Abstract
Craniomaxillofacial (CMF) surgery is a challenging and very demanding field that involves the treatment of congenital and acquired conditions of the face and head. Due to the complexity of the head and facial region, various tools and techniques were developed and utilized to aid surgical procedures and optimize results. Virtual Surgical Planning (VSP) has revolutionized the way craniomaxillofacial surgeries are planned and executed. It uses 3D imaging computer software to visualize and simulate a surgical procedure. Numerous studies were published on the usage of VSP in craniomaxillofacial surgery. However, the researchers found inconsistency in the previous literature which prompted the development of this review. This paper aims to provide a comprehensive review of the findings of the studies by conducting an integrated approach to synthesize the literature related to the use of VSP in craniomaxillofacial surgery. Twenty-nine related articles were selected as a sample and synthesized thoroughly. These papers were grouped assigning to the four subdisciplines of craniomaxillofacial surgery: orthognathic surgery, reconstructive surgery, trauma surgery and implant surgery. The following variables – treatment time, the accuracy of VSP, clinical outcome, cost, and cost-effectiveness – were also examined. Results revealed that VSP offers advantages in craniomaxillofacial surgery over the traditional method in terms of duration, predictability and clinical outcomes. However, the cost aspect was not discussed in most papers. This structured literature review will thus provide current findings and trends and recommendations for future research on the usage of VSP in craniomaxillofacial surgery.
Background
Technology has been used in the medical field for standardization and predictability in results contributing to significant change in daily practice particularly in the surgical field. In surgery, advancements in technology are transforming how surgeons visualize, plan, make surgical implants and prototype models, and perform preoperative planning procedures. This is known as Virtual Surgical Planning (VSP) [Citation1–4] and is widely utilized in craniomaxillofacial (CMF) surgery among developing economies with the purpose of treating congenital and acquired conditions of the face and head. The surgical process comprises the perioperative period which consists of the preoperative, intraoperative, and postoperative periods [Citation1,Citation4–7]. VSP is a preoperative planning method that uses 3D imaging computer software to visualize a surgical procedure [Citation5,Citation8–11] and enables surgeons to predefine the steps in a surgical procedure. Performing craniomaxillofacial surgery is challenging and very demanding due to the complex anatomy of the facial region, having many vital organs and structures such as an intricate network of blood vessels and nerves, as well as the brain, eyes, nose and vital teeth [Citation10,Citation12,Citation13]. Presently, several tools and techniques are being used with the intent to control the activities in surgery and to successfully achieve the expected results. [Citation2,Citation14,Citation15]. VSP, computer-aided design (CAD), and computer-aided manufacturing (CAM) have revolutionized the planning process and are now established methods in craniomaxillofacial surgery. For this purpose, several surgical planning applications have recently been developed such as modeling and simulation software that enables clinicians to interact with patient-specific virtual models to simulate surgical procedures and improve planning. Studies revealed that the VSP components available to surgeons are three-dimensional virtual planning, stereolithographic models, intraoperative cutting guides, intraoperative dental splints and patient-specific implants [Citation8]. Furthermore, VSP has been widely implemented in craniomaxillofacial surgery and is commonly used in mandibular reconstruction, orthognathic surgery, maxillofacial trauma and temporomandibular joint reconstruction [Citation16,Citation17]. The usage of computer-assisted planning in surgery is intended to increase surgical accuracy, decrease operation time and produce consistent results.
VSP is prevalent in the primary reconstruction of craniofacial defects involving both maxilla and mandible [Citation3,Citation18–20]. Additionally, the technique has proven its benefits in mandibular reconstruction by optimizing the accuracy and operating time, as well as increasing the predictability of surgical outcomes [Citation1,Citation3,Citation15,Citation19,Citation21]. VSP tools are also used to design and manufacture surgical guides such as customized plates made of titanium, epoxide acrylate hydroxyapatite, hydroxyapatite or polyether ether ketone (PEEK) [Citation7,Citation21–25]. The custom-fitting surgical guide is created as a ‘bridge’ between virtual planning and surgery and eliminates the ‘guesswork’ intraoperatively [Citation11,Citation21,Citation26]. These tools have become widely accepted in many institutions and are commonly used in craniomaxillofacial surgery, aiding higher accuracy in translating the planned surgery to the operating room. Currently, some medical institutions outsource the performance of virtual surgical planning to private companies. This causes an inherent risk to patient information. [Citation2]. Another identified challenge in using VSP is the high processing costs, prolonged delivery time before surgery and time-consuming meetings with the partner company for the development of VSP [Citation2]. Virtual planning in surgery is becoming more popular; as with all new technologies, it has drawbacks such as high costs, planning time, preparation time and additional training [Citation4,Citation21]. VSP cannot guarantee successful surgical outcomes on its own and there are factors to consider where errors can occur at any point in the process. These include 3D integration with patient’s anatomical data, segment identification and mobilization, computer-aided surgical simulation, fabrication of splints and surgical guides, 3D image superimposition and occlusion determination in virtual space [Citation2,Citation3]. A thorough understanding of the sources of errors in VSP can lead to successful surgical outcomes whether the procedure is performed in-house or outsourced.
A growing number of studies have been published in recent years on virtual planning in surgery. A significant number of these publications compared virtual surgical planning to conventional surgical planning. Various studies explore VSP tools in manufacturing patient-specific surgical implants but such methods do not offer surgical flexibility that any changes to the surgical plan during the intraoperative period may result in the patient-specific implant being simply discarded [Citation3]. Thus, additional costs to patients and needing to iterate the work of the surgeons. Previous studies on the application of virtual planning in surgery have small sample sizes. Moreover, various studies provide insufficient insights from the users involved in utilizing VSP in craniomaxillofacial surgery, specifically only surgeons skilled in using modern medical technology [Citation27]. The degree of inconsistency found in the previous literature on the utilization of virtual surgical planning in craniomaxillofacial surgery prompted the development of this review. This paper aims to provide a comprehensive examination on the findings of the studies on the application of virtual surgical planning in craniomaxillofacial surgery by conducting an integrated approach in reviewing the literature related to the use of VSP in craniomaxillofacial surgery. A structured review method was used to explore and synthesize the current usage of VSP. This study will contribute to the existing knowledge by presenting an in-depth understanding on the current studies focused on the utilization of virtual surgical planning in craniomaxillofacial surgery. It will also provide an input and recommendations for future research to address gaps in the earlier studies.
Methodology
Literature Profile
Literature reviews serve as a foundation for all types of research, creating guidelines for policy and practice, providing evidence of an effect and if well conducted, having the capacity to engender new ideas and directions for a specific field. Thus, they provide the foundation for future research and theory [Citation28]. In addition, the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020, provides a set of items that are useful for reporting reviews that include synthesis such as pairwise meta-analysis or other statistical synthesis methods. [Citation29]. On account of this, shows that this structured review was conducted based on the guidelines provided by the PRISMA 2020 following an integrated approach to determine the sample literature included in the analysis [Citation18,Citation30,Citation31]. The articles considered and used in this review were extracted from two databases: PubMed and Mendeley, containing the keywords ‘virtual surgical planning’, ‘VSP’ ‘3D surgical planning’, searched combined with the terms ‘maxillofacial’, ‘craniofacial’, ‘maxillomandibular’, ‘craniomaxillofacial’, ‘CMF’, ‘head and neck surgery’, ‘implant surgery’, ‘trauma surgery’, ‘midfacial surgery’, ‘orthognathic surgery’, ‘reconstruction surgery,’ [Citation2,Citation15,Citation18,Citation32]. The selection of sample studies was limited to studies published between the year 2012 and 2022 to ensure that the study results of VSP utilization are novel. Non-English technical reports and literature reviews were excluded from the study. The initial search yielded 7486 potentially relevant studies, including 2200 and 5286 studies from PubMed and Mendeley, respectively. Related articles were retrieved only from these two databases to avoid duplication. Furthermore, an additional 27 articles were found after conducting a backward search to find related studies from the list of references cited by the articles initially retrieved. After removing 14 duplicate studies, 185 studies were compiled in a literature bank stored in a Google Drive after a review of the title and abstract. Subsequently, the remaining papers undergo a more in-depth review by examining the full introduction and conclusion sections. This step aims to identify whether the records provide relevant data on the utilization of virtual surgical planning in craniomaxillofacial surgery. During this phase, 114 papers were excluded as it became evident that some of the content did not align with the research question of this study, despite what the titles and abstracts suggested. Furthermore, duplicates were identified and removed, leaving only 60 papers for a comprehensive full-text assessment. These studies were further digested using the tool Journal Assessment Matrix (JAM) tabulating the literature’s title, publication year, authors, description, hypothesis, problem statement and objectives, methodology, results and discussion. The number of articles was reduced as the screening disqualified articles that did not meet the sample size criteria, narrowing the scope of the study papers. One paper is excluded because it is not written in English, and another one is excluded because it was published more than 10 years ago. The remaining papers are filtered to include only journal articles, excluding 25 papers from the list. Of these 25 papers, 4 are also not indexed by Scopus or Web of Science (WoS). Additionally, 4 more papers are not indexed by Scopus or WoS. In total, 8 journals are not indexed by Scopus or WoS. As a result, the total sample size was 29 studies.
After conducting a thorough review and synthesis of the sample literature, the next step is profiling these studies in order to develop an overview of their research background. The researchers tallied the literature’s publication year, country of study, research methods, author’s background and journal of publication to strengthen the study’s credibility [Citation1,Citation15]. The SCImago Journal Rank, in addition to the Web of Science and Scopus, was also used to verify the credibility of the journals providing additional information about the journal’s subject areas and categories.
Literature synthesis
This section describes the structured review analysis method for identifying groupings that will facilitate in understanding the utilization of VSP in craniomaxillofacial surgery. The researchers noticed patterns in the VSP literature and used the method described in [Citation32] to discuss in this paper the usage of VSP in craniomaxillofacial surgery by category. Historically, the four major areas of interest in craniomaxillofacial surgery are: pediatric craniofacial and orthognathic surgery, craniomaxillofacial trauma surgery, craniomaxillofacial reconstructive surgery, and craniomaxillofacial oncologic surgery. As a surgical field dealing mainly with rare pediatric craniofacial anomalies, CMF expanded to the management of facial trauma, tumor reconstruction and also esthetic surgery. Orthognathic surgery focuses on how the teeth fit together, normalizing facial proportions involving the jaw and also treating obstructive sleep apnea. The term implant surgery is usually associated with dental implant surgery, which deals with medical devices implanted into the jaw to restore the appearance of the teeth and the ability to chew.
After profiling the 29 studies included in the review, the papers were grouped into four subdisciplines related to craniomaxillofacial surgery as shown in : orthognathic surgery, reconstructive surgery, implant surgery and trauma surgery. An in-depth analysis was then conducted on the 29 journal articles on how VSP was utilized in each group. For orthognathic surgery, this was achieved by focusing on whether the paper used the VSP technique in the correction of jaw deformities and malocclusions that can affect a patient’s ability to chew, speak and breathe properly. Orthognathic surgery involves repositioning of the upper jaw, lower jaw, or both, to achieve the correct alignment and function of the teeth and jaw. [Citation2,Citation15,Citation16,Citation30,Citation33]. VSP can be used on the functions of orthognathic surgery such as creating a 3D model to help surgeons in making a diagnosis on the patient’s condition. Once the diagnosis is made, the 3D model created can also be used by the surgeons to plan a surgical procedure and lead other functions such as the fabrication of surgical guides and to predict the outcome of the surgery [Citation30,Citation34–36].
Reconstructive surgery in craniomaxillofacial surgery refers to a surgical procedure performed to restore the structure, function and appearance of the skull, face and jawbone. This type of surgery is often necessary for patients who suffered severe facial trauma, congenital anomalies or cancer of the head and neck. The goal of reconstructive surgery is to repair or replace damaged missing tissues, bones and organs and to create a more esthetically pleasing and functional appearance [Citation37–39]. VSP technology provides relevant assistance to reconstructive surgeons to make precise surgical planning in a virtual environment using advanced software to manipulate 3D images. These are adapted from the patient’s head and neck, allowing them to plan the precise location, size and shape of bone cuts, bone grafts and implant placement, reducing the likelihood of surgical errors [Citation10,Citation40, Citation41].
VSP technique in implant surgery is used to visualize the patient’s craniomaxillofacial anatomy in a 3D model to obtain a detailed visualization of the bones, soft tissues and other structures. Considering that each patient has a unique anatomy and has underlying medical conditions, a virtual model is beneficial for surgeons. This guides them to plan the placement and positioning of the implants, as well as the simulation of the surgery, to achieve desired outcomes and identify potential issues and adjust the plan as necessary [Citation39,Citation42,Citation43]. In craniomaxillofacial surgery, trauma surgery involves the management of injuries and fractures to the skull, face and jaw caused by accidents, falls, injuries and other forms of physical trauma. VSP in trauma surgery helps the surgeons to visualize the extent of the damage, plan the surgical approach and determine the optimal positioning of plates, screws and other implants. With the use of VSP, surgeons can create a 3D model of the patient’s craniomaxillofacial region and simulate the surgical procedure, allowing them to make adjustments and refine the plan before the operating room [Citation19,Citation44].
After profiling the literature, each article was then analyzed in detail and reports were recorded using a tally table. The researchers utilized a combination of inductive and deductive qualitative coding approaches to examine common themes and variables. Based on the outcomes of the initial tally, this paper decided to follow the approach used by several literature reviews and included the following variables: treatment time, accuracy of VSP, clinical outcome, cost, and cost-effectiveness [Citation1,Citation18,Citation25,Citation32]. The operating room time, or treatment time, refers to the time spent in the operating room and/or the overall duration of the treatment compared to the conventional method. The number of papers that reported time reduction, no difference in time, or time increase were recorded. The accuracy was assessed by comparing the virtual plan and postoperative results [Citation45], and by measuring the accuracy of anatomical models or surgical implants and guides on the printed part [Citation4]. For accuracy, the study recorded the number of papers that evaluated the effectiveness of VSP in surgery and classified them into three categories: better/good accuracy, average accuracy or bad accuracy. Clinical outcomes were assessed based on the quality of improvement, including precision and esthetics. The study likewise recorded the number of papers that reported an improvement, equal improvement compared to traditional methods, or resulted in a negative impact. Moreover, the study recorded the cost and cost-effectiveness variables if mentioned by the authors. Specifically, the papers were analyzed to determine whether VSP was cheaper, equally expensive or more expensive than traditional methods, and whether the use of VSP in craniomaxillofacial surgery was deemed cost-effective, neutral or not cost-effective. Finally, the study also recorded the number of papers that did not report results on any of the variables.
Research gap analysis
Identifying gaps in the existing literature on VSP in craniomaxillofacial surgery provides justification for future research projects in this field. Insufficient or missing information also limits the ability to reach a conclusion for specific questions regarding this discipline. Further surgical advancements and innovations can be achieved as gaps and rationale for more studies are sought.
This step involved surveying each conclusion and recommendation of the 29 journal articles and conducted inductive qualitative coding and then organized them into themes. Initial codes were subsequently generated from the groupings. These codes include keywords that are frequently mentioned in the conclusion and recommendation of each article. Codes were validated and finalized by thoroughly assessing the articles again on which codes made sense, and communicated relevant knowledge and information about VSP utilization in craniomaxillofacial surgery. Finally, results on these codes highlighted significant gaps in the literature related to VSP in craniomaxillofacial surgery.
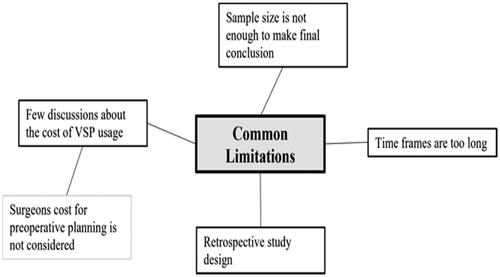
In this structured review analysis of the virtual surgical planning literature, several gaps were identified after a thorough synthesis of the sample: (1) insufficient discussion of cost considerations on the usage of VSP, (2) very few case subjects, and (3) the case time frame. The preceding issues will serve as a guide to discuss recommendations for future research.
Results
Literature Profile results
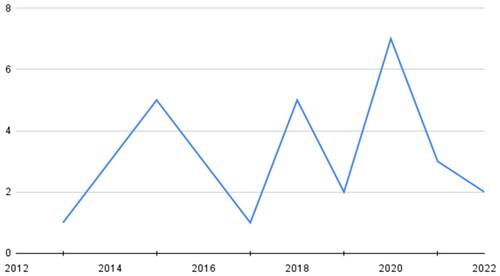
To analyze the sample articles, this study followed the approach of several review studies and focused on yearly publication trends, research methods, country of research setting, author background and journal of publication. illustrates the publication trend of sample studies related to VSP from 2013 to 2022. The oldest literature included in the sample dates back to 2013 and there is an irregular trend in VSP literature publications, suggesting that studies related to this field typically require several years to gather enough participants and months to observe and obtain sufficient results. Notably, 2020 had the highest number of publications (n = 7), but the number decreased in 2021 and 2022.
The small number of publications that exist for VSP is understandable and may have several implications. Foremost, the field of VSP is growing slowly and takes considerable time, as the long-term validation of a medical implant would be highly important. In addition, the smaller number of publications in 2021 and onwards are not exactly peculiar, as medical experts were preoccupied in the interim due to more pressing issues such as the COVID-19 pandemic.
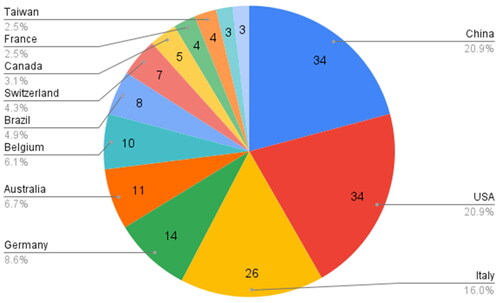
The sample size of literature for this review uses a variety of research methods, as no specific methods are excluded. The results are shown in where quantitative methods were used in 16 of the 29 sample studies from 13 different countries, primarily because most studies on virtual surgical planning attempt to test the accuracy, time and cost consumption of the technology. The rest used mixed methods, qualitative and case studies, and empirical research to investigate the effectiveness and describe the user experience with VSP [Citation10]. These mixed methods, including qualitative means, are not to be disregarded. Patient outcomes should center around the patient and their experiences are fairly difficult to quantify. Furthermore, the studies were identified based on where they were conducted, as reflected by the sample literature country setting. A total of six sample studies were conducted in China. As highlighted in the literature, China is one of the most advanced countries in the world in the clinical diagnosis and treatment of disease through oral and maxillofacial surgery (OMS). It also housed the largest number of OMS in Asia and has carried out a series of complex surgeries for years. [Citation46]. The rest of the studies were mostly conducted in the USA and some clinically advanced European cou ntries. There may be several factors at play. Primarily, any attempted research would have to be in a country with enough research interest and resources to attempt VSP procedures. Likewise, the low amount of research in smaller European countries might be attributed to their lower populations. It may be of value to future researchers to qualify insurance coverage as a further means to understand and anticipate VSP frequency.
The literature sample size was written by 163 authors from 13 different countries. shows that thirty-four of these authors resided in China, 34 were from the USA and 26 were from Italy. Furthermore, the majority of the authors are medical doctors with oral and maxillofacial surgery as their primary field of specialization, and subspecialized in other related fields such as plastic and reconstructive surgery, craniofacial surgery and orthognathic surgery. Numerous authors also earned a doctorate degree in philosophy and some have multiple degrees. Authors from the USA earned the most degrees and 23 of them have medical degrees. This was validated in the author’s websites, Google Scholar profiles, ORCID profiles, LinkedIn profiles, ResearchGate profiles and university as well as institutional official websites.
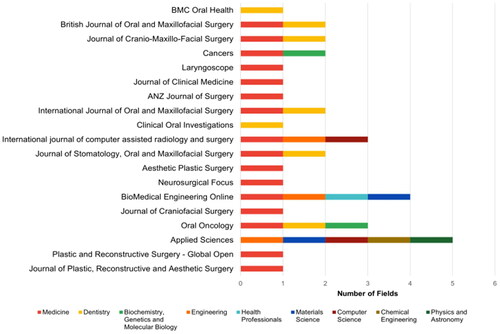
In addition to author’s profiling, sample literature was also profiled according to its journal of publication. The results are listed in where five among 29 articles were published in the Journal of Craniofacial Surgery and the leading subject area and category of these journals is medicine and surgery, respectively. However, only one of the following entries is a regional journal (ANZ Journal of Surgery) and the rest being subsets of the medical field. This shows two factors: (1) that the field of craniomaxillofacial surgery has ample journals that directly concern the field, and (2) that more than just medical field-specific journals are concerned with the rise of VSP.
Table 1. Journal and categories.
Applied Sciences, BioMedical Engineering Online, and Cancers are three journals that are not directly involved in the specific area of craniomaxillofacial surgery but still found the topic relevant enough to review and publish. shows that in order to reiterate the state of VSP in craniomaxillofacial surgery, journal coverage is not yet mature enough for deep characterization. This can change as more journals accept such publications in this area as the technology becomes more accessible to populations across the globe. Readers can then expect more comprehensive coverage. In the meantime, coverage is expected to be focused mostly in areas with established expertise of the method.
Literature synthesis results
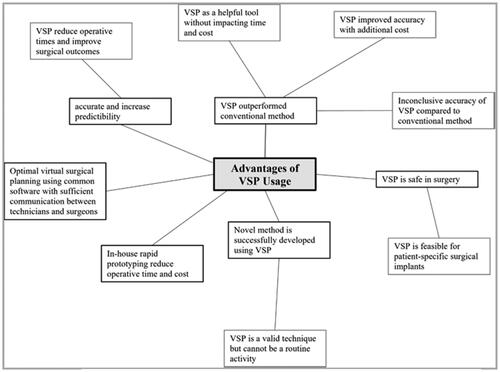
The aim of the literature synthesis is to provide justification and rationale for embarking on this review while also enabling a better understanding of the published literature. The retrieved data were coded to identify important characteristics and results of the studies. Following the coding process was the analysis and integration of results. demonstrates that most of the literature that has been published on VSP has either evaluated the accuracy and feasibility of this technique or has explored the potential benefits of VSP over the more traditional method of craniomaxillofacial surgery. Furthermore, most of the sample studies found that VSP is a useful tool in surgical procedures, from planning, implant and plate fabrication, and to guiding the actual operation, with the benefits of reduced operative times, improved surgical outcomes and potentially reducing costs. However, some studies found an improvement in accuracy but with added costs. Studies that described new methods on surgery utilizing VSP found an inconclusive accuracy compared to traditional methods and only can be utilized in specific cases [Citation37,Citation45].
summarizes that the qualified papers were divided into groups assigned to the four subdisciplines related to craniomaxillofacial surgery: orthognathic surgery, reconstructive surgery, trauma surgery and implant surgery, of which VSP is widely utilized [Citation32]. The number of papers were listed in each category with a total of 42 which exceeds the number of samples, as one paper can research the usage of VSP across the subdisciplines of craniomaxillofacial surgery.
Figure 8. Literature synthesis results [Citation25].
![Figure 8. Literature synthesis results [Citation25].](/cms/asset/92d8ad94-31d5-4ff1-8a04-f4aa485156d8/icsu_a_2271160_f0008_c.jpg)
Orthognathic surgery
Orthognathic surgery is a procedure commonly performed to correct craniofacial and dentofacial deformities and malocclusion. One of the most common congenital deformities treated with orthognathic surgery is cleft lip palate (CLP) [Citation45,Citation47]. As shown in , there were 15 studies that utilized VSP in orthognathic surgery and seven among these found a time reduction in their operation and/or treatment time [Citation4,Citation8,Citation9,Citation34,Citation35,Citation45,Citation48]. Meanwhile, one study experienced an increase in their procedure time due to the complex and time-consuming procedures needed to perform on their case subjects [Citation23]. Twelve studies mentioned a good/better accuracy of their VSP technique and eight found an improvement on their clinical outcomes [Citation4,Citation8,Citation9, Citation16,Citation34,Citation38,Citation45,Citation48–54]. Cost is usually not the focus of these studies. However, five papers mentioned cost-effectiveness but did not specify if it is an increase or decrease in their cost. [Citation4,Citation8,Citation9,Citation34,Citation45].
Table 2. Results on the factors of VSP usage in orthognathic surgery.
Reconstructive surgery
The findings revealed that the majority of the papers in the sample were exploring the utility of VSP in reconstructive surgical procedures. shows that 10 studies cited the advantages of VSP over traditional methods in terms of operating room time and clinical outcomes [Citation8,Citation10,Citation11,Citation37,Citation40, Citation41,Citation55–58]. Better accuracy was also obtained in 12 studies [Citation8,Citation10,Citation11,Citation14,Citation38,Citation40,Citation49,Citation54–57,Citation59]. Regardless, there is one study that revealed a negative clinical impact and an increase in treatment time in using VSP compared to the conventional method [Citation58]. In terms of cost, five studies claimed that using technology was less expensive and more cost-effective [Citation8, Citation10,Citation11,Citation40,Citation41,Citation57]. However, three studies found that it was equally expensive depending on the complexity of their cases or that they needed to work with outsourcing companies for virtual planning [Citation14,Citation55,Citation57].
Table 3. Results on the factors of VSP usage in reconstruction surgery.
Trauma surgery
Trauma surgery is done on patients that obtained fractures or injuries caused by impact from high-energy mechanisms such as vehicle collisions and gunshots. Treating these fractures is a challenge for surgeons due to the delicate structure of the face and skull; VSP was seen with the potential to guide surgeons on these procedures [Citation36]. Trauma and reconstruction surgery is sometimes done simultaneously for maxillomandibular fixation. revealed a positive impact on the use of VSP to aid trauma surgeries with three studies that mentioned a reduction in operation time and improved accuracy [Citation8,Citation10,Citation57]. Two studies described the improvement in clinical outcomes and lower overall cost of the procedure, indicating its cost-effectiveness [Citation10,Citation57].
Table 4. Results on the factors of VSP usage in trauma surgery.
Implant surgery
Implant surgery is a procedure that replaces damaged bones or teeth with artificial ones. Custom implants are used in craniomaxillofacial surgery to fix any bone damage in this area. Most implants are made of titanium or polyether ether ketone (PEEK) [Citation8,Citation23,Citation25,Citation56,Citation58]. The results on revealed that seven out of eight studies that utilized VSP in implant surgery achieved a time reduction on their operation and overall treatment [Citation8,Citation11,Citation37,Citation40,Citation56,Citation58,Citation61], and of which five of these studies obtained better accuracy of the implants. [Citation8,Citation11,Citation40,Citation56,Citation61]. Three studies revealed positive clinical outcomes and a reduction in cost. [Citation8,Citation11,Citation37,Citation40,Citation56,Citation61].
Table 5. Results on the factors of VSP usage in implant surgery.
Discussion
This section discusses the gaps in the sample literature on virtual surgical planning in craniomaxillofacial surgery. In the earlier section, one of the common factors in the utilization of VSP in surgery is cost, but more than half of the sample did not mention in their papers the cost of VSP usage as shown in . This would be exceptionally important to know going forward, especially to look at the ongoing cost of VSP. It could perhaps enable more equitable access to surgery as the most successful surgeons, at the end of their careers with less mechanical skill, could plan the surgeries so that younger, learning surgeons could do the physical work of the operation. However, this is predicated on the existence of appropriate internet infrastructure and a healthcare system that citizens could access. As a perceived innovative technological tool in the area of surgery, the cost of VSP should also be taken into account to prove its practicality in this field. On profiling, VSP is only utilized in countries where technology is advanced such as China, the USA, Italy and Germany, currently indicating that less advanced countries cannot afford such technology. This review also found limitations in the sample population of the literature, as fewer number of case subjects are susceptible to bias. Usually, these studies introduced a new VSP technique on certain surgical procedures [Citation11,Citation14,Citation16,Citation54,Citation57,Citation61]. This may very well be an ongoing issue in the field. If a patient is closely similar to a baseline patient that has been operated on before, the surgeon may not feel compelled to use VSP techniques in order to better utilize time constraints. This would also be true in some cases of trauma surgery. It is entirely possible that unless VSP becomes a matter of course in a hospital system, that all studies will only ever have a limited subset of subjects. This in turn limits the utility of the research completed. There is also a limitation in the time frame of the studies which can be attributed to the number of case subjects and study type. Retrospective studies select and study sample subjects based on their prior information. This type of study most likely will have more case subjects but in a longer time frame. While in prospective studies, sample individuals are studied over time to observe any changes in their characteristics, cases occurring at the same time are at a bare minimum in surgery though the time frame is shorter.
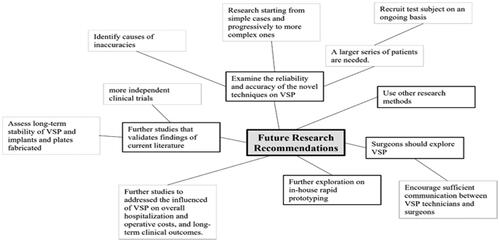
To address the limitations found in the current literature, common recommendations from the sample were identified and highlighted to serve as a guide for future studies. As shown in , these include further studies to validate the findings of the previous research on VSP utilization in craniomaxillofacial surgery [Citation45,Citation48,Citation55,Citation58]. For novel methods in surgical procedures using VSP, further research is recommended on the new method starting from simple cases to complex ones with a larger number of case subjects that are an ongoing basis to obtain conclusive results, as well as identify and address the inaccuracies experienced by the previous researchers [Citation4,Citation10,Citation11,Citation14,Citation16,Citation35,Citation41,Citation48]. Furthermore, in-house rapid prototyping was seen as a potential to save cost on operations, thus further exploration is highly suggested as well as surgeons’ exploration of VSP. [Citation10,Citation23,Citation41,Citation51,Citation52,Citation57,Citation58]. The above-mentioned recommendations to guide future studies may very well become adaptable as ways to measure the outcomes of all VSP procedures in the future, and thus become the foundation by which to analyze the effectiveness of newer surgical procedures.
In the field of craniomaxillofacial surgery the mainstay goal of the treatment is to restore the function and form of the facial structure. Due to the complexity of the facial configuration, it makes the reconstruction process challenging and time consuming. However, the advent of VSP, it helps produce better surgical outcomes, lessen operative time and shorten the hospital stay of patient with complex CMF cases. VSP serves as a stimulator wherein the clinician can outline the existing and potential problems, visualize the size of the bony defect, and predict the accuracy of the bony reduction and test the fit of the implant.
The application of VSP varies per subdisciplines of CMF surgery. In CMF trauma surgery, VSP is used to produce models that will be use as a template for pre-bending the implants. While in Orthognathic surgery, it plays a pivotal role in stimulating the surgery and producing splints to achieve the ideal facial projections and occlusion. And in reconstructive surgery, surgical cutting guides to attain the optimal bony contacts in filling the gaps and restoring the contour of the face. At present, VSP is used to fabricate patient specific implants in the craniomaxillofacial region to address the complexity of the facial structure and precision in bridging two bony segments to promote optimum bone growth. Several studies have been published in 3d printed biomaterials both in vitro and vivo. This technology has a great potential to flourish, it will eliminate donor morbidity and provide an alternative option in the scenario where bone graft is not available.
In clinical practice, the three main drawbacks of VSP are the cost, technical skill set and technology specifically the needed software and equipment. Currently, there are several free access software and low-cost in-house printing equipment available in the market which makes VSP more accessible. However, in some complex cases and fabrication of patient specific implants for reconstruction third-party outsourcing will be needed which will entails longer planning time and an increase in production cost. In terms of the cost, it is variable depending on the degree of difficulty of the planning process, and the types of implants to be used.
The literature also noted that there are two related perspectives on time consumption of VSP in craniomaxillofacial surgery. The first is the preoperative time which is expected to increase since planning time and preparation time increases as surgeons use VSP in the conduct of surgical planning. The second is the intraoperative time which shows that patient spends less time in the operating room [Citation4,Citation8–11,Citation14,Citation23,Citation34,Citation35,Citation37,Citation40,Citation41,Citation45,Citation48,Citation55–58,Citation61]. The literature that was analyzed in this study did not focused on the preoperative time that the surgeons spent in the planning but instead focused on the intraoperative time. In a patient-centered analysis, VSP usage which results in additional time that surgeons spend in planning can be justified by the decrease in the intraoperative time that the patient spends in the operating room. As brought about by the surgeon’s utilization of VSP, clinical outcomes t for the patients to avoid prolonged surgery could result in lesser blood loss, lesser consumption of anesthesia, lesser amount of errors, lesser risks of complications, and even the actual post-operative outcome which could either be esthetic as well as functional [Citation4,Citation9,Citation10,Citation14,Citation16,Citation34,Citation37,Citation38,Citation41,Citation45,Citation49,Citation52,Citation53,Citation55–57,Citation59,Citation61]. Overall, the preoperative VSP cost can be offset by the intra-operative cost due to shorter operative time that will imply lesser consumption of anesthesia, usage of oxygen and other expenses. Another limitation is the technical skill set, clinicians will need to undergo additional trainings and several practice sessions to enhance their skill in VSP because mastery of this technology will ensure accurate post-operative outcomes.
Conclusion and recommendations
The usage of virtual surgical planning (VSP) in craniomaxillofacial surgery is expanding and it is commonly used in orthognathic, reconstructive, trauma, and implant surgery. VSP enables surgeons to visualize complex defects and more accurately predict the unique reconstruction and treatment requirements of each patient. This paper synthesized 29 journal articles to produce significant contributions to the body of knowledge in surgery, specifically the usage of VSP in craniomaxillofacial surgery. The researchers defined the factors that influenced the usage of VSP stated in the sample articles. These include the impact on operative and treatment time, accuracy, surgical outcomes and cost. Results revealed that VSP offers advantages in craniomaxillofacial surgery over the traditional method in terms of duration, predictability and clinical outcomes. However, there is very little literature that addresses the cost factor and if there is any additional cost of VSP, it may be offset by increased precision and shorter operative times, which may reduce hospitalization length of stay and overall cost.
In addition to providing an overview of current findings and trends, this review will also give recommendations for future research to address the literature gaps identified. The researchers encourage future investigation on the cost impact of VSP to further conclude that it will indeed be a practical technique in surgery. Additionally, future researchers are recommended to conduct quantifiable studies on the extent of additional increase in time that surgeons consume in utilizing VSP during the planning phase while comparing it to the decrease of time that the patient spends in the operating room as a result of VSP utilization. With this, future studies should investigate whether the integration of preoperative VSP leads to an increase or decrease in overall surgical time, comprising both preoperative planning and intraoperative surgical time. Additionally, research should aim to determine the extent of this time difference and assess whether the associated duration can be justified by improved clinical outcomes. Furthermore, future researchers on VSP are recommended to gather enough case subjects and use prospective types of study, as it is subject to less bias and ensures that the cases and tools are timely. Technology advances so quickly that studies on the usage of innovative techniques such as VSP should be conducted in a short time frame, as the new technology may no longer remain new in papers published thereafter.
Acknowledgement
The authors would like to thank the support of the Mindanao State University-Iligan Institute of Technology (MSU-IIT), the Office of the Vice Chancellor for Research and Enterprise, and the Office of the Vice Chancellor for Public Affairs for their assistance in this study. This work is supported by MSU-IIT as internally funded research for the MSU-IIT College of Computer Studies and as an extension project of the WE CARE Office for the Information Systems program of the Department of Information Technology. The authors would also like to thank the assistance of ILIGANiCE (Innovation through Leveraging Industry, Government, Academe Networks and inclusive Community Engagements).
Disclosure statement
No potential conflict of interest was reported by the author(s)
Additional information
Funding
References
- Barr ML, Haveles CS, Rezzadeh KS, et al. Virtual surgical planning for mandibular reconstruction with the fibula free flap: a systematic review and meta-analysis. Ann Plast Surg. 2020;84(1):117–122. doi: 10.1097/SAP.0000000000002006.
- Kwon T-G, Lee S-T, Choi S-Y, et al. Considerations for virtual surgical planning and simulation in orthognathic surgery—a narrative review. Front Oral Maxillofac Med. 2020;2:27–27. doi: 10.21037/fomm-20-54.
- Bhandari K, Lin C-H, Liao H-T. Secondary mandible reconstruction with computer-assisted-surgical simulation and patient-specific pre-bent plates: the algorithm of virtual planning and limitations revisited. Appl. Sci. 2022;12(9):4672. doi: 10.3390/app12094672.
- Efanov JI, Roy A-A, Huang KN, et al. Virtual surgical planning: the pearls and pitfalls. Plast Reconstr Surg Glob Open. 2018;6(1):e1443. doi: 10.1097/GOX.0000000000001443.
- Chung RD, Hunter-Smith DJ, Spychal RT, et al. A systematic review of intraoperative process mapping in surgery. Gland Surg. 2017;6(6):715–725. doi: 10.21037/gs.2017.11.02.
- Adolphs N, Haberl E-J, Liu W, et al. Virtual planning for craniomaxillofacial surgery – 7 years of experience. J Craniomaxillofac Surg. 2014;42(5):e289–e295. doi: 10.1016/j.jcms.2013.10.008.
- Ghai S, Sharma Y, Jain N, et al. Use of 3-D printing technologies in craniomaxillofacial surgery: a review. Oral Maxillofac Surg. 2018;22(3):249–259. doi: 10.1007/s10006-018-0704-z.
- Kalmar CL, Xu W, Zimmerman CE, et al. Trends in utilization of virtual surgical planning in pediatric craniofacial surgery. J Craniofac Surg. 2020;31(7):1900–1905. doi: 10.1097/SCS.0000000000006626.
- Schneider D, Kämmerer PW, Hennig M, et al. Customized virtual surgical planning in bimaxillary orthognathic surgery: a prospective randomized trial. Clin Oral Investig. 2019;23(7):3115–3122. doi: 10.1007/s00784-018-2732-3.
- Maglitto F, Dell’Aversana Orabona G, Committeri U, et al. Virtual surgical planning and the ‘in-house’ rapid prototyping technique in maxillofacial surgery: the current situation and future perspectives. Appl. Sci. 2021;11(3):1009. doi: 10.3390/app11031009.
- Smithers FAE, Cheng K, Jayaram R, et al. Maxillofacial reconstruction using in-house virtual surgical planning: centre-specific virtual surgical planning. ANZ J Surg. 2018;88(9):907–912. doi: 10.1111/ans.14353.
- Sukegawa S, Kanno T. Computer-assisted navigation surgery in oral and maxillofacial surgery. In: K. Bonanthaya, E. Panneerselvam, S. Manuel, V. V. Kumar, and A. Rai, editors. Oral and maxillofacial surgery for the clinician. Singapore: Springer Nature Singapore; 2021, pp. 841–862. doi: 10.1007/978-981-15-1346-6_41.
- Hua J, Aziz S, Shum JW. Virtual surgical planning in oral and maxillofacial surgery. Oral Maxillofac Surg Clin North Am. 2019;31(4):519–530. doi: 10.1016/j.coms.2019.07.011.
- Soleman J, Thieringer F, Beinemann J, et al. Computer-assisted virtual planning and surgical template fabrication for frontoorbital advancement. Neurosurg Focus. 2015;38(5):E5. doi: 10.3171/2015.3.FOCUS14852.
- Alkaabi S, Maningky M, Helder MN, et al. Virtual and traditional surgical planning in orthognathic surgery – systematic review and meta-analysis. Br. J. Oral Maxillofac. Surg. 2022;60(9):1184–1191. p. S026643562200225X, doi: 10.1016/j.bjoms.2022.07.007.
- Barrera JE. Virtual surgical planning improves surgical outcome measures in obstructive sleep apnea surgery: VSP improves surgical outcomes in OSA surgery. Laryngoscope. 2014;124(5):1259–1266. doi: 10.1002/lary.24501.
- Levine JP, Patel A, Saadeh PB, et al. Computer-aided design and manufacturing in craniomaxillofacial surgery: the new state of the art. J Craniofac Surg. 2012;23(1):288–293. doi: 10.1097/SCS.0b013e318241ba92.
- Jacobs CA, Lin AY. A new classification of three-dimensional printing technologies: systematic review of three-dimensional printing for patient-specific craniomaxillofacial surgery. Plast Reconstr Surg. 2017;139(5):1211–1220. doi: 10.1097/PRS.0000000000003232.
- Herford AS, Miller M, Lauritano F, et al. The use of virtual surgical planning and navigation in the treatment of orbital trauma. Chin J Traumatol. 2017;20(1):9–13. doi: 10.1016/j.cjtee.2016.11.002.
- Andrew TW, Baylan J, Mittermiller PA, et al. Virtual surgical planning decreases operative time for isolated single suture and multi-suture craniosynostosis repair. Plast Reconstr Surg Glob Open. 2018;6(12):e2038. doi: 10.1097/GOX.0000000000002038.
- Huang Y-H, Seelaus R, Zhao L, et al. Virtual surgical planning and 3D printing in prosthetic orbital reconstruction with percutaneous implants: a technical case report. Int Med Case Rep J. 2016;9:341–345. doi: 10.2147/IMCRJ.S118139.
- Pijpker PAJ, Wagemakers M, Kraeima J, et al. Three-dimensional printed polymethylmethacrylate casting molds for posterior fossa reconstruction in the surgical treatment of Chiari I malformation: technical note and illustrative cases. World Neurosurg. 2019;129:148–156. doi: 10.1016/j.wneu.2019.05.191.
- Rios O, Lerhe B, Chamorey E, et al. Accuracy of segmented Le fort I osteotomy with virtual planning in orthognathic surgery using patient-specific implants: a case series. J Clin Med. 2022;11(19):5495. doi: 10.3390/jcm11195495.
- Ma J, Ma L, Wang Z, et al. The use of 3D-printed titanium mesh tray in treating complex comminuted mandibular fractures: a case report. Medicine . 2017;96(27):e7250. doi: 10.1097/MD.0000000000007250.
- Tack P, Victor J, Gemmel P, et al. 3D-printing techniques in a medical setting: a systematic literature review. Biomed Eng Online. 2016;15(1):115. doi: 10.1186/s12938-016-0236-4.
- Willinger K, Guevara-Rojas G, Cede J, et al. Comparison of feasibility, time consumption and costs of three virtual planning systems for surgical correction of midfacial deficiency. Maxillofac Plast Reconstr Surg. 2021;43(1):2. doi: 10.1186/s40902-020-00284-1.
- May MM, Howe BM, O'Byrne TJ, et al. Short and long‐term outcomes of three‐dimensional printed surgical guides and virtual surgical planning versus conventional methods for fibula free flap reconstruction of the mandible: decreased nonunion and complication rates. Head Neck. 2021;43(8):2342–2352. doi: 10.1002/hed.26688.
- Snyder H. Literature review as a research methodology: an overview and guidelines. J. Bus. Res. 2019;104:333–339. doi: 10.1016/j.jbusres.2019.07.039.
- Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. J Clin Epidemiol. 2021;134:178–189. doi: 10.1016/j.jclinepi.2021.03.001.
- Alkhayer A, Piffkó J, Lippold C, et al. Accuracy of virtual planning in orthognathic surgery: a systematic review. Head Face Med. 2020;16(1):34. doi: 10.1186/s13005-020-00250-2.
- Fu S, Chen D, He H, et al. Clinical concept extraction: a methodology review. J Biomed Inform. 2020;109:103526. doi: 10.1016/j.jbi.2020.103526.
- Lisiak-Myszke M, Marciniak D, Bieliński M, et al. Application of finite element analysis in oral and maxillofacial surgery—a literature review. Materials. 2020;13(14):3063. doi: 10.3390/ma13143063.
- Swennen GRJ, Mollemans W, Schutyser F. Three-dimensional treatment planning of orthognathic surgery in the era of virtual imaging. J Oral Maxillofac Surg. 2009;67(10):2080–2092. doi: 10.1016/j.joms.2009.06.007.
- Scolozzi P. Computer-aided design and computer-aided modeling (CAD/CAM) generated surgical splints, cutting guides and custom-made implants: which indications in orthognathic surgery? Rev Stomatol Chir Maxillofac Chir Orale. 2015;116(6):343–349. doi: 10.1016/j.revsto.2015.09.005.
- Sun Y, Luebbers H-T, Agbaje JO, et al. Accuracy of upper jaw positioning with intermediate splint fabrication after virtual planning in bimaxillary orthognathic surgery. J Craniofac Surg. 2013;24(6):1871–1876. doi: 10.1097/SCS.0b013e31829a80d9.
- Cousley RR, Turner MJ. Digital model planning and computerized fabrication of orthognathic surgery wafers. J Orthod. 2014;41(1):38–45. doi: 10.1179/1465313313Y.0000000075.
- Sozzi D, Filippi A, Canzi G, et al. Surgical navigation in mandibular reconstruction: accuracy evaluation of an innovative protocol. J Clin Med. 2022;11(7):2060. doi: 10.3390/jcm11072060.
- Swendseid BP, Roden DF, Vimawala S, et al. Virtual surgical planning in subscapular system free flap reconstruction of midface defects. Oral Oncol. 2020;101:104508. doi: 10.1016/j.oraloncology.2019.104508.
- Matias M, Zenha H, Costa H. Three-dimensional printing: custom-made implants for craniomaxillofacial reconstructive surgery. Craniomaxillofac Trauma Reconstr. 2017;10(2):89–98. doi: 10.1055/s-0036-1594277.
- Mazzola F, Smithers F, Cheng K, et al. Time and cost-analysis of virtual surgical planning for head and neck reconstruction: a matched pair analysis. Oral Oncol. 2020;100:104491. doi: 10.1016/j.oraloncology.2019.104491.
- Yang W-F, Choi WS, Leung YY, et al. Three-dimensional printing of patient-specific surgical plates in head and neck reconstruction: a prospective pilot study. Oral Oncol. 2018;78:31–36. doi: 10.1016/j.oraloncology.2018.01.005.
- Flügge T, Kramer J, Nelson K, et al. Digital implantology—a review of virtual planning software for guided implant surgery. Part II: prosthetic set-up and virtual implant planning. BMC Oral Health. 2022;22(1):23. doi: 10.1186/s12903-022-02057-w.
- Jardini AL, Larosa MA, de Carvalho Zavaglia CA, et al. Customised titanium implant fabricated in additive manufacturing for craniomaxillofacial surgery: this paper discusses the design and fabrication of a metallic implant for the reconstruction of a large cranial defect. Virtual Phys. Prototyp. 2014;9(2):115–125. doi: 10.1080/17452759.2014.900857.
- Kongsong W, Sittitavornwong S. Utilization of virtual surgical planning for surgical splint-assisted comminuted maxillomandibular fracture reduction and/or fixation. Craniomaxillofac Trauma Reconstr. 2020;13(4):334–341. doi: 10.1177/1943387520948677.
- Wang Y, Li J, Xu Y, et al. Accuracy of virtual surgical planning-assisted management for maxillary hypoplasia in adult patients with cleft lip and palate. J Plast Reconstr Aesthet Surg. 2020;73(1):134–140. doi: 10.1016/j.bjps.2019.07.003.
- Zheng J, Fang B, Zhang S, et al. Oral and maxillofacial surgery in China: past, present and future. OJST. 2013;03(07):354–358. doi: 10.4236/ojst.2013.37060.
- Quereshy FA, Levintov N, Nguyen JL, et al. The role of virtual surgical planning in increasing the predictability in orthognathic surgery. JDMS. 2019;2(1):136–141. doi: 10.18314/jdms.v2i1.1633.
- Antonini F, Borba AM, Pagnoncelli RM, et al. Does a learning curve exist for accuracy in three-dimensional planning for maxillary positioning in bimaxillary orthognathic surgery? Int J Oral Maxillofac Surg. 2020;49(6):787–793. doi: 10.1016/j.ijom.2019.10.005.
- Liao Y-F, Chen Y-A, Chen Y-C, et al. Outcomes of conventional versus virtual surgical planning of orthognathic surgery using surgery-first approach for class III asymmetry. Clin Oral Investig. 2020;24(4):1509–1516. doi: 10.1007/s00784-020-03241-4.
- Ritto FG, Schmitt ARM, Pimentel T, et al. Comparison of the accuracy of maxillary position between conventional model surgery and virtual surgical planning. Int J Oral Maxillofac Surg. 2018;47(2):160–166. doi: 10.1016/j.ijom.2017.08.012.
- De Riu G, Virdis PI, Meloni SM, et al. Accuracy of computer-assisted orthognathic surgery. J Craniomaxillofac Surg. 2018;46(2):293–298. doi: 10.1016/j.jcms.2017.11.023.
- Li Y, Jiang Y, Zhang N, et al. Clinical feasibility and efficacy of using virtual surgical planning in bimaxillary orthognathic surgery without intermediate splint. J Craniofac Surg. 2015;26(2):501–505. doi: 10.1097/SCS.0000000000001530.
- Ying X, Tian K, Zhang K, et al. Accuracy of virtual surgical planning in segmental osteotomy in combination with bimaxillary orthognathic surgery with surgery first approach. BMC Oral Health. 2021;21(1):529. doi: 10.1186/s12903-021-01892-7.
- Ye N, Long H, Zhu S, et al. The accuracy of computer image-guided template for mandibular angle ostectomy. Aesthetic Plast Surg. 2015;39(1):117–123. doi: 10.1007/s00266-014-0424-1.
- Liu Y, Xu L, Zhu H, et al. Technical procedures for template-guided surgery for mandibular reconstruction based on digital design and manufacturing. Biomed Eng Online. 2014;13(1):63. doi: 10.1186/1475-925X-13-63.
- Qu X, Wang M, Xu L, et al. Occlusion guided double-barreled fibular osteoseptocutaneous free flap for refined mandibular reconstruction aided by virtual surgical planning. J Craniofac Surg. 2017;28(6):1472–1476. Sep doi: 10.1097/SCS.0000000000003841.
- Mendez BM, Chiodo MV, Patel PA. Customized ‘in-Office’ three-dimensional printing for virtual surgical planning in craniofacial surgery. J Craniofac Surg. 2015;26(5):1584–1586. doi: 10.1097/SCS.0000000000001768.
- Knitschke M, Bäcker C, Schmermund D, et al. “Impact of planning method (conventional versus virtual) on time to therapy initiation and resection margins: a retrospective analysis of 104 immediate jaw reconstructions. Cancers. 2021;13(12):3013. doi: 10.3390/cancers13123013.
- Sembronio S, Tel A, Costa F, et al. Accuracy of custom-fitted temporomandibular joint alloplastic reconstruction and virtual surgical planning. Int J Oral Maxillofac Surg. 2019;48(8):1077–1083. Aug doi: 10.1016/j.ijom.2019.01.024.
- Gh. Moghaddam M, Garcia GJM, Frank-Ito DO, et al. Virtual septoplasty: a method to predict surgical outcomes for patients with nasal airway obstruction. Int J Comput Assist Radiol Surg. 2020;15(4):725–735. doi: 10.1007/s11548-020-02124-z.
- Haq J, Patel N, Weimer K, et al. Single stage treatment of ankylosis of the temporomandibular joint using patient-specific total joint replacement and virtual surgical planning. Br J Oral Maxillofac Surg. 2014;52(4):350–355. doi: 10.1016/j.bjoms.2014.01.004.

![Figure 1. Flowchart of the study selection process according to the PRISMA 2020 statement [29].](/cms/asset/10a52f53-374d-4508-a5e1-1db0025cc08a/icsu_a_2271160_f0001_b.jpg)