Abstract
Mucocele of sphenoid sinus can present with a myriad of symptoms; headache is one of them and sphenoidal mucocele has to be kept in mind when evaluating patients with headache. It can be characterized by an asymptomatic initial period. We present a case of a 75-year-old diabetic and non-hypertensive female patient, presented with persistent headache since six months. After consulting with neurology, neurosurgery and ophthalmology, she was referred to the department of otolaryngology. Computed tomography and magnetic resonance imaging showed features consistent with sphenoidal mucocele with partial erosion of the sella. Endoscopic drainage of the sphenoidal mucocele with bilateral wide sphenoidotomy with posterior septectomy was done; the sphenoid sinus was irrigated with normal saline. The patient’s symptoms improved dramatically in the post-operative period. Sphenoidal mucocele may be an unusual cause of persistent headache. Early diagnosis and treatment are necessary to avoid potential complications.
Introduction
Mucocele of sphenoid sinus can present with a myriad of symptoms; headache is one of them and sphenoidal mucocele has to be kept in mind when evaluating patients with headache. Sphenoidal mucocele may be characterized by an asymptomatic initial period. Its expansion causes deformity and complications, unless diagnosed early and treated. The high-resolution computed tomography (CT) and the magnetic resonance imaging (MRI) are the investigations of choice. The treatment is surgical exploration and may be approached by conventional methods or by functional endoscopic sinus surgery. We report a case of sphenoid sinus mucocele presenting with persistent headache.
Case report
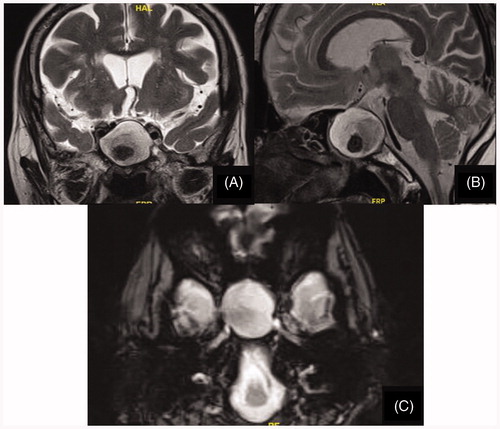
A 75-year-old diabetic and non-hypertensive female patient, presented with a history of persistent headache since six months. The patient had consulted neurology, neurosurgery and ophthalmology clinics for the same. Her visual acuity was normal with no diplopia, proptosis or facial numbness. Field of vision by confrontation method did not reveal any field defects. There was no evidence of neck stiffness. She was referred to the department of otolaryngology because CT imaging revealed isolated opacification and expansion of both sphenoid sinuses with maintained bony continuity along the periphery of the sinus; features were consistent with sphenoidal mucocele (Figure ). Partial erosion of the sella was also noted, however the size and shape of pituitary gland was normal. MRI showed expansion of the sphenoid sinuses with thin walls (Figure ).
Figure 1. (A and B) CT of the nose and paranasal sinuses (coronal view): shows a hypo dense lesion occupying both sphenoid sinuses causing expansion of the sinuses. There is no destruction of the adjacent bony walls. These findings are consistent with sphenoid sinus mucocele.
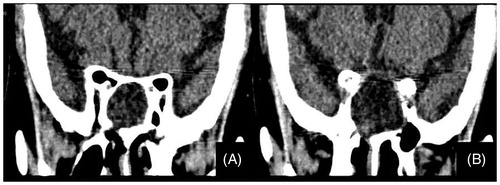
Figure 2. MRI of the nose and paranasal sinuses (A, coronal view; B, sagittal view and C, axial view) showing an expansile cystic lesion in the sphenoid sinus with hypointense debris within, consistent with sphenoid sinus mucocele. Infundibulum of pituitary and optic chiasma are pushed superiorly.
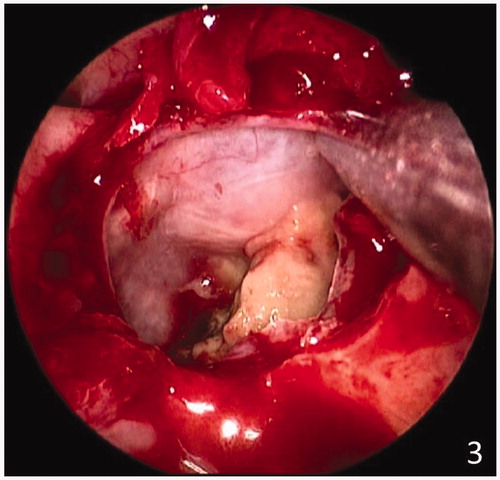
The patient’s consent was taken and endoscopic drainage of the sphenoidal mucocele was done under general anaesthesia. Bilateral wide sphenoidotomy with posterior septectomy was done. This revealed a cystic lesion under pressure, which was decompressed. Thick mucoid content was suctioned out. The sphenoid sinus was irrigated with normal saline, which revealed the erosion of the osseous walls, exposing the underlying dura (Figure ). The patient’s symptoms improved dramatically in the post-operative period.
Figure 3. Intraoperative Endoscopic view of the sphenoid sinus after marsupialisation of the sphenoidal mucocele.
The microbiological reports were unremarkable, and histopathological findings were consistent with that of a mucocele (proteinaceous material with polymorphonucleate infiltrate). The patient is on regular follow up for two years. Follow up nasal endoscopy was done every 6 months and showed no signs of recurrence. The patient remains asymptomatic till date.
Discussion
Mucocele is an expansile cystic lesion in the paranasal sinuses. This is due to the accumulation and retention of mucous secretion within the sinus due to the obstruction of its drainage through the ostium.[Citation1] Mucocele more commonly affects the frontal and ethmoid sinuses, less commonly the maxillary sinuses and rarely the sphenoid sinuses. Sphenoid sinus mucocele comprises 1–2% of all paranasal sinus mucoceles.[Citation2] The first case of sphenoid mucocele was described by Berg in 1889. Mucocele of the sphenoid is usually seen in fourth decade of life, and does not have any sex predilection.[Citation3] The symptoms of sphenoidal mucocele are non-specific. They occur as a result of mechanical pressure on neighbouring structures and/or due to an inflammatory process involving the nerves. The most common symptoms include headache, visual disturbances and 3rd, 4th and 6th cranial nerve palsies.[Citation4] Optic nerve involvement can lead to decreased visual acuity and even blindness, which is usually irreversible. The presentation is usually drooping of the upper eyelids, diplopia and restricted ocular movements. Sphenoid sinus mucoceles usually do not cause bitemporal hemianopia as seen with other sphenoidal and sellar lesions, such as pituitary macroadenoma.[Citation3]
Sphenoidal mucocele causing headache should be differentiated from other causes, which are either ophthalmological (like acute angle closure glaucoma) or neurological (like causes of increased intracranial pressure). Sphenoid sinus mucoceles may present as bilateral, gradually progressive headache which can temporarily be relieved by non-steroidal anti-inflammatory drugs (NSAIDs).
There are various causes for headache in patients with sphenoid mucocele. It could be due to mucosal inflammation of the paranasal sinuses, referred along the distribution of the ophthalmic division of the trigeminal nerve, or local bony destruction and irritation of the overlying dura. Also certain inflammatory cytokines such as TNF alpha, IL-6, IL-1, and PGE2 are found within the mucoceles which may cause trigeminal sensitization[Citation5]
The investigations for diagnosis of a sphenoid sinus mucocele include CT scan and MRI scans of the paranasal sinuses. The CT scan would show a hypodense cystic lesion in the sphenoid sinus with or without extension to the adjacent sellar and parasellar regions. It has to be differentiated from other cystic lesions such as craniopharyngioma, Rathke cleft cyst, cystic pituitary adenoma, epidermoid cyst, cystic optic nerve glioma and arachnoid cyst. MRI scan of the paranasal sinuses can confirm the diagnosis and extension of the mucocele.[Citation2,Citation6]
The sphenoidal mucocele should be managed surgically. Nowadays, the recommended management of a sphenoidal mucocele is endoscopic transnasal sphenoidotomy with drainage of the mucocele, along with sufficient removal of the anterior and inferior walls of the sinus (as in our case). This allows adequate drainage of the sphenoid sinus so as to avoid recurrences.[Citation7,Citation8]
Conclusion
Sphenoid sinus mucocele should be kept in mind in patients presenting with persistent headache. This unusual cause should be differentiated from other causes of headache like ophthalmological or neurological causes. Early diagnosis with the aid of cross-sectional imaging and its treatment is required in these cases in order to prevent complications. Endoscopic transnasal sphenoidotomy and drainage of the mucocele along with sufficient removal of the anterior and inferior walls of the sinus allows adequate drainage and helps to avoid recurrences.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
References
- Abe T, Ludecke D. Mucocele like formation leading to neurological symptoms in prolactinoma secreting pituitary adenomas under dopamine agonist therapy. Surg Neurol. 1999;52:274–279.
- Moriyama H, Hesaka H, Tachibana T, et al. Mucoceles of ethmoid and sphenoid sinus with visual disturbance. Arch Otolaryngol Head Neck Surg. 1992;118:142–146.
- Bahgat M, Bahgat Y, Bahgat A. Sphenoid sinus mucocele. BMJ Case Rep. Published Online: 22 Oct 2012. doi:10.1136/bcr-2012-007130.
- Kösling S, Hintner M, Brandt S, et al. Mucoceles of the sphenoid sinus. Eur J Radiol. 2004;51:1–5.
- Lee KE, Kim KS. Headache induced by the sphenoid sinus mucocele. Braz J Otorhinolaryngol. 2015;81:113–114.
- Kennedy DW, Josephson JS, Zinreich SJ, et al. Endoscopic sinus surgery for mucoceles: a viable alternative. Laryngoscope. 1989;99:885–895.
- Lund VJ. Endoscopic management of paranasal sinus mucocoeles. J Laryngol Otol. 1998;112:36–40.
- Har-El G. Endoscopic management of 108 sinus mucoceles. Laryngoscope. 2001;111:2131–2134.
