign intra-masseteric LEC. Excision of such deep facial lesions can be very delicate and tedious mostly because of the excessive retraction applied to the facial nerve branches.
Disclosure statement
All authors have equal contribution and no conflicts of interest to disclose.
Funding
No financial or material support was obtained for the production of this manuscript.
References
- Ahamed AS, Kannan VS, Velaven K, et al. Lymphoepithelial cyst of the submandibular gland. J Pharm Bioallied Sci. 2014;6:S185–S187.
- Peña S, Jeyakumar A. Radiology quiz case 2. Diagnosis: benign lymphoepithelial cyst of the parotid gland. Arch Otolaryngol Head Neck Surg. 2012;138:975–976.
- Glosser JW, Pires CAS, Feinberg SE. Branchial cleft or cervical lymphoepithelial cysts: etiology and management. J Am Dent Assoc. 2003;134:81–86.
- Kooper DP, Leemans CR, Hulshof MC, et al. Management of benign lymphoepithelial lesions of the parotid gland in human immunodeficiency virus-positive patients. Eur Arch Otorhinolaryngol. 1998;255:427–429.
- Mandel L, Hong J. HIV-associated parotid lymphoepithelial cysts. J Am Dent Assoc. 1999;130:528–532.
- Ihrler S, Zietz C, Sendelhofert A, et al. Lymphoepithelial duct lesions in Sjögren-type sialadenitis. Virchows Arch. 1999;434:315–323.
- Righini CA, Berta E, Atallah I. Intramuscular cavernous hemangioma arising from the masseter muscle. Eur Ann Otorhinolaryngol Head Neck Dis. 2014;131:57–59.
- Espinoza S, Halimi P. Interpretation pearls for MR imaging of parotid gland tumor. Eur Ann Otorhinolaryngol Head Neck Dis. 2013;130:30–35.
- Pillai S. Benign lymphoepithelial cyst of the parotid in HIV negative patient. J Clin Diagnostic Res. 2016;10:5–6.
- Castro JGL, Ferreira GM, Mendonça EF, et al. A rare occurrence of lymphoepithelial cyst in the palatine tonsil: a case report and discussion of the etiopathogenesis. Int J Clin Exp Pathol. 2015;8:4264–4268.
