Abstract
Following recent health crises—mad cow, SARS, H1N1—, countries and subnational entities refined their policy infrastructure to better respond to outbreaks, leading to pandemic emergency plans. These plans, which are the result of complex public policy-making processes, were translated into public policies during the COVID-19 pandemic, leading to important policy issues and changes. Were these plans applied as planned? How did they evolve, as a policy object, during the pandemic? How do they compare among national/subnational entities? This paper proposes a comparative analysis of the existing plans, their temporal mobilization during the first 3 weeks of the pandemic, the policies they led to, and their successive revisions within a short period of time. Our analysis problematizes the translation process between policy and practice, bringing new light to the policy-making process under emergency and crisis. Informed by policy learning research and using a qualitative content analysis of existing COVID-19 pandemic plans in the three largest and most affected Canadian provinces (Québec, Ontario, and British Columbia), this article provides not only a better understanding of real-time policy making but also crisis-induced policy learning at the organizational level.
Introduction
Pandemics, including the 2009 H1N1 influenza virus, the 2003 SARS-CoV-1 virus, and more recently COVID-19 (caused by the SARS-CoV-2 virus), have consistently demonstrated their ability to wreak havoc on the operational capacities of healthcare systems (Madhav et al. Citation2017), and have proven to be a substantive threat to global public health (Stein and Sridhar Citation2017).
Yet their unpredictable nature (Gellin and Qadri Citation2016) makes it very difficult for policymakers to adequately plan and prepare for what most consider to be the inevitable occurrence of future pandemics (Fan, Jamison, and Summers Citation2018). Nonetheless, countries strive to attain a level of ‘pandemic preparedness’ (Fineberg Citation2014), typically through the development of formalized response plans outlining the preventative and mitigation measures to be taken should a pandemic occur.
While an extensive amount of research exists on pandemic preparedness planning (Fineberg Citation2014; Jennings et al. Citation2008; Oshitani, Kamigaki, and Suzuki Citation2008; World Health Organization Citation2009), very little research has been done on the adherence of said plans - the extent to which government’s actions throughout a pandemic correspond to the steps outlined in their respective pandemic preparedness plan and how it is effectively translated into public policies. Moreover, in a federal setting like Canada, pandemics expose how intertwined our political and administrative systems are and how codependent we are nationally, globally and locally.
This paper has two objectives: (1) compare the existing emergency and pandemic preparedness plans from various levels of government in the Canadian provinces of Québec, Ontario and British Columbia; (2) analyze the translation of these plans into public policies, underlining how COVID-19 became a public policy problem.
To do so, existing emergency management strategies and preparedness plans developed prior to COVID-19 are analyzed, paying particular attention to the responses from the federal, provincial and municipal governments. Pandemic preparedness is an extremely complex phenomenon (World Health Organization Citation2009, Citation2018), and governments are required to operate in a dynamic environment with a multitude of actors involved. Three elements are key and were researched in our qualitative analysis (more of the methodology below): (1) the concept of pandemic preparedness, (2) the impacts of multi-level governance and (3) policy coherence among and between decisions and policies.
Pandemic preparedness
Following the occurrence of multiple pandemics in the span of a few decades, pandemic preparedness and planning has increasingly become a priority for public health authorities across the globe (Hanvoravongchai et al. Citation2010), Canada included (Henry and Gadient Citation2017). According to Nelson et al. (Citation2007), public health emergency preparedness can be defined as “the capability of the public health and healthcare systems, communities, and individuals, to prevent, protect against, quickly respond to, and recover from health emergencies, particularly those whose scale timing, or unpredictability threatens to overwhelm routine capabilities” (9). That said, the concept of pandemic preparedness is difficult to precisely evaluate and quantify. Also, while the number of evaluation approaches demonstrates a willingness on the part of policymakers to improve their countries’ pandemic planning, it also highlights the lack of a “robust validated approach” to policy making and planning (Krumkamp et al. Citation2010, 92). The defining characteristic of Canada’s response to the COVID-19 pandemic was the existence of a coherent set of existing preparedness plans, which, by and large, followed the guidelines set by the World Health Organization (Citation2009). However, these plans were developed not only at the federal level, but also at the provincial level, as well as by municipal and regional health authorities where concrete policies were developed and enacted during the pandemic. In addition to diverging greatly between provinces and territories, the severity of the COVID-19 pandemic also varied drastically, impacting as such the deployment of pandemic preparedness plans.
Multi-level governance
Conceived in the context of European integration, the notion of multi-level governance has been rapidly gaining momentum in global policy circles (Betsill and Bulkeley Citation2006), and its appeal has extended far beyond its origins within the European Union, including environmental (Homsy and Warner Citation2015) or health governance (Studlar and Cairney Citation2019). Multi-level governance usually refers to a “system of governance where there is a dispersion of authority upwards, downwards, and sideways between levels of government – local, regional, national and supra-national – as well as across spheres and sectors, including states, markets and civil society” (Daniell and Kay Citation2017, 4). Its meaning is not, however, homogeneous. Hooghe and Marks (Citation2001) identify and define two distinct forms of multi-level governance – Type I and Type II. Similar to federalist thought, Type I multi-level government consists of a dispersion of authority restricted to a “limited number of non-overlapping jurisdictions at a limited number of levels” (Hooghe and Marks Citation2001, 4). Conversely, Type II views multi-level governance as being a “complex, fluid patchwork of innumerable, overlapping jurisdictions” (Hooghe and Marks Citation2001, 4). In this article, we pay particular attention to Type I, as we analyze the complex role of intergovernmental decision-making in Canada’s federal system. While multi-level governance certainly has its advantages, it can also be problematic, as jurisdictional boundaries of authority tend to overlap, creating confusion among decision-makers and resulting in different type of policies enacted, a phenomenon noticed in our analysis (see below). This risk is particularly salient in the context of pandemics, which transcend not only physical borders, but also across multiple jurisdictional areas of competency (Heymann et al. Citation2015).
Policy coherence
Given Canada’s federalist governmental structure and the diverse set of actors involved in the policy-making process, the need for coordination and policy coherence when dealing with health and pandemic issues has become increasingly evident (Inwood, O’Reilly and Johns, Citation2011). Defining the term policy coherence is no simple task, given the ample number of varying definitions that have been proposed. For instance, Challis et al. (Citation1988) broadly define policy coordination as being the “pursuit of coherence, consistency, comprehensiveness and of harmonious compatible outcomes” (25). According to Nilsson, public policy coherence should be viewed as “an attribute of policy that systemically recuses conflicts and promotes synergies between and within different policy areas to achieve outcomes associated with jointly agreed policy objectives” (Nilsson et al. Citation2012, 396). In this perspective, policy coherence can be understood as the degree of synergy between different policy areas, with the goal of attaining common outcomes (in our case, responding to a pandemic that does not respect jurisdictional borders). Alternatively, Savard (Citation2010) proposes that policy coherence be defined as “the integration of ideas from different actors, which generate a synergy between elements of public policies associated with the same domain and thus providing a common understanding of the expected effects of these policies” (cited in Savard, Villeneuve, and Caron Citation2013, 152). Policy coherence is understood here as the level of integration between the ideas of different parties, and their respective public policies, thus instilling a common understanding of the expected outcomes. The concepts of coordination and harmonization are key here. Policy coherence can thus be seen as a mechanism for enhanced collaboration and coordination between levels of government within the same policy area. Likewise, in the context of pandemics, Quigley argues the need for partnerships when it comes to policy making (Citation2013, 149). Moreover, Katz et al. (Citation2018) suggest that, in order to improve pandemic preparedness, partnerships need to extend beyond the public and para-public sector, thus including the private sector. As Savard, Villeneuve, and Caron (Citation2013) notes, the concept of policy coherence is typically discussed in relation to two axes—vertical and horizontal—the former referring to the degree of coherence between entity of different levels (for instance between the central government and the cantons) and with the latter referring to policy coherence within the same level of government (151). Both axes are used in our analysis.
Methodology
As a major and complex issue, COVID-19 response involves a multiplicity of actors at all levels of governments. For the purpose of this paper, our analysis is limited to the federal government, three provincial governments (Québec, Ontario and British Columbia) as well as three municipalities within these provinces (Montréal, Toronto and Vancouver). These three provinces are representative of Canada’s responses to COVID-19, as they account for 75% of the Canadian population, are representative of the ideological, cultural and political diversity of Canada. They also have different strategies regarding their preparedness as well as different relationship with the federal government, in addition to completely different experience of the severity of the COVID-19 pandemic. below shows the COVID-19 data by province, as of August 27 2020.
Table 1. COVID-19 dataFootnote1.
Our research design is based on a qualitative case-study analysis of existing government pandemic preparedness plans and related documentation (document analysis) that we compared with the government response during the first 3 weeks of the pandemic (analysis of statements, policies and programs).
Regarding the document analysis, seven government pandemic preparedness plans from the Federal government the provinces of Québec, Ontario and British Columbia along with three major cities Montréal, Toronto and Vancouver were analyzed using content analysis. All documents were coded using NVivo12 to document the concepts of pandemic preparedness, multi-level governance arrangements and policy coherence among and between the plans.
Following that, the translation of the different emergency plans into policies, programs and government actions for the three provinces/cities were analyzed from the beginning of the pandemic (March 11 2020) to March 31Footnote2. In order to study the translation phase (from emergency plan to actual governmental responses during the crisis), we gathered all the measures, policies and programs implemented by the actors analyzed through an analysis and classified them by policy area. These measures where identified through an analysis of all the communication, press conferences and announcements by the different stakeholders. The database can be shared on request.
Planning for preparedness
The federal government
Multi-level governance and coordination are at the heart of the Canadian Pandemic Influenza Preparedness Plan adopted in 2018 (Minister of Health, 2018). The influenza plan was the one used in the early stage of the COVID-19 response. Its preface points out that it was reviewed extensively by the federal, provincial, and territorial governments as well as community services and indigenous people. Through the Pan-Canadian Public Health Network, the federal government had consulted with the different levels of government before the publication of the plan, emphasizing on coordination mechanisms under multi-level governance architecture. The plan underlines the importance of how each region of the country will face different issues due the country’s diversity, both culturally and geographically. The plan also underlines that the different governments will coordinate to update the preparedness plan with the input of all levels of government involved.
The plan emphasizes that, while it should be used as recommendations for all levels of government, it is up to the provincial and territorial governments to create their own plans:
Canada is responsible for coordinating the whole of government response when the federal government is involved in the response to an emergency. Within the PTs a similar function is performed by the appropriate ministry or emergency measures organization. In a pandemic situation, a pan-Canadian whole-of-government response is required so that all potential resources can be applied to minimizing the pandemic's negative health, social and economic impacts. Pandemic plans should be aligned across jurisdictions to facilitate successful FPT collaboration during a pandemic. (Government of Canada Citation2018, 22)
From that document, we observe that the federal government responsibility is to facilitate the coordination between different stakeholders during a pandemic and to fill in the gaps between the different levels of government. As such, responsibilities between the different levels of government are divided into different sections: (1) information sharing/recommendations, (2) medication/vaccines, (3) healthcare provisions and federal population. Regarding the first element, the plan states that the federal government is in charge of risk assessment for pandemic and for coordinating the pan-Canadian response. Communication is highly stressed throughout the plan between the different levels of government, targeting “surveillance information; jurisdictional communications, strategies and messaging” (Government of Canada Citation2018, 25). The objective is to favor the transmission/harmonization of information needed to make evidence-based policy-making.
Regarding medication and vaccines, the federal government’s role is to represent the country as a whole at the international level when working with pharmaceutical companies. On the other hand, the responsibilities of the provincial and territorial governments are to “maintain, monitor, distribute and administer the use of antiviral medications and vaccines in their respective jurisdictions.” (Government of Canada Citation2018, 25) The plan states that the governments will work together to “develop strategies to mitigate the effects of insufficient or delayed antiviral drug and/or vaccine supply, should such a situation arise.” (Government of Canada Citation2018, 26)
As for the third section, it is mainly the provincial/territorial governments’ responsibility, which includes, but is not limited to, providing healthcare, medication, supplies, monitoring data of healthcare, and establishing healthcare guidelines. They are also responsible for creating a plan to increase healthcare capacity, in coordination with the federal government. On that level, the federal government is responsible for assuring that healthcare services, medications, supplies and equipment are provided to the provinces.
The federal government plan thus gives a framework regarding the federal, provincial, and territorial governments’ responsibilities should a pandemic arise. The plan also shows that coordination and cooperation appear to be key when dealing with a pandemic from the federal point of view. The plan nonetheless shows how there are some overlaps in jurisdictions and responsibilities.
Québec-Montréal
Québec’s Pandemic Plan clearly identifies the Ministère de la Santé et des Services sociaux (MSSS—Health and social services ministry) as the governmental organization in charge of virus-related emergencies. The plan was adopted in 2006 and uses influenza as a base plan. As with the federal government’s plan, coordination is also at the heart of the preparedness plan, underlining that Québec-wide initiatives should be prioritized. It also highlighted that an integrated approach must be favored, calling for cooperation with other levels of government (Gouvernement du Québec Citation2006).
Québec plan identifies a series of challenges that the province would face during a pandemic, including: “increased patient traffic, the management of health and social services network personnel in the face of absences due to illness, the coordination of several social partners, the procurement of drugs, supplies and equipment […], and the importance of communications […]” (Gouvernement du Québec Citation2006). It is interesting to note that the first weeks of the pandemic saw all these challenges materialized, underlining the importance of preparedness during crisis. The plan also identifies three principles its responses during a pandemic should follow: (1) a strategy coherent with the overall health network, (2) a top-down approach, and (3) effective organization, focusing on coordination. Compared with the other plans analyzed, the Québec one is, however, the vaguest one, simply enunciating these objectives without clear mechanisms to enforce them. Three elements are also important to note regarding this plan: (1) the emphasis on surveillance, (2) self-care for minor health issues and (3) at home services. As discussed later, these elements posed various problems to the Québec government in the first weeks of the pandemic, and especially their interaction (for example, the problematical interaction between coordination and at home services).
The Québec metropolis, Montréal, has also its own pandemic preparedness plan, developped by the Agence de la santé et des services sociaux de Montréal (Montreal agency of health and social services), thus being a specific actor in this bureaucratic architecture. This plan, adopted in 2007, attempts to be based on both the federal government’s plan and on the provincial one (the MSSS) in order to have a better coordination with each level of government, underlining the complexity of multi-level governance from the point of view of the provinces. During a pandemic, Montréal plans to work with stakeholders in the city, such as the Organization régionale de sécurité civile (ORSC—regional organization for civil security), Services Québec and the Montréal health network (Agence de la santé et des services sociaux de Montréal Citation2007).
The plan also recognizes that the structure of coordination must have a top-down approach, echoing the provincial government and reinforcing the coherence argument. The deployment of this approach is made through different coordination committees created by the province, but in collaboration with several stakeholders to assure that the region has a well-coordinated plan regionally and provincially.
When it comes to vaccines and medications, the Montréal plan states that it will prioritize those who are working to fight the pandemic, meaning essential workers, people with compromised immune systems, the elderly, and children. It is the responsibility of the MSSS to supply the city of Montréal with resources including, but not limited to, vaccines, antiviral drugs, equipment, etc.
The plan also has a communication strategy with the objective to inform the residents of the city about the evolution of the pandemics. The plan also emphasizes communication with the media to share information about mitigation strategies.
As mentioned previously, the Québec provincial plan states the need for coordination and cohesion with the local governments but does not detail how this coordination should be. The Montreal Pandemic Influenza Plan better explains the ideal coordination mechanism between the city and provincial government, underlining the role of regional and local partners. A limitation to the Québec and Montréal Region plans is the lack of a clear responsibility sharing between the different actors involved and how precisely they should work together and/or with the federal government.
Ontario-Toronto
The Ontario Health Plan has a different organization and is mainly based on influenza-related preparedness scenarios. The Ontario Health Plan for an Influenza Pandemic (OHPIP) was adopted in 2013 and developed with the contribution of many different governmental organizations within the province, including various indigenous tribes different health departments and organizations (Government of Ontario Citation2013), something we do not find with the other provinces analyzed. Should a pandemic arise, the Ministry of Health/Ministry of Long-Term Care (MOHLTC) is the provincial governmental organization in charge of pandemic responses. It is also responsible for cooperating with other provinces and the Canadian federal government.
The Ontario provincial plan recognizes the possibility of differences arising between the federal and provincial plan, thus anticipating the difficulties with multi-level governance. The Ontarian plan states that it will try the utmost to align its plan with the federal one, adding that health sector employers and health workers should follow Ontario’s guidelines when delivering healthcare services within the province (Government of Ontario Citation2013). The OHPIP underlines that the recommendations are developed with inputs from Ontario stakeholders. When it comes to influenza pandemic, the MOHLTC highlights and explains the differences between Public Health Agency of Canada’s and the MOHLTC’s recommendations in its communications with the health system, an effort of responsibility explanation that wasn’t seen within the province of Québec.
At the municipal level, the City of Toronto has a municipal health authority called “Toronto Public Health” (TPH) which is responsible for dealing with the pandemic at the local level. The Toronto Pandemic Plan was adopted in 2007 and is based on an older version of the Canadian Pandemic Influenza Plan as well as the OPHIP (City of Toronto Citation2007). It stresses that the TPH is responsible for the different elements delegated to the city and to collaborate and communicate with the MOHLTC. In the introduction of the TPH’s plan, it is stressed the need for flexibility and adjustments.
TPH responsibilities are the following: surveilling & reporting on the local level; case and contact investigation and management; assessing health risks and communicating infection control advice; working with the hospitals and other stakeholders; assessing the capacity of local health services, including health human resources; community-based disease control strategies; vaccine distribution; planning for alternative strategies for influenza assessment, treatment and referral services for vulnerable and underserved populations. The city is also responsible for implementing public health measures decided by the Provincial Chief Medical Officer of Health.
The Toronto Pandemic Plan has a lot more details on the requirements for services than the provincial or federal pandemic plan. The city’s plan has guidelines for services should a pandemic occur. All services need to have a business continuity plan with the following requirements: (1) identify the organization’s mandated and critical services, (2) rank all services in order of priority, and (3) identify the internal and external effects of disruptions.
Since businesses will be affected as well when a pandemic occurs, the city has a list of requirements to follow in the event of a pandemic for them. The city requires for example that businesses prepare for disruptions and develop their own business continuity plan, including: (1) the establishment of a steering committee or lead individuals, (2) a business impact analysis, (3) a business continuity plan, and (4) readiness procedures.
What is striking with the local level plan for the city of Toronto is that, compared to the provincial and federal plans, we can see how the local level is responsible for the entire frontline events and pandemic response mechanisms. It deals with people directly while coordinating with the provincial and federal government. It follows what we could characterize as a more bottom-up approach.
Although the provincial pandemic plan does not go into much detail about coordination or cohesion with the federal or local governments, the Toronto Public Health pandemic plan gives a lot more insight on how the city works with the province during a pandemic. Unlike the Québec plan, and in line with the Vancouver one (below), the Toronto plan is relatively clear when it comes to who is responsible for what during a pandemic.
British Columbia-Vancouver region
The British Columbia’s pandemic plan which was adopted in 2012 seems to favor a different approach, as it clearly argues that all regional health authorities are responsible for having their own Pandemic Influenza Contingency Plan that should include the role of local governments, stressing the importance of delegating responsibilities to the appropriate actor. It underlines the importance of municipal governments working with their regional health authorities to manage and create its own procedures (Government of British Columbia Citation2012).
Interestingly, the British Columbia plan identifies other provincial actors required to have their own pandemic response plan, something not found with other provincial plans. This precise requirement for several BC actors shows the emphasis put on coordinated responses at the provincial level. Coordination is ensured by the Joint Emergency Preparedness Program (JEPP). Launched in the 80 s, JEPP allows the federal government to “contribute to or undertake jointly with the provinces and territories, projects to ensure a relatively uniform level of emergency preparedness and response across Canada.”Footnote3 It allows the province to give the federal government permission to get involved in provincial affairs and help fund the provinces during emergency.
The responsibilities are also well identified, the regions being in charge of (1) providing information relating to the pandemic concerning the number of cases, deaths, hospitalization, etc., (2) providing vaccines/antiviral drugs to the public, and (3) communicating with the public in their region. British Columbia’s Pandemic Plan delegates some of the roles in the federal plan to the regional level and describes in its own plan what the province is responsible for, versus what the regional health authorities are responsible for.
As a consequence, Vancouver adopts a regional approach when it comes to dealing with pandemic preparedness. At this level, it is the Vancouver Coastal Health (VCH) organization that deals with issues related to pandemic. Pandemic declaration comes from the Provincial Health Officer (PHO) within the British Columbia’s ministry of health. The current legislation allows the PHO to enact the provincial pandemic plan for the whole province. It is, however, the responsibility of the local Medical Health Officer to enact stricter measures. According to the VCH pandemic plan, when the PHO declares a pandemic, the VCH’s Chief Medical Health Officer needs to confirm the pandemic and direct the local response (Vancouver Coastal Health Citation2018).
The VCH has a special unit called the Public Health Surveillance Unit (PHSU) within the VCH that does surveillance for influenza. When there is a pandemic, the PHSU also performs surveillance and reports this information to the BC Center for Disease Control (BCCDC) who communicates with the federal government. In the need of enhanced surveillance, it is the responsibility of the Chief Medical Health Officer to give the greenlight for the PHSU to start performing it. The province of British Columbia is responsible for creating infrastructure for all the regional health authorities within the province while the VCH is responsible for the actual monitoring of the regional surveillance as well as giving information to the healthcare facilities within its jurisdiction.
The VCH will get its vaccines directly from the province. It is required to follow the regulations that the province puts out when it comes to the vaccine. The VCH is responsible for following provincial guidelines and distributing the vaccine accordingly. People with high-risk health problems, pregnant women, and children have priority to receive the vaccine.
Should a pandemic arise, it is the Canadian Border Service Agency’s (CBSA) responsibility to determine who can be turned away from the border or placed in a federal quarantine location. The plan recommends that the regional health authorities collaborate with the federal government if the federal government does not have enough resources to screen arrivals as well as to develop and implement policies and procedures for ports of entry.
Interestingly, British Columbia not only collaborates with the federal and local government, but also with international partners, as it has signed a memorandum of understanding with the state of Washington. The two governments have agreed to collaborate with each other in preparing, responding, and recovering from a pandemic. A memorandum of understanding was also signed with the province of Alberta, showing how BC recognized the importance of multi-level governance compared with the provinces of Québec and Ontario.
Based on our analysis, we identified the following structural differences between the preparedness plans of the three provinces and the federal (). Three types of plans emerged: (1) a more top-down and individualistic approach (Québec), a bottom-up and multi-actor approach (Ontario), and (2) a local-based/delegation type approach (British Columbia). These three ached resulted, as we suggest in the next section, in different policy responses.
Table 2. Structural differences between the plans analyzed.
The translation of the preparedness plans into policies
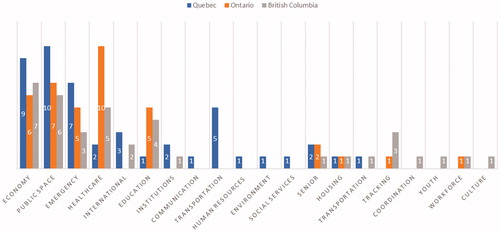
How the plans were translated into policies, programs and governmental responses during the first weeks of the pandemic? This section seeks to analyze the translation process from preparedness plan to policies. The deployment of the emergency plans in Québec, Ontario and British Columbia during this period encompasses 20 policy areas (see Graphs 1 and 2 for the complete list – data available on request). As shown by , the policy responses for each province/city focus on different targeted policy areas, showing the different strategies and framing (see below) during the implementation of the emergency plans. Overall, Québec and British Columbia deployed their actions on a wider variety and diversity of policy areas compared to Ontario (15 versus 10 policy areas covered—a 50% increase), which represents a significant policy concentration for Ontario. The state of emergency was also declared slightly earlier in Québec (4 days earlier), but at the same time for British Columbia and Ontario. In terms a policy framing process during the deployment of the emergency plan, we identified three dominant frames: (1) the economic and infrastructure frame (Québec), (2) the healthcare and social policy one (Ontario) and, (3) the coordination and multi-level focus (British Columbia).
Overall, Québec deployed more measures and policies compared with the two other provinces (47 versus 38 − 23% more). Québec emphasis is placed on four distinct policy areas: public space (the most important one), followed closely by the economy, emergency and transportation. Echoing the importance put on the economy by the Québec government as seen by the fact that it is the second most important policy area targeted, the first measures implemented by this government being an economic one. Compared with the other two provinces, Québec is the one with the most emphasis on public space-related measures (closure of public space and facilities, gathering limitations, physical distancing, etc.). It is also the one with the most emphasis on the international level (none for Ontario, and slightly less than Québec for British Columbia). It also is the only province focusing on transportation.
It is interesting to note that tracking does not appear in the deployment of the emergency plan of Québec/Montréal in the early stage of the pandemic compared with the two other provinces. Similarly, Québec is also the province with the less emphasis put on healthcare in the early stage of the pandemic (only two specific measures). The same thing applies when it comes to education, with only one measure for Québec. What is also striking overall is the fact that Québec, the most affected province, has more measures and policies, for a wider variety of policy areas, but have really few healthcare related measures compared with the two other provinces. Education also appears as a key policy area targeted early on in Ontario and British Columbia compared with Québec.
Ontario follows a slightly different strategy, targeting five key policy areas (one more than Québec), but in a different order, and adding education as a targeted policy area. It also as 38 measures (equal than British Columbia, and way less than Québec). The five policy areas are: healthcare (the most important one, as well as the first put in place), followed by public space, the economy, emergency and education. The key difference is definitely the importance put on healthcare (10 measures, compared with 2 for Québec and 5 for British Columbia). The emphasis on healthcare in the Ontarian deployment can be seen over the entire period of time analyzed ().
British Columbia emphasis is put on four policy spheres: the economy (the most important one), followed by public space, healthcare and education. Interestingly, British Columbia deployed its emergency plan right at the beginning with a measure on coordination, which echoes the emphasis on coordination found in its preparedness plans. It is also the only province with several measures for tracking cases, measures that we find predominantly in the second half of the time frame analyzed (). Noticeable, culture and youth-related measures appear only in British Columbia emergency policies and responses. British Columbia, compared to the two other provinces, thus deployed some measures on several policy areas unexplored by the two other provinces. It is also the only one emphasizing tracking early on in its deployment of its emergency plans.
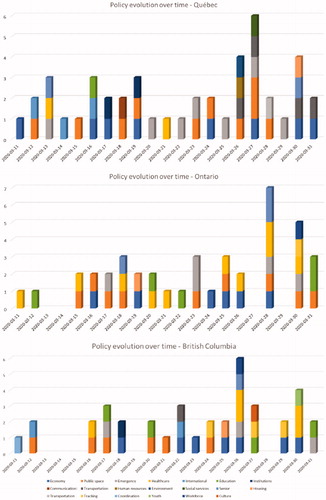
shows the evolution of the different measures, for each province/city, over time. What is interesting to notice is the emphasis put on the first days of the pandemic for the different provinces. Québec definitely emphasized economic and international related measures and also has more measures overall during the first weeks of the crisis, compared with Ontario and British Columbia, which has slightly less measures at the beginning, also targeting different policy areas. Ontario focused on healthcare and public space, and British Columbia mainly on public space during the first week of the pandemic. Public space-related measures arrived late in Québec, compared with the two other provinces where it is found relatively earlier. Compared with Québec, Ontario and British Columbia have on the opposite economic measures coming relatively late in the emergency plan deployment. Ontario also has several healthcare related measures by the second half of the period analyzed.
Recommendations and conclusion
Our analysis underlines several interesting elements. First, it is apparent that there is an attempt of cohesion within multi-level governance structure with the federal plan to clarify its responsibility from those of the provinces. A number of factors also explain why pandemic policy fail. One of them is slow and subpar information between multi-level administrations, which ultimately results in heterogenous outbreak responses (Krumkamp et al. Citation2010).
After the federal government’s pandemic plan, British Columbia and Vancouver’s pandemic plans are the most detailed, explaining how they should coordinate with each other as well as with the federal government. What is interesting about British Columbia and Vancouver plans is that they intend on coordinating with the CBSA should the CBSA lack resources from the federal government. The Ontarian and Québec’s pandemic plans do not deal with ports of entry issues like British Columbia and Vancouver. Also interesting about this plan is that it is in fact a regional plan, not only for the city of Vancouver. Relative to health authorities’ responsibilities, British Columbia is also very clear as to how they need to work within the province, stressing geographically the boundaries and jurisdictions. British Columbian/Vancouver pandemic are good examples of how multi-level governance works during a pandemic, including international actors.
In contrast, Québec and Ontario plans lack explaining how precisely coordination with other levels of government should be implemented during a pandemic, although the municipal plans of both the city of Toronto and Montréal communicate better how they work with the province. The plans still do not explain fully the mutual responsibilities of the local and provincial governments and lack how they would deal with surveillance during a pandemic. This last point is important as (improper) surveillance was a key issue early on during the pandemic (Peeri et al. Citation2020; Klonowska and Bindt Citation2020).
The effectiveness of a government’s pandemic response requires an adequate level of pandemic preparedness for successfully mitigating their impact. As itself, the coherence of pandemic preparedness plans is not a guarantee an effective governmental response. A plethora of political factors influence the success of a government’s pandemic response, as evidenced by the US during COVID-19, which, despite being ranked first out of 195 countries for pandemic preparedness based on the 2019 Global Health Security IndexFootnote4, has done extraordinarily poorly in the face of COVID-19 and is arguably one of the hardest-hit countries worldwide.
Canada, on the other hand, has performed significantly better, despite sharing certain key characteristics with the U.S., namely its federalist governmental structure. It seems that the level of cooperation from multi-level governance is what makes countries more or less effective at weathering the storm of a major pandemic like COVID-19. This would explain why the United States, who’s highly disorganized response, with an apparent lack of coherence between not only the federal and state government’s actions and policies, but also between the various state governments themselves, ultimately was not able to sufficiently contain the virus. In comparison, Canada’s response, barring slight variations between provinces, has been more coordinated and coherent, with the federal, provincial and municipal governments all working together to prevent further spread of the virus and to mitigate its negative economic impacts.
The policy relevance of our finding are numerous. For example, focusing early on healthcare related measure during the deployment of an emergency plan seems to better equip governments to respond to health crisis. Less policy areas targeted and better-focused measures by these plans seem to facilitate coordination and integration, both between policy areas, but also between policy levels and actors. A top-down approach also seems less adequate to respond to public health crisis, as the day-to-day actors involved with patients and at-risk groups are frontlines and localized groups and workers. Anticipating multi-level governance tension and identifying adequate mechanism to counterbalance these tensions also appear to be key. Lastly, clear responsibility and appropriate delegation structure seems to be an active ingredient of governmental responses to public crisis.
The challenge here in terms of public-policy making is the learning process (Schiffino et al. Citation2015) when a crisis become the new normal. How can government and state authorities can learn from crisis and from the evolution of the situation? Multiple factors can affect this learning process. However, a bottom-up, localized strategies for preparedness plan seems more appropriate to learning processes as information and inputs from frontline workers can more easily reach back to government and inform the policy-making process.
Responding to pandemics, through preparedness plans and other measures, is a risky business, as proved by the different examples analyzed here. Evolving in a complex and dynamic environment, governments must adapt their responses rapidly. Our analysis nonetheless shows that focusing on key elements, such as coordination, tracking and communication, and less, but better focused measures, seem to play an important role in the success, or failure, of preparedness plans.
Acknowledgements
The authors are also thankful to Centre on Governance of the University of Ottawa.
Correction Statement
This article was originally published with errors, which have now been corrected in the online version. Please see Correction (http://dx.doi.org/10.1080/25741292.2021.1880808)
Additional information
Funding
Notes
1 Data from the INSPQ (the National Institute of Public Health of Québec – https://www.inspq.qc.ca/), the Government of Ontario COVID-19 database (https://covid-19.ontario.ca/data) and the British Columbia Center for Disease Control (http://www.bccdc.ca/health-info/diseases-conditions/covid-19/data)
2 The choice of March 11 is the date when the WHO declared COVID-19 a Pandemic (WHO 2020). Alternatively, the choice of March 31 is based on the fact that after this date, is it difficult to retrace the original pandemic response because of the scale of the crisis asking for a completely new and different policy architecture. In other words, after the end of March, COVID-19 is the new normal, thus descaling the emerging nature on the policy implemented.
3 https://www.publicsafety.gc.ca/cnt/rsrcs/pblctns/archive-vltn-jnt-mrgnc-2008-09/index-en.aspx, accessed on July 15 2020.
4 See https://www.ghsindex.org/, accessed on August 4 2020.
References
- Betsill, M. M., and H. Bulkeley. 2006. “Cities and the Multilevel Governance of Global Climate Change.” Global Governance: A Review of Multilateralism and International Organizations 12 (2): 141–160. doi:10.1163/19426720-01202004.
- Challis, L., R. Klein, S. Fuller, M. Henwood, W. Plowden, A. Webb, P. Whittingham, and G. Wistow. 1988. Joint Approaches to Social Policy: Rationality and Practice.Cambridge: Cambridge University Press.
- City of Toronto. 2007. Toronto Pandemic Plan. Toronto Public Health. Toronto, Canada.
- Daniell, K. A., and A. Kay. 2017. “Multi-Level Governance: An Introduction.” In Multi-Level Governance: Conceptual Challenges and Case Studies from Australia, Acton, Australia: ANU Press, 3–32.
- Fan, V. Y., D. T. Jamison, and L. H. Summers. 2018. “Pandemic Risk: How Large Are the Expected Losses?” Bulletin of the World Health Organization 96 (2): 129–134. doi:10.2471/BLT.17.199588.
- Fineberg, H. V. 2014. “Pandemic Preparedness and Response-Lessons from the H1N1 Influenza of 2009.” The New England Journal of Medicine 370 (14): 1335–1342. doi:10.1056/NEJMra1208802.
- Gellin, B. G., and F. Qadri. 2016. “Preparing for the Unpredictable: The Continuing Need for Pandemic Influenza Preparedness.” Vaccine 34 (45): 5391–5392. doi:10.1016/j.vaccine.2016.09.023.
- Gouvernement du Québec. 2006. Québec Pandemic Influenza Plan—Health Mission. Ministère de la Santé et des Services sociaux, Québec, Canada, 123 p.
- Government of British Columbia. 2012. British Columbia Pandemic Influenza Preparedness Plan. Vancouver, Canada, BC Ministry of Health.
- Government of Canada. 2018. Canadian Pandemic Influenza Preparedness: Planning Guidance for the Health Sector. Minister of Health, Pan-Canadian, Ottawa, Canada, Public Health Network, 64 p.
- Government of Ontario 2013. Ontario Health Plan for an Influenza Pandemic. Ministry of Health, Health System Emergency Management Branch. http://www.health.gov.on.ca/en/pro/programs/emb/pan_flu/pan_flu_plan.aspx.
- Hanvoravongchai, Piya, Wiku Adisasmito, Pham Ngoc Chau, Alexandra Conseil, Joia de Sa, Ralf Krumkamp, Sandra Mounier-Jack, et al. 2010. “Pandemic Influenza Preparedness and Health Systems Challenges in Asia: Results from Rapid Analyses in 6 Asian Countries.” BMC Public Health 10 (1): 1–11. doi:10.1186/1471-2458-10-322.
- Henry, B., and S. Gadient. 2017. “Outbreak Detection: Canada’s Pandemic Vaccine Strategy.” Canada Communicable Disease Report 43 (7/8): 164–167. doi:10.14745/ccdr.v43i78a05.
- Heymann, David L., Lincoln Chen, Keizo Takemi, David P. Fidler, Jordan W. Tappero, Mathew J. Thomas, Thomas A. Kenyon, et al. 2015. “Global Health Security: The Wider Lessons from the West African Ebola Virus Disease Epidemic.” Lancet (London, England) 385 (9980): 1884–1901. doi:10.1016/S0140-6736(15)60858-3.
- Homsy, G. C., and M. E. Warner. 2015. “Cities and Sustainability: Polycentric Action and Multilevel Governance.” Urban Affairs Review 51 (1): 46–73. doi:10.1177/1078087414530545.
- Hooghe, L., and G. Marks. 2001. Types of Multi-Level Governance. European integration online papers (EIoP) 5(11), 30 p.
- Inwood, Gregory J., Patricia O’Reilly, and Carolyn Johns. 2011. Intergovernmental Policy Capacity in Canada: Inside the Worlds of Finance, Environment, Trade, and Health. Montreal and Kingston: McGill-Queen’s Press - MQUP, 548 p.
- Jennings, L. C., A. S. Monto, P. K. Chan, T. D. Szucs, and K. G. Nicholson. 2008. “Stockpiling Prepandemic Influenza Vaccines: A New Cornerstone of Pandemic Preparedness Plans.” The Lancet. Infectious Diseases 8 (10): 650–658. doi:10.1016/S1473-3099(08)70232-9.
- Katz, R., M. Wentworth, J. Quick, A. Arabasadi, E. Harris, K. Geddes, and A. Jha. 2018. “Enhancing Public—Private Cooperation in Epidemic Preparedness and Response.” World Medical & Health Policy 10 (4): 420–425. http://dx.doi.org.proxy.bib.uottawa.ca/10.1002/wmh3.281. doi:10.1002/wmh3.281.
- Klonowska, K., & Bindt, P. 2020. The COVID-19 pandemic two waves of technological responses in the european union.Hague Centre for Strategic Studies. http://www.jstor.com/stable/resrep24004
- Krumkamp, R., S. Mounier-Jack, A. Ahmad, R. Reintjes, and R. Coker. 2010. “Evaluating Health Systems’ Preparedness for Emerging Infectious Diseases: A Novel Conceptual and Analytic Framework.” Health Policy (Amsterdam, Netherlands) 98 (2–3): 91–97. http://dx.doi.org.proxy.bib.uottawa.ca/10.1016/j.healthpol.2010.06.004. doi:10.1016/j.healthpol.2010.06.004.
- Madhav, N., B. Oppenheim, M. Gallivan, P. Mulembakani, E. Rubin, and N. Wolfe. 2017. “Pandemics: Risks, Impacts, and Mitigation.” In Disease Control Priorities (Third Edition): Volume 9, Disease Control Priorities, edited by D. T. Jamison, H. Gelband, S. Horton, P. Jha, R. Laxminarayan, C. N. Mock, and R. Nugent. Washington, DC: World Bank.
- Nelson, C., N. Lurie, J. Wasserman, and S. Zakowski. 2007. “Conceptualizing and Defining Public Health Emergency Preparedness.” American Journal of Public Health 97 (Supplement_1): S9–S11. doi:10.2105/AJPH.2007.114496.
- Nilsson, M., T. Zamparutti, J. E. Petersen, B. Nykvist, P. Rudberg, and J. McGuinn. 2012. “Understanding Policy Coherence: Analytical Framework and Examples of Sector–Environment Policy Interactions in the EU.” Environmental Policy and Governance 22 (6): 395–423. doi:10.1002/eet.1589.
- Oshitani, H., T. Kamigaki, and A. Suzuki. 2008. “Major Issues and Challenges of Influenza Pandemic Preparedness in Developing Countries.” Emerging Infectious Diseases 14 (6): 875–880. doi:10.3201/eid1406.070839.
- Peeri, Noah C., Nistha Shrestha, Md Siddikur Rahman, Rafdzah Zaki, Zhengqi Tan, Saana Bibi, Mahdi Baghbanzadeh, Nasrin Aghamohammadi, Wenyi Zhang, and Ubydul Haque. 2020. “The SARS, MERS and Novel Coronavirus (COVID-19) Epidemics, the Newest and Biggest Global Health Threats: what Lessons Have we Learned?” International Journal of Epidemiology 49 (3): 717–726. doi:10.1093/ije/dyaa033.
- Quigley, K. 2013. “Man Plans God Laughs”: Canada’s National Strategy for Protecting Critical Infrastructure.” Canadian Public Administration 56 (1): 142–164. doi:10.1111/capa.12007.
- Savard, J. F., J. P. Villeneuve, and I. Caron. 2013. “Institutional Policy Coherence: The Case of Swiss Transparency Act.” Jahrbuch der Schweizerischen Verwaltungswissenschaften 4 (1): 151–161.
- Savard, J.-F. 2010. “La cohérence des politiques publiques.” In L’analyse des politiques publiques, edited by S. Paquin, L. Bernier and G. Lachapelle, 309–335. Montréal: Les Presses de L’Université de Montréal.
- Schiffino, N., L. Taskin, C. Donis, and J. Raone. 2015. Organizing After Crisis: The Challenge of Learning, Bruxelles, Belgium: Peter Lang.
- Stein, F., and D. Sridhar. 2017. “Health as a “Global Public Good”: Creating a Market for Pandemic Risk.” BMJ (Clinical Research ed.) 358: j3397. doi:10.1136/bmj.j3397.
- Studlar, D., and P. Cairney. 2019. “Multilevel Governance, Public Health and the Regulation of Food: Is Tobacco Control Policy a Model?” Journal of Public Health Policy 40 (2): 147–165. doi:10.1057/s41271-019-00165-6.
- Vancouver Coastal Health. 2018. The Regional Pandemic Outbreak Response Plan, Vancouver, British Columbia.
- Agence de la santé et des services sociaux de Montréal. 2007. Le Plan montréalais de lutte à une pandémie d’influenza. Agence de la santé et des services sociaux de Montréal, Montréal, Canada.
- World Health Organization. 2009. Pandemic Influenza Preparedness and Response: A WHO Guidance Document. Geneva:World Health Organization.
- World Health Organization. 2018. Essential Steps for Developing or Updating a National Pandemic Influenza Preparedness Plan (No. WHO/WHE/IHM/GIP/2018.1). Geneva: World Health Organization.
- World Health Organization. 2020. “WHO Director-General’s opening remarks at the media briefing on COVID-19.” Accessed 11 March 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19-11-march-2020