Abstract
Background
Mushrooms exposures are uncommon, difficult to characterize, and occasionally cause serious morbidity and mortality. We describe mushroom exposures reported to the Kansas Poison Control Center (KSPCC).
Methods
We queried the KSPCC database for all mushroom exposures from 1 January 2013 to 31 December 2018. We abstracted age, sex, exposure date, reason, management site, laboratory values, medical outcome, GI symptoms, interventions, mycologist consultation, presence of mushroom picture, and identification of the mushroom.
Results
We identified 441 cases. Typical cases were young children with exploratory ingestion in summer managed at home (279) with no clinical effect (257). Vomiting or diarrhea occurred in 135 cases. Treatments included either no intervention or PO liquids (304), IV fluids (76), anti-emetics (59), or N-acetylcysteine (5). AST was normal in 52 of 55 cases. CPK was high in 3 of 7 patients. Care included hospital admission (56) including ICU in nine. There were no deaths. Most frequently identified were Chlorophyllum (29) and Psilocybe sp. (13).
Conclusions
Mushroom exposures reported to KPCC were most common in summer months and typically involved unintentional exposures in young children. Vomiting and diarrhea occurred in approximately one-third of cases. Morbidity was minimal. No deaths occurred. In most cases, the mushroom was never identified.
Keywords:
Introduction
Mushroom exposures are a relatively infrequent but consistent source of calls to Poison Centers in the United States with over 6000 exposures reported in 2018 [Citation1,Citation2]. In general, morbidity and mortality from North American mushroom exposures are rare [Citation1,Citation3]. Most result in self-limiting gastrointestinal symptoms with nausea, vomiting, diarrhea and abdominal pain frequently reported [Citation4,Citation5]. However, rare mortality is associated with exposures to Amanita phalloides and other cyclopeptide-containing mushrooms which can cause acute liver injury [Citation6]. Other mushroom species such as Amanita smithiana or those of the Cortinarius genus can cause renal injury [Citation7,Citation8]. Exact identification of mushrooms involved in an exposure is difficult and sometimes impossible in cases where the mushroom has been fully consumed. Regional variability exists for the presence of certain mushroom species, such as Amanita smithiana, but in the majority of United States exposures, the mushroom species remains unknown [Citation9]. Given these facts, studies of the characteristics of local mushroom exposures may benefit in identifying and assisting in the management of patients. Few states have published their experience with mushroom ingestions. We describe the characteristics of Kansas mushroom exposures reported to the Kansas Poison Control Center (KSPCC).
Methods
The Kansas Poison Control Center is the designated regional poison control center for the state of Kansas and receives calls from health care professionals and the public. Trained poison information specialists collect demographic and clinical data for all calls and store them in a searchable, electronic database (TOXICALL®, Computer Automation Systems, Inc.). We queried this database for all human mushroom exposures from 1 January 2013 to 31 December 2018. The University of Kansas Medical Center Institutional Review Board approved this study.
All investigators underwent training to ensure consistent inter-rater reliability in data extraction. We included the following data points: age, sex, date of exposure, reason for exposure, management site and disposition, medical outcome, identity of the mushroom, days of follow up, presence and timing of GI symptoms, and interventions. We categorized the reason for exposure as one of the following five reasons: unintentional/exploratory exposure (limited to children), misuse for hallucinogenic effect, suicide attempt, intentional consumption of the mushroom as food, or unknown. We recorded the following laboratory values when available: creatinine (Cr), aspartate transaminase (AST), international normalized ratio (INR), and creatinine kinase (CPK). In addition, we documented if a mycologist was consulted in the case, if the caller had obtained and submitted a picture of the mushroom, and if the mycologist identified the mushroom. We analyzed all data using Microsoft Excel (Redmond, WA).
Results
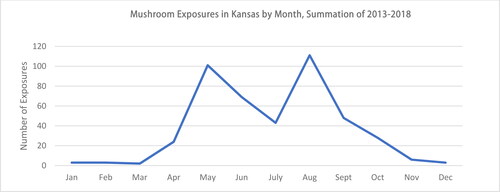
We identified a total of 441 cases between the years 2013 and 2018. displays corresponding demographic and clinical data. The majority of cases (n = 333) were pediatric (age < 18 y.o.) with the average age being 13.2 years (SD 18.5). There were 259 cases (58.7%) with an age of 5 years or younger. Just over half of cases were male (n = 245, 55.6%). demonstrates the exposures per month and by year. Most exposures occurred between May and August. Few exposures occurred in November through March. Geographically, most exposures took place in Sedgwick and Johnson counties, which are the two most populous counties in the state. illustrates the geographical nature of mushroom exposures in Kansas.
Figure 2. Population density of Kansas in 2016 (left) [Citation11] compared with total occurrence of mushroom exposures by county in Kansas from years 2013–2018 (right).
![Figure 2. Population density of Kansas in 2016 (left) [Citation11] compared with total occurrence of mushroom exposures by county in Kansas from years 2013–2018 (right).](/cms/asset/a3eb4b6a-a42e-46cf-ae48-d8fca7ff8859/ttxc_a_1893972_f0002_c.jpg)
Table 1. Demographic and clinical effects of mushroom exposures in Kansas between 2013 and 2018.
Unintentional/exploratory ingestion was the most common reason for exposure, representing over two-thirds of cases (n = 307). There were 38 cases of misuse for hallucinogenic effect. Most cases were able to be managed at home (63%, n = 279) and resulted in no clinical effect (58.3%, n = 257). Vomiting or diarrhea occurred in 135 cases (31%). The time to onset of these symptoms was 3.5 h (SD 4.49) from mushroom ingestion, however the onset of symptoms was obtainable in only 132 cases. Only 15 of these cases had an onset of symptoms greater than 6 h after ingestion. Onset of GI symptoms had no correlation with severity of outcome. Most cases (n = 304) received either no intervention or basic dilution with oral liquids.
The number of cases who sought hospital evaluation was 162 (37%). One hundred and six required only emergency department management. Intravenous fluids were given in 76 cases (17%), and 59 cases (13%) received anti-emetics. Charcoal was given in 56 cases (13%). AST was reported in 55 cases, but in only 3 cases was it over 100 u/L (205-227 u/L). Five cases received N-acetylcysteine. Seven cases had a creatinine kinase (CPK) reported, and in three cases the level was over 1000 u/L, including one case with a max CPK of 27,853 u/L after a reported hallucinogenic mushroom ingestion. In total, fifty-six cases (13%) were admitted to the hospital, including nine (2%) to critical care beds. No deaths occurred.
Of the 441 total exposures, 13 cases were reported to be Psilocybe sp. or “hallucinogenic” mushrooms. Of the remaining 428 exposures, mycologists were consulted for 101 of them (24%), and they identified the mushroom in 76 of those cases (75%). They relied on a photograph for 94.7% of their identifications. For 23 cases (23%), the consulting mycologist could not identify the mushroom despite the availability of a photograph. Chlorophyllum molybdites was the most commonly identified mushroom (n = 29). lists the most commonly identified mushrooms from this study.
Table 2. List of identified mushroom exposures by species and number.
Discussion
Mushrooms are a diverse group of fungi, and their ingestions can lead to variable toxicities depending on the species involved. Most ingestions are nontoxic or result in clinically mild symptoms, however life-threatening ingestions are occasionally reported. The most dangerous North American mushrooms contain cyclopeptides, or amatoxin, and can result in fulminant liver failure. Clinically similar to acetaminophen toxicity, cyclopeptide containing mushrooms cause centrilobular hepatocellular necrosis via inhibition of RNA polymerase II. The majority of North American deaths from mushroom ingestions are attributed to amatoxin-containing mushrooms [Citation12].
While no deaths secondary to mushroom exposures occurred in our study, it is interesting that 5 patients received N-acetylcysteine. We presume this was for suspected liver injury on the part of the clinician given the handful of reported elevations of AST and ALT (however not all patients receiving N-acetylcysteine had documented transaminase levels, and in one case the maximum AST recorded was 28). N-acetylcysteine has hepatoprotective effects and is the mainstay of treatment for acetaminophen ingestion. Similarly, it is recommended in cases of suspected cyclopeptide mushroom exposure, however it is not considered an antidote. All of the patients who received N-acetylcysteine in our study were found to fully recover, and they were ultimately not suspected of cyclopeptide toxicity. This is consistent with the low mortality reported in the available national and regional studies of mushroom ingestions [Citation13,Citation14]. However, a 2000 study in California attributed one death to a cyclopeptide mushroom exposure [Citation3]. Currently, there is no antidote to cyclopeptide toxicity, and rapid decontamination with activated charcoal as well as early referral for liver transplantation remains the mainstay of treatment of suspected cases. Silibinin has been proposed as a potential treatment for cyclopeptide toxicity but was never administered to the patients in our study [Citation8].
Given the challenge in identifying a mushroom following exposure, current medical care focuses on separating severe mushroom toxicities from mild to non-toxic using the variation in clinical presentation. With regards to cyclopeptide-containing mushrooms, a classic teaching is that cyclopeptide mushrooms cause delayed gastrointestinal symptoms, typically greater than 6 h after ingestion, whereas more benign mushroom exposures, as seen with Chlorophyllum sp. (see ), lead to more rapid gastrointestinal irritation, usually seen within the first few hours after exposure. However, it is important to remain cautious as patients who have foraged for mushrooms may have consumed a mixture of different species of mushrooms, and so a lack of rapid onset of symptoms cannot be assumed to exclude cyclopeptide mushroom exposure. We found that the majority of mushroom exposures in Kansas were associated with onset of gastrointestinal symptoms less than 6 h following ingestion, thus likely indicating a benign exposure. Notably, those patients whose symptoms did start more than six hours after ingestion did not go on to mortality in this study.
Overall, our investigation showed that most mushroom exposures in Kansas are both benign and pediatric, which is similar to previously performed national and regional studies [Citation4,Citation12,Citation15,Citation16]. We found that the majority of pediatric exposures were able to be managed at home. This was also noted in a study from Pennsylvania examining “backyard” pediatric exposures where they found that nearly 80% of pediatric mushroom exposures had no effect [Citation17]. It should be noted that in our study, only 58% of pediatric cases called into the KSPCC were asymptomatic. This difference could perhaps be explained by geographic variation in mushroom species or more likely the limitation of the Pennsylvania study to mushrooms exposures occurring only on “cultivated lawn area[s]” [Citation15].
Ideally, management of mushroom exposures would be guided by knowing the specific species that is ingested, however this is frequently difficult to obtain. Our study is one of the first to evaluate the utility of having an on-call mycologist identify the mushroom associated with the exposure. Just under a quarter (23%) of our cases consulted a mycologist, and the identity of the mushroom to at least the genus if not the species was determined in 75% of those cases. However, in 25% of cases submitted to a mycologist, they were neither able to identify the species nor the genus despite having access to a photograph.
Hospital admissions as well as ICU admissions represented a minority of cases in other comparable studies. However, Kansas rates for admissions to critical care beds and non-critical care beds diverged from data obtained from a 2000 California study where they reported 1.0% and 1.5% admission rate, respectively, compared to Kansas PCC data of 2% and 13% for critical care beds and non-critical care beds, respectively [Citation4].
Seven cases diagnosed rhabdomyolysis, including one with a CPK that reached 27,853 u/L for a reported psilocybin mushroom ingestion. Rhabdomyolysis is described albeit rarely with psilocybin ingestions [18]. Rhabdomyolysis-inducing mushrooms are classically associated with Tricholoma equestre, which is described frequently in European case reports with similar measured levels of serum myoglobin [19]. This mushroom is unlikely to have been the culprit in any of the rhabdomyolysis cases seen in this study.
Limitations
There are several limitations inherent to our study. Reporting to the Kansas Poison Control Center is voluntary, and it is possible that not all mushroom exposures were accounted for, resulting in a reporting bias. It is also possible that only serious cases were reported. Many incidental exposures may not have been called into the PCC, or patients perhaps sought medical advice from alternative authorities such as outpatient clinics or emergency departments, who in turn may not have reported the ingestion to the PCC.
Another limitation is incomplete data collection or availability. In some cases, pertinent data may have been missed due to it not being requested by the poison center specialist or simply not being available.
Finally, poison center data does not comment on immigration status which has been shown in other studies to be associated with greater clinical severity of symptoms [Citation3].
Conclusions
The results of this regional study mirror previously reported national data. Clinical effects associated with mushroom exposures reported to the Kansas Poison Control Center were largely benign in nature, and most were able to be managed at home. Exposures commonly took place during summer months and typically involved unintentional ingestions in young children. While vomiting and diarrhea occurred in approximately one-third of cases, basic supportive care measures were typically sufficient. Morbidity was minimal, and mortality was absent. In most cases, the mushroom was never formally identified.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Brandenburg WE, Ward KJ. Mushroom poisoning epidemiology in the United States. Mycologia. 2018;110(4):637–641.
- Gummin DD, Mowry JB, Spyker DA, et al. 2018 annual report of the American Association of Poison Control Centers' National Poison Data System (NPDS): 36th annual report. Clin Toxicol (Phila). 2019;57(12):1220–1413.
- Beuhler MC, Sasser HC, Watson WA. The outcome of North American pediatric unintentional mushroom ingestions with various decontamination treatments: an analysis of 14 years of TESS data. Toxicon. 2009;53(4):437–443.
- Nordt SP, Manoguerra A, Clark RF. 5-Year analysis of mushroom exposures in California. West J Med. 2000;173(5):314–317.
- Barbee G, Berry-Cabán C, Barry J, et al. Analysis of mushroom exposures in Texas requiring hospitalization, 2005-2006. J Med Toxicol. 2009;5(2):59–62. PubMed PMID: 19415588; PubMed Central PMCID: PMC3550325.
- Vo KT, Montgomery ME, Mitchell ST, et al. Amanita phalloides mushroom poisonings - Northern California, December 2016. MMWR Morb Mortal Wkly Rep. 2017;66(21):549–553.
- West PL, Lindgren J, Horowitz BZ. Amanita smithiana mushroom ingestion: a case of delayed renal failure and literature review. J Med Toxicol. 2009;5(1):32–38.
- Judge BS, Ammirati JF, Lincoff GH, et al. Ingestion of a newly described North American mushroom species from Michigan resulting in chronic renal failure: Cortinarius orellanosus. Clin Toxicol (Phila). 2010;48(6):545–549.
- Tulloss RE, Lindgren JE. Amanita smithiantaxonomy, distribution, and poisonings. Mycotaxon. 1992;45:373–387.
- Enjalbert F, Rapior S, Nouguier-Soulé J, et al. Treatment of amatoxin poisoning: 20-year retrospective analysis. J Toxicol Clin Toxicol. 2002;40(6):715–757.
- Kansas Population by County. Maps of World. 2019. Available from: https://www.mapsofworld.com/usa/states/kansas/population.html.
- Diaz JH. Evolving global epidemiology, syndromic classification, general management, and prevention of unknown mushroom poisonings. Crit Care Med. 2005;33(2):419–426.
- Trestrail JH, III. Mushroom poisoning in the United States-an analysis of 1989 United States Poison Center data. J Toxicol Clin Toxicol. 1991;29(4):459–465.
- Gussow L. The optimal management of mushroom poisoning remains undetermined. West J Med. 2000;173(5):317–318. PubMed PMID: 11069865; PubMed Central PMCID: PMC1071150.
- Kintziger KW, Mulay P, Watkins S, et al. Wild mushroom exposures in Florida, 2003-2007. Public Health Rep. 2011;126(6):844–852. PubMed PMID: 22043100; PubMed Central PMCID: PMC3185320.
- Mrvos R, Swanson-Biearman B, Krenzelok EP. Backyard mushroom ingestions: no gastrointestinal decontamination-no effect. J Emerg Med. 2007;33(4):381–383. Epub 2007 Jul 20.
- Bickel M, Ditting T, Watz H, et al. Severe rhabdomyolysis, acute renal failure and posterior encephalopathy after 'magic mushroom' abuse. Eur J Emerg Med. 2005;12(6):306–308. PMID: 16276262.
- Laubner G, Mikulevičienė G. A series of cases of rhabdomyolysis after ingestion of Tricholoma equestre. Acta Med Litu. 2016;23(3):193–197. PubMed PMID: 28356809; PubMed Central PMCID: PMC5287993.