Abstract
Correct mechanical alignment (180° hip-knee-angle (HKA)) may be difficult to obtain on a consistent basis in obese patients. This is a randomized controlled study comparing the post-operative coronal alignment in obese patients between two surgical total knee arthroplasty (TKA) techniques – conventional and computer assisted navigation. The primary outcome was the post-operative HKA. A total of 60 patients were assigned to undergo conventional total knee arthroplasty (30 patients) or computerized assisted stereotaxic navigation system with Bluetooth communication surgery (30 patients). One patient from the study group was excluded due to malfunction of the navigation system. Good quality x-rays were available in 57 patients. There was no difference between the groups. Post-operative HKA was 2.8° and 2.9° in the study and control groups, respectively (p = 0.87). In obese patients undergoing TKA, computerized navigation had no impact on post-op HKA.
Clincal Trial Registration Number: HMO 0092-13
Introduction
Obesity was declared a global epidemic in 2000 by the World Health Organization, affecting both developed and developing countries regardless of socioeconomic levels [Citation1]. It is estimated that in the year 2030 at least 40% of the US population will be obese (BMI >30), and greater than 10% will be severely obese (BMI > 40) [Citation2]. The combination of aging population with obesity epidemic will lead to an increased incidence of knee osteoarthritis in obese patients. Although post-operative results of knee arthroplasty may be similar for patients with high BMI [Citation3], they are at increased risk of complications such as wound complications, infection and medial collateral injury [Citation4]. Long-term survival of TKA may be related to correct prosthesis and knee alignment [Citation5]. Correct alignment may be more difficult to achieve in obese patients, where some of the anatomic landmarks are obscured by fatty soft tissue. Several studies showed the relation between increased BMI and malalignment causing increased risk of failure [Citation5–7].
The use of navigation systems in TKA have been shown to improve alignment and significantly reduce outliers [Citation8]. Thus, in this randomized controlled study, the main aim was to compare the coronal radiological outcome of implant placement in obese patients (BMI > 30) using computerized assisted stereotaxic navigation system with Bluetooth communication versus conventional instrumentation in total knee arthroplasty. We hypothesized that the use of CAS would achieve better coronal alignment in obese patients.
Material and methods
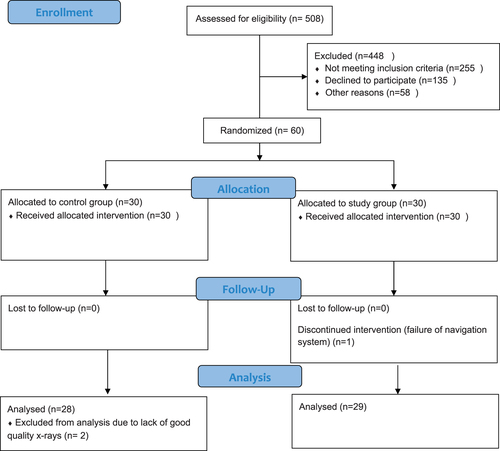
After obtaining approval from the ethical committee, we performed a randomized, controlled trial that compared CAS to conventional instrumentation in patients who underwent primary TKA. Sixty patients were enrolled; the study group consisted of 30 patients that underwent TKA with a computerized assisted stereotaxic navigation system with Bluetooth communication - the iAssist® Knee System (Zimmer Biomet CAS, Montreal, Canada), and 30 control patients that underwent TKA with conventional instrumentation. In both groups the Persona® (Zimmer Biomet, Warsaw, IN) knee prosthesis was used.
Inclusion criteria were patients that underwent primary TKA for the treatment of non-inflammatory degenerative joint disease, over 18 years old, and BMI ≥ 30. Exclusion Criteria were active infection, severe hip arthrosis, neurological and vascular disorders, previous ipsilateral knee surgery, hip or knee ankyloses, collateral ligament insufficiency and cancer.
The study workflow is depicted in the attached CONSORT flow chart ().
Patients who had appropriate indication to be candidates for TKA and who met the specified inclusion and exclusion criteria, were informed about the CAS and offered entry into the study. Informed consent was obtained from all patients and randomization then occurred. The randomization process is discussed further under the randomization procedure.
Surgical technique
All surgeries were performed by one of four surgeons well versed in the navigation system. (GR, YM, LK and ML).
Regional anesthesia was used in 50 patients and general anesthesia in 10 patients ().
Table 1. Study demographics.
In all arthroplasties, a medial parapatellar approach was used under tourniquet without patella eversion. Patellae were not resurfaced. A posterior cruciate sacrificing knee implant was used in all cases.
The surgical technique of the study group consisted of navigated distal femoral and proximal tibia cuts. In the femoral side, the point of entry to the medullary canal was identified and a short rod was attached to it without piercing the medullary canal. A position sensor (pod) was attached to the rod and a conical shape movement of the thigh allowed the navigated system to identify the physiological femoral center of rotation. A second pod was then attached to a cutting guide assembly and a perpendicular plane to the coronal mechanical axis was identified. The aim was for a distal femoral cut perpendicular to the mechanical axis with 3 degrees of flexion in the sagittal plane. The rest of the femoral preparation was completed with a 4-in-1 technique setting external rotation at 3 degrees compared to the posterior condylar axis. For the tibial proximal cut an extramedullary type construct with a pod connected to it was attached to the malleoli and the tibial surface over the PCL attachment point. Medial and lateral movement of the knee was used to set the tibial mechanical alignment. A cutting guide apparatus was attached to the proximal tibia medial to the tibial tubercle with a second pod connected. After the mechanical alignment was obtained the first pod was also attached to the cutting guide assembly with an aim of a cut perpendicular to the coronal mechanical axis with a 3 degrees posterior slope in the sagittal plane.
Conventional surgical technique consisted of an intramedullary femoral alignment jig set at 5 degrees valgus cut and extramedullary tibial alignment aimed at 90 degrees coronal plane cut and a 3 degrees posterior slope in the sagittal plane.
The tourniquet was deflated after skin closure.
All patients were treated with low molecular weight heparin (LMWH) 40 mg daily from post-operative day (POD) 1. Full weight bearing was encouraged with a plan for home discharge.
Radiographic measurements
Full-length standing anteroposterior radiographs were collected from all patients pre-operatively and at 6-weeks post-operatively. All x-rays collected were performed with the same technique of bipodal standing with no hip rotation and patella facing forward. The change in alignment of the knee and the position of the tibial and femoral components were measured from these films. The mechanical axis is defined as the axis of the lower limb with its proximal extremity at the center of the femoral head and its distal extremity at the center of the ankle. The femoral mechanical axis is defined by the center of the femoral head and the center of the knee (the center of the knee being the center of the medial shaft in the intercondylar notch of the femur or femoral component). The tibial mechanical axis is defined by the center of the ankle and the middle of the tibia plateau.
The study endpoints consisted of several different angles which were monitored to evaluate the lower limb alignment. They are as follows:
Primary outcomes
The hip-knee-ankle (HKA) angle – the angle between the femoral and tibial mechanical axis. The primary criterion is that HKA should be in the range 180°±3°, which is considered a correct position of the prosthesis.
Secondary outcomes
For easier calculations we used mechanical medial femoral distal angle (mMDFA), as described by Hirschmann et al. [Citation9] the medial angle formed between the mechanical femoral axis and the axis connecting most distal points of the medial and lateral femoral condyles.
Mechanical medial proximal tibial angle (mMPTA) – the medial angle formed between the mechanical tibial axis and the tibial tangent in the native knee. In the operated knee the tibial proximal angle is formed by the mechanical axis and the axis of the lower border of the tibial tray.
Randomization procedure
A random number series was generated and assigned with a unique number. Envelopes labeled with the patient’s randomization number contained a sticker inside identifying the randomization group. The surgeon was provided with the envelopes and instructions for using them before the start of the study.
Prior to surgery, the envelope that contained the patient’s randomization number and treatment assignment to one of the two groups – either the study group or the control group. The randomization envelopes were used in sequential order of patient enrollment.
Between June 1st 2015 and January 25th 2017 a total of 508 TKAs were performed. Of these, 253 had a BMI > 30. Sixty-four patients were excluded and 129 refused to participate in the study.
Statistical analysis
A sample size of 30 patients in each group was calculated to detect a difference of 3 degrees between groups by the primary endpoint (HKA angle), with alpha of 0.05 and power of 0.9. From previous studies we know that standard deviation in postoperative HKA angle is around 3 degrees, and multiple studies have shown that deviation of 3 degrees is clinically important [Citation6,Citation10,Citation11]. As we believe the navigation will provide a benefit in this population, we considered a 3% difference as a conservative estimate. Independent samples, two-tailed, t-test was used for comparing different angles between the two groups and a Fischer’s exact test was used for comparing the number of outliers. Significance was assessed at the 0.05 level. Excel software (Microsoft, Redmond Washington) was used for statistical analysis.
Results
Out of 60 surgeries performed, one patient of the study group was excluded due to malfunction resulting in a wrong distal femur cut, navigation was aborted and surgery was completed using conventional technique. Data from the navigation pods were analyzed by the developing team of the manufacturer but the reason for the misguidance was not found, neither in the surgical technique nor in the pods themselves.
Complete data with good quality x- rays was available from 57 operations, 29 in the study group and 28 in the control group.
Data of preoperative and post operative coronal angles are listed in .
Table 2. Radiographic measurements.
Outliers were defined as angles deviating more than 3° from the desired 90° in both femur and tibia coronal alignment. Outliers in the medial distal femoral angle were seen in 8 patients in the control group compared to 5 in the study group (p = 0.358). Proximal medial tibial angle outliers were seen in 3 patients in the control group and none in the study group (p = 0.11). There was no difference between the two groups in outliers regarding HKA (p > 0.99).
Discussion
In our randomized control trial we showed that good coronal alignment can be achieved in obese patients using both CAS and conventional surgical techniques. There was no significant difference between both groups regarding post-operative coronal alignment. This was true for overall alignment (HKA) and specifically for the femoral component and the tibial component alignment.
The most common cause for late revision (more than 2 years from index surgery) is aseptic loosening [Citation12]. Finite element analysis studies showed deviations from mechanical alignment leads to increased and asymmetric pressures mainly on the tibial interface which may lead to loosening [Citation10,Citation13]. Fang et al. showed increased risk of loosening when the HKA alignment exceeds 2.4 degrees of varus and 7.2 degrees of valgus [Citation5]. Computerized assisted surgery (CAS) is considered to improve coronal alignment and reduce the outliers [Citation8,Citation14–16]. Obese patients have a higher risk of developing knee osteoarthritis [Citation17,Citation18]. TKA in these patients is more technically demanding with a higher complication rate both intraoperatively such as medial collateral damage and in the early post-operative period such as wound problems and infections [Citation19–21]. Still, other studies show a relation between higher BMI and poor coronal alignment [Citation7,Citation22]. The combination of increased weight and poor alignment may cause unbalanced pressure on the prosthesis-cement-bone interface leading to early loosening. Therefore, obese patients may prove to be a group of patients more likely to benefit from CAS TKA. From previous studies, we know that with standard instrumentation, the amount of outliers varies and may be as high as 30% [Citation5,Citation23,Citation24].
Although we used computerized randomization the two groups had slight difference between them. The average age of the control group was 70.1 compared with 66.9 in the study group (p = 0.014). There was no difference in BMI between the groups (p = 0.265).
Patients in the control group had a higher preoperative HKA than patients in the study group (12.3° vs 8.9°) yet both groups were corrected to a non statistically and clinically significant HKA (2.9° and 2.8°).
Navigated surgical technique increased the mean surgical time by only 7 min which is not clinically significant and was not statistically significant.
There are several limitations to our study. The power analysis was calculated for the difference in the coronal alignment. With regards to outliers, the groups may have been too small, limiting our ability to reach statistical significance.
We used BMI > 30 as an inclusion criteria and a mean BMI of approximately 35. Only 7 patients were morbidly obese with BMI > 40 (5 in the study group and 2 in the control group) limiting our ability to extrapolate conclusions to that very important group of patients.
In our institute we use bipodal long AP radiographs to evaluate HKA. This technique has inherent limitations with standardization [Citation25] and also with the accuracy of 1 to 2 degrees (Skyta et al.). [Citation26] To overcome this limitation in further studies it would be prudent to use CT scan and EOS (EOS imaging, France)
This navigation system is useful only with regards to coronal alignment. It lacks the possibility to determine correct femoral rotation. Determining femoral rotation in our study was done with the conventional 3° external rotation. Digital accessories for correct femoral external rotation position are available.
Conclusion
In obese patients undergoing TKA, good coronal alignment can be achieved both in conventional technique and navigation assisted surgery. The use of navigation did not show significant differences in achieving good coronal alignment.
Ethical approval
Ethical Review Board: Our institutional review board approved this study
Trial registration ID: CLINCAL TRIAL REGISTRATION NUMBER: HMO 0092-13
Informed consent was obtained from all patients and randomization then occurred.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World health organ tech rep ser. 2000.
- Finkelstein EA, Khavjou OA, Thompson H, et al. Obesity and severe obesity forecasts through 2030. Am J Prev Med. 2012;42(6):563–570.
- Singh JA, Gabriel SE, Lewallen DG. Higher body mass index is not associated with worse pain outcomes after primary or revision total knee arthroplasty. J Arthroplasty. 2011;26(3):366–374.e1.
- Winiarsky R, Barth P, Lotke P. Total knee arthroplasty in morbidly obese patients. J Bone Joint Surg Am. 1998;80(12):1770–1774.
- Fang DM, Ritter MA, Davis KE. Coronal alignment in total knee arthroplasty: just how important is it. J Arthroplasty. 2009;24(6 Suppl):39–43.
- Ritter MA, Davis KE, Meding JB, et al. The effect of alignment and BMI on failure of total knee replacement. J Bone Joint Surg Am. 2011;93(17):1588–1596.
- Estes CS, Schmidt KJ, McLemore R, et al. Effect of body mass index on limb alignment after total knee arthroplasty. J Arthroplasty. 2013;28(8 Suppl):101–105.
- Chin PL, Yang KY, Yeo SJ, et al. Randomized control trial comparing radiographic total knee arthroplasty implant placement using computer navigation versus conventional technique. J Arthroplasty. 2005;20(5):618–626.
- Hirschmann MT, Moser LB, Amsler F, et al. Functional knee phenotypes: a novel classification for phenotyping the coronal lower limb alignment based on the native alignment in young non-osteoarthritic patients. Knee Surg Sports Traumatol Arthrosc. 2019;27(5):1394–1402. Epub 2019 Apr 11. PMID: 30976825.
- Perillo-Marcone A, Barrett DS, Taylor M. The importance of tibial alignment: finite element analysis of tibial malalignment. J Arthroplasty. 2000;15(8):1020–1027.
- Jeffery RS, Morris RW, Denham RA. Coronal alignment after total knee replacement. J Bone Joint Surg Br. 1991;73(5):709–714.
- Sharkey PF, Lichstein PM, Shen C, et al. Why are total knee arthroplasties failing today – has anything changed after 10 years? J Arthroplasty. 2014;29(9):1774–1778.
- Innocenti B, Bellemans J, Catani F. Deviations from optimal alignment in TKA: is there a biomechanical difference between femoral or tibial component alignment? J Arthroplasty. 2016;31(1):295–301.
- Bäthis H, Perlick L, Tingart M, et al. Alignment in total knee arthroplasty. J BONE Jt Surg. 2004;86(5):7.
- Brin YS, Nikolaou VS, Joseph L, et al. Imageless computer assisted versus conventional total knee replacement. A bayesian meta-analysis of 23 comparative studies. Int Orthop. 2011;35(3):331–339.
- Chen JY, Chin PL, Tay DKJ, et al. Less outliers in pinless navigation compared with conventional surgery in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2014;22(8):1827–1832.
- Felson DT, Anderson JJ, Naimark A, et al. Obesity and knee osteoarthritis. The framingham study. Ann Intern Med. 1988;109(1):18–24.
- Coggon D, Reading I, Croft P, et al. Knee osteoarthritis and obesity. Int J Obes Relat Metab Disord. 2001;25(5):622–627.
- Winiarsky R, Barth P, Lotke P. Total knee arthroplasty in morbidly obese patients. JBJS. 1998;80(12):1770–1774.
- Kerkhoffs GMMJ, Servien E, Dunn W, et al. The influence of obesity on the complication rate and outcome of total knee arthroplasty. J Bone Joint Surg Am. 2012;94(20):1839–1844.
- Järvenpää J, Kettunen J, Kröger H, et al. Obesity may impair the early outcome of total knee arthroplasty a prospective study of 100 patients. Scand J Surg. 2010;99(1):45–49.
- Krushell RJ, Fingeroth RJ. Primary total knee arthroplasty in morbidly obese patients: a 5- to 14-Year follow-up study. J Arthroplasty. 2007;22(6 Suppl 2):77–80.
- Mahaluxmivala J, Bankes MJK, Nicolai P, et al. The effect of surgeon experience on component positioning in 673 press fit condylar posterior cruciate-sacrificing total knee arthroplasties. J Arthroplasty. 2001;16(5):635–640.
- Dennis DA, Channer M, Susman MH, et al. Intramedullary versus extramedullary tibial alignment systems in total knee arthroplasty. J Arthroplasty. 1993;8(1):43–47.
- Cooke TD, Sled EA, Scudamore RA. Frontal plane knee alignment: a call for standardized measurement. J Rheumatol. 2007;34(9):1796–1801.
- Skyttä ET, Haapamäki V, Koivikko M, et al. Reliability of the hip-to-ankle radiograph in determining the knee and implant alignment after total knee arthroplasty. Acta Orthop Belg. 2011;77(3):329–335.