Abstract
Incidence of carbon monoxide (CO) poisoning in Nepal has not been studied. The objective of this study was to evaluate baseline carboxyhemoglobin (COHb) concentrations, population risk factors, and incidence of CO poisoning at a single hospital in Nepal. This was a prospective, observational study of patients presenting to Patan Hospital Emergency Department from April 2019 to March 2020. Demographics, risk factors for CO poisoning, symptoms, and clinical pretest probability of CO poisoning was documented. COHb concentration was obtained using a noninvasive co-oximeter. Significant CO exposure was defined as COHb concentration > 10%. CO poisoning was defined as COHb > 10% coupled with symptoms. Of 1,040 patients, 745 patients had a recordable COHb concentration. Median age was 40 years (IQR 33) with 407 (55%) females. Average COHb was 7.2%. Warm months were associated with higher COHb concentrations (8.1% vs 6.0%, p < 0.05). Firewood use had higher COHb concentrations compared to gas heating (8.6% vs 7.0%, p < 0.05). Overall, 228 (31%) patients had a COHb concentration > 10% indicating significant CO exposure. Sixteen patients had CO poisoning. We found a significant baseline incidence of COHb > 10% (31%) in patients presenting to a hospital in Nepal. Risk factors for higher baseline COHb concentrations included warm months and cooking with firewood.
Introduction
Carbon monoxide (CO) poisoning is a common cause of accidental and preventable death worldwide. In the United States, a study evaluating unintentional, non-fire related CO poisonings from 1999-2010 noted an average of 430 deaths per year [Citation1]. Nationwide, individuals in Nepal are exposed to higher concentrations of carbon monoxide. Home cooking and heating mechanisms commonly rely on solid fuels, including charcoal, coal, cropwaste, dung and wood [Citation2,Citation3]. In the setting of generally poor indoor ventilation, carbon monoxide may accumulate in the ambient air, posing an ongoing health hazard. Various organizations working with United Nation Foundation’s Global Alliance for Clean Cookstoves project have installed improved cookstoves that aim to decrease the amount of indoor air pollution [Citation4]. A study showed that although there were subjective improvements in the cooking experience, carbon monoxide concentrations were still above the safe level set by the World Health Organization [Citation5,Citation6].
Similar to most health facilities in Nepal, the diagnosis of CO poisoning at Patan Hospital is clinical; there is no mechanism to test for CO poisoning by either blood sampling or CO-oximetry. In suspected cases, patients are empirically treated with oxygen via face mask. Additionally, there are no studies evaluating risk factors, baseline carboxyhemoglobin (COHb) concentration or prevalence of CO poisoning in Nepal. The majority of reports are in Nepali news articles with suspected poisonings based on clinical suspicion [Citation7,Citation8].
The objective of this study was to evaluate baseline COHb concentration, population risk factors, and incidence of CO poisoning in patients presenting to the emergency department in a single hospital in Nepal.
Methods
Study design
A prospective observational study of patients presenting to Patan Hospital Emergency Department was performed over one year from April 2019 until March 2020. Ethical approval was obtained from the Patan Academy of Health Sciences Institutional Review Committee (drs1901181238) and Indiana University Institutional Review Committee (#1808991747).
Study settings
The study was performed at Patan Hospital Emergency Department. Patan Hospital is a large urban teaching hospital located in Kathmandu Valley that cares for approximately 48,000 patients each year. The Kathmandu Valley is located at an elevation of 1400 meters. The climate is mild with average temperatures ranging during the warm months (March – September) between 63-75 °F (17-24 °C) with temperature highs around 85 °F (29 °C) [Citation9,Citation10]. During colder months (October – February), there is a wider range of average temperatures from 50-68 °F (10-20 °C) with temperatures cold at night and milder during the day [Citation9,Citation10]. Located in a valley with a dense population and growing industrialization, Kathmandu had a PM2.5 reading of 48 µg/m3 as a yearly average in 2019, placing it in an unhealthy category for air quality, significantly higher than the WHO guideline that recommends an annual average PM2.5 less than 5 µg/m3 to protect the public from the health effects of pollution [Citation6,Citation11].
Study population
All patients 18 years and older presenting to the Patan Emergency Department were eligible for inclusion. If patients required immediate resuscitation, participants or families were surveyed once stabilized.
Study protocol
The authors studied a convenience sample of patients presenting to the Emergency Department over the course of one year. To collect a representative sample of patients presenting to the ED, we chose different days of the week and times of the day to collect the data. During those collection times, we collected data on all the patients in the ED at that time. If a patient with a high suspicion of CO poisoning presented outside of these data collection periods, clinicians also collected data on these patients.
Informed consent was obtained from the patient or family. Demographic information (age, sex, occupation), smoking status, vital signs, chief complaint, and any symptoms suggestive of CO poisoning (headache, dizziness, weakness, nausea/vomiting, chest pain, syncope, seizure, or confusion) were logged on a data collection form. Information about the home including cooking and heating source was also collected. The provider was then asked to record a pretest probability of CO poisoning based on history and clinical examination. High pretest probability was based on clinical history, risk factors, and symptoms suggestive of CO poisoning.
Patients then had a noninvasive COHb concentration recorded using Rad57 Masimo. This measurement is taken similar to pulse oximetry. The Rad57 Masimo CO-oximeter was approved with data demonstrating COHb concentrations varied from 1-3% above or below the blood COHb concentration [Citation12]. The measurements were entered on the data collection form by the study personnel or physician caring for the patient. For the purposes of the study, a significant CO exposure was defined as a COHb concentration > 10%, as this level is typically outside the physiological range and the concentration at which poisoning is often considered to have occurred [Citation13,Citation14].
Patients with clinical suspicion of CO poisoning or symptoms of CO poisoning and COHb concentrations greater than 10% were diagnosed with CO poisoning and treated accordingly. Additionally, information regarding other family members in the home was gathered for appropriate risk stratification to provide appropriate counseling. For those who had high concentration and risk factors, counseling was given for those risk factors and to ensure family members were aware of their risks for CO poisoning and appropriate prevention measures.
Statistical analysis
Descriptive statistics were used to determine prevalence, average baseline COHb concentration, and percentage of patients with risk factors. Comparison of mean COHb concentrations for demographics variables and risk factors were analyzed using independent sample t-test. Chi-square test was used to evaluate association of COHb > 10 with demographic variables and risk factors. Logistic regression was also done to evaluate any correlation between COHb concentration with monthly temperatures.
Results
Our study included 1,040 patients who completed the questionnaire. Of these, 745 patients had a recordable COHb concentration using the CO-oximeter. Median age was 40 years (IQR 33) with 407 (55%) female patients and 153 (21%) smokers ().
Table 1. Patient demographics with COHb recordings.
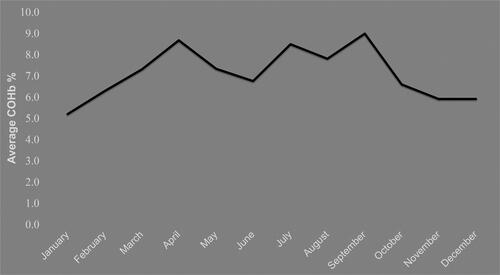
Four hundred twenty-five (57%) patients were assessed during warm months (March-September) and 320 (43%) were assessed during cold months (October-February). The overall average COHb was 7.2%. During warm months, patients had an average COHb concentration of 8.1% compared to winter months with an average COHb of 6.0%, which was statistically significant (p < 0.05) ( and ). Also the incidence of COHb > 10% was significantly higher in warmer months than colder months (p < 0.001). Also, there was a strong correlation between average COHb concentration and average monthly temperatures (r = 0.91) ().[Citation9]
Figure 2. Correlation (r = 0.91) between average COHb recordings and average daily temperatures when controlling for same cooking source and number of windows in the home [Citation9].
![Figure 2. Correlation (r = 0.91) between average COHb recordings and average daily temperatures when controlling for same cooking source and number of windows in the home [Citation9].](/cms/asset/ca271469-0776-407b-9af7-5b62fef0ea37/ttxc_a_2010955_f0002_c.jpg)
Occupations were divided into farmer/outdoor-based occupation (n = 121), home/home-based trade (n = 336), or office/merchant trade (n = 288). There were no significant differences in COHb concentrations between the three groups of occupation.
Regarding cooking source, those using firewood alone had statistically significantly higher COHb concentrations compared to those using any gas heat and was associated with higher incidence of CO poisoning ().
Table 2. Demographics and factors related to patients with COHb > 10%.
Two hundred twenty-eight (31%) of the patients were identified as having a significant CO exposure based on a COHb concentration > 10%. All patients with high pretest probability of having CO poisoning were identified during the winter, 16 out of 228. All of these patients were either sleeping in an enclosed space without a vent, showering with a gas geyser, or using a sauna ().
Table 3. History of patients with high-pretest probability for CO poisoning.
Of 1040 patients, 295 COHb concentrations were unobtainable. As age increased, the percentage of patients with unrecordable concentrations increased. Of patients below 40 years, 17% had COHb concentration that could not be obtained while 30% of patients age 40-59 and 42% of patients over 60 years had a unrecordable COHb concentrations. COHb concentrations in patients with a SPO2 < 92% were more likely to be unobtainable – only 13 of 121 patients had obtainable COHb concentrations when SPO2 < 92%.
Discussion
This is the first study to evaluate the incidence and risk factors of CO exposure and poisoning in an Emergency Department population in Nepal.
Our study found the average COHb concentration was 7.2% regardless of smoking history. This is higher than expected, especially among nonsmokers who usually have COHb concentration <3% [Citation15]. It is possible that the common practices for cooking and heating in Nepal compounded by air pollution have caused chronic CO exposure, leading to this higher baseline COHb concentration. In contrast to the studies done in Turkey and Israel [Citation16,Citation17], this study showed significantly higher COHb concentrations in warm months compared to cold months. Increased concentrations in the warmer months may be due to Nepali people staying indoors more during the summer/monsoon months [Citation18]. This unexpected finding emphasizes the need to consider CO poisoning in warmer months when baseline concentrations are higher, indicating exposure may be more significant during this season. Use of the CO-oximeter as a screening tool may help clinicians identify patients with CO poisoning, especially during “atypical” seasons when exposures may be hard to identify and symptoms can be subtle [Citation19].
Our study also revealed that while the majority of patients used natural gas for cooking in comparison to firewood, those using only firewood were more vulnerable to CO poisoning compared to those using gas. This was not surprising as firewood generates more CO emission compared to gas (52.8 to 14.2 gm/kg) [Citation20].
Similar to other case reports in Nepal, we found patients presenting with CO poisoning related to gas geyser use in showers and saunas [Citation21,Citation22]. Geysers that heat showers and saunas are connected to a liquid petroleum gas cylinder. During combustion, carbon dioxide is predominantly produced with a small amount of carbon monoxide; however, in small rooms with poor ventilation, there is an increase in carbon monoxide due to incomplete combustion [Citation23]. The exposure is further exacerbated by the small space and poor ventilation. Further public health education regarding risk of using firewood for cooking and gas geysers in showers could help individuals take appropriate precautions to avoid CO poisoning.
The noninvasive readings using the CO-oximeter did not give any reading in 28% of patients, with larger percentage of unrecordable readings in older patients. This could be due to thickened skin over time from manual labor or worsening hypoxia with progressing lungs diseases, such as chronic obstructive pulmonary disease [Citation24,Citation25]. It is helpful to understand the limitations of the noninvasive CO-oximeter and advocate for laboratory blood gas measurements of COHb in this patient population or when CO-oximeter concentrations are not attainable.
This study has several limitations. While we attempted to collect a representative sample, this study was a convenience study and only collected a small portion of the patients presenting to a single ED. Despite this, the high percentage of elevated CO concentration highlights the need for further study on CO poisoning in Nepal. The study was also based on use of noninvasive CO-oximetry instead of the gold standard blood COHb measurement. The CO-oximeter was approved with COHb concentrations varying from 1-3% above or below the blood COHb concentration [Citation12]. Several studies have shown varying results both questioning and supporting use of noninvasive CO-oximetry, demonstrating the importance of comparison with blood COHb concentrations for validation in this population [Citation19,Citation26–29]. Also, readings were difficult to obtain in hypoxic patients and the elderly. Therefore, this population of patients, who may have been more likely to have CO poisoning, could not be adequately included in this study. Further study evaluating definitive diagnostic testing for CO poisoning is needed in low-resource settings.
Conclusion
We found a significant baseline incidence of COHb > 10% (31%) in a convenience sample of adult patients presenting to a hospital in Nepal. Risk factors for higher baseline COHb concentrations identified in this sample included warmer months and cooking with firewood. This study highlights that CO poisoning should remain on the differential even in warmer months.
Acknowledgments
We thank the doctors and staff of Patan Hospital and the General Practice and Emergency Department for their support and assistance with this study. We also thank Dr. Mark Liao for donation of the Rad57 Masimo CO-oximeter for this study.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Centers for Disease Control and Prevention. QuickStats: Average Annual Number of Deaths and Death Rates from Unintentional, Non–Fire-Related Carbon Monoxide Poisoning,*† by Sex and Age Group — United States, 1999. –2010 2014 [cited 2020 March 19]. Available from: https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6303a6.htm?s_cid=mm6303a6_e.
- Energypedia. Nepal energy situation 2020. [cited 2021 April 29]. Available from: https://energypedia.info/wiki/Nepal_Energy_Situation.
- Paudel D, Jeuland M, Lohani SP. Cooking-energy transition in Nepal: trend review. Clean Energy. 2021;5(1):1–9.
- Aryal M. Clean cookstoves could change the lives of millions in Nepal. Inter Press Service News Agency; 2015. [cited 2021 April 29]. Available from: http://www.ipsnews.net/2015/04/clean-cookstoves-could-change-the-lives-of-millions-in-nepal/.
- Parajuli I, Lee H, Shrestha KR. Indoor air quality and ventilation assessment of rural mountainous households of Nepal. Int J Sustainable Built Environ. 2016;5(2):301–311.
- World Health Organization. WHO global air quality guidelines: particulat matter (PM2.5 and PM10), ozone, nitrogen dioxide, sulfur dioxide and carbon monoxide: executive summary. 2021. [cited 2021 October 30]. Available from: https://apps.who.int/iris/handle/10665/345334.
- Jayachandran N. Eight Indians die in Nepal of suspected carbon monoxide poisoning: precautions you can take 2020. [cited 2021 April 29]. Available from: https://www.thenewsminute.com/article/8-indians-die-nepal-suspected-carbon-monoxide-poisoning-precautions-you-can-take-116567.
- The Kathmandu Post. Couple, infant found dead in bed 2015. [cited 2021 May 1]. Available from: https://kathmandupost.com/miscellaneous/2015/02/23/couple-infant-found-dead-in-bed.
- AccuWeather. Patan, Bagmati, Nepal Monthly Weather 2021. [cited 2020 August 19]. Available from: www.accuweather.com/en/np/patan/241811/September-weather/241811?year=2019.
- Climates to Travel: World Climate Guide. Climate - Nepal 2021. [cited 2021 November 2]. Available from: https://www.climatestotravel.com/climate/nepal.
- IQAir. Air Quality in Kathmandu 2021. [cited 2021 November 2]. Available from: https://www.iqair.com/nepal/central-region/kathmandu.
- O’Reilly M. Performance of the rad-57 pulse co-oximeter compared with standard laboratory carboxyhemoglobin measurement. Ann Emerg Med. 2010;56(4):442–444. author reply 444–5.
- Hampson NB, Piantadosi CA, Thom SR, et al. Practice recommendations in the diagnosis, management, and prevention of carbon monoxide poisoning. Am J Respir Crit Care Med. 2012;186(11):1095–1101.
- Olson K, Smollin C. Carbon monoxide poisoning (acute). BMJ Clin Evid. 2008;2008:2103.
- Guzman JA. Carbon monoxide poisoning. Crit Care Clin. 2012;28(4):537–548.
- Salameh S, Amitai Y, Antopolsky M, et al. Carbon monoxide poisoning in Jerusalem: epidemiology and risk factors. Clin Toxicol (Phila)). 2009;47(2):137–141.
- Keles A, Demircan A, Kurtoglu G. Carbon monoxide poisoning: how many patients do we miss? Eur J Emerg Med. 2008;15(3):154–157.
- Ghimire S, Mishra SR, Sharma A, et al. Geographic and socio-economic variation in markers of indoor air pollution in Nepal: evidence from nationally-representative data. BMC Public Health. 2019;19(1):195.
- Suner S, Partridge R, Sucov A, et al. Non-invasive pulse CO-oximetry screening in the emergency department identifies occult carbon monoxide toxicity. J Emerg Med. 2008 May;34(4):441–450.
- World Health Organization. Indoor air quality guidelines: household fuel combustion. 2014. Available from: https://www.who.int/publications/i/item/9789241548878.
- Bista B, Manandhar D, Mishra R, et al. Carbon monoxide poisoning due to gas water heater. Janaki Med Coll J Med Sci. 2018;5(2):56–59.
- Himalayan News Service. Couple dies of suffocation in sauna 2020. [cited 2021 November 2]. Available from: https://thehimalayantimes.com/kathmandu/couple-dies-of-suffocation-in-sauna.
- Correia P, Agrawal C, Ranjan R. Gas geyser syndrome: an important preventable cause of disabling neurological events. Ann Indian Acad Neurol. 2013;16(2):245–248.
- Feiner JR, Rollins MD, Sall JW, et al. Accuracy of carboxyhemoglobin detection by pulse CO-oximetry during hypoxemia. Anesth Analg. 2013;117(4):847–858.
- US Food and Drug Administration. Pulse oximeter accuracy and limitations: FDA safety communication 2021 [cited 2021 May 1]. Available from: https://www.fda.gov/medical-devices/safety-communications/pulse-oximeter-accuracy-and-limitations-fda-safety-communication.
- Weaver LK, Churchill SK, Deru K, et al. False positive rate of carbon monoxide saturation by pulse oximetry of emergency department patients. Respir Care. 2013;58(2):232–240.
- Zaouter C, Zavorsky GS. The measurement of carboxyhemoglobin and methemoglobin using a non-invasive pulse CO-oximeter. Respir Physiol Neurobiol. 2012;182(2–3):88–92.
- Touger M, Birnbaum A, Wang J, et al. Performance of the RAD-57 pulse CO-oximeter compared with standard laboratory carboxyhemoglobin measurement. Ann Emerg Med. 2010;56(4):382–388.
- Roth D, Herkner H, Schreiber W, et al. Accuracy of noninvasive multiwave pulse oximetry compared with carboxyhemoglobin from blood gas analysis in unselected emergency department patients. Ann Emerg Med. 2011;58(1):74–79.