ABSTRACT
Hand, foot, and mouth disease (HFMD) is a public health issue in Haiphong, as it is in Vietnam overall. In 2011, a large outbreak of HFMD in Vietnam resulted in 113,121 children seeking medical attention, of whom 170 died. According to a Vietnam General Department of Preventive Medicine report in 2012, HFMD has the 2nd highest incidence of pediatric disease among 10 common diseases. There were 157,654 cases, of which 45 patients died, ranking 3rd among Vietnamese children’s causes of death. In 2017, HFMD broke out again in Haiphong. Haiphong Children’s Hospital (HCH) is the only hospital in Haiphong to examine and treat HFMD for children. This study aims to describe the clinical characteristics of HFMD seen in HCH and review the results of disease control efforts in 2017. A retrospective descriptive study. Clinical data were obtained by reviewing the patients’ case records from January 2017 through December 2017 in HCH. There were 2610 patients admitted to HCH in 2017. Most patients were under 3 years old (94.8%). The disease prevalence increased from April 1st through September 30th. Common symptoms were: fever (99%), mouth ulcers, sore throat (96.4%), rash on hand and foot (64.4%), startle (33.9%). Diagnosis mainly was clinical-grade 2a (79.8%). PCR was performed in 526 patients with grade 2b, 3, 4, and 218 cases (41.4%) were positive with EV71. Most of the cases’ prognosis was excellent, with 99.3% of cases cured and no deaths. Despite stringent measures taken in kindergartens, it is clear that HFMD is currently a public health problem in Vietnam. It is a highly contagious infectious disease, including several potential complications, and results in a number of cases leading to death. The disease is a particular cause of concern, especially when HFMD cases can overload already crowded hospitals. A high degree of vigilance should be maintained over the disease and its consequences.
Background
Hand, foot, and mouth disease (HFMD) is a syndrome caused by a group of intestinal viruses belonging to the family Picornaviridae. In particular, the leading cause of the clinical disease is caused by two groups of Coxsackie A and Enterovirus. EV71 is of the most concern because it can cause serious complications leading to rapid death, especially in young children (Chan et al., Citation2003). HFMD is usually manifested by symptoms such as fever, skin eruptions on hands and feet, vesicles in the mouth, etc … (H. Zhou et al., Citation2012). The world’s first reported outbreak of HFMD caused by EV71 occurred in Sarawak province (Malaysia) in 1997, resulting in 31 deaths. In 1998, a major epidemic of HFMD in Taiwan caused 1.5 million infections, and 405 children had severe complications (Chen et al., Citation2007). In 2009, an outbreak in mainland China resulted in 1,155,525 cases, including 13,810 severe cases and 353 deaths. Outbreaks have been reported in other countries in the Western Pacific Region, including Australia, Brunei Darussalam, Japan, Malaysia, Mongolia, the Republic of Korea, Singapore, and Vietnam (World Health Organization – Western Pacific Region, Citation2011). In 2012, the Ministry of Health outbreak in Cambodia reported an outbreak of severe illness with high mortality. Between April and July 2012, 78 children were affected, 54 of whom died (Sabanathan et al., Citation2014). According to a WHO report dated July 13th, 78 cases in 14 provinces in Cambodia had been identified since April of that year, mostly in children under 3 years. Most died within a day of hospital admission, causing public panic and international concern. Based on the latest laboratory results, a significant proportion of the samples tested positive for enterovirus 71 (EV-71), which also causes HFMD (WHO, Citation2012). In Vietnam, HFMD broke out nationwide in 2011 with a high number of infected children and deaths. It was widespread in cities, occurring in every province, with a national toll of 113,121 cases and 170 deaths recorded (Nguyen et al., Citation2014). The highest incidence of morbidity and mortality occurred in the southern provinces because Southern provinces’ mean air temperature was always higher than other provinces (Nguyen et al., Citation2014). In Vietnam, as of December 2017, the cumulative number of hospitalised paediatric patients with HFMD in 63 provinces was 48,009 (WHO, Citation2018).
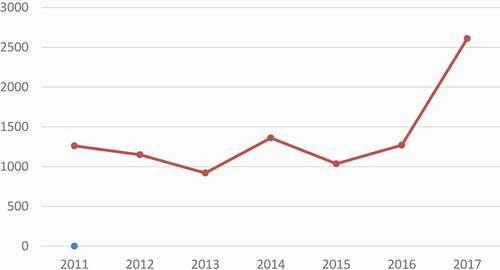
HFMD broke out again in Haiphong city in 2017 and that year experienced a noticeable increase to above 2500 cases in the number of HFMD patients (see ). Our research’s objective was to describe the clinical characteristics of HFMD in Haiphong Children’s Hospital and the result of disease control efforts in 2017.
Methods
We conducted a retrospective descriptive study of 2610 cases with HFMD admitted to Haiphong Children’s Hospital in 2017 – accounting for 5.32% of children with HFMD hospitalised in Vietnam. HFMD cases were defined according to the Vietnam Ministry of Health guidelines (Vietnam Ministry of Health, Citation2011).
Patients were classified into five grades of illness at the time of admission, from mild to severe, according to clinical management guidelines produced by the Vietnam Ministry of Health (Vietnam Ministry of Health, Citation2011). The five grades of illness were outlined in the guidance of the Vietnam Ministry of Health (see ).
Table 1. The five grades of illness were outlined in the guidance of the Vietnam Ministry of Health
The following data were included: age, gender, residence, seasonality (see ), clinical symptoms, laboratory test results, clinical grade at hospital admission, days of hospitalisation, and treatment outcome. The Data collection form was used to gather all of the information (see Appendix). Following the Ministry of Health’s guidance in Vietnam, there is no specific treatment for HFMD, only supportive treatment; close monitoring, early detection, and treatment of complications; ensuring adequate nutrition to improve children’s health. A standard form was used to collect the information from medical records. We reviewed all data entered from medical records for accuracy and completeness.
Table 2. Demographic characteristics of HFMD hospitalised in Haiphong Children’s Hospital in 2017
Table 3. Percentage of HFMD hospitalised by season
Type of residence
Rural (defined as children living in communes in rural districts) including Vinh Bao, Tien Lang, An Duong, Thuy Nguyen, Cat Hai, Bach Long Vi, An Lao, Kien Thuy. Urban (defined as children are living inwards in urban districts) including Ngo Quyen, Le Chan, Hong Bang, Hai An, Kien An, Duong Kinh, Do Son
The study was approved by the Medical Ethics Council of Haiphong University of Medicine and Pharmacy and Haiphong Children’s Hospital. All patients and families agreed to participate in the study.
Results
In 2017, there were 2610 children with HFMD admitted to Haiphong Children’s Hospital.
shows that most HFMD cases were in the age group under 36 months. The group of 12–24 months had the highest frequency (45.1%).
showed that HFMD most commonly appears in summer and autumn. Few cases were occurring in winter.
shows that most of the patients with HFMD had clinical classification grade 2a (79.1%).
Table 4. Clinical classification of HFMD at Haiphong hospital admission
showed that most paediatric patients hospitalised had symptoms of fever, mouth ulcers, sore throat, and hand – food rash (see ). Only a small number of patients had convulsions or myoclonic jerks.
Table 5. Common clinical symptoms of HFMD
Laboratory diagnosis
PCR assays for the detection of EV71 were conducted at Haiphong Children’s Hospital laboratory. Of 526 children with HFMD of grade 2b and above, up to 218 (41.4%) cases were diagnosed EV71-positive.
The results of showed that although the number of patients with HFMD in 2017 was about 2 times higher than in 2011, the proportion of children with severe illness (from level 2b and above) was lower than in the year 2011 (p < 0.05).
Table 6. Comparing the clinical grade and the outcome of patients with HFMD in 2011 and 2017 at Haiphong Children’s Hospital
There is no specific treatment for HFMD. Patients are encouraged to drink lots of water, plus they receive symptomatic treatment of fever and pain from ulcers as required. As a result of treatment in 2017, the percentage of completely cured children was significantly higher, but the length of hospitalisation was shorter than for the children treated in 2011. There were no deaths in either year.
Discussion
In 2017, a total of 12,140 patients with HFMD visited Haiphong Children’s Hospital. Of these, 2610 patients were hospitalised. The number of patients with HFMD in 2017 was nearly 3.2 times higher than in 2011. The number of inpatients increased by 2.3 times as compared to those in 2011. This suggests that HFMD is becoming more widespread and more challenging to control. Among these 2017 patients, there were 1595 boys (61.1%) and 1015 girls (38.9%); the male to female ratio was 1.57:1. This ratio was in keeping with the previous reports from outbreaks in Taiwan, Singapore, southern Vietnam, and China. Those previous reports showed a male/female ratio ranging from 1.5:1 to 2.5:1 (Chan et al., Citation2003; Chen et al., Citation2007; Van Hoang et al., Citation2019; Xu et al., Citation2018). The proportion of patients with HFMD living in rural areas (45.7%) was lower than patients living in urban areas (54.3%). The urban to rural ratio was 1.19:1 (p < 0.001). Our finding was quite consistent with the study of Z. M. Zhou et al. (Citation2016) in Wenzhou, China. In that study, the authors observed that a highly dense population was associated with a higher risk for HFMD spreading. Thus, areas with high population density need to be monitored more closely for HFMD (Citation2016).
The age group of HFMD patients was mainly concentrated in the age group under 36 months; the age group from 12 to 24 months accounted for the highest proportion (45.1%). This figure was entirely consistent with the study of Xu L et al. (2018) in Qinghai, China. In that study, 67% of children with HFMD were under 36 months of age (Xu et al., Citation2018). A previous study in Vietnam showed that 93.4% of children with HFMD were 3 years old or younger (Van Pham et al., Citation2017).
In recent years, global efforts have been made to identify the mechanisms facilitating the continuous HFMD outbreaks. Evidence of the seasonality of HFMD has been found in studies from many countries. In countries with relatively higher latitudes, such as Finland and Japan, peaks of HFMD occur during the summer or autumn months (Blomqvist et al., Citation2010; Onozuka & Hashizume, Citation2011; Van Pham et al., Citation2017). These findings are consistent with our study; most cases occurred in summer and autumn, only a few cases in winter.
Regarding clinical grades of HFMD, our study showed that most of the children with HFMD had grade 2a (79.1%). No cases of grade 4 were recorded, perhaps due to timely treatment. Another report in Daklak Hospital, Vietnam, reported the same figure, with 681 (91.5%) cases classified as mild (1, 2a grades) and 63 (8.5%) cases as severe (grade of 2b, 3 and 4)” (Van Pham et al., Citation2017). This suggests that parents took note of previous outbreaks (2011) experiences and brought their children to visit the hospital in a more timely way. Most patients in Haiphong Children’s Hospital with HFMD had a fever, rash on hand or foot, mouth ulcers, and sore throat. Only a small number of patients had dangerous signs such as convulsions and myoclonus.
PCR assays for detecting EV71 were conducted for all the patients with grade 2b and above. Of these PCR tests, 218 cases (41.4%) were EV71- positive. Our result is relatively consistent with the study of Pham VH et al. in 2014 (Nguyen et al., Citation2014). They reported that 82% (84/103) of cases tested positive for EV71. In another study in Wenzhou, China (Xu et al., Citation2018), the authors found that EV71 was the most common strain for children with HFMD, and it often caused severe disease.
As reported from other research before, 1.1% of the patients had neurological or cardiopulmonary complications, 3% died. Overall, the case-fatality rate was 0.03% (n = 2457), and 93% of the laboratory-confirmed deaths (n = 1737) were associated with EV71 (Sabanathan et al., Citation2014). Most of the patients were cured, and there were no deaths in the 2017 outbreak. Previously, in 2011, there was an HFMD outbreak in Haiphong with 4220 visits, of which 1260 children were admitted to hospital, mainly at grade 2a, and 46 children had acute pulmonary oedema and required artificial ventilation. It can be said that this is an encouraging result in medical examination and treatment at Haiphong Children’s Hospital. Finally, HFMD is believed a disease with a good prognosis if it is promptly treated and well monitored.
This study has some limitations. First, the study only describes clinical and laboratory characteristics related to HFMD. The study has not yet provided epidemiological factors related to the severe condition of HFMD in order to be able to classify patients and appropriate handling attitude quickly. Second, it is a retrospective descriptive study collecting data from medical records, so we have no additional information about the patient’s condition after discharge.
Conclusions
Our study is the first to delve into the clinical and laboratory characteristics of HFMD patients in Haiphong. The results of the study showed that most patients with HFMD disease were under 3 years old. It also shows that the outbreaks commonly occur in summer and autumn from April 1st to September 30th. Common clinical symptoms and signs of patients with HFMD were: fever, mouth ulcers, sore throat, rash on the hands and feet, and startle in severe cases. The majority of hospitalised patients with HFMD were classified as grade 2a. Most of the patients with HFMD were cured, and there were no deaths.
The innovative contribution of research
Outbreak control measures are targeted at interrupting virus transmission from child to child, as well as through contact with contaminated surfaces (such as toys) or fomites. Therefore, health education messages that focus on personal hygiene and good sanitation should be given to parents, babysitters, and kindergarten staff. Despite stringent measures taken in kindergartens, HFMD is still a significant public health problem in Haiphong city.
A high degree of vigilance should be maintained over the disease situation.
It is imperative to follow up with hospitalised HFMD patients to recognise both its early signs and cardiopulmonary and neurological complications.
Disclosure statement
The authors declare that they have no competing interests.
Additional information
Notes on contributors
Sang Ngoc Nguyen
Associate Professor Sang Ngoc Nguyen is now a senior lecturer of the Pediatric Department, Haiphong University of Medicine and Pharmacy; Vice head of Department of Nephrology – Hematology – Endocrinology, Haiphong Children Hospital; Vice President of Vietnam Pediatric Uro – Nephrology – Dialysis and Kidney Transplant Association. He graduated from Hanoi Medical University in 1981 and completed a residency program in 1987 at the National Hospital of Pediatrics. Since 1988, he has been working as a lecturer for Haiphong University of Medicine and Pharmacy at the Pediatric Department. He completed the MSc program and received an MSc certificate at Hanoi Medical University in 1995. Awarded Ph.D. in Hanoi Medical University in 1999. Completed over 100 researches in different fields: Childhood diseases, Primary health care, Preventive health care, Medical education. Awarded the title of Associate Professor in 2005. Besides, Dr. Sang is an Honorary Associate Professor from the University of Sydney, Australia.
Chuc Van Dang
Associate Professor Chuc Van Dang was born in 1962 in Vietnam. He graduated from Hanoi Medical University as a Pediatrician, graduated from the University of Washington in 2002 as a Master of Public Health, graduated from Hanoi Medical University as Ph.D. in 2010. He is now responsible for the Pediatrics Department of Haiphong University of Medicine and Pharmacy. Up to now, he has been teaching and doing research and, at the same time, working at Haiphong Children Hospital for 36 years. Currently, he owns more than 100 scientific articles published in the country and 05 international articles and participates in editing 05 textbooks in the field of pediatrics. He has already participated in many seminars on medical teaching innovation in the country and overseas. In addition, he has had more than one year as FFI at Rouen Hospital in France.
Tham Thi Tran
Dr. Tham Thi Tran MD, Ph.D. graduated from Haiphong University of Medicine and Pharmacy, Vietnam in 2008. Then, she became a lecturer in the Pediatric Department at Haiphong University of Medicine and Pharmacy. She is also working for the Respiratory Department at Haiphong Children Hospital. In 2003, she completed her Pediatric Master Degree and International Postgraduate Pediatric Certificate (IPPC). She was awarded Ph.D. in Haiphong University of Medicine and Pharmacy, Vietnam, in 2021. She is young lecturer who has strong passion for scientific research, and has published over ten medical articles in Vietnam and international journals.
References
- Blomqvist, S., Klemola, P., Kaijalainen, S., Paananen, A., Simonen, M.-L., Vuorinen, T., & Roivainen, M. (2010). Co-circulation of coxsackieviruses A6 and A10 in hand, foot and mouth disease outbreak in Finland. Journal of Clinical Virology, 48(1), 49–54. https://doi.org/https://doi.org/10.1016/j.jcv.2010.02.002 PMID: 20189452
- Chan, K.P., Goh, K.T., Chong, C.Y., Teo, E.S., Lau, G., & Ling, A.E. (2003). Epidemic hand, foot and mouth disease caused by human Enterovirus 71, Singapore. Emerging Infectious Diseases, 9(1), 78–85. https://doi.org/https://doi.org/10.3201/eid1301.020112
- Chen, K.T., Chang, H.L., Wang, S.-T., Cheng, Y.-T., & Yang, J.-Y. (2007). Epidemiologic feature of hand, foot and mouth disease and herpangina caused by enterovirus 71 in Taiwan 1999-2005. Pediatric, 120(2), 244–252. https://doi.org/https://doi.org/10.1542/peds.2006-3331
- Nguyen, N.T., Pham, H.V., Hoang, C.Q., Nguyen, T.M., Nguyen, L.T., Phan, H.C., Phan, L.T., Vu, L.N., & Tran Minh, N.N. (2014). Epidemiological and clinical characteristics of children who died from hand, foot and mouth disease in Vietnam, 2011. BMC Infectious Diseases, 14(1), 341. https://doi.org/https://doi.org/10.1186/1471-2334-14-341
- Onozuka, D., & Hashizume, M. (2011). The influence of temperature and humidity on the incidence of hand, foot, and mouth disease in Japan. Science of the Total Environment, 410-411, 119–125. PMID: 22014509. https://doi.org/https://doi.org/10.1016/j.scitotenv.2011.09.055
- Sabanathan, S., Tan, L.V., Thwaites, L., Wills, B., Qui, P.T., & Rogier van Doorn, H. (2014, June). Enterovirus 71 related severe hand, foot and mouth disease outbreaks in South-East Asia: Current situation and ongoing challenges. Journal of Epidemiology and Community Health, 68(6), 500–502. https://doi.org/https://doi.org/10.1136/jech-2014-203836
- Van Hoang, M.T.V., Nguyen, T.A., Tran, T.T., Vu, T.T.H., Le, N.T.N., Nguyen, T.H.N., Le, T.H.N., Nguyen, T.T.H., Nguyen, T.H., Le, N.T.N., Truong, H.K., Du, T.Q., Ha, M.T., Ho, L.V., Do, C.V., Nguyen, T.N., Nguyen, T.M.T., Sabanathan, S., Phan, T.Q., Nguyen Van, V.C., & van Doorn, H.R. (2019). Clinical and aetiological study of hand, foot and mouth disease in southern Vietnam, 2013-2015: Inpatients and outpatients. International Journal of Infectious Diseases, 80, 1–9. https://doi.org/https://doi.org/10.1016/j.ijid.2018.12.004
- Van Pham, H., Hoang, T.N.A., Duong, H.T., Phan, L.T., Phan, U.T.N., Ho, N.X., Hoang, C.Q. (2017). Clinical characteristics of hand, foot and mouth disease in Daklak Province, Vietnam and associated factors of severe cases. Indian Virological Society, VirusDisease, 28, 430–433. DOI:https://doi.org/10.1007/s13337-017-0402-8
- Vietnam Ministry of Health. (2011). Guideline for hand – Foot – Mouth disease management. http://benhviennhitrunguong.org.vn/huong-dan-chan-doan-dieu-tri-benh-tay-chan-mieng.html
- WHO. (2012). Undiagnosed illness in Cambodia – Update. https://www.who.int/csr/don/2012_07_09/en/
- WHO. (2018). Hand, foot, and mouth disease situation update number 530. https://iris.wpro.who.int/bitstream/handle/10665.1/14191/HFMD-20180102.pdf
- World Health Organization - Western Pacific Region. (2011). A guide to clinical management and public health response for hand, foot and mouth disease (HFMD). http://www.wpro.who.int/emerging_diseases/documents/HFMDGuidance/en/
- Xu, L., Shi, Y., Rainey, J.J., Zhang, Z., Zhang, H., Zhao, J., Li, Y., Rao, H., Li, Y., Liao, Q., & Ma, Y. (2018). Epidemiological features and spatial clusters of hand, foot, and mouth disease in Qinghai Province, China, 2009–2015. BMC Infectious Diseases, 18(1), 624. https://doi.org/https://doi.org/10.1186/s12879-018-3509-7
- Zhou, H., Guo, S.Z., Zhou, H., & Zhu, Y.F. (2012, April). Clinical characteristics of hand, foot and mouth disease in Harbin and the prediction of severe cases. Chinese Medical Journal, 125(7), 1261–1265. PubMed PMID: 22613598, https://insights.ovid.com/pubmed?pmid=22613598.
- Zhou, Z.-M., Yi, X., Cai-Song, H., Qiong-Jiao, P., Jing-Jiao, W. (2016). Epidemiological features of hand, foot and mouth disease during the period of 2008–14 in Wenzhou, China. Journal of Tropical Pediatrics, 2017 Jun 1;63(3):182–188. DOI:https://doi.org/10.1093/tropej/fmw070
Appendix.
Data collection form
OTHER INFORMATION:
_____________________________________________________________
_____________________________________________________________
_____________________________________________________________
Completed by:
Name: ___________________________________________
Signature: ________________________________________
Date: ____________________________________________