Abstract
Acetaminophen poisoning remains a leading cause of acute liver failure. Some cases may be difficult to diagnose when clinical findings are equivocal, the patient’s history is misleading or incomplete, or the acetaminophen concentration is low or undetectable at arrival to care. We describe a case of a medically complicated young child whose acute liver failure had two of these features. Measurement of acetaminophen-protein adducts confirmed acetaminophen as the primary cause of her liver failure.
Introduction
Acetaminophen (N-acetyl para-amino phenol, paracetamol or APAP) is a leading cause of acute liver failure (ALF). In some cases, the cause of ALF may not be clear from the patient’s history. APAP measurements obtained many hours after the last ingestion of APAP may be negative or inconclusive in establishing a diagnosis, particularly in patients with repeated supratherapeutic ingestions.
In therapeutic doses of acetaminophen, the primary elimination pathways are sulfate conjugation and glucuronide conjugation. In acetaminophen poisoning, a larger fraction of the APAP undergoes oxidation – primarily by CYP 2E1 and CYP 1A2 – to form N-acetyl para-amino benzoquinone imine (NAPQI) [Citation1]. NAPQI rapidly binds to sulfhydryl groups on cysteine. Glutathione (GSH), a tripeptide containing cysteine, binds and detoxifies NAPQI in a reaction that consumes the GSH. When intracellular stores of GSH become depleted, NAPQI covalently binds to cysteine residues in proteins (such as hepatic enzymes) forming APAP-protein adducts [Citation2]. This disrupts the tertiary structures of affected proteins, denatures these proteins, and leads to cell death. In patients with early diagnosis of APAP poisoning, N-acetylcysteine (Acetadote®, Cumberland Pharmaceuticals, Nashville TN) binds and detoxifies NAPQI to avoid acute liver injury.
Emerging technology allows detection of APAP-protein adducts in serum with a longer detection time than for APAP [Citation3–5]. In patients who present with acute liver injury (such as a person reaching care two to three days after acute APAP overdose), the diagnosis may be unclear if the APAP exposure history is missing or inaccurate. Measuring APAP-protein adducts can identify whether APAP is the likely cause of the observed liver injury. We illustrate a case of diagnostic uncertainty about the cause of acute liver failure in a toddler with a complicated medical history.
Case report
A 2 year-old girl came to the ED at Arkansas Children’s Hospital when her condition worsened with two days of lethargy, vomiting, and fever after two weeks of apparent viral infection.
Her history included perinatal anoxic brain injury resulting in cerebral palsy, failure to thrive (8.8 kg or <5th percentile), recurrent ear infections, and a gastrostomy tube for feeding and medications. Her mother reported treating her fever with “one mill” (1 mL) of APAP elixir (160 mg/5 mL) with each dose. Abnormal laboratory values in the ED included WBC 27.18 k/mm3 (78% neutrophils), sodium 150 mmol/L, CO2 16 mmol/L, BUN 46 mg/dL, glucose 30 mg/dL (1.7 mmol/L). Her urinalysis and analysis of cerebral spinal fluid were non-diagnostic. The ED did not order liver enzymes or coagulation studies.
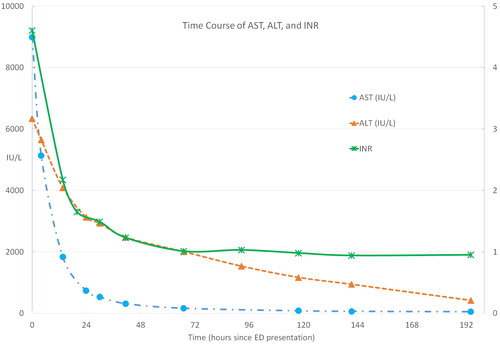
Upon admission, further laboratory testing revealed that AST and ALT were 8989 IU/L and 6338 IU/L, respectively, with an INR of 4 (). Her APAP concentration was 55 mcg/mL. Repeat AST and ALT were 5136 IU/L and 5646 IU/L.
She underwent immediate transfer to a regional pediatric liver transplant center at St. Louis Children’s Hospital, where the ICU team consulted both gastroenterology and toxicology. She received IV N-acetylcysteine (NAC) after transfer in a 30 mg/mL solution with 150 mg/kg/h x 1 h followed by 12.5 mg/kg/h. Her AST and ALT after transfer were 1831 IU/L and 4087 IU/L with INR 2.17 (). APAP concentration was < 5 mcg/mL, and her total bilirubin was 0.5 mg/dL. Her plasma ammonia concentration was 80 μmol/L (normal 5-50). Nasal swab testing confirmed adenovirus by PCR. The gastroenterology consultants concluded that she had acute hepatitis caused by adenovirus.
Her mother continued to insist that the APAP dose was “one mill” (about 32 mg or about 3.6 mg/kg). The dose stated by the mother was well below the usually recommended dose of 10-15 mg/kg in children. The toxicology service remained concerned for APAP toxicity, and she continued receiving IV N-acetylcysteine until her transaminases and INR improved to AST 533 IU/L, ALT 2932 IU/L, and INR 1.49 with total bilirubin 0.6 mg/dL. Hepatic ultrasound was normal. Organic acid screening for metabolic or mitochondrial disorders was normal.
Rapid consultation with a research laboratory specializing in APAP protein adducts led to testing of the original blood for APAP adducts by high performance liquid chromatography with electrochemical detection (HPLC-EC). Four samples all showed APAP-cysteine adduct concentrations of 11 to 12 nmol/mL. Previous research has demonstrated the relationship between serum adducts > 1.0 nmol/mL and ALT values above 1000 IU/L in APAP-related acute liver failure [Citation6]. Children receiving repeated therapeutic doses of APAP during acute illness rarely develop APAP-protein adduct concentrations above 1 nmol/mL [Citation7].
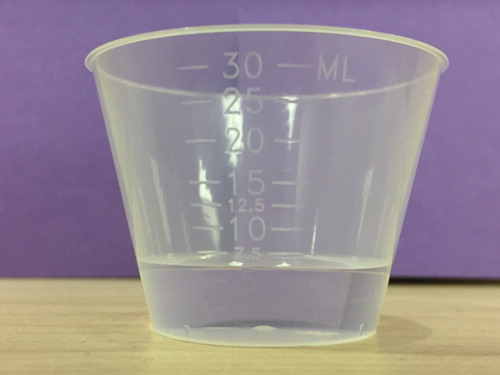
Subsequently, when asked to demonstrate 1 mL with water, the mother filled a medicine cup with 7 mL (). This volume of APAP elixir would contain 224 mg (or about 25 mg/kg per dose). Assuming the child received four doses per day, she likely received approximately 100 mg/kg/d.
Discussion
This case illustrates the diagnostic uncertainty that sometimes occurs with APAP poisoning. The mother’s firm history that she was giving “1 mL” of APAP at a time, and the positive virology test made the diagnosis unclear. Even with her low weight, the stated APAP dose of approximately 32 mg or 3.6 mg/kg per dose was inconsistent with toxicity.
The APAP-protein adducts assay conclusively confirmed the APAP was the direct cause of her liver injury. APAP-protein adduct measurement by HPLC-EC or LC-MS/MS remains experimental and limited to research centers [Citation3–7]. A rapid immunoassay is in development and may become available for clinical use. The immunoassay shows high agreement with HPLC-EC [Citation4].
Conclusion
The assay for APAP-protein adducts is useful in resolving the cause of acute liver injury when the role of APAP is unclear.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Jollow DJ, Mitchell JR, Potter WZ, et al. Acetaminophen-induced hepatic necrosis. II. Role of covalent binding in vivo. J Pharmacol Exper Ther. 1973;187:195–202.
- Potter WZ, Davis DC, Mitchell DR, et al. Acetaminophen-induced hepatic necrosis. III. Cytochrome P-450-mediated covalent binding in vitro. J Pharmacol Exper Ther. 1973;187:203–210.
- Chiew AL, James LP, Isbister GK, et al. Early acetaminophen-protein adducts predict hepatotoxicity following overdose (ATOM-5). J Hepatol. 2020;72:450–462. 10.1016/j.jhep.2019.10.030.
- Roberts DW, Lee WM, Hinson JA, et al. An immunoassay to rapidly measure acetaminophen protein adducts accurately identifies patients with acute liver injury or failure. Clin Gastroenterol Hepatol. 2017;15(4):555–562.
- Heard K, Green JL, Anderson V, et al. Paracetamol (acetaminophen) protein adduct concentrations during therapeutic dosing. Br J Clin Pharmacol. 2016;81(3):562–568.
- Alonso EM, James LP, Zhang S, et al. Acetaminophen adducts detected in serum of pediatric patients with acute liver failure. J Pediat Gastroenterol Nutrit. 2015;61:102–107.
- Jiang S, Vozmediano V, Abdel‐Rahman S, et al. Acetaminophen protein adducts in hospitalized children receiving multiple doses of acetaminophen. J Clin Pharmacol. 2019;59(10):1291–1299.