ABSTRACT
Purpose
To audit hormonal contraceptive use and associated symptomology in elite women’s soccer in England.
Methods
Seventy-five elite women’s soccer players from the Women’s Super League (WSL) completed a questionnaire to assess: hormonal contraceptive (HC) use or non-use, reasons for initiation and discontinuation and the symptoms experienced by HC and non-HC users.
Results
Twenty-eight per cent reported current HC use, with 43% having used HCs previously. Combined HCs accounted for 62% of total usage, with progestin-only HCs making up the remainder. Eighty-six per cent pre-empted negative symptoms before commencing HCs, with 38% experiencing adverse symptoms. Negative symptoms were most common in progestin-only HC users (63%). Eighty-six per cent reported benefits associated with HC usage include pain management and the ability to predict or control their cycles. Six non-HC users reported amenorrhea, with one medically diagnosed. Negative MC-related symptoms were reported by 74%, with 4% unable to train due to these symptoms. Unfavorable symptoms typically occurred during the first days of menstruation (59%).
Conclusion
Most WSL players do not currently use HCs (72%). Most HC users reported benefits of HC usage, whilst most non-HC users reported negative symptoms especially around menstruation. Practitioners should track players' MCs to help minimise discomfort and maximise performance.
Introduction
In 2015, the Women’s Super League (WSL) became the first professional women’s soccer league in England. Since then, women’s soccer has grown in popularity and participation. The increased number of players and competitions is driving the need for researchers and practitioners to understand the potential impact of ovarian steroid hormones on training and performance. To capitalise on previous research in this field (Julian et al. Citation2017) and to underpin future research, we need to define the menstrual characteristics (i.e., hormonal contraceptive [HC] use and non-use) of elite women’s soccer players.
A greater number of athletes use HCs (49.5%) compared to the general population (30%) (Cea-Soriano et al. Citation2014; Martin et al. Citation2018). HCs are exogenous steroid hormones that inhibit ovulation and result in consistently low levels of endogenous oestrogen and progesterone (Elliott-Sale and Hicks Citation2018). Data from Schaumberg et al. (Citation2018) showed that athletes use HC for perceived performance benefits; however, data from a recent review indicated that HCs may impair performance in some sportswomen (Elliott-Sale et al. Citation2020). It is crucial to establish how many WSL players use a HC, their reason for usage and any side effects experienced, in order to ascertain their potential implications for players (i.e., this approach will help to minimise any potential negative effects on performance and maximise any potential positive effects on adverse menstrual cycle symptoms (Oxfeldt et al. Citation2020), thus ensuring that players can perform to the best of their ability on any given day, regardless of ovarian hormone profile).
In the absence of menstrual irregularities, non-HC users typically have an idealized 28-day MC, although cycles can vary between 21 and 35 days (Lamina et al. Citation2013). Abnormalities of the MC occur in 6–79% of sportswomen, with the prevalence of menstrual dysfunction varying with athletic discipline and level of competition (Warren and Perlroth Citation2001). Whilst menstrual function data have been collected in many types of sportswomen (Cobb et al. Citation2003; Fahrenholtz et al. Citation2018; Hoch et al. Citation2009, Citation2011; Melin et al. Citation2015; Torstveit and The Female Citation2005), there are limited data in women’s soccer (Prather et al. Citation2016; Reed et al. Citation2013; Sundgot-Borgen and Torstveit Citation2007) and currently no data on players in England since soccer turned professional. It is important to determine the menstrual characteristics of non-HC users in order to understand their potential consequences for players.
The aim of this study was to audit HC and non-HC use, determine the reasons for initiation and discontinuation of HCs, and report the symptoms experienced by HC users and non-users, in WSL players. These data will build upon previous information gathered in 2015–2016 by Martin et al. (Citation2018) in a diverse range of sportswomen, by providing soccer-specific information relevant to the professional game. These findings can be used by practitioners to benchmark their own players and implement strategies to support players with their reproductive health and associated conditions.
Methods
Participants
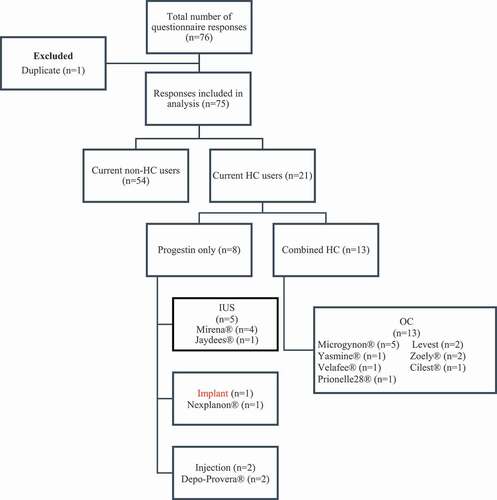
Between 2017 and 2018, players were recruited from the WSL. All 10 WSL clubs were contacted, and six clubs participated. Players were contacted through support staff, who took written informed consent and administered the questionnaires. All players were recruited using the same procedures; that is, no player or type of player was specifically targeted for recruitment. Each player returned their own questionnaire in individual, sealed envelopes. Athletes had to be >18 years old, contracted to a WSL club and have played at least one game in the WSL. Seventy-six players out of 194 in the WSL completed the questionnaire (). All players were nulliparous. The study was approved by the non-invasive ethics committee at Nottingham Trent University. Written informed consent was obtained from each player with the acknowledgement that their data would be used for publishing and fully anomymised.
Questionnaire
Data were collected using a modified version of a previously designed questionnaire (Martin et al. Citation2018). The questionnaire was designed to identify the self-reported: (Julian et al. Citation2017) period prevalence and characteristics of HC and non-HC users; (Martin et al. Citation2018) reasons for initiation and discontinuation of HCs; and (Cea-Soriano et al. Citation2014) perceived symptoms associated with HC use and non-use. As such, all data reported in this study are ‘self-reported’ and ‘perceived’. Participants were required to record demographic information, age of menarche, competitive level, time competing at this level, and weekly training frequency and duration (). Participants were required to complete different sections of the questionnaire depending on HC use or non-use. The final section of the questionnaire required all participants to provide details on previous HC use, including preparation, duration of use and reason for discontinuation.
Table 1. Characteristics for the football associations Women’s Super League players; hormonal contraceptive and non-hormonal contraceptive users
Data analysis
Data were analysed using Microsoft Excel. To prevent duplicate data, date-of-births and identical values were visually checked. HC and non-HC user characteristics were compared using independent samples t-tests; the level of significance was set at P ≤ 0.05. All data were handled in the same way. For qualitative questions, a content analysis was carried out separately by two researchers (LP and GC) to categorise responses, whereby a frequency analysis was performed to elicit common themes. Differences between the researchers were discussed until a consensus was reached. Data are represented as means (±SD), frequencies and percentages.
Results
Period prevalence and characteristics of hormonal contraceptive users
The period prevalence and descriptive characteristics of HC users are presented in and . The average length of HC usage was 3.1 ± 3.1 years. The main reasons for choosing a particular HC method were: General Practitioner advice (38%), easiest form (20%), and friends’ recommendation (14%). Only 55% of the players discussed their HC use with their coach or team doctor.
Previous hormonal contraceptive use
Of the players that did not currently use HCs, 20% reported previous usage. Of the players with current HC use, 19% had previously used a different HC formulation. The reasons for discontinuing or switching HC formulation are shown in .
Symptomology of hormonal contraceptive users
The frequency and prevalence of symptoms experienced by players using HCs are presented in . show the anticipated positive and negative side effects before players commenced HCs. Negative symptoms were more common in progestin-only HCs (63%) compared with combined HCs (23%).
Table 2. Sample frequency (n = 21) and prevalence of self-reported perceived negative and positive symptoms experienced by hormonal contraceptive users
Period prevalence and characteristics of non-hormonal contraceptive users
The period prevalence and descriptive characteristics of non-HC use are presented in and . None of the non-HC users used a non-hormonal IUD. The mean cycle length was 31 ± 10 days, with 67% reporting that their cycle varied in length (cycle length varied by 3–63 days). Six players reported being amenorrhoeic and eight players reported being oligomenorrheic, although only one case of amenorrhea was diagnosed by a clinician.
Symptomology of non-hormonal contraceptive users
The frequency and prevalence of adverse symptoms for non-HC users are presented in . Adverse MC-related symptoms were reported by 74% of players, with 4% stating that these symptoms had prevented them from training. Reasons for having to miss training included ‘heavy bleed’, ‘back pain,’ and ‘being sick’. These issues mainly occurred during the first 2–3 days of menstruation (59%) and in the days leading up to menstruation (17%). Medication was used by 19% of the players to deal with menstrual-related issues, with 13% using nonsteroidal anti-inflammatory drugs (NSAIDs) and 6% taking paracetamol.
Table 3. Sample frequency (n = 54) and prevalence of negative self-reported perceived symptoms during the menstrual cycle for non-hormonal contraceptive users
Discussion
The aim of the present study was to audit HC and non-HC use in the WSL and to describe the associated symptomology. This study provides novel data on the reproductive characteristics of elite women’s soccer players. Less than a third of players currently use a form of HCs. From the players using HCs, 86% reported benefits and 38% reporting negative symptoms. From the non-HC using players, 74% reported negative symptoms and none reported benefits.
In the non-HC users, all players without menstrual irregularities fulfilled the eumenorrheic criterion for cycle length (Lamina et al., Citation2013). Six players reported amenorrhea, although only one player was diagnosed by a clinician. Eight players reported oligomenorrhea, none of which were diagnosed by a clinician. Although our questionnaire did not explore the reasons behind this observation, it highlights that WSL players are not discussing their menstrual characteristics with a health-care professional. This observation is supported by recent data (Findlay et al. Citation2020; Larsen et al. Citation2020), which suggests that: (i) sportswomen have little/no medical support; (ii) sportswomen do not feel confident enough to disclose their menstrual issues with support staff; (iii) support staff often do not have a good understanding of the best practice to deal with MC/HC symptoms; and (iv) sportswomen do not have a full understanding about amenorrhea and their own menstrual function. As such, we recommend that players and support staff receive suitable training/education such that they have a good understanding of menstrual function and dysfunction, from both a health and performance perspective, for example, as a potential indicator of Relative Energy Deficiency in Sport. As menstrual irregularities were self-reported in this questionnaire, future research should involve medical screening/diagnosis to provide data on how prevalent menstrual irregularities are in WSL.
Nine negative symptoms were reported by non-HC users (), with 74% of players reporting at least one symptom. This is similar with the general population (Ju et al. Citation2014) and other elite athletes (Martin et al. Citation2018), although a study in elite female rugby players reported that 93% of players had negative MC-related symptoms (Findlay et al. Citation2020). A limitation of the present study was that it did not specifically ask if these symptoms could have been affected by factors other than the MC (e.g., a medical condition, such as endometriosis); however, data collected on current medication usage did not infer any of the players having a medical condition that would have significantly influenced the reported symptoms. Symptoms were mainly experienced in the initial days of menstruation (59%), but also occurred in days leading up to menstruation (17%). In the present study, only two players reported that they missed training as a result of their MC symptoms, thus supporting previous research in elite athletes (Martin et al. Citation2018). Despite non-HC users reporting symptoms interfering with their training, there was no statistical difference between groups in the number of training sessions per week, average training session duration or total weekly training duration (). A limitation of the present study was that we did not establish the severity of the symptoms experienced, the frequency of missed training sessions, or if players trained despite feeling unable to do so. Findlay et al. (Citation2020) reported that some women’s rugby players, no matter the severity, did not feel that their menstrual related symptoms were an acceptable reason to take rest or abstain from training. With 74% of players in the current study suffering from symptoms, further research is required to understand the frequency, severity, duration and impact of these on training, and if ‘soccer’ allows players to adapt their training without negative repercussions. Ideally, practitioners need to allow flexibility in training sessions to accommodate the most severe symptoms.
The prevalence of HC use in elite female soccer players (28%) is similar to that of the general British (30%) (Cea-Soriano et al. Citation2014) and American (27.6%) public (Daniels et al., Citation2014) but less than in other elite female sports (47.1% and 49.5%) (Martin et al. Citation2018; Larsen et al. Citation2020). This lower prevalence might be accounted for by the infancy of the professional soccer game. Previous research indicates that athletes often manipulate and control their MC by using HCs (Schaumberg et al. Citation2018), and that elite (43%) versus sub-elite (22.5%) athletes are more likely to do this (Martin et al. Citation2018). In addition, this lower prevalence might be accounted for less severe symptoms in the non-HC group, meaning that they did not feel the need to use a HC in response to their symptoms. It will be interesting to track if more WSL players switch to using HCs to manipulate their MC in the coming years as the sport becomes more professional.
Most players anticipated negative symptoms before taking HCs (76%), with weight gain being the most common (33%) concern. Thirty-eight per cent experienced negative symptoms, with mood swings and still having a ‘period’, the most common issues (both 10%), and only one player reporting weight gain. Negative symptoms were most common in progestin only-HC users compared to combined HC users, which is a similar to previous findings (Martin et al. Citation2018). It is important to note that each pill formulation carriers its own unique concentration of synthetic hormones which needs to be considered when interpreting data. These pre-conceived ideas and lived experienced can be used to guide players to make informed HC choices.
Conclusion
This study is the first to audit HC and non-HC use in the WSL. Less than one-third of WSL players use a form of HC. Although most HC users reported benefits of HC use, it is not the intention of this paper to endorse or denounce HC use as we do not yet fully understand if the symptomatic benefits of HC result in any adverse health or performance-related consequences. Almost three-quarters of players reported negative symptoms during their MC, with 4% of players abstaining from training due to these unfavourable effects. These data can be used to inform support staff about the hormonal profile of women’s soccer players and to consider interventions in line with the demands and features of their sport.
Acknowledgements
The authors would like to thank all practitioners that helped facilitate this research and all players for taking the time to complete the questionnaires.
Disclosure statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Data availability statement
The data that support the findings of this study are available from the corresponding author, GC upon reasonable request https://symplectic.ljmu.ac.uk/.
Additional information
Funding
References
- Cea-Soriano L, García Rodríguez L, Machlitt A, Wallander MA. 2014. Use of prescription contraceptive methods in the UK general population: a primary care study. BJOG: An International Journal of Obstetrics & Gynaecology. 121(1):53–61. doi:https://doi.org/10.1111/1471-0528.12465.
- Cobb KL, Bachrach LK, Greendale G, Marcus R, Neer RM, Nieves J, Sowers MF, Brown BW Jr, Gopalakrishnan G, Luetters C, Tanner HK, Ward B, Kelsey JL. 2003. Disordered eating, menstrual irregularity, and bone mineral density in female runners. Med Sci Sports Exerc. 35(5):711–719. doi:https://doi.org/10.1249/01.MSS.0000064935.68277.E7
- Daniels K, Daugherty J, Jones J. 2014. Current contraceptive status among women aged 15-44: United States, 2011-2013. NCHS Data Brief. (173):1–8.
- Elliott-Sale KJ, Hicks KM. 2018. Hormonal-based contraception and the exercising female. In J Forsyth & C-M Roberts (eds), The Exercising Female: Science and Its Application. Routledge Research in Sport and Exercise Science, Taylor & Francis; p. 30–43.
- Elliott-Sale KJ, McNulty KL, Ansdell P, Goodall S, Hicks KM, Thomas K, Swinton PA, Dolan E. 2020. The effects of oral contraceptives on exercise performance in women: a systematic review and meta-analysis. Sports Medicine. 50(10):1785–1812. doi:https://doi.org/10.1007/s40279-020-01317-5
- Fahrenholtz IL, Sjodin A, Benardot D, Tornberg AB, Skouby S, Faber J, J, Sundgot-Borgen JK, Melin AK 2018. Within-day energy deficiency and reproductive function in female endurance athletes. Scand J Med Sci Sports. 28(3):1139–1146. doi:https://doi.org/10.1111/sms.13030
- Findlay RJ, Macrae EHR, Whyte IY, Easton C, Forrest LJ. 2020. How the menstrual cycle and menstruation affect sporting performance: experiences and perceptions of elite female rugby players. Br J Sports Med. 54(18):1108–1113. bjsports-2019-1. doi:https://doi.org/10.1136/bjsports-2019-101486.
- Hoch AZ, Pajewski NM, Moraski L, Carrera GF, Wilson CR, Hoffmann RG, Schimke JE, Gutterman DD. 2009. Prevalence of the female athlete triad in high school athletes and sedentary students. Clinical Journal of Sport Medicine. 19(5):421–428. doi:https://doi.org/10.1097/JSM.0b013e3181b8c136
- Hoch AZ, Papanek P, Szabo A, Widlansky ME, Schimke JE, Gutterman DD. 2011. Association between the female athlete triad and endothelial dysfunction in dancers. Clinical Journal of Sport Medicine. 21(2):119–125. doi:https://doi.org/10.1097/JSM.0b013e3182042a9a.
- Ju H, Jones M, The Prevalence MG. 2014. Risk factors of dysmenorrhea. Epidemiol Rev. 36(1):104–113. doi:https://doi.org/10.1093/epirev/mxt009.
- Julian R, Hecksteden A, Fullagar HH, Meyer T. 2017. The effects of menstrual cycle phase on physical performance in female soccer players. PLoS One. 12(3):e0173951. doi:https://doi.org/10.1371/journal.pone.0173951.
- Lamina S, Ezema CI, Ezugwu UA, Amaeze AA, Nwankwo MJ, Ngozi AF. 2013. Exercise and menstrual function: a review study. Health. 05(12):2014–2017. doi:https://doi.org/10.4236/health.2013.512272.
- Larsen B, Morris K, Quinn K, Osborne M, Minahan C. 2020. Practice does not make perfect: a brief view of athletes’ knowledge on the menstrual cycle and oral contraceptives. Journal of Science and Medicine in Sport. 23(8):690–694. doi:https://doi.org/10.1016/j.jsams.2020.02.003.
- Martin D, Sale C, Cooper SB, Elliott-Sale KJ, Prevalence P. 2018. Perceived side effects of hormonal contraceptive use and the menstrual cycle in elite athletes. Int J Sports Physiol Perform. 13(7):926–932. doi:https://doi.org/10.1123/ijspp.2017-0330.
- Melin A, Tornberg AB, Skouby S, Moller SS, Sundgot-Borgen J, Faber J, Sidelmann JJ, Aziz M, Sjödin A. 2015. Energy availability and the female athlete triad in elite endurance athletes. Scand J Med Sci Sports. 25(5):610–622. doi:https://doi.org/10.1111/sms.12261
- Oxfeldt M, Dalgaard LB, Jørgensen AA, Hansen M. 2020. Hormonal contraceptive use, menstrual dysfunctions, and self-reported side effects in elite athletes in denmark. Int J Sports Physiol Perform. 15(10): 1377–1384.
- Prather H, Hunt D, McKeon K, Simpson S, Meyer EB, Yemm T, Brophy R. 2016. Are elite female soccer athletes at risk for disordered eating attitudes. Menstrual Dysfunction, and Stress Fractures? PM R. 8(3):208–213.
- Reed JL, De Souza MJ, Williams NI. 2013. Changes in energy availability across the season in division I female soccer players. J Sports Sci. 31(3):314–324. doi:https://doi.org/10.1080/02640414.2012.733019.
- Schaumberg MA, Emmerton LM, Jenkins DG, Burton NW. 2018. Janse de jonge XAK, skinner TL. Use of Oral Contraceptives to Manipulate Menstruation in Young, Physically Active Women International Journal of Sports Physiology and Performance. 13(1):82–87.
- Sundgot-Borgen J, Torstveit MK. 2007. The female football player, disordered eating, menstrual function and bone health. Br J Sports Med. 41(Suppl Supplement 1):i68–72. doi:https://doi.org/10.1136/bjsm.2007.038018.
- Torstveit MK, The Female S-BJ. 2005. Athlete triad exists in both elite athletes and controls. 37(9):1449–1459. doi:https://doi.org/10.1249/01.mss.0000177678.73041.38
- Warren MP, Perlroth NE. 2001. The effects of intense exercise on the female reproductive system. J Endocrinol. 170(1):3–11. doi:https://doi.org/10.1677/joe.0.1700003.