Abstract
Background: Endobronchial foreign bodies (EFBs) are rare in children over the age of three. Case presentation: Two school-age children had EFBs due to accidental inhalation of metal-containing foreign bodies in the mouth. In case 1, CT showed a needle-like foreign body at the entrance of the right upper lobe bronchus, and in case 2, it was found in the posterior basal segment of the right lower lobe. The EFB in case 1 was successfully removed by rigid bronchoscopy. In case 2, the EFB was not accessible via fiberoptic bronchoscopy, and the foreign body was accidentally pushed into the right main bronchus during the thoracotomy for foreign body removal; however, it was later removed by rigid bronchoscopy. Conclusion: In cases of special types of bronchial foreign bodies, the surgical approach should be selected based on the features of the foreign body to minimize patient injury as much as possible.
Introduction
Endobronchial foreign body (EFB) is an acute and critical condition in otolaryngology, most commonly affecting children aged 1-3, and the majority of foreign bodies are of plant origin. The standard procedure for removing foreign bodies is through rigid or fiberoptic bronchoscopy [Citation1,Citation2]. Aspiration of foreign bodies in the trachea is also common in children over 3 years old. However, the types of foreign bodies at this age are not limited to plant-based materials; thus, selecting the appropriate surgical method can be challenging. For non-plant EFBs, it is often necessary to remove the foreign bodies through tracheotomy or thoracotomy. Here, we report 2 cases of needle-type EFBs that encountered difficulties during conventional bronchoscopy foreign body removal. By combining preoperative CT, we were able to remove the foreign bodies with minimal injury, and the children recovered quickly during subsequent treatment.
Case reports
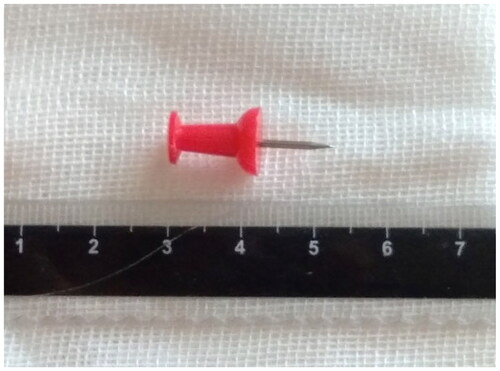
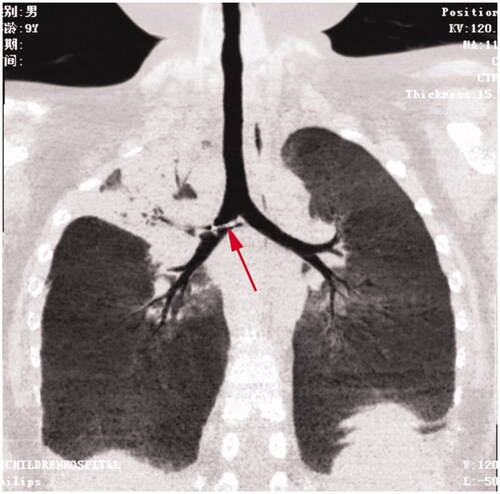
Case 1 was a nine-year-old boy who was initially admitted due to a persistent cough that lasted over half a month and a fever persisting for four days. The child denied any history of foreign body aspiration. Physical examination revealed a temperature of 38.9 °C, diminished breath sounds, and rales in the right upper lung region. Right upper lobe pneumonia and atelectasis were seen on a chest CT due to a needle-like metallic foreign body lodged in the right main bronchus and upper lobe bronchus (Figure ) The CT scan confirmed that the foreign body was located in the right upper lobe bronchus, a position rarely encountered in clinical practice. Despite the child’s denial of any history of foreign body aspiration, the diagnosis of an endobronchial foreign body was considered based on the patient’s symptoms and CT findings. We decided to perform a rigid bronchoscopy examination and foreign body removal under general anesthesia ().
Figure 1. A needle-like metallic foreign body in the right main bronchus and right upper lobe bronchus.
Following standard anesthesia for patients with tracheal foreign bodies (while maintaining spontaneous breathing), a rigid bronchoscope was inserted, and 100% oxygen was administered at 2 L/min through the side port. The anesthetist controlled the patient’s breathing with the assistance of the manual resuscitator. The tip of a needle-like foreign body was found within the right upper lobe bronchus, accompanied by granulation tissue surrounding the bronchial wall. Since the foreign body was located in the bronchus of the right upper lobe, the rigid bronchoscope could only explore the opening of the right upper lobe bronchus and could not provide a clear view of the entire foreign body. During the removal, the foreign body could not pass through the lumen of the rigid bronchoscope, indicating that it was more complex than a simple needle-like foreign body and that the distal end might have had an enlarged, non-radiopaque portion. The foreign body was securely grasped by the bronchial forceps, and both the bronchial forceps along with the foreign body were simultaneously withdrawn together with the rigid bronchoscope.
When the foreign body reached the glottis, resistance was reencountered. To prevent injury to the glottis from the enlarged distal end of the foreign body, succinylcholine was administrated to relax the laryngeal muscles, allowing the foreign object to pass through the glottis with less resistance. A face pressure mask was used to provide oxygen after the foreign object had passed through the glottis. The surgical procedure proceeded smoothly, with minimal blood loss of approximately 1 ml, which was controlled after rinsing with 1:10000 epinephrine saline. There was no significant decrease in blood oxygen saturation during the operation.
Postoperatively, the patient was returned to the ward and administered intravenous antibiotics (cefathiamidine 150 mg BID based on his weight of 30 kg) for anti-inflammatory treatment, as well as steroids (hydrocortisone 150 mg IV QD and Pulmicort 1 mg nebulized BID) to alleviate edema. A three-day postoperative radiograph showed no residual foreign bodies or complications such as pneumothorax, and the child was discharged.
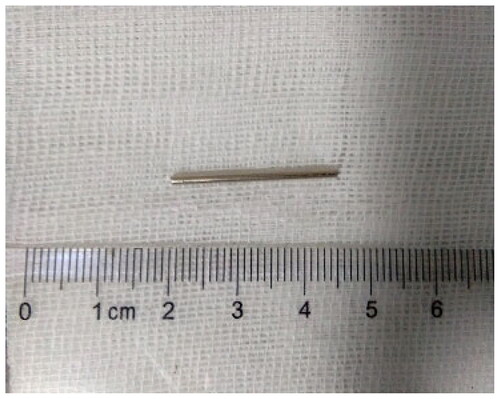
Case 2 was a 10-year-old boy who was admitted to the hospital after accidentally inhaling a metal needle-like foreign body three days prior. A chest CT scan revealed an EFB in the basal segment of the right lower lobe (Figure ). The physical examination showed a temperature of 36.4 °C and clear breath sounds in both lungs, with no rales or wheezing. CT imaging indicated that the EFB was far from the oropharynx and unlikely to be reachable with a conventional rigid bronchoscopy, so a fiberoptic bronchoscopy with a 3.0 mm diameter was performed first. However, the foreign body was not visible at any bronchial entrance during the fiberoptic bronchoscopy.
After failing to change the foreign body’s location by patting the back, inversion, and magnet attraction, a thoracotomy was performed. Following general anesthesia and intubation, a preoperative chest radiograph was obtained, which showed the foreign body’s location near the T9-10 vertebrae on the right side. Initial thoracoscopic exploration was conducted, but the foreign body was not observed under thoracoscopy. An intraoperative chest radiograph revealed that the foreign body had moved to the T5-6 level. Consequently, an incision was made between the 5th and 6th ribs. The surgeon palpated the area where the foreign body was located on the chest radiograph, but it was still inaccessible. Intraoperative chest radiograph revealed that the foreign body had moved to the right main bronchus. The endotracheal tube was withdrawn, and an otolaryngologist inserted a rigid bronchoscope through the mouth. With the assistance of an anesthesiologist using a manual resuscitator, the otolaryngologist successfully extracted the foreign body. (Figure ) The patient had no postoperative complications, including pneumothorax, hoarseness, or laryngeal stridor. Based on his weight of 37 kg, he received postoperative intravenous anti-infection treatment (cefuroxime 750 mg TID for 7 days). The child made a full recovery and was discharged without complications.
Discussion
Preoperative CT scans in both cases revealed a needle-shaped high-density object within the bronchus, and the EFBs were ultimately removed. Both children made a complete recovery and were discharged. The locations of the foreign bodies in the two cases were uncommon, and the clinical features were distinct in each case. Notably, the two surgical procedures differed significantly, necessitating further discussion.
The inflammation caused by Endobronchial foreign bodies (EFBs) is related to the duration of the foreign body’s presence in the airway and the type of foreign body. The longer the foreign body is present, the more severe the bronchial inflammation [Citation3,Citation4]. However, simple steel-type foreign bodies cause less bronchial inflammation. In Case 1, the history of inhaling a foreign body was denied preoperatively, so the surgeon was unaware of the specific shape of the EFB. A preoperative CT scan showed atelectasis in the right upper lobe bronchus due to long-term obstruction caused by the foreign body [Citation5]. Therefore, we preoperatively speculated that the foreign body in Case 1 was not a simple steel foreign body that could have a non-radiopaque enlarged part on the surface or at one end.
The location of the foreign body in the bronchus in Case 1 was uncommon. When a foreign body enters the lower airway, it typically follows a more vertical and gravity-gradient direction. As a result, it is more commonly lodged in the right main bronchus, which is relatively straighter, wider, shorter, and closer to the trachea than the left main bronchus. Bernoulli’s effect explains rarer cases of a foreign body lodging in the left bronchus. Due to the smaller diameter of the left main bronchus compared to the right, more negative suction pressure occurs during coughing, laughing, or speaking, leading to aspiration of the foreign body to the left side[Citation6]. Therefore, it is extremely rare for a foreign body to enter the right upper lobe bronchus [Citation7].
Postoperative analysis showed that the location of this foreign body was related to its structure. The foreign body was made of plastic on one end and steel on the other. The densities at the two ends were quite different. The plastic end had a unique shape, with a narrow end that gradually increased in diameter (as shown in Figure ). During the descending process after entering the trachea, the plastic end was lodged in the entrance of the right upper lobe bronchus due to its shape.
Figure 3. (a, b) Chest anteroposterior and lateral radiographs showing a needle-shaped metallic foreign body aligned with the bronchial path; (c, d) Transverse sections revealing a short rod-shaped dense shadow; (e, f) Tracheobronchial reconstruction images showing a slender rod-shaped metallic dense shadow within the right lower lobe basal segmental bronchus.

The EFB in Case 2 was notably different from the EFB in Case 1. This EFB was an elongated, simple steel foreign body that didn’t irritate the bronchial wall, so conservative observation was considered a viable option. However, no reports of long-term conservative observation for related foreign bodies were found in the literature, and current guidelines for EFB treatment still recommend removal upon initial discovery [Citation7]. Moreover, the child’s young age increases the risk of complications such as migration, granulation tissue growth, and mechanical issues, which would make the surgery more difficult and potentially harmful to the child. As a result of failing to move the foreign body using techniques such as patting the back, inversion, and magnet attraction, a thoracotomy was performed. However, it was discovered during the thoracotomy that the foreign body had moved to the right main bronchus. We infer that during the surgical procedure, as the thoracic forceps and the surgeon manipulated and searched for the foreign body by palpating and turning the lung tissue in various directions, the foreign body was impacted by the gas. This caused it to be propelled along the airflow into the right main bronchus, in a manner somewhat similar to the Heimlich maneuver. Ultimately, the foreign body was successfully removed using a rigid bronchoscope, avoiding more significant damage, such as lung tissue resection.
Conclusion
We present two cases of endobronchial foreign bodies (EFBs) in school-aged children, as shown in preoperative CT scans. We developed a minimally invasive surgical approach for both cases based on the characteristics of the EFBs and their locations. In Case 1, the unusual location of the foreign body within the trachea was related to its shape and texture. Additionally, the foreign body’s representation on CT scans didn’t accurately reflect its actual shape. Therefore, it is essential to assess the type and shape of the foreign body comprehensively, considering its location and the severity of inflammation. During surgery, the margin and shape of the foreign body should be carefully identified under rigid bronchoscopy. The needle-shaped foreign body in case 2 was unreachable with fiberoptic bronchoscopy and required thoracotomy intervention. We suggest that during the thoracotomy, by inserting a fiberoptic bronchoscope through the endotracheal tube, we could monitor real-time changes in the foreign body’s position as the lung tissue is palpated and rotated in various directions. This manipulation of the lung tissue might potentially cause the foreign body to shift its position. If we notice the foreign body moving towards the desired path while palpating and rotating the lung tissue, we can repeat those movements to guide the foreign body to a reachable location for bronchoscopy, thereby avoiding the need for lung tissue resection.
Informed consent
The patients provided informed consent for the publication of this article.
| Abbreviations | ||
| EFBs | = | Endobronchial foreign bodies |
| EFB | = | Endobronchial foreign body |
| CT | = | computed tomography |
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Huang Z, Zhou A, Zhang J, et al. Risk factors for granuloma formation in children induced by tracheobronchial foreign bodies. Int J Pediatr Otorhinolaryngol. 2015;79(12):2394–2397.
- Ding G, Wu B, Vinturache A, et al. Tracheobronchial foreign body aspiration in children: a retrospective single-center cross-sectional study. Medicine. 2020; 2999(22):e20480.
- Xu Y, Ren HB, Jiang L, et al. Analysis of related factors for the retention time of tracheobronchial foreign bodies in pediatrics. J Surg Res. 2019;233:262–267.
- Idris S, Murphy RA, Witmans M, et al. A simple management option for chronically impacted sharp tracheobronchial foreign bodies in children. J Otolaryngol Head Neck Surg. 2018;47(1):26.
- Xu Y, Feng RL, Jiang L, et al. Correlative factors for the location of tracheobronchial foreign bodies in infants and children. J Thorac Dis. 2018;10(2):1037–1042.
- Sidam S, Gupta V, Mishra UP. Spontaneous expulsion of foreign body bronchus: understanding the mechanism. Indian J Otolaryngol Head Neck Surg. 2022;74(Suppl 3):5381–5383.
- Abraham ZS, Kahinga AA, Mapondella KB, et al. Spontaneous expulsion of an intrabronchial sharp metallic foreign body and migration to the gastrointestinal tract at muhimbili national hospital: case report and literature review. Int J Surg Case Rep. 2020;72:423–425.