Abstract
Ethylene glycol toxicity can be fatal without prompt treatment. Treatment options may include ethanol, fomepizole, and intermittent hemodialysis (IHD). IHD is usually preferred; however, depending on a patient’s clinical presentation continuous renal replacement therapy (CRRT) for the removal of ethylene glycol may be desirable. A 36-year-old male presented after transfer from a referring hospital with coma, severe acidosis, and elevated osmolal gap. With suspicion of toxic alcohol poisoning, an ethylene glycol serum concentration was ordered and eventually resulted at 163 mg/dL. The care team decided to initiate treatment with fomepizole and IHD. Due to severe hypotension requiring vasopressors, the patient underwent CRRT in lieu of IHD. We further describe the rapid clearance of ethylene glycol with concurrent fomepizole and CRRT. High flow rate continuous venovenous hemodiafiltration (CVVHDF) combined with fomepizole, removes ethylene glycol from the body in a timely manner.
Introduction
Ethylene glycol is a chemical most commonly found in antifreeze. In 2019, the American Association of Poison Control Centers recorded 6,739 ingestions of automotive ethylene glycol with 12 reported deaths [Citation1]. Despite typically being a severe poisoning, patients can survive with fast and accurate treatment.
In clinical practice, an ethylene glycol concentration of 50 mg/dL is a widely acceptable threshold for initiation of treatment with both an inhibitor of alcohol dehydrogenase (ethanol and fomepizole) and hemodialysis [Citation2]. Since timely ethylene glycol concentrations are seldom available, suspicion of ethylene glycol poisoning with a high anion gap metabolic acidosis, or high osmol gap warrants antidotal treatment and hemodialysis [Citation3,Citation4]. At this time the only FDA approved pharmacologic agent is fomepizole, which exerts its clinical effects by competitively inhibiting alcohol dehydrogenase (ADH). Inhibition of ADH prevents the metabolism of ethylene glycol into its toxic metabolites glycolic acid and oxalic acid [Citation5,Citation6]. In regards to dialysis, intermittent hemodialysis (IHD) is preferred, however, using IHD may be challenging in hemodynamically unstable patients. Continuous renal replacement therapy (CRRT) or sustained low efficiency dialysis (SLED) would be the next option for hemodynamically unstable patients [Citation7]. To our knowledge, there are two case reports on the use of CRRT with ethylene glycol poisoning [Citation8,Citation9].
In accordance with the CARE guidelines (https://www.care-statement.org), we report rapid and successful clearance of ethylene glycol using fomepizole and CRRT in a patient with severe ethylene glycol poisoning. The authors obtained consent from the next of kin.
Case report
Emergency services brought a 36-year-old male (weight 66 kg) with past medical history significant for alcohol abuse to a referring hospital after family found him unresponsive with agonal breathing. Upon evaluation, the referring hospital sought further transfer to our facility for higher level of care. Per the family, they last saw the patient approximately two-and-a-half hours prior to finding him. The family also reported the patient had a binge drinking episode four to five days prior, and in the days following, the patient was not feeling well, but he did not complain of any fever, headache, or neck pain.
At the referring hospital, the patient presented with a Glasgow Coma Score (GCS) of 3, pH < 6.8 and potassium > 6 mEq/L, he was emergently intubated. Upon admission to our facility, pertinent vitals were: blood pressure 154/119 mmHg, pulse rate 137 beats/min, and tympanic temperature 36.2 °C. Laboratory values showed hyperkalemia and anion gap metabolic acidosis (). Of note the urine drug screen was negative for methamphetamines, benzodiazepines, opiates, amphetamines, barbiturates, and cocaine. The patient was admitted to the intensive care unit (ICU) for further evaluation and management.
Table 1. Laboratory values upon admission.
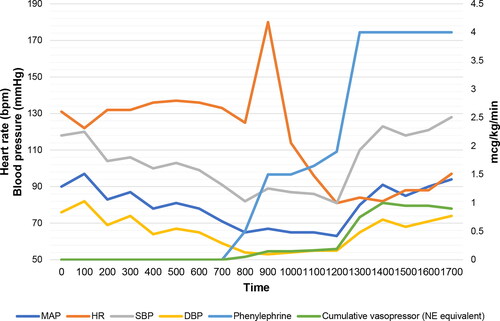
Approximately 12 h after admission an ethylene glycol concentration resulted at 163 mg/dL, as well as a serum osmolality of 338 mOsm/kg and the osmolal gap at 46 mOsm/kg. As soon as the ethylene glycol concentration result was available, the care team consulted the local poison control and fomepizole was to be initiated at a dose of 15 mg/kg every 4 h with planned hemodialysis. However, the patient went into refractory shock requiring increasing doses of vasopressors and sodium bicarbonate infusion (). Due to the unstable hemodynamics, IHD was not feasible and instead the team initiated continuous venovenous hemodiafiltration (CVVHDF). The CVVHDF specifics are as follows; an average filter pressure of 168 mHg, blood flow rate of 200 mL/min, pre-blood pump of 2000 mL/h, dialysate of 2000 mL/h, replacement filter 2000 mL/h, and effluent dose of 76 mL/kg/h. PrismaSOL BGK 4/2.5 solution® was used. The filter was changed every 72 h or when 780 L had been processed.
Figure 1. Hemodynamics and vasopressor doses. Change in hemodynamics: heart rate (HR), MAP (Mean arterial pressure), SBP (systolic blood pressure), DBP (diastolic blood pressure) from admission (time = 0) till 17:00 the same day. Escalation in phenylephrine dose and cumulative vasopressor doses (in norepinephrine equivalent dose) from admission (time = 0) till 17:00 the same day.
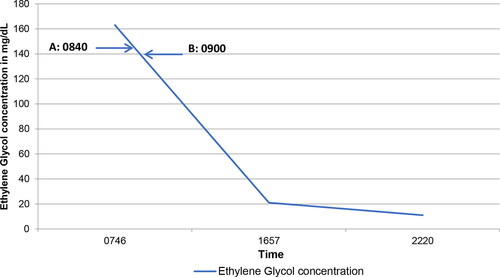
After the initiation of fomepizole and CRRT, repeat ethylene glycol concentrations were drawn (). Eight hours after initiating treatment the ethylene glycol concentration was 21 mg/dL, with the next concentration at roughly another five-and-a-half hours resulting at 11 mg/dL. At this time, CRRT continued without fomepizole for another day due to acute kidney injury and ongoing high anion gap metabolic acidosis.
Figure 2. Ethylene glycol concentration in relation to treatment. Ethylene glycol concentration was 163 mg/dL at 07:46. A = Fomepizole started. B = Initiation of continuous renal replacement therapy. Ethylene glycol concentration dropped to 21 mg/dL and 11 mg/dL at 16:57 and 22:20, respectively.
Due to continued coma after fomepizole and CRRT treatment, he underwent magnetic resonance imaging (MRI) of the brain with and without contrast, which indicated anoxic or metabolic injury with abnormalities in the basal ganglia, thalamus, midbrain, posterior pons, and medulla. The patient ultimately succumbed to complications of anoxic and metabolic injury from ethylene glycol poisoning.
Discussion
Ethylene glycol poisoning may result in different clinical presentations based on arrival time post ingestion. Physical signs may range from inebriation without an “ethanol” smell to comatose [Citation10,Citation11]. Hallmark laboratory findings include an osmolal gap, metabolic acidosis, and elevated ethylene glycol concentration [Citation2–7,Citation10,Citation11]. Starting fomepizole treatment at an ethylene glycol concentration of 20 mg/dL or greater is appropriate [Citation2]. In this case, the patient arrived in a comatose state, with a high anion gap metabolic acidosis with no initial serum osmolality measured. Based on history reported by the family, the patient most likely consumed the ethylene glycol four to five days prior with co-ingestion of high amounts of ethanol. When resulted, the patient had an ethylene glycol concentration roughly eight times greater than current recommendations indicate for initiating treatment.
Although, the parent compound, ethylene glycol, is non-toxic, its metabolites are [Citation12]. Ethylene glycol is rapidly absorbed in the gastrointestinal tract, and its small volume of distribution (0.5 to 0.8 L/kg) allows for wide and rapid distribution throughout the body [Citation2,Citation13]. The first step of metabolism occurs via ADH; which converts ethylene glycol to glycolic acid, which is then further metabolized to oxalic acid. The buildup of glycolic acid leads to metabolic acidosis. Whereas, oxalic acid binds with calcium, forming calcium crystals that distribute throughout the body and end up in organs, eventually leading to organ failure; including myocardial, neurologic, pulmonary, and renal failure [Citation2,Citation14]. In this specific patient, the organ damage caused by theses formed crystals was the ultimate reason for fatality.
Without intervention, the elimination of ethylene glycol by the kidneys is about 20%, with a half-life of three to eight hours [Citation13]. However, with the concurrent consumption of ethanol the elimination half-life is increased to 17 h. With initiation of treatment, half-life of ethylene glycol with fomepizole only is roughly 19 h and four hours with the addition of hemodialysis. In comparison, the half-life of glycolic acid is 10 h with initiation of fomepizole and three hours with the addition of hemodialysis [Citation13]. Since fomepizole is actively dialyzed, frequency was increased from every 12 h to every 4 h during IHD [Citation3,Citation15]. Due to the patient becoming hemodynamically unstable, the use of CRRT was more feasible than IHD. The use of CRRT was important to clear the ethylene glycol quicker than fomepizole could alone. The downside to CRRT is that it occurs at slower clearance rate in comparison to IHD [Citation7]. Knowing this major difference in dialysis procedures, the decision was made to use a high flow rate during CRRT. Ultimately, a blood flow rate of 200 mL/h, effluent dose of 76 mL/kg/h and dialysate rate of 2000 mL/h, along with fomepizole reduced the ethylene glycol concentration from 163 mg/dL to 21 mg/dL in roughly eight hours. After another five hours, the ethylene glycol concentration dropped from 21 mg/dL to 11 mg/dL. A total of six doses of fomepizole were administered.
Both the available case reports did not discuss the CRRT effluent rate or treatment details. In the case report by Chukkambotla et al., fomepizole was not used to treat the patient [Citation9]. Kamps et al., used fomepizole with an initial dose of 780 mg (based on body weight) followed by 1 mg/kg/hour continuous infusion [Citation8]. Ethylene glycol follows first order kinetics [Citation16]. Kamps et al. observed an elimination rate constant of 0.1805 h−1 and the half-life of 3.84 h compared to an elimination rate constant of 0.247 h−1 and a half-life of 2.81 h in our case [Citation8]. In a retrospective study by Iliuta et al., the ethylene glycol median half-life in patients with AKI on high efficiency IHD was 2.92 h [Citation14], which is comparable to the half-life in our case (2.81 h). The median blood flow rate was 379 mL/min which is higher than the blood flow rate in our case (200 mL/min). However, Iliuta et al. did not observe an association between the blood flow rate and the ethylene glycol half-life [Citation14].
This is the first report that details the use fomepizole in combination with CRRT to treat severe ethylene glycol toxicity. This case illustrates that CVVHDF can effectively remove ethylene glycol with extraction that is comparable to IHD.
Disclosure statement
The authors have disclosed that they do not have any conflicts of interest.
References
- Gummin DD, Mowry JB, Beuhler MC, et al. 2019 Annual report of the American association of poison control centers’ national poison data system (NPDS): 37th annual report. Clin Toxicol (Phila). 2020;58(12):1360–1541.
- Barceloux DG, Krenzelok EP, Olson K, et al. American academy of clinical toxicology practice guidelines on the treatment of ethylene glycol poisoning. Ad Hoc Committee. J Toxicol Clin Toxicol. 1999;37(5):537–560.
- Sivilotti MLA, Burns MJ, McMartin KE, et al. Toxicokinetics of ethylene glycol during fomepizole therapy: Implications for management. Ann Emerg Med. 2000;36(2):114–125.
- Mégarbane B, Borron SW, Baud FJ. Current recommendations for treatment of severe toxic alcohol poisonings. Intensive Care Med. 2005;31(2):189–195.
- Brent J, McMartin K, Phillips S, et al . Fomepizole for the treatment of ethylene glycol poisoning. Methylpyrazole for Toxic Alcohols Study Group. N Engl J Med. 1999;340(11):832–838.
- Baud FJ, Bismuth C, Garnier R, et al. 4-Methylpyrazole may be an alternative to ethanol therapy for ethylene glycol intoxication in man. J Toxicol Clin Toxicol. 1986;24(6):463–483.
- Goodman JW, Goldfarb DS. The role of continuous renal replacement therapy in the treatment of poisoning: CRRT and poisoning. Semin Dial. 2006;19(5):402–407.
- Kamps MJA, Vermeulen Windsant-van den TA, de Jager CPC. Intoxication with ethylene glycol treated with fomepizole: a case report. Neth J Crit Care. 2014;18(4):24–26.
- Chukkambotla S, Hurst T. Ethylene glycol poisoning - a challenge for the intensivist. J Intensive Care Soc. 2007;8(3):33–35.
- Moreau CL, Kerns W, Tomaszewski CA, et al . Glycolate kinetics and hemodialysis clearance in ethylene glycol poisoning. META Study Group. J Toxicol Clin Toxicol. 1998;36(7):659–666.
- Velez LI, Gracia R, Neerman MF. Ethylene glycol poisoning: current diagnostic and management issues. J Emerg Nurs. 2007;33(4):342–345.
- Jacobsen D, Øvrebø S, Østborg J, et al. Glycolate causes the acidosis in ethylene glycol poisoning and is effectively removed by hemodialysis. Acta Med Scand. 1984;216(4):409–416.
- Kraut JA, Kurtz I. Toxic alcohol ingestions: clinical features, diagnosis, and management. Clin J Am Soc Nephrol. 2008;3(1):208–225.
- Iliuta IA, Lachance P, Ghannoum M, et al . Prediction and validation of the duration of hemodialysis sessions for the treatment of acute ethylene glycol poisoning. Kidney Int. 2017;92(2):453–460.
- Jacobsen D, Østensen J, Bredesen L, et al. 4-Methylpyrazole (4-MP) is effectively removed by haemodialysis in the pig model. Hum Exp Toxicol. 1996;15(6):494–496.
- Kim Y. Plotting of ethylene glycol blood concentrations using linear regression before and during hemodialysis in a case of intoxication and pharmacokinetic review. Case Rep Nephrol. 2015;2015:359101–359104.
