Abstract
Neonatal nasal obstruction can cause significant functional impairment because neonates are obligatory nasal breathers in the first three months of life. Some neonates with nasal septum issues may be asymptomatic or exhibit mild symptoms that could resolve as they grow in the first few years of life. However, in cases of patients with an uncorrected deviated nasal septum, it can have physiological, anatomical, cosmetic, and psychological impacts. Many studies have reported different approaches to correct neonatal deviated nasal septum, including observation, stenting, close reduction, and septoplasty. Herein, we present two cases aged 14 days and 35 days old with severe symptoms of deviated nasal septum, balloon dilatation septoplasty, a minimally invasive approach, was employed, with low-risk complications and good outcomes. Up to this date, this approach has not been reported in this age group.
Introduction
Neonatal airway obstruction may occur at different anatomical levels. Nasal airway obstruction can be caused by many pathologies, including mucosal edema, neonatal rhinitis, choanal atresia, pyriform aperture stenosis, midnasal stenosis, deformed lateral nasal cartilage, medial growth of lateral nasal walls, congenital cysts, and traumatic septal deviation [Citation1]. The deviated nasal septum (DNS) is estimated to be 1 − 30% in different studies [Citation2]. In Saudi Arabia, the estimated prevalence is 7.2% [Citation3]. A deviated septum may occur to varying degrees during pregnancy or delivery and can be classified into two types: anterior septal dislocation and combined septal dislocation. Anterior septal dislocation, which represents subluxation of the septal cartilage from the maxillary crest, was found more commonly developed during spontaneous vaginal delivery than during cesarean section, 22.2% and 3.9%, respectively [Citation4]. Meanwhile, combined septal dislocations include the entire septum, both anterior and posterior. In a previous study, they proposed the theory of maxillary molding, which holds that neonatal deformities are caused by prolonged transmitted pressure in utero, resulting in a combined deformity [Citation5]. In contrast to anterior septal dislocation, the combined deformity has an equal incidence in vaginal and cesarean deliveries [Citation2,Citation4]. Cartilaginous septal subluxation presents with lateral deviation of the nasal tip, asymmetry of the nostrils (Metzenbaum’s sign), and the oblique position of the columella. The nasal tip is easily flattened by a light digital pressure known as a ‘compression test’, and inspection with a small speculum or an otoscope shows the dislocation of the lower end of the quadrangular cartilage toward the narrowed nostril [Citation6]. In many cases, the septal dislocation returns to normal position within a few weeks of life without intervention, but persistent deviation may occur and can cause physiological, anatomical, cosmetic, and psychological impactions [Citation7]. Severe DNS in neonates and infants can lead to cyanotic spells, feeding difficulties that predispose them to rhinosinusitis, eustachian tube dysfunction, otitis media, chronic suppurative otitis media, facial asymmetry, and epiphora due to nasolacrimal duct obstruction. In more severe cases, it could lead to increased pulmonary resistance, pulmonary hypertension, and, if left untreated, respiratory failure [Citation2,Citation8,Citation9]. Urgent management of nasal obstruction can be critical in neonates and infants as their obligatory nasal breathing [Citation10]. In the cases of septal deviation, when and how to intervene is not yet universally agreed upon [Citation2]. The decision to operate is based primarily on the extent of the functional impairment and the severity of the esthetic deformity [Citation9]. To the best of our knowledge, for all interventions of neonatal septoplasty, we present the first balloon dilatation septoplasty performed in neonates. Two patients underwent this procedure with satisfactory outcomes. this work has been reported in line with the SCARE criteria [Citation11].
Case report
Patient 1
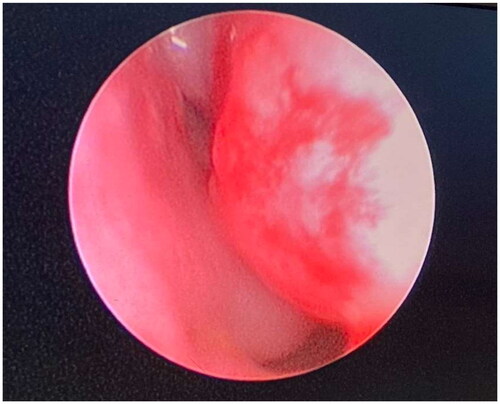
A baby girl born prematurely by cesarean section at 34 + 1 gestational weeks with respiratory distress syndrome and desaturation, she was intubated and admitted to the neonatal intensive care unit (NICU). The mother had polyhydramnios and uncontrolled gestational diabetes and was on insulin during pregnancy. Later, the baby was diagnosed with oculocerebrofacial syndrome and distinctive dysmorphic features, including microtia, micro and retrognathia, low set ears, short neck, short limbs, flat nasal bridge, microphthalmia, and small face. During her prolonged stay in NICU, the patient developed sepsis twice and was extubated on day 13 but was on continuous positive airway pressure (CPAP), alternating with high flow nasal cannula, as she continues to be in respiratory distress. We also observed that the patient had stridor while she was on the nasal cannula and was associated with crying and agitation, mostly inspiratory stridor. Examination showed no external nasal deformity; flexible nasopharyngoscope could not pass through the right nostril due to the severe DNS (Figure ). Computed tomography (CT) paranasal sinus (PNS) showed severe DNS to the right side.
Figure 1. Nasal endoscopic picture of right nasal cavity of patient 1 showing deviated nasal septum touching the inferior turbinate.
After reviewing the CT and the scope results, she was taken to the operating room at age of 8 weeks for bronchoscopy and nasal endoscopy with septoplasty balloon dilation. Bronchoscopy showed laryngomalacia with short aryepiglottic folds. We used CRE™ Pulmonary Balloon Dilatation Catheter size 5 mm (Boston scientific). Using the rigid nasal scope, a balloon catheter was inserted in the floor of the right nasal cavity; pressure was built gradually to 2 atmospheric pressure (ATM) and kept for 2 min while inspecting the other patent side to avoid septum subluxation and overcorrecting to the other side. Immediate improvement was observed, and the bilateral nasal cavities were patent. At the end of the procedure, endotracheal tube (ETT) size 3 was inserted in each nostril, as a stent to stabilize the nasal septum and fixed with Prolene size 3-0 with a sublabial suture.
Postoperatively the patient was kept on CPAP, then she was shifted to a high-flow nasal cannula a few days later. Normal saline drops through the stents every 4 h, and suction through the stent was performed. The stents were removed on day 11, and the patient was on a high-flow nasal cannula with a patent nasal airway bilaterally. The patient was administered neomycin and polymyxin B sulfate and dexamethasone nasal drops every 8 h. On further follow-up and flexible nasopharyngoscopy of the patient, she continued to have a patent nasal cavity bilaterally, but was not weaned off oxygen due to her condition and bronchopulmonary dysplasia.
Patient 2
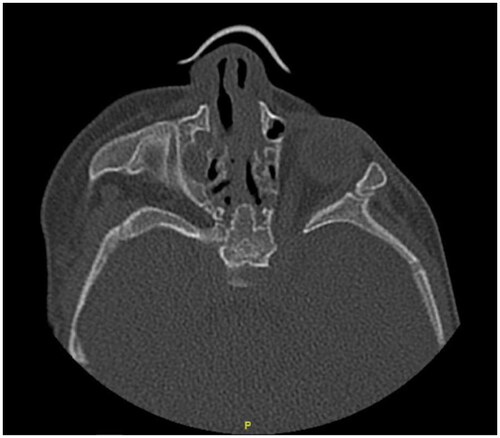
A 3-month-old preterm baby boy was delivered at 32 gestational weeks (35 days corrected age) due to oligohydramnios. The baby was admitted to the NICU for 18 days, with a history of 1-day intubation and prolonged nasogastric tube (NGT) in both nostrils. The patient was diagnosed to have a small atrial septal defect. The baby was then transferred to the neonatal high dependency unit for approximately 17 days, the NGT was removed, and the patient was discharged. The mother had recurrent urinary tract infections during pregnancy. The patient was presented to the pediatric otolaryngology clinic with unilateral nasal discharge and feeding concerns. In a detailed history from the parents, they reported left nasal obstruction and right nasal discharge, associated with on and off snoring and stertor, frequent left medial canthus secretions, prolonged feeding, frequent choking with milk. Normal crying and feeding, no cyanosis, stridor, recurrent upper respiratory tract infections, hearing issues, or ear discharge. On examination, the patient was a normal-looking child with no dysmorphic features. The patient’s weight was 3.4 kg (birth weight 1.7 kg), with no stridor, sleeping with his mouth closed, inhaling from his nose, and exhaling from his mouth. The flexible nasopharyngoscope was utilized, revealed adhesion at the level of the right middle turbinate; part of the nasopharynx can be seen. Also it showed DNS to the left side, for which the scope could not pass further in the left side. CT scan PNS showed right nasolacrimal duct cyst, anterior DNS to the left, thick vomer, and patent choana (Figure ).
Figure 2. CT PNS axial cut of patient 2: showing left side deviated nasal septum with minimal adhesions on right side.
The patient was taken to the operating room and underwent an endoscopic nasal examination, which confirmed the previously mentioned CT findings. Balloon septoplasty was performed, along with nasolacrimal duct cyst marsupialization. Bilateral silastic sheets were applied, and bilateral stents with size 3 ETT were inserted and fixed with sublabial suture using Prolene 3-0.
Postoperatively, the patient was doing good in terms of feeding and breathing, and was discharged after 1 week of operation with bilateral nasal stents and silastic sheets on, he was prescribed neomycin and polymyxin B sulfate and dexamethasone nasal drops and normal saline drops. After 1 month, the patient was taken to the operating room again, in which the bilateral stents and silastic sheets were removed; the endoscopic nasal examination revealed improved DNS to the left, adhesions of the left middle turbinate to both the septum and the inferior turbinate, small band between the right middle turbinate and the septum, adhesion release was performed bilaterally. Mitomycin was applied on the left side, silastic sheet was inserted and secured on the left side. The patient was discharged the same day on neomycin and polymyxin B sulfate and dexamethasone and normal saline drops. The silastic sheet was removed 2 weeks postoperatively in the clinic. In subsequent follow-up visits, the family reported significant improvement in sleeping, feeding, and the patient gaining weight.
Discussion
In many studies, neonatal DNS prevalence ranges from 1% to 30%; most of these deviations will be spontaneously corrected within a few days of life. For those whose deviations are persistent, an intervention should be considered. As they are obligatory nasal breathers, nasal obstruction will have a considerable physiological, anatomical, cosmetic, and psychological impact [Citation2,Citation7]. Since there is no universal agreement on how and when to intervene, many authors described different approaches and techniques, from observation to conventional septoplasty. Pooniya and Pandey reported a conservative measure of the neonate with right septal deviation with placement of the size 3 ETT on the more patent side (left), intermittently removed for a progressively increasing duration and removed completely at the age of 3 weeks, and the septal deformity corrected spontaneously; however, they did not mention the presence of subluxation of the septum from the maxillary crest [Citation9].
Two neonates in the Ochnser clinic underwent closed reduction under general anesthesia; to achieve patent airway, Asch forceps, Cottle, and Goldman elevators were used to manipulate the septum back to the midline. The intervention was performed at 14 days of life and 3 days of life for Patient 1 and Patient 2, respectively. The fashioned Telfa packing was inserted into the deviated side for stenting and removed on day 5 postoperatively; both experienced good feeding, no more snoring or stertor, and satisfactory cosmetic appearance [Citation2]. In one study, they successfully corrected 54 out of 63 patients (9 patients with irreplaceable deformity) using Sulsenti’s forceps immediately after birth. Approximately 13 years of follow-up after reduction in 49 children, of which 40 had good anatomical and functional results. Moreover, Metzenbaum considers that an intervention should be performed within the third week of life [Citation7]. Delayed intervention is difficult and often unsuccessful due to the production of fibrous tissue.
Gray states that the deviation becomes much greater with subsequent growth of the nose and recommends immediate treatment [Citation5,Citation6]. Emami reported one patient (8 days old) product of prolonged labor and vaginal delivery presented with external nasal deformity and cyanosis during agitation and feeding. Polysomnography revealed 36 episodes of oxygen desaturation to SaO2 73% in 4-h of monitoring. The patient underwent flexible and rigid laryngoscopy, bronchoscopy, and esophagoscopy, which did not reveal any significant anomalies; it also revealed that the patient had DNS to the left. The patient then underwent limited transnasal septoplasty with minimal resection of the cartilage and repositioned of the cartilage over the maxillary crest with endotracheal stenting size 3. Follow-up after 1 year revealed normal nasal growth and a well-developed healthy child [Citation1].
Conclusion
Neonatal DNS is a frequent finding in newborns. Since they are obligate nasal breathers, it can lead to troublesome consequences. Several approaches have been deployed for neonatal DNS, ranging from observation to conventional septoplasty. This study presents a novel, minimally invasive technique. The two cases presented here have shown improvements in nasal breathing, oxygen requirements, and feeding, with no observed complications.
Ethical consideration
Patients’ parents were informed and consented. No patients’ identifications were exposed.
Disclosure statement
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Emami AJ, Brodsky L, Pizzuto M. Neonatal septoplasty: case report and review of the literature. Int J Pediatr Otorhinolaryngol. 1996;35(3):271–275. doi:10.1016/0165-5876(95)01306-7.
- Lawlor CM, Grant M, Levy J, et al. Neonatal nasal septal deviation: two cases of successful early surgical intervention. www.entjournal.com.
- Hamid OA. Deviated nasal septum in Saudi newborns. Ann Saudi Med. 1990;10(3):293–295.
- Kawalski H, Piewak S. How septum deformations in newborns occur. Int J Pediatr Otorhinolaryngol. 1998;44(1):23–30. doi:10.1016/s0165-5876(98)00036-6.
- Grayt LP. Septal and associated cranial birth deformities types, incidence and treatment*. Med J Aust. 1974;1(15):557–563.
- Tasca I, Compadretti GC. Immediate correction of nasal septum dislocation in newborns: long-term results. American J Rhinology. 2004;18(1):47–51. doi:10.1177/194589240401800110.
- Cashman EC, Farrell T, Shandilya M. Nasal birth trauma: a review of appropriate treatment. Int J Otolaryngol. 2010;2010:752974. doi:10.1155/2010/752974.
- Bhattacharjee A, Uddin S, Purkaystha P. Deviated nasal septum in the newborn-a 1-year study. Indian J Otolaryngol Head Neck Surg. 2005;57(4):304–308.
- Pooniya V, Pandey N. A novel approach to treatment of symptomatic deviated nasal septum in a newborn baby. Int J Pediatr Otorhinolaryngol Extra. 2012;7(3):147–148. doi:10.1016/j.pedex.2012.06.003.
- Smith MM, Ishman SL. Pediatric nasal obstruction. Otolaryngol Clin North Am. 2018;51(5):971–985. doi:10.1016/j.otc.2018.05.005.
- Agha RA, Franchi T, Sohrabi C, SCARE Group., et al. The SCARE 2020 guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int J Surg. 2020;84:226–230. doi:10.1016/j.ijsu.2020.10.034.
