Abstract
Foreign body ingestion is a common otorhinolaryngological emergency encountered. Most frequently noted are fish bones, which usually get impacted at the level of cricopharynx. However, sometimes few may migrate extraluminally, or even extrude subcutaneously. We present a case of an adult with foreign body ingestion (fish bone) which had migrated and embedded in the left pyriform sinus and larynx, requiring open surgery for removal.
Introduction
Ingested foreign bodies can present life-threatening emergencies if left untreated. Foreign bodies commonly ingested in the adult group are fish bones, chicken bones and dentures.[Citation1] They usually get impacted in the tonsils, base of tongue and upper esophagus.[Citation1] Precipitating factors noted in adult foreign body ingestion are dental procedures, neurological dysfunction, mental retardation, edentulous, seizures and alcoholism.[Citation2] Patients presented with odynophagia, after accidental ingestion. Trial of removal can be done under direct or endoscopic vision in a clinical setting, failing which, removal can be attempted under general anaesthesia. A computer tomography (CT) scan can aid to map the site of foreign body to assist removal. Most foreign bodies are able to pass through the GI tract spontaneously, 10–20% require non-operative intervention while less than 1% require surgery.[Citation3] Migration of foreign body extraluminally is rare, we report a case in which the fish bone had migrated to the larynx, requiring open surgery for removal.
Case report
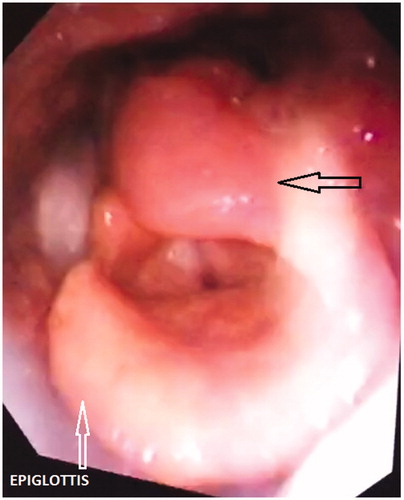
A 64-year-old man was admitted with a four-day history of accidental fish bone ingestion. He presented with odynophagia, leading to reduction in oral intake. Oral examination was unremarkable, a flexible scope showed swollen arytenoids (Figure ) , left more than right, otherwise no foreign body was noted. A flexible esophagoscopy was clear up to 45cm from upper incisor. He was started on antibiotics and kept nil by mouth.
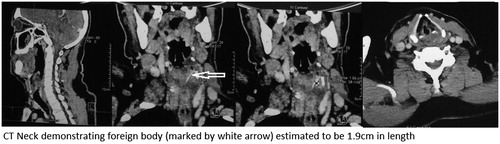
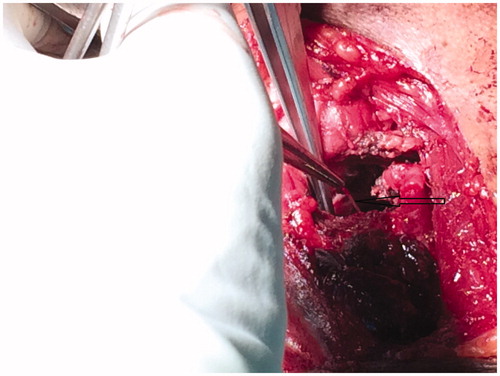
A repeat scope showed bilateral arytenoids swollen with edema of the false cords and post cricoids region, hence a CT neck was performed, which revealed a foreign body embedded within the left pyriform sinus (Figure ), extending into the posterior aspect of left mid arytenoid cartilage. Attempts of removal via direct laryngoscopy, by inspecting the entry point at the left arytenoid as based on CT scan, were unfruitful. A decision was made to convert to open surgery. Using a lateral pharyngotomy approach, the pharynx was exposed and examined. A 2 cm fish bone was found to be embedded in the left arytenoids, extending inferomedially into the left pyriform fossa and was removed uneventfully (Figures and ).
Post-operative flexible scope showed laryngeal inlet edema, bilateral vocal cords being mobile. He was discharged with Ryle’s tube for feeding. There was a reduction in swelling of arytenoids, in a subsequent scope two weeks later. A month post operatively, the arytenoid swelling had subsided, and he was able to swallow and Ryle’s tube was removed. No post-operative complications were noted.
Discussion
Foreign body ingestion is a common presentation in any otorhinolaryngology clinic. Most foreign bodies get impacted at the level of cricopharynx; rarely, they may migrate extraluminally.[Citation4] The incidence of foreign body impacted in the larynx is 4% in Cohen Series.[Citation5] In the Chee and Sethi series, they reported 24 foreign body migration in the neck, all of which were sharp and linear.[Citation1] Extraluminal migration of foreign bodies is rare, and are usually associated with late presentation to seek medical treatment.[Citation6] Remsen et al. reported that out of 321 cases of penetrating esophageal foreign bodies, 43 migrated extraluminally.[Citation7] Extraluminal migration of foreign bodies can cause serious life-threatening complications. Some complications include oesophageal perforation, mediastinitis, vascular complications, abscess formation and airway compromise.[Citation8]
In our patient, clues suggesting foreign body migration was late presentation to seek treatment, and there was persistent left arytenoid swelling. Late presentation was also seen in the Divya and Hameed series.[Citation6] First line plain X-rays should be ordered to look for the presence of foreign body or free gas. Initial attempts of foreign body removal can be done under direct or endoscopic vision. Following which, rigid instrumentation or flexible esophagoscopy is the next option. The rate of success for rigid instrumentation ranges from 94% to 100%, while flexible esophagoscopy is between 76% and 98.5%.[Citation9] If all the rest fail, neck exploration with the assistance of CT guidance is recommended.
A CT scan assists in planning the appropriate surgical approach to avoid any further complication, for example, vocal cord palsy as noted in the Tang and Singh series.[Citation10] The problem lies in finding out the exact location note in the CT where the foreign body may not be situated, as in the Divya and Hameed series.[Citation6] In our case, we were able to estimate the location of the foreign body, and successfully remove the fish bone with minimal complications with the help of a CT scan. The author recommends to keep patients on Ryle’s tube feeding post operatively, to allow adequate wound healing.
Conclusion
Extraluminal migration of foreign bodies is a rare occurrence. Late presentation in seeking professional help is a predictive factor. A high index of suspicion is required when endoscopy fails to identify a foreign body. CT scan of the neck assists in providing a road map to identify the exact location and appropriate approach for the removal of foreign body. By knowing the relation of important structures with the foreign body, we can minimize the risk of complications, such as bleeding and nerve injury, during neck exploration and retrieval of the object.
Acknowledgements
The authors would like to thank the Ministry of Health, Malaysia for allowing usage of patient’s records.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
References
- Chee LW, Sethi DS. Diagnostic and therapeutic approach to migrating foreign bodies. Ann Otol Rhinol Laryngol. 1999;108:177–180.
- Chouhan M, Yadav JS, Bakshi J. Unusual presentation of foreign body in larynx. Egyptian J Ear,Nose,Throat Allied Sci. 2012;13:61–63.
- Schwartz GF, Polsky HS. Ingested foreign bodies of the gastrointestinal tract. Am Surg. 1976;42:236–238.
- Pang KP, Pang YT. A rare case of foreign body migration from the upper digestive tract to the subcutaneous neck. Ear Nose Throat J. 2002;81:730–732.
- Cohen SR, Herbert WT, Lewis GB Jr, et al. Foreign bodies in the airway. Five-year retrospective study with special reference to management. Ann Otol Rhinol Laryngol. 1980;89:437–442.
- Divya GM, Hameed AS, Ramachandran K, et al. Extraluminal migration of foreign body: a report of two cases. Int J Head Neck Surg. 2013;4:98–101.
- Remsen K, Lawson W, Biller HF, et al. Unusual presentation of penetrating foreign bodies of upper aerodigestive tract. Ann Otol Rhino Laryngol Suppl. 1983;105:32–44.
- Monnier P, Savary M. Foreign bodies of the esophagus: a retrospective study in 1436 adults. Proceedings of the International Congress of Thorax Surgery, Monduzzi Editore: Bologna, 1997:197–200.
- Shreshtha D, Sikka K, Singh CA, et al. Foreign body esophagus: when endoscopic removal fails. Indian J Otol Head Neck Surg. 2013;65:380–382.
- Tang IP, Singh S, Shoba N, et al. Migrating foreign body into the common carotid artery and internal jugular vein-a rare case. Auris Nasus Larynx. 2008;36:380–382.