Abstract
Fungal laryngeal infection is commonly seen in immunocompromised individuals, and can mimic other laryngeal diseases like gastroesophageal reflux disease, granulomatous disease, leucoplakia and carcinoma. Therefore, it is important for correct initial diagnosis and treatment to avoid morbid consequences. We have reported a patient with laryngeal candidiasis who was previously diagnosed with laryngeal cancer and treated by concurrent chemoradiation therapy, presented with shortness of breath and stridor, requiring an emergency tracheostomy. Laryngoscopy examination revealed the presence of irregular mucosa at the posterior 2/3 of the left vocal cord extending to the left false cord and biopsy taken. Histopathological examination revealed necrotic tissue with colonies of bacteria and Actinomyces, and closer examination revealed fungal organisms exhibiting round, budding structures along with branching hyphae of varying sizes. Special histochemistry with Gomori Methenamine. Silver (GMS) and periodic acid-Schiff (PAS) stains confirmed the presence of fungal bodies. Tissue for culture and sensitivity grew Candida albicans, and the patient treated with IV fluconazole and discharge home with oral fluconazole. Post-treatment follow-up laryngoscopy examination revealed normal laryngeal mucosa with no evidence of fungal bodies or tumours recurrence. A conclusion can be made that diagnosis of a patient with fungal laryngitis requires early detection and treatment, as misdiagnosis or delay in treatment may result in further impairment to the anatomical and functional properties of the larynx. Invasive fungal infection can mimic or hide underlying concomitant laryngeal malignancies. Therefore, performing a biopsy during initial presentation allows the exclusion of underlying malignancy and further progression of the malignancy.
Introduction
Fungal laryngeal infection is an uncommon occurrence and more frequently seen in immunocompromised individuals, and it accounts for approximately 40 reported cases in the literature.[Citation1] It has been described in individual with underlying chronic diseases, broad-spectrum antimicrobial therapy, steroid administration, chemotherapeutic therapy, diabetes mellitus, and mechanical, chemical or thermal injury to the mucosal barrier.[Citation2,Citation3] Fungi infection can occur superficially on the mucosal surface of the larynx or can invade the mucosa resulting in a more adverse outcome.
We have reported a case of laryngeal candidiasis in a patient presenting with recurrent laryngeal cancer.
Case report
A 56-year-old Chinese gentleman underlying supraglottic cancer received a total 35 fraction (70Gy) radiation with concurrent Cisplatin 50 mg/m2 IV weekly for a total of 7 weeks and completed in September 2014, presented to the emergency department at University Malaya Medical Centre in March 2015 with complaints of progressively worsening shortness of breath, hoarseness and stridor over the period of two weeks. Upon examination, he appeared tachypnoeic with a respiratory rate of 30 breaths pre min and with the presence of audible inspiratory stridor. Flexible nasal laryngoscopy revealed bilateral false cord and arytenoid oedema, unable to visualise true vocal cord and with a minimal glottic opening. The patient underwent an emergency Tracheostomy under LA, followed by a direct laryngoscopy and examination under anaesthesia. Intraoperative findings revealed the presence of irregular mucosa at the posterior 2/3rd of the left vocal cord extending to the left false cord, and a biopsy taken.
Histopathological examination of the biopsy from left true cords and arytenoids revealed necrotic tissue with colonies of bacteria and Actinomyces (Figure ). Closer examination revealed fungal organisms exhibiting round, budding structures along with branching hyphae of varying sizes. Special histochemistry with Gomori Methenamine. Silver (GMS) and periodic acid-Schiff (PAS) stains confirmed the presence of fungal bodies (Figure ).
Figure 1. Fragments of cartilage with the edges showing colonies of bacteria and degenerative material [Haematoxylin & Eosin, 40× magnification].
![Figure 1. Fragments of cartilage with the edges showing colonies of bacteria and degenerative material [Haematoxylin & Eosin, 40× magnification].](/cms/asset/79b4fa8e-216e-4247-9bb6-bca1d2a6c52a/icro_a_1257915_f0001_c.jpg)
Figure 2. Same specimen showing fungal spores and hyphae with varying morphology [GMS, 200× magnification].
![Figure 2. Same specimen showing fungal spores and hyphae with varying morphology [GMS, 200× magnification].](/cms/asset/b882d8a5-fb09-456d-890f-70f5e2912bbd/icro_a_1257915_f0002_c.jpg)
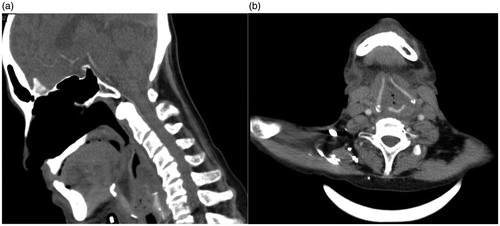
Tissue sent for culture, and sensitivity showed the presence of fungal elements, consistent with Candida albicans. The patient was treated with iv Fluconazole and discharge home a course of oral fluconazole. CT Neck contrast was done 2 weeks post treatment revealed no residual tumour and no evidence of bone or cartilage erosion seen. (Figure ) A repeat direct laryngoscopy and biopsy was performed one-month post initial treatment confirmed no residual tumour or fungal bodies.
Discussion
Fungal laryngitis was commonly seen in immunocompromised individuals and uncommonly seen in immunocompetent individuals. The radiological and endoscopic appearance can mimic that of laryngeal malignancy. The case presented above is a patient with previously treated glottic cancer which has represented with fungal laryngitis. There are multiple predisposing factors in the development for fungal laryngitis which has been broadly divided into (1) Factors reducing immune response: Diabetes, immunodeficiency status, immunosuppressive medications (e.g. chemotherapy, corticosteroids), nutritional deficiency, etc. (2) Factors affecting mucosal barriers: prior radiotherapy, inhaled corticosteroids, gastroesophageal reflux disorder, trauma (intubation), smoking.[Citation2]
The usual presentation of fungal laryngitis in immunocompromised patients is variable and can present as hoarseness, dysphagia, dysphonia, odynophagia, stridor and respiratory distress.[Citation4] The presence of fungal laryngeal infections can mimic gastroesophageal reflux disease, granulomatous diseases, leucoplakia and carcinoma.[Citation3] These symptoms are derived from the functional anatomical alteration of the larynx and involvement of adjacent structures. Fungal infection of the larynx usually presents as a superficial infection characterised by mucosal hyperplasia as a result of the direct invasion. Cases of fungal laryngitis with invasion can further present with systemic manifestation like fever, chills and malaise.[Citation4]
The most common fungi causing laryngitis is Candida. Other fungal infections like Aspergillosis, Crypto Cryptococcal, Blastomycosis and Histoplasmosis is also implicated.[Citation2,Citation3] Infection usually occurs as a secondary to pulmonary or oropharyngeal infection.
Histologic evaluation of tissues is a quick and easy way to identify fungal organisms, and a strong adjunct to microbiologic culture for diagnosis of fungal infections. Histologic evaluation of granulomatous inflammation and granulomas must include special stains to exclude or include the presence of fungi and acid-fast bacteria. Gomori Methenamine Silver (GMS) and periodic acid-Schiff (PAS) are the two most common stains used to look for fungi in tissues and cytology specimens. In the tissues, fungi usually occur either as hyphae, budding yeast, endo sporulating spherules or a combination of these forms.[Citation5,Citation6] Candida has Spherical to subspherical budding yeast-like cells or blastoconidia, pseudohyphae with blastoconidia and terminal vesicles.
The literature search has shown a variation regarding the first-line antifungal agent and the mode of initial treatment (local or systemic). In immunocompetent patients with no evidence of spreading disease, topical nystatin (as a suspension or pastille) for 3 weeks is recommended. Excision of the lesion with the application of gentian violet has also been reported to be successful. If the condition does not resolve, the patient is treated with a systemic oral antifungal agent such as Fluconazole or Itraconazole daily for 3 or 4 weeks. The first-line treatment is oral antifungal agent, especially for the immunocompromised patient with a non-invasive disease. Intravenous Amphotericin B is used for refractory cases or in patients with significant tissue invasion. The cases reported here was administered fluconazole 200 mg daily for 3 weeks and showed marked improvement with complete resolution of signs and symptoms.
Conclusions
Diagnosis of a patient with fungal laryngitis requires early detection and treatment, as misdiagnosis or delay in treatment may result in further impairment of the anatomical and functional properties of the larynx. Invasive fungal infection can mimic or hide underlying concomitant laryngeal malignancies. Our case has demonstrated a possibility of fungal laryngitis in a patient with initial laryngeal malignancy post radiation therapy with no recurrent malignancy. Therefore, performing a biopsy during initial presentation allows the exclusion of underlying malignancy and further progression of the malignancy.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
References
- Nair AB, Chaturvedi J, Venkatasubbareddy MB, et al. A case of isolated laryngeal candidiasis mimicking laryngeal carcinoma in a immunocompetent individual. Malays J Med Sci. 2011;18:75–78.
- Mehanna Hisham M, Kuo T, John C, Taylor G, et al. Fungal laryngitis in immunocompetent patients. J Laryngol Otol. 2004;118:379–381.
- Ravikumar A, Prasanna Kumar S, Somu L, et al. Fungal laryngitis in immunocompetent patients. Indian J Otolaryngol Head Neck Surg. 2014;66:375–378.
- Henry LR, Packer MD, Brennan J. Airway-obstructing laryngeal candidiasis in an immunocompetent host. Otolaryngol Head Neck Surg. 2005;133:808–810.
- Chandler FW, Watts JC. Pathologic diagnosis of fungal infections. Chicago: ASCP Press; 1987.
- Haque AK, McGinnis MR. Dail and Hammar’s pulmonary pathology. New York: Springer; 2008. Chapter 10. Fungal infections, 349–408.