Abstract
Midodrine is a prodrug metabolized to the peripheral acting alpha agonist desglymidodrine and is used to treat orthostatic hypotension. Reports of overdose are rare, consequently there is little guidance regarding treatment of overdose. We report a case of toxicity following midodrine overdose and describe clinical findings and response to treatment. We also review the prior reported cases to determine what clinical findings are consistent and suggest a therapeutic approach. A 65-year-old man ingested 500 milligrams of midodrine. The patient presented to the emergency department within 45 min of the ingestion asymptomatic but with a blood pressure of 246/151 mmHg and heart rate of 69 beats per minute. The patient was treated for approximately 24 h with intravenous nitroglycerine with decrease in blood pressure. The patient recovered without apparent adverse sequelae. Midodrine overdose produces marked hypertension and relative bradycardia. These effects occur rapidly and resolve. Nitroglycerin appears to be safe and effective in controlling blood pressure following midodrine overdose.
Introduction
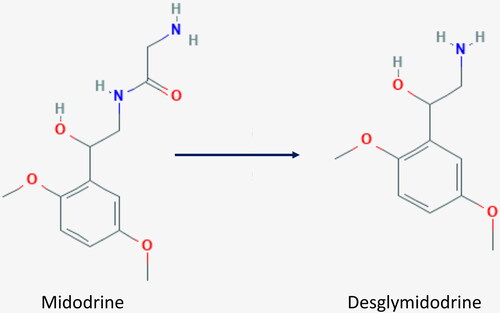
Midodrine is a prodrug metabolized to desglymidodrine, an alpha 1 receptor agonist of the arteriolar and venous vasculature () [Citation1]. There are few reports describing toxicity and no clear consensus regarding management [Citation1–5].
We treated a 65-year-old man following the largest total milligram (mg) overdose of midodrine reported. We report our experience, in accord with the CARE guidelines, and review previous reports in an effort to suggest an approach to overdose and toxicity.
Case report
A 65-year-old man with a history of atrial fibrillation, hypertension, diabetes, orthostatic hypotension, and sleep apnea presented approximately 45 min after ingestion of 500 mg of midodrine. The patient was asymptomatic. Vitals signs included blood pressure (BP) of 246/151 mmHg (baseline 140/80 mmHg) and pulse of 69 beats per minute (BPM). Physical examination was unremarkable. Diagnostic studies (chest x-ray, complete blood count, electrolytes, blood urea nitrogen, salicylate and acetaminophen concentrations) were normal or negative excepting a mild increase in troponin I of 0.473 ng/mL (normal < 0.1 ng/mL). Electrocardiogram revealed non-specific t wave changes in the inferior and lateral leads.
The patient received infusion of nitroglycerin (NTG) at 10–15 micrograms per minute to maintain BPs ranging from 184/89 to 147/79 mmHg. NTG was rapidly weaned from 15 to 5 micrograms per minute after 19 h then discontinued after 21 h. His BP 3 h after discontinuing NTG was 144/71 mmHg. Repeat troponin concentration drawn after 12 h was 0.430 ng/mL. He suffered no apparent sequelae.
Discussion
Adverse effects of therapeutically dosed midodrine include hypertension and bradycardia [Citation6,Citation7]. Few cases of overdose have been described. Hofer et al. published (in abstract) a series of five children and five adults identified retrospectively from a poison control center database [Citation2]. Seven patients developed bradycardia, confirmed to be sinus bradycardia in three patients, and hypertension. All recovered fully without intervention [Citation2]. Gao and O’Connell reported (in abstract) a case of a woman who ingested between 200 and 250 mg of midodrine and developed junctional bradycardia and BP of 154/80 mmHg. She recovered rapidly and uneventfully [Citation3]. The midodrine package insert reports two cases of overdose with minimal details. One patient was treated with 20 mg phentolamine after ingestion of 250 mg and development of a BP of greater than 200 mmHg and discharged “shortly” thereafter. The second patient, described as obtunded after ingestion of 205 mg midodrine, underwent gastric lavage and recovered within 24 h [Citation1]. Willner reported (in abstract) a case of a 48-year-old woman who ingested between 300 and 400 mg of midodrine and developed subarachnoid hemorrhage and posterior reversible encephalopathy syndrome (PRES). She was initially treated with intravenous NTG then switched to nicardipine with the mean arterial pressure lowering from a peak of 137 mmHg to 65–90 mmHg while on nicardipine. The patient “recovered well” [Citation4]. We find one case published as full manuscript describing a 22-year-old woman who ingested up to 350 mg midodrine and developed lethargy, hypertension and bradycardia. The patient was treated with transdermal nitrates and recovered uneventfully [Citation5].
Review of our case and the cases reported previously reveals several repeated observations which are consistent with the known therapeutic effects of midodrine and suggest an approach to evaluation and therapy following overdose.
The existing evidence suggests that toxicity is of rapid onset and resolves quickly. Our patient presented within 45 min of ingestion with a markedly elevated BP. In the report by Wong et al. the time from ingestion to development of toxicity was reported to be 2.5 h [Citation5]. Rapid rise in BP likely contributed to the development of PRES syndrome in the case reported by Willner et al. [Citation4]. Midodrine is known to be rapidly absorbed with a rapid onset of action following therapeutic dosing [Citation7]. The period of toxicity observed for our patient was brief-approximately 21 h. All prior reports that document duration of toxicity indicate that this is less that 24 h [Citation1,Citation4,Citation5].
The predominant physical finding noted in 11 of the 15 previously reported cases was bradycardia (three sinus, one junctional, others not described) [Citation1–5]. Three of the four patients without bradycardia were children under the age of two years [Citation1,Citation2].
Important issues are choice of therapeutic agents and duration of observation or therapy. Given the rapid onset of symptoms, frequency of developing bradycardia, rapid recovery and likely mechanism of toxicity, agents producing vasodilatation without effect on cardiac conduction that can be rapidly titrated would seem the agents of choice. While Willner reports using nicardipine in the setting of subarachnoid hemorrhage, combined experience, including our case, would suggest that nitrates be used as first line agents [Citation4,Citation5]. Further, the rapid rise in BP suggests that therapy be aimed at return to baseline BP rather than the limited reduction indicated for treatment of hypertensive emergency where there are concerns regarding cerebral vascular autoregulation. Lack of adverse sequelae with rapid lowering of BP in our case and the cases previously reported supports this approach. Given the majority of good outcomes with effective BP control patients may not require intensive care units. Also, given the apparent rapid onset and resolution of toxicity a prolonged period of observation of asymptomatic patients following reported ingestion may not be necessary.
Disclosure statement
The authors (Jessica Peck MD and Steven D. Salhanick, MD) report no conflicts of interest. This data has not been previously presented.
References
- Product information: ProAmatine®, midodrine. Eatontown (NJ): Roberts Pharmaceutical Corporation; 1998.
- Hofer KE, Rauber-Lüthy C, Kupferschmidt H, et al. Acute midodrine overdose: a case series. Clin Toxicol. 2012;50(4):362.
- Gao H, O’Connell C. Midodrine overdose presenting with junctional bradycardia. Clin Toxicol. 2019;57(10):947.
- Willner C. A pressing matter of drug toxicity. Chest. 2017;152(4):A381.
- Wong LY, Wong A, Robertson T, et al. Severe hypertension and bradycardia secondary to midodrine overdose. J Med Toxicol. 2017;13(1):88–90.
- McClellan KJ, Wiseman LR, Wilde MI. Midodrine. A review of its therapeutic use in the management of orthostatic hypotension. Drugs Aging. 1998;12(1):76–86.
- McTavish D, Goa KL. Midodrine. A review of its pharmacological properties and therapeutic use in orthostatic hypotension and secondary hypotensive disorders. Drugs. 1989;38(5):757–777.