Abstract
Pituitary metastasis is a rare situation in clinical practice and has been estimated to take up no more than 1% of tumors found in sellar region, in which the incidence of a secondary metastatic lesion to the sella by hepatocellular carcinoma (HCC) is extremely rare, only 15 cases of which has been reported yet. The aim of this study is to share the detailed procedures and clinical strategies of this rare case and review the whole 15 HCC-derived PM cases since 1857. We present an extremely rare case of an HCC metastasis to the pituitary gland with his condition and clinical course. We then discuss the dominant diagnosis and clinical therapy of HCC-derived PM and review the literature. This case demonstrated the difficulties encountered in the diagnosis of PM and the need for accurate judgment when confronting pituitary tumors with atypical features. In addition, the appropriate therapy needs to be well considered, because of the poor prognosis and severe symptoms.
Abbreviations: CTA: computed tomography angiography; ETTS: endoscopic transnasal transsphenoidal surgery; HCC: hepatocellular carcinoma; ICA: internal carotid artery; PET-CT: positron emission tomography-computed tomography; PM: pituitary metastasis
Introduction
Pituitary metastasis (PM) is a rare situation in clinical practice and has been estimated to take up no more than 1% of tumors found in the sellar region (He et al. Citation2015). The first case of PM was discovered at autopsy in 1857, which was defined as a disease in 1913 (Chiang et al. Citation1990). Clinical presentation, tumor growth and progression, and therapeutic strategies should be brought to the forefront due to its unique feature. Majority of PMs are asymptomatic, only 7% of which are symptomatic (Teears and Silverman Citation1975). Thus, they are generally discovered at autopsy specimens. The main presenting symptoms in patients with PMs are oculomotor nerve palsy and/or diabetes insipidus (DI) (He et al. Citation2015). Common symptoms of primary pituitary adenoma, such as hormone dysfunction, are much less encountered by physicians (Max et al. Citation1981).
In the current era, many cases have been reported, which involved a variety of original metastatic diseases, such as thyroid papillary carcinoma (Ardhaoui et al. Citation2020), lung adenocarcinoma (Yao et al. Citation2019), gastric carcinoma (Prablek et al. Citation2019), renal cell carcinoma (Gopan et al. Citation2007), breast carcinoma (Ng et al. Citation2020), and melanoma (Chiang et al. Citation1990). Among them, breast cancer (40%) and lung cancer (33%) are reported as the most common origins (Chiang et al. Citation1990). PM from HCC has been rarely reported in literature. Up to date, only 15 cases have been revealed (Aung et al. Citation2002; Karamouzis et al. Citation2003; Komninos et al. Citation2004; Hirsch et al. Citation2005; Moreno-Perez et al. Citation2007; Takigawa et al. Citation2011; Tamura et al. Citation2013; Wilson and Kirby Citation2013; He et al. Citation2015; Tanaka et al. Citation2015; Mattogno et al. Citation2017; Mishima et al. Citation2019).
In this study, we reported a case of a PM patient with a previous history of HCC, who presented unilateral visual defect and oculomotor nerve palsy with a headache. The majority of pituitary mass was within the sphenoidal sinus, with extension to the optic canal and compression of the optic nerve and oculomotor nerve, which cause clinical symptoms. The patient was previously diagnosed with hepatocellular carcinoma and was found to have metastatic tumors in lung, spinal, and sellar region by PET-CT. Subsequently, the patient underwent endoscopic endonasal transsphenoidal surgery (EETS) for decompression. In addition, pathologic analysis demonstrated the PM from HCC. At last, we presented a systemic review of literature to highlight the rarity of the pituitary gland as a location of HCC metastasis. The aim of this study is to share the detailed procedures and clinical strategies in this rare case and review the whole 15 HCC-derived PM cases since 1857, of which the significance is growing.
Clinical presentation
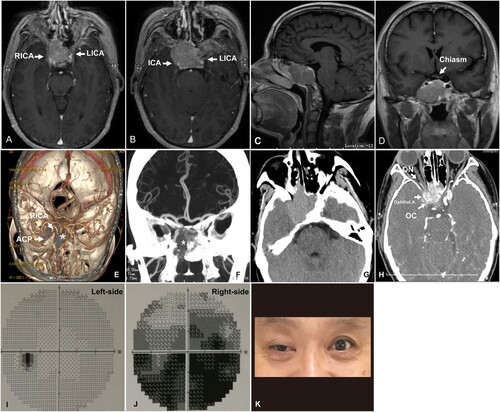
A 50-year-old man presented with one-month history of onset of worsening vision and diplopia on the right side with a previous surgical history of hepatic carcinoma. The patient denied nausea, vomiting, polyuria, polydipsia, and impaired eye movement. The patient was then admitted to our institution for further treatment, where pituitary magnetic resonance imaging (MRI) with contrast revealed a 2.9 × 2.8 × 2.3 cm mass centered within the sella turcica. The majority of the tumor was located in the sphenoidal sinus with lateral extension into the right optic canal and posterior extension into the superior part of the clivus. Adjacent structures were involved as well, in addition, the right internal carotid artery (ICA) and cavernous sinus were shifted to the posterior portion (Figure (A–D)). Moreover, the cranial computed tomography angiography (CTA) revealed the narrowed and constricted right ICA due to mass compression. The optic canal was also involved, sparing the optic chiasm (Figure (E–H)). Ophtalmic examination indicated right-side hemianopia. However, initial laboratory tests of hormonal levels and electrolytes are normal.
Figure 1. Preoperative MRI T1 with contrast, CTA, and ophthalmic examination. Enhanced Axial (A, B), sagittal (C), and coronal (D) MRI showed a sellar pituitary mass with sphenoidal extension and invasion. The right ICA was compressed and shifted posteriorly. The optic chiasm was not affected. 3D reconstruction (E), coronal (F), coronal with and without (G) contrast showed that the main portion of the tumor (*) was located in the sphenoidal sinus. The right ICA and the optic canal were involved (H). (I, J) The test revealed a severe visual field defect on the right side and a slight defect on the left side. (K) The patient presented a symptom with CN III palsy.
The patient presented a 4-year history of HCC (size 6 × 6 cm) in the right liver lobe and underlying hepatitis C virus-associated Child-Pugh stage B liver cirrhosis. Sorafenib has been using for a long time and recently lenvantinib or atezolizumab/bevacizumab were used as standard therapies in the treatment of metastatic HCC (Chapman et al. Citation2018; Kudo et al. Citation2018; Finn et al. Citation2020; Tang et al. Citation2020). Because of the poor physical condition of this patient, he rejected the choice of chemoradiotherapy and was treated with tumorectomy and post-operative chemoradiotherapy. Indeed, most chemo drugs do not have a great effect on liver cancer. However, chemotherapy is currently acknowledged worldwide as the standard treatment plan for advanced HCC including patients who have extrahepatic metastasis (Ikeda et al. Citation2018). And radiotherapy can offer high local control rates in unresectable HCC, especially in metastatic cases, radiotherapy can provide good palliation (Chen Citation2019). In this case, the post-operative PET-CT scan showed vertebral and lung metastases and trace signal in the sellar region, which means that the residual tumor was left. So the treatment of chemo and radiotherapy were decided to be performed, which was also confirmed by multidisciplinary discussions.
According to the clinical presentation, imaging and history, the diagnosis should be considered as PM rather than primary pituitary adenoma for the reasons as follows (He et al. Citation2015). The tumor center was originated from the sphenoidal sinus and directly invaded the optic canal, whereas the primary pituitary adenoma is supposed to stay within the sella turcica, with medial cavernous sinus membrane and diaphragma sellae breakthrough and extension of the parasellar and suprasellar region (Chiang et al. Citation1990). The patient presents with oculomotor nerve palsy due to the invasion of the optic canal rather than the breakthrough of oculomotor triangle which was prevalent in invasive pituitary adenoma (Teears and Silverman Citation1975). Ophthalmic testing indicated hemianopia, which is unlikely in pituitary adenoma patients as they would instead presenting as bitemporal hemianopsia (Figure (I–K)). Consequently, the surgical strategy should focus on the decompression of optic canal for the ophthalmic symptom relief. Besides, the surgical approach should follow the major portion of the tumor towards the direction of the optic canal. Following the operation, radiology and chemotherapy were also recommended.
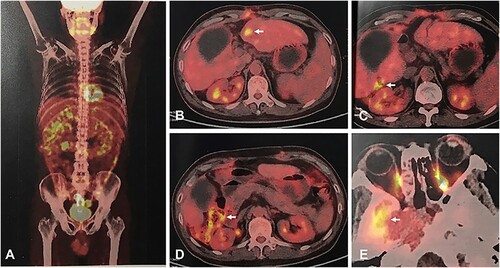
Subsequently, the patient underwent the EETS to relieve the compression symptoms. Due to the abundant blood supply in the tumor, full blood products were prepared for potential intraoperative blood transfusion. During the surgery, we discovered a soft solid mass with distinct hypervascularity compared to typical pituitary adenomas (Figure (A,B). Post-operative MRI indicated that the mass effect of the tumor was resolved, and the right ICA was returned to normal position (Figure (C,D). The patient displayed a slight visual improvement and recovered well following the total resection surgery. Intraoperative frozen section revealed a solid tumor, in which neoplastic cells were irregular-shaped with high-grade nuclear atypia. The histopathological analysis showed a malignant hepatic cells infiltration with positive immunohistochemistry staining for cytokeratin CK18 and the Ki67, up to approximately 20% (Figure (E–H)). Moreover, the IHC analysis showed negative results for pituitary hormones (growth hormone, PRL, ACTH, TSH, FSH, and LH). The post-operative positron emission tomography-computed tomography (PET-CT) scan showed vertebral and lung metastases and trace signal in the sellar region (Figure ), thus the patient was treated with chemotherapy.
Figure 2. Intraoperative snapshot and histological tumor specimens. (A, B) exhibited the tumor (*) was soft and with abundant blood supply. (C, D) Post-operative MRI indicated the mass effect of the tumor was resolved and the right ICA was returned to normal locality. (E) Hematoxylin and eosin staining of the pituitary tumor demonstrating a tumor without pituitary tissues. Immunohistochemical expression of (F) hepatocytes, (G) ki67, and (H) CK18. Bar: 60 μm.
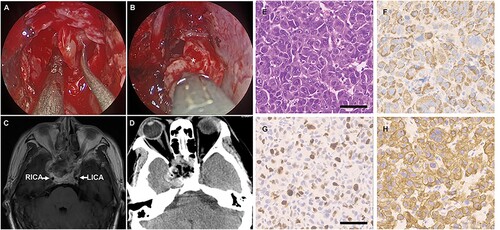
Figure 3. Post-operative PET-CT scan. PET-CT showed high radioactive uptake in the right and anterior abdominal wall (A), liver lobe (B, C), colonic wall (D), and active lesions in the sphenoid sinus (E).
The symptom of headache was relieved, while hemianopia persisted. The patient consented to undergo radio- and chemotherapy on an outpatient basis following discharge. He was recommended to take cisplatin and paclitaxel as subsequent therapy. The patient died of deterioration of the HCC six months after the operation. All performance was approved by the ethics committee of Shanghai General Hospital and the patient consented to the publication.
Discussion
The majority of masses in the sellar region are adenoma-typed pituitary tumors. Metastasis to the pituitary gland is rare in clinical practice and has been estimated to be approximately 1% of tumors discovered in the sellar region (He et al. Citation2015). Although rare, an increasing number of PM cases have been reported during the past decades. The majority of these reports are single case reports, or small case series, and few systematic reviews on this topic were published. A pooled analysis showed that about 1.9% of patients with metastatic malignant cancer could be accompanied by such an uncommon situation (He et al. Citation2015). Lung and breast carcinoma are two of the most common PM origin followed by renal cell, gastrointestinal, prostate carcinoma (Altay et al. Citation2012), with rare cases from HCC.
PMs from HCC are extremely rare, and only 15 cases of PM from HCC have been reported up to date (Table ). Based on analysis of the previous reports and our own case, we found that the DI is extremely rare in the patient with PM from HCC (only 4 out of 15), except which headache (11/15), nerves palsies (9/15), and vision defect (7/15) are more common. Male preponderance has been exerted in this examination. Consistent with a previous study, 13 out of 15 patients are males (Tangkijvanich et al. Citation2004). A recent study suggested that the PM from HCC showed a significantly lower incidence of anterior pituitary insufficiency comparing to the other types of PM (He et al. Citation2015), only 40% of which were accompanied with slight or moderate endocrinological dysfunctions and only 1 case showed panhypopituitarism. Interestingly, among these 16 cases, the unilateral visual field defect was only presented in our case, which is dissimilar with pituitary adenoma presented as bitemporal hemianopsia caused by charism compression. The patient also presents with oculomotor nerve palsy because of invasion in the optic canal rather than the breakthrough of oculomotor triangle which was prevalent in invasive pituitary adenoma. Consequently, the surgical strategy should focus on the decompression of optic canal for the ophthalmic symptom relief, and the surgical approach should follow the majority of the tumor in the direction of the optic canal.
Table 1. Pooled analysis of HCC-derived PM.
In this case, the right visual field defect and oculomotor nerve were the first signs of HCC-derived PM. The presence of HCC was already evident from previous surgical history, and metastasis was revealed from PET-CT. The pathological diagnosis made from the surgical specimen also revealed advanced-stage cancer with widely metastatic disease. Because both HCC and pituitary adenomas originated from epithelial cells, it is possible to show similar pictures, leading to the misdiagnosis of PM. Mishima et al. reported a case of clival metastasis of HCC with an initial histopathological diagnosis of atypical pituitary adenoma, which emphasized the importance of the combination of the pathological diagnosis and the patient’s clinical course (Mishima et al. Citation2019). Due to the aggressive nature of the tumor mass, the presence of marked atypia, and increased mitotic activity should rise to the suspicion of malignance. Ambalavanan et al. reported a rare case of HCC metastasizing to pituitary and cavernous sinus, revealing the aggressive nature, which caused panhypopituitarism and bilateral ophthalmoplegia (Ambalavanan et al. Citation2020). Besides, the intriguing aspects of our case were the enriched blood supply within the sellar region because of the metastasis of HCC and the symptomatic PM. In general, HCC is known to with rich vascularity because of its aggressive nature and propensity for hematogenous dissemination, hemorrhage from HCC-derived PM frequently results in a critical state. Tamura et al. (Citation2013) reported a case with HCC-derived PM, who was admitted to the local hospital due to shock caused by hemorrhage from the metastatic tumor. And Takigawa et al. (Citation2011) reported a case with a critical state caused by nasal bleeding and was impossible for general anesthesia, so endovascular transarterial embolization was selected. According to CTA, which was performed at the time of submission to our hospital, images revealed the rich metastatic tumor vascularity. Therefore, the surgery was performed not only for effective decompression, but also for the prevention of hemorrhage. It is worth noting that PMs from HCC showed high aggressiveness and hypervascularity, so we should prepare enough blood in case of intraoperative blood transfusions.
In the transnasal transsphenoidal approach, maximized resection and aggressive treatment exert effective relief of clinical symptoms, but do not improve the survival rate (Morita et al. Citation1998). Although the patient died six months later, he responded symptomatically well to the operative treatment. The short survival time is consistent with that of HCC patients with a median survival time of five months, which suggested that the survival time was not improved despite of aggressive treatment aiming at PM. Generally, distant metastases usually have a poor prognosis. However, surgical resection of the metastatic lesion can effectively relieve mass effect, alleviate symptoms caused by the metastatic tumor, and improve life quality. Furthermore, the patient declined adjuvant treatments. The above strategies indicated that despite of progressive treatment, the survival time and prognosis is not improved after therapy of HCC-derived PM, and the treatment should be basically palliative and based on the symptoms.
In summary, with regard to the management of HCC-derived PM, treatment including surgery, radiotherapy, chemotherapy, or combined treatment modalities can be considered. Literature shows no significance in survival time between surgical and nonsurgical therapy groups, which illustrated that the prognosis of PM is generally related to the characteristics of primary malignancy (Aung et al. Citation2002; Karamouzis et al. Citation2003; Komninos et al. Citation2004; Hirsch et al. Citation2005; Moreno-Perez et al. Citation2007; Takigawa et al. Citation2011; Tamura et al. Citation2013; Wilson and Kirby Citation2013; He et al. Citation2015; Tanaka et al. Citation2015; Mattogno et al. Citation2017; Mishima et al. Citation2019). Therefore, the management of patients with PM is palliative, aiming to minimize morbidity, alleviate clinical symptoms, and maximize the quality of life.
Authors’ contributions
AZ and LY were the main contributors to the writing of the manuscript. SL performed the histological examination of the tumor tissues. HX provided the patient data and images. ML analyzed and interpreted the literature reviews of metastasis of hepatocellular carcinomas. YX and YX are the first author’s advisors for the elaboration of the master’s thesis in medicine. The authors read and approved the final manuscript.
Consent for publication
Written informed consent was obtained from the patient for publication of this case, including all individual details and accompanying images. The consent form is available for review by the editor of the journal upon request.
Ethics approval and consent to participate
This study was approved by the Medical Ethics Committee of Shanghai General Hospital of Shanghai Jiaotong University.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data and materials supporting this study are available, without breaching participant confidentiality, in the Harvard Dataverse Repository [https://dataverse.harvard.edu/] at https://doi.org/10.7910/DVN/PWXGFD.
Additional information
Funding
References
- Altay T, Krisht KM, Couldwell WT. 2012. Sellar and parasellar metastatic tumors. Int J Surg Oncol. 2012:647256–647256.
- Ambalavanan J, Peravali M, Perry DJ. 2020. Rare case of hepatocellular carcinoma metastasising to the pituitary and cavernous sinus causing panhypopituitarism and bilateral ophthalmoplegia. BMJ Case Rep. 27;13(10):e236377.
- Ardhaoui H, Halily S, Elkrimi Z, Rouadi S, Abada R, Roubal M, Mahtar M. 2020. Thyroid papillary carcinoma with an insular component metastasizing to the sella turcica and sphenoid sinus: case report. Int J Surg Case Rep. 67:254–257.
- Aung TH, Po YC, Wong WK. 2002. Hepatocellular carcinoma with metastasis to the skull base, pituitary gland, sphenoid sinus, and cavernous sinus. Hong Kong Medical Journal [Xianggang yi xue za zhi]. 8:48–51.
- Chapman WC, Korenblat KM, Fowler KJ, Saad N, Khan AS, Subramanian V, Doyle MBM, Dageforde LA, Tan B, Grierson P, et al. 2018. Hepatocellular carcinoma: where are we in 2018? Curr Probl Surg. 55:450–503.
- Chen CP. 2019. Role of radiotherapy in the treatment of hepatocellular carcinoma. J Clin Transl Hepatol. 7:183–190.
- Chiang MF, Brock M, Patt S. 1990. Pituitary metastases. NeuroChirurgia (Stuttg). 33:127–131.
- Finn RS, Qin S, Ikeda M, Galle PR, Ducreux M, Kim TY, Kudo M, Breder V, Merle P, Kaseb AO, et al. 2020. Atezolizumab plus bevacizumab in unresectable hepatocellular carcinoma. N Engl J Med. 382:1894–1905.
- Gopan T, Toms SA, Prayson RA, Suh JH, Hamrahian AH, Weil RJ. 2007. Symptomatic pituitary metastases from renal cell carcinoma. Pituitary. 10:251–259.
- He W, Chen F, Dalm B, Kirby PA, Greenlee JD. 2015. Metastatic involvement of the pituitary gland: a systematic review with pooled individual patient data analysis. Pituitary. 18:159–168.
- Hirsch D, Benbassat CA, Drozd T, Okon E, Blum I. 2005. Pituitary and bilateral adrenal enlargement: an unusual presentation of hepatocellular carcinoma. J Endocrinol Investig. 28:454–458.
- Ikeda M, Morizane C, Ueno M, Okusaka T, Ishii H, Furuse J. 2018. Chemotherapy for hepatocellular carcinoma: current status and future perspectives. Jpn J Clin Oncol. 48:103–114.
- Karamouzis MV, Melachrinou M, Fratzoglou M, Labropoulou-Karatza C, Kalofonos HP. 2003. Hepatocellular carcinoma metastasis in the pituitary gland: case report and review of the literature. J Neuro-Oncol. 63:173–177.
- Komninos J, Vlassopoulou V, Protopapa D, Korfias S, Kontogeorgos G, Sakas DE, Thalassinos NC. 2004. Tumors metastatic to the pituitary gland: case report and literature review. J Clin Endocrinol Metab. 89:574–580.
- Kudo M, Finn RS, Qin S, Han KH, Ikeda K, Piscaglia F, Baron A, Park JW, Han G, Jassem J, et al. 2018. Lenvatinib versus sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: a randomised phase 3 non-inferiority trial. Lancet (London, England). 391:1163–1173.
- Mattogno PP, LAR G, Pompucci A, Coli A, Rigante M, Mangiola A. 2017. An extremely rare case of a single isolated pituitary metastasis from hepatocellular carcinoma. J Neurosurg Sci. 61:213–215.
- Max MB, Deck MD, Rottenberg DA. 1981. Pituitary metastasis: incidence in cancer patients and clinical differentiation from pituitary adenoma. Neurology. 31:998–1002.
- Mishima H, Ayabe J, Watanabe M, Togin S, Tsuchiya Y, Kawasaki T, Noda N, Maruyama T, Tanaka Y. 2019. Clival metastasis of hepatocellular carcinoma with an initial histopathological diagnosis of atypical pituitary adenoma. J Neurol Surg Rep. 80:e18–e22.
- Moreno-Perez O, Peiro FM, Lopez P, Boix E, Meoro A, Serna-Candel C, Aranda FI, Pico AM. 2007. An isolated pituitary metastasis as presentation of a differentiated hepatocellular carcinoma mimicking a nonfunctioning macroadenoma. J Endocrinol Investig. 30:428–433.
- Morita A, Meyer FB, Laws ER, Jr. 1998. Symptomatic pituitary metastases. J Neurosurg. 89:69–73.
- Ng S, Fomekong F, Delabar V, Jacquesson T, Enachescu C, Raverot G, Manet R, Jouanneau E. 2020. Current status and treatment modalities in metastases to the pituitary: a systematic review. J Neuro-Oncol. 146:219–227.
- Prablek M, Srinivasan VM, Srivatsan A, Holdener S, Oneissi M, Heck KA, Jalali A, Mandel J, Viswanathan A, Patel AJ. 2019. Gastrointestinal stromal tumor with intracranial metastasis: case presentation and systematic review of literature. BMC Cancer. 19:1119–1119.
- Rocca G. L., Mattogno P. P., Pompucci A., Coli A., Rigante M., Mangiola A. 2017. An extremely rare case of a single isolated pituitary metastasis from hepatocellular carcinoma. J Neurosurg Sci. 61(2):213–215.
- Takigawa T, Matsumaru Y, Hayakawa M, Ikeda K, Matsumura A. 2011. Transarterial embolization with use of lipiodol and gelatin sponge for active nasal bleeding from hepatocellular carcinoma metastasis in the pituitary gland. Neurol Med Chir (Tokyo). 51:592–595.
- Tamura T, Kawamura Y, Ikeda K, Seko Y, Fukushima T, Kumada H, Yamada S, Matumaru Y. 2013. Hepatocellular carcinoma metastasis to the brain mimicking primary pituitary tumor around the sella turcica. Clin J Gastroenterol. 6:319–325.
- Tanaka T, Hiramatsu K, Nosaka T, Saito Y, Naito T, Takahashi K, Ofuji K, Matsuda H, Ohtani M, Nemoto T, et al. 2015. Pituitary metastasis of hepatocellular carcinoma presenting with panhypopituitarism: a case report. BMC Cancer. 15:863.
- Tang J, Sui CJ, Wang DF, Lu XY, Luo GJ, Zhao Q, Lian QY, Jeong S, Lin XM, Zhu YJ, et al. 2020. Targeted sequencing reveals the mutational landscape responsible for sorafenib therapy in advanced hepatocellular carcinoma. Theranostics. 10:5384–5397.
- Tangkijvanich P, Mahachai V, Suwangool P, Poovorawan Y. 2004. Gender difference in clinicopathologic features and survival of patients with hepatocellular carcinoma. World J Gastroenterol. 10:1547–1550.
- Teears RJ, Silverman EM. 1975. Clinicopathologic review of 88 cases of carcinoma metastatic to the pituitary gland. Cancer. 36:216–220.
- Wilson TC, Kirby PA. 2013. A 50-year-old man with back pain and a sellar mass. Metastatic hepatocellular carcinoma. Brain Pathol. 23:365–366.
- Wilson T. C., Kirby P. A. 2013. A 50-year-old man with back pain and a sellar mass. Metastatic hepatocellular carcinoma. Brain Pathol. 23(3):365–366.
- Yao H, Rui W, Zhang Y, Liu Y, Lin S, Tang H, Zhao W, Wu Z. 2019. Prolactin-secreting lung adenocarcinoma metastatic to the pituitary mimicking a prolactinoma: a case report. Neurosurgery. 85:E773–E778.
