ABSTRACT
Misophonia is still an unclassified disorder and means literally “strong dislike (hate) of sounds”. In this paper, we present a case report of an adolescent female who had misophonia that was complicated with two non-fatal suicide attempts. She presented with anxiety features and started to follow up for three years. Assessment of the level of misophonia for a year using Amsterdam Misophonia Scale (A-MISO-S) showed an extreme degree soon after the second suicide attempt. Initially, psychotherapy was noticed to be ineffective due to her poor motivation. Escitalopram was added to the management plan and improvement was reported in the depressive symptoms and obsessional thoughts of misophonia but were intolerable eventually because of the weight gain. Therefore, it was switched into Fluoxetine and Bupropion but six weeks later she attempted her second suicide by Bupropion overdose. At that point, the psychiatrist, the patient and her parents agreed to continue therapy with non-psychopharmacological treatment. Gradually she became more engaged in psychotherapy sessions after noticing its effectiveness. It was concluded that significant improvement of misophonia was reported when she was treated by Selective Serotonin Reuptake Inhibitors (SSRI) namely Escitalopram or Fluoxetine, motivated in psychotherapy sessions, adapted good coping strategies, decreased her dysfunctional challenging behaviour, rejoined social interaction and activity in her life, was more insightful and aware about her illness and developed self-acceptance.
Introduction
Misophonia is a Greek word and it means “strong dislike (hate) of sounds”. The term was coined by Margaret Jastreboff and Pawel Jastreboff in 2001 [Citation1]. The source of these sounds could originate from human or non-human subjects and cause severe emotional distress to the individual [Citation2,Citation3]. This condition was first identified in the 1990s by Audiologist Marsha Johnson and named it the Selective Sound Sensitivity Syndrome or shortly refer to by (4S) [Citation4]. What makes misophonia of an interest in behavioural science to psychologist and psychiatrist is the aversive behavioural reactions from the disturbing sounds. The aetiology of this condition is still unknown and limited data available in the literature. Misophonia is still not listed in the International Classification of Diseases and Related Health Problems (ICD-10) nor the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). Schröder et al. proposed criteria for misophonia. These criteria have six points to diagnose misophonia. They argued that misophonia should be considered as a psychiatric disorder. A tool was developed and adapted from Yale Brown Obsessional Scale (YBOS) and named it the Amsterdam Misophonia Scale (A-MISO-S) [Citation2].
What makes these aversive behavioural reactions clinically significant is that it may affect the functioning. It can cause strained relationships with housemates and family members, causing social isolation & avoidance to inter-social relationship, urges confronting others and asking them to stop producing sounds, decrease in ability to concentrate at school or in the workplace, an inability to meet new friends and to maintain an ongoing relation or limit social activities such as eating meals with others [Citation3,Citation5]. Misophonia was reported to be related with obsessive compulsive, anxiety and depressive symptoms. It been also noticed that misophonia symptoms and rage behaviours are strongly correlated with anxiety [Citation6]. Misophonia has been associated with many comorbidities such as Mood Disorder, Panic disorder, Attention Deficit Hyperactivity Disorder (ADHD), Tourette Syndrome, Hypochondria, Obsessive Compulsive Disorder (OCD), Obsessive Compulsive Personality Disorder (OCPD), Trichotillomania (TTM), Skin pickling. It also been reported that patients with misophonia may have features of Intermittent explosive disorder with impulsive aggressions and rarely to lose control [Citation2]. There been reported cases of misophonia with Eating Disorders such as Anorexia Nervosa or Bulimia Nervosa [Citation7].
In this paper, we present a case report of an adolescent female who had Misophonia that was complicated with two non-fatal suicide attempts. It is important to notice that it is extremely rare to find an individual with misophonia presenting with a suicidal tendency [Citation3]. It is important to increase the awareness among colleagues on this condition as well as support researchers investigating it. With the limited research available in the literature, we were fortunate to assess and manage this case that eventually improved significantly.
Case presentation
The patient and her father consented to present the case thoroughly within the scientific community with respect of the anonymity.
The patient is 18 years old female, single student, living with her parents in the kingdom of Bahrain and has five sisters, born in Manama and vaginally delivered without any complications. She was raised in a middle-eastern Muslim family. She enjoys listening to music, reading books and shared a dream to work as a psychologist.
Patient's complaint: At the age of 12, she started to experience distressing feelings from listening to her family eating. The first time she reported expressing her distress and irritations was after listening to her father eating a banana in front of her. Despite the fact that she respects and loves him, she found it distressful and reported her disgusting feelings and ordered him to stop eating. With time, her father noticed that she was isolating herself from the family and brought her for psychiatric assessment. Her first contact with the Anxiety Department was at the age of 15 on (12/2015).
Patient's course of illness: During the early onset of her illness, she was able to sit with her family and can tolerate the irritation of the audible eating sounds produced and disgusting thoughts that were running in her mind especially while chewing foods. Her triggering sounds were specific toward eating habits of certain foods that crunches and produces high pitched sounds such as apple, carrot, nuts and biscuits. She could bear her own eating sounds but not others. She gradually started to withdraw from joining her family during meals/eating times and easily irritated once she saw or heard someone eating. She tried to cope with it through avoiding these discomforting situations before they happen and to stay alone in her room or at school. Sometimes she felt obliged to put her fingers inside her ears or close her eyes whenever she observed someone eating. She became more preoccupied with these distressful thoughts and intrusive imaginations with time. She reported hitting her colleagues in the class occasionally out of anger after she listened to them eating. She could not tolerate listening to anyone eating “It's disgusting to listen to them eating”. These symptoms limited her social activity with her family, friends and the school, despite her excellent academic performance. The patient went through two non-structured psychiatry assessments on (12/2015) before being finally diagnosed with misophonia. Psychiatric Assessment using The Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I) further reported no disorders for her symptoms [Citation8]. Initially, psychoeducation about the condition and management was instructed to the patient and her father. Psychotherapy showed ineffective outcomes due to her poor motivation and her preference for medication. She believed that medication was more effective than other forms of therapy. Her parents refused psychopharmacology. She joined four psychotherapy sessions during one month only. After stopping following up for a year, she revisited the clinic on (12/2016) reported that her condition deteriorated markedly. She was experiencing at that time anticipatory anxiety about people eating habits, became more isolated than before, her social interactions were limited with her family and was poorly adherent to her management plan. After another seven months of stopping attending, she presented on (6/2017) with four months untreated depressive episode and suicidal thoughts of two weeks. She was bothered more during the holy month of Ramadan “I can't stand the sound fasting Muslims make with their dry mouth”. Her academic performance markedly dropped. She attended two psychotherapy sessions during one month only. It was reported that she took extra pills of over the counter drugs as an act of “suicide” on (7/2017). She was later treated at a local hospital. Escitalopram started then reached 20 mg/day and continued for six weeks. Augmentation with Mirtazapine 15 mg/day was added for only one week and later discontinued because of the increase in her weight(from 51KG to 54KG). Significant improvement reported while on Escitalopram for three months. She rejoined her usual social activities and became more tolerant toward the triggering sounds. Her weight continued increasing while on Escitalopram alone (from 54KG to 59KG). She developed Atypical Bulimia Nervosa that was characterized by several attempts to self-induce vomiting that was specific and limited during the treatment duration. It lasted for three months only and was flared up by her obsessional concerns about her weight gains. She had eight unstructured psychotherapy sessions. Despite, the recovering signs Escitalopram 20 mg/day was discontinued because she felt over-weighted and an alternative Selective Serotonin Reuptake Inhibitors (SSRI) Fluoxetine 20 mg/day was prescribed on (10/2017). During the subsequent visits, the patient was still expressing depressive and misophonia symptoms. She also lacked in motivation in daily activities. Fluoxetine increased to 40 mg/day and later augmented with Bupropion 150 mg/day to improve her motivation. It was reported at that time that she was under severe stress from multiple quarrels with her parent about her adolescent lifestyle. She tried to end her life by taking around 30 tablets of Bupropion on (12/2017). While she was admitted and managed medically, she persuaded her father to sign a discharge against medical advice (DAMA). Assessment of her misophonia symptoms utilizing (A-MISO) was initiated soon after her second suicide attempt on (12/2017) and was followed up for a year until (12/2018) as illustrated in ( and ) [Citation2]. She reported a sense of relief after her second suicide attempt.
Table 1. Amsterdam Misophonia Scale (A-MISO-S).
Afterward, she found no alternative solution for her mental illness other than facing her fears. During one year she was actively engaging in twenty psychotherapy sessions. She was attending the sessions regularly and noticed to do her homework correctly. She became more insightful of her mental illness journey and still today continues to follow up with the Anxiety Department. Minnesota Multi-phasic Personality Inventory (MMPI) conducted on (12/2018) reported no personality disorders.
Patient's physical examination and laboratory investigations: She had no clinical abnormalities and her Body Mass Index(BMI) was 19.5.
Patient's medical history: She has sickle cell trait and treated for chronic urticaria. She was operated for a para-umbilical hernia during infancy and correction for squint (Ectropion) during early childhood. The patient reported that she never abused any substance.
Patient's Family History: Her father and several relatives were treated for Obsessive Compulsive Disorder. No family member reported to have misophonia.
Patient's mental state examination of her last visit on (12/2018): The patient was an average build adolescent that was putting on clean clothes with a scarf on her head. She was sitting comfortable on the chair and was talking with a good eye to eye contact. She was smiling and interacting with the examiner. Her speech was relevant, coherent and was average in tone, volume and tempo. She expressed Euthymic mood with reactive affect. Her thought form was directly goal with no thought disorders elicited. There were no psychotic symptoms. Her risk of suicide or homicide was low. There were no ideas or plans reported. She did not show any cognitive impairment. She was attentive and fully oriented to time, place and person. She was insightful about her illness and needs for treatment.
Psychometric assessment
A-MISO-S:
Its the only known Scale that assess severity of misophonia. There is still no study on the validity or reliability of this scale. It was developed and adapted from Y-BOCS. This scale has six items.
The severity is categorized into 5 degrees, and it is based on a total score (range 0-24), 0–4 subclinical, 5–9 mild, 10–14 moderate, 15–19 severe, 20–24 extreme [Citation2].
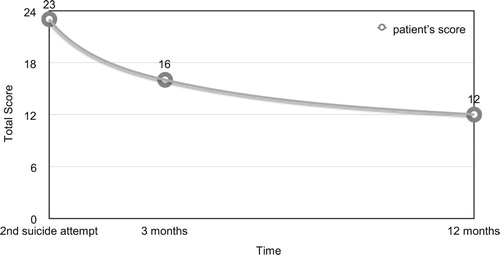
Assessment of her misophonia symptoms utilizing (A-MISO) was initiated soon after her second suicide attempt on (12/2017), three months afterward on (3/2018) and was followed up for a year until (12/2018), as illustrated in ( and ). The patient was able to comprehend the English version, and no translation to Arabic language was needed.
SCID-I:
Patient's assessment was conducted at the initial presentation on (12/2015) and did not reveal any Mental disorders.
MMPI:
Patient's assessment was conducted on (12/2018) and reported no personality disorders. It also reported that the patient most probably is suffering from long-standing problems which she is currently adjusting well to them to the extent that she feels good about herself while still admitting to some bad feelings. There are, however, some evidence of hypersensitivity and withdrawal tendency.
Discussion
To our best of knowledge, this is the first documented case of misophonia that attempted suicide, which reflects that individuals with extreme form of misophonia have the potential to end their lives. We rarely see cases of misophonia in our psychiatric service. This does not mean that misophonia is rare but could reflect the lack of awareness in the public that this condition may need a psychiatric help. Limited studies on the prevalence of misophonia showed that it can reach up to 20% among undergraduate students [Citation6]. Another explanation could be that there are barriers or stigma toward seeking mental health treatment and fear to be called “crazy” [Citation9]. It was reported by Marsha Johnson that parents who have a child with misophonia might be seen by another healthcare provider such as primary care doctors, alternative providers of therapies (i.e. hypnosis, neurofeedback, etc.), audiologists, alternative medical providers (i.e. naturopath, chiropractor, etc.), and otologists or even non-healthcare providers (i.e. Teachers) for help [Citation10]. There are different views on where shall misophonia be listed and if it is a symptom or psychiatric disorder [Citation11]. This could be by itself an important barrier in the scientific community and among clinicians.
The proposed criteria helped us diagnose this case and the severity [Citation2]. Our case fulfilled the criteria. She followed in the clinic for three years irregularly. We managed to monitor her misophonia for a year using (A-MISO-S) soon after the second suicide attempt, 3 months post-suicide and 12 months post-suicide. Initially, the patient reported extreme degree of misophonia ( and ). A lot of the features in our case matches results of previous study. These include that the commonest triggering sounds were of eating/chewing/crunching, stimulated by certain individuals but not self, worsening over time until her second suicide attempt, similar automatic thoughts upon exposing to triggering sounds, anxiety features with emotional and behaviour reactions, certain coping strategies that act as safety behaviours and dysfunction at social, educational and personal levels [Citation3]. It been also reported that individuals with misophonia could engage involuntarily in violence physical behaviour as a response to triggering sounds of smacking mouth while eating. This behaviour could reflect the lack of coping capacity that is distressful to the patient, leaving social gatherings and regretful thoughts [Citation12].
The management of misophonia in our patient was challenging. She thought initially that the only effective therapy for the condition was medication. When she started to follow up, misophonia had already influenced her behaviour. She presented to us with anxiety, obsessional thinking, irritability, and avoidance which are correlated [Citation6]. In two studies misophonia severity was reported to be strongly associated with the level of impairment, and anxiety was validated as a mediator for anger outbursts [Citation6,Citation13]. Interestingly, a recent study in Singapore on psychiatric patients with misophonia found that anxiety level could predict the severity of misophonia [Citation14]. This could explain why she was referred to the Anxiety Department. Its thus of importance that clinicians and specifically Anxiety Disorder Specialists be aware of this condition [Citation15]. The patient did complain of the increase in her weight, after being on Escitalopram and Mirtazapine, that caused her additional anxiety that affected her general adolescent feminine image. She was coping with it through adapting self-induced vomiting behaviour and presented with Atypical Bulimia Nervosa. Her interest in psychology and searching to find a solution on the Web during the onset of her illness made her condition worse and delayed her adherence to our management plan. The avoidance was a consequence of misophonia and a start of Depression which exacerbates her suffering and provoked tendencies toward Suicide over time. A recent preliminary study reported an association between Depression and Suicidality with misophonia [Citation16]. Assessment of the aetiology of her suicide attempts showed that it is mutifactorial. The main starting stress was the misophonia as it created a burden on the patient. It affected her functioning significantly in several aspects. She was mostly isolated at home and at school. The patient was highly social and really suffered from this isolation. She became depressed and irritable which is not her usual as she was known to be a calm person before misophonia and after therapy. This irritability pushed her into several quarrels and conflicts. Her school performance deteriorated and her motivation in studying was clearly affected. The increase in weight was another stressful event for a young slim adolescent. The Fluoxetine may increased her impulsivity. We believe that her second suicide attempt, that could be flared by Fluoxetine paradoxical side effect, acted as an emotion-regulation behaviour for her misophonia [Citation17]. Studies showed that self-injurious behaviour can be followed by “feeling relieved” and a significant decrease in “feeling angry at my self”, “feeling anxious” and “feeling angry of others” [Citation18]. The psychiatrist, the patient and her parents agreed to continue therapy with nonpsychopharmacological treatment for several reasons. The first reason is that medications did not cure her mental illness and suffering. The second reason is that she misused the medications in two previous overdose suicide attempts. The third reason is the lack of a strong evidence in the literature for psychopharmacology in treating misophonia. The severity of misophonia symptoms reduced (from extreme to severe) with a reduction of 30.4% by engaging in psychotherapy sessions, adapting a new positive approach in coping with her condition namely the use of Earplugs, Headsets and Music, focusing her conscious toward her own sounds, self-distraction and positive internal dialogue [Citation3]. In one of the studies CBT reported to improve 48% of patients with misophonia [Citation19]. When she decreased her dysfunctional challenging behaviour, rejoined social interaction and activity in her life, worked more on her good coping strategies, was more insightful and aware about her illness and developed self-acceptance, the severity of misophonia reduced (from severe to moderate) with additional of 17.4% reduction. We report a total of 47.8% reduction of misophonia severity during one-year adherence to the management plan. In total the patient received twenty psychotherapy sessions. Jastreboff reported a success rate of 83% and listed four specific protocols for treatment. Interestingly we believe that our patient had implemented some of these techniques by her own [Citation20].
The role of biological interventions in treating misophonia, e.g. antidepressant especially (SSRI) is still unknown. No study yet conducted to investigate the effectiveness of psychotropics on such patients. In our case, we observed an improvement in her condition while on Escitalopram or Fluoxetine. We could not identify if that was a direct effect or indirect through treating her comorbid depression and anxiety. We are still at the beginning to understand this phenomenon, and more research is recommended. In the literature, there is a suggested plan by Cavanna and Seri for researching misophonia that we support. They think misophonia should be further investigated in all aspects Epidemiology, Phenomenology, Genetics, Pathophysiology and Treatment [Citation11].
It is clear from our patient and the literature that misophonia can significantly affect life and in our case it was complicated with Suicidality. misophonia is still an unclassified disorder and should be considered within the updated editions of ICD-10 and DSM-5. We argue that misophonia has variable presentations with wide range of severity. At one point being harmless and on the other reaching an extreme level of distress that risks one's own life.
Acknowledgements
The authors have declared that there are no existed current or recent funding that might influence the publication of this case report. The authors thank the patient and her father for their consent and input to publish the case.
Disclosure statement
No potential conflict of interest was reported by the authors.
ORCID
Jehad Alekri http://orcid.org/0000-0002-8995-0226
Feras Al Saif http://orcid.org/0000-0002-5842-5947
References
- Jastreboff MM, Jastreboff PJ. Components of decreased sound tolerance: hyperacusis, misophonia, phonophobia. ITHS News Lett. 2001;2:5–7.
- Schröder A, Vulink N, Denys D, et al. Misophonia: diagnostic criteria for a new psychiatric disorder. PLoS One. 2013;8:e54706. doi:10.1371/journal.pone.0054706.
- Edelstein M, Brang D, Rouw R, et al. Misophonia: physiological investigations and case descriptions. Front Hum Neurosci. 2013;25:3–11. doi:10.3389/fnhum.2013.00296.
- Bernstein RE, Angell KL, Dehle CM. A brief course of cognitive behavioural therapy for the treatment of misophonia: a case example. Cognit Behav Therapist. Cambridge University Press. 2013;6:e10. doi:10.1017/S1754470X13000172.
- Taylor S. Misophonia: a new mental disorder? Med Hypotheses. 2017;103:109–117. doi:10.1016/j.mehy.2017.05.003.
- Wu MS, Lewin AB, Murphy TK, et al. Misophonia: incidence, phenomenology, and clinical correlates in an undergraduate student sample. J Clin Psychol. 2014;70:994–1007. doi:10.1002 /jclp.22098 doi: 10.1002/jclp.22098
- Kluckow H, Telfer J, Abraham S. Should we screen for misophonia in patients with eating disorders? A report of three cases. Int J Eat Disord. 2014;47:558–561. doi:10.1002/eat.22245.
- First MB, Spitzer RL, Gibbon M, et al. Structured clinical interview for DSM-IV-TR Axis I disorders, research version, patient edition. (SCID-I/P). New York (NY): Biometrics Research: New York State Psychiatric Institute; November 2002.
- Kumar S, Hancock O, Cope T, et al. Misophonia: a disorder of emotion processing of sounds. J Neurol Neurosurg Psychiatry. 2014;85:e3. doi:10.1136 / jnnp-2014-308883.38.
- Misophonia JM. (April 4 2013). Considerations for providing misophonia care in your practice. Paper presented at The National Meeting of the American Academy of Audiology. Anaheim C A.
- Cavanna AE, Seri S. Misophonia: current perspectives. Neuropsychiatr Dis Treat. 2015;18:2117–2123. doi:10.2147/NDT.S81438.
- Tunç S, Serdar Başbuğ H. An extreme physical reaction in misophonia: stop smacking your mouth!. Psychiatry Clin Psychopharmacol. 2017;27(4):416–418. doi:10.1080/24750573.2017.1354656.
- Zhou X, Wu MS, Storch EA. Misophonia symptoms among Chinese university students: Incidence, associated impairment, and clinical correlates. J Obsessive Compuls Relat Discord. 2017;14:7–12. doi:10.1016/j.jocrd.2017.05.001.
- Quek TC, Ho C, Choo CC, et al. Misophonia in Singaporean psychiatric patients: a cross-sectional study. Int J Environ Res Public Health. 2018;15:1410. doi:10.3390/ijerph15071410.
- Hadjipavlou G, Baer S, Lau A, et al. Selective sound intolerance and emotional distress: what every clinician should hear. Psychosom Med. 2008 Jul;70(6):739–740. doi:10.1097/PSY.0b013e318180edc 2 doi: 10.1097/PSY.0b013e318180edc2
- Erfanian M, Jo Brout J, Keshavarz A. Misophonia, emotional dysregulation and affective disorders: a preliminary study. Eur. Neuropsychopharmacol. 2018;28(6):771–772. doi:10.1016/j.euroneuro.2017.10.014.
- Hammad TA, Laughren T, Racoosin J. Suicidality in pediatric patients treated with antidepressant drugs. Arch Gen Psychiatry. 2006;63(3):332–339. doi:10.1001/archpsyc.63.3.332.
- Smithuis L, Kool-Goudzwaard N, de Man-van Ginkel JM, et al. Self-injurious behaviour in patients with anorexia nervosa: a quantitative study. J Eat Disord. 2018;6:26. doi:10.1186/s40337-018-0214-2.
- Schröder AE, Vulink NC, van Loon AJ, et al. Cognitive behavioral therapy is effective in misophonia: an open trial. J Affect Disord. 2017;217:289–294. doi:10.1016/j.jad.2017.04.017.
- Jastreboff PJ, Jastreboff MM. Treatments for decreased sound tolerance (hyperacusis and misophonia). Semin Hear. 2014;35(02):105–120. doi:10.1055/s-0034-1372527.